Adult Attention-Deficit/Hyperactivity Disorder: Diagnosis, Treatment, and Implications for Drug Development: Proceedings of a Workshop (2024)
Chapter: 4 Shared Decision-Making
4
Shared Decision-Making
Highlights of Key Points Made by Individual Speakers*
- Given the multiple possible treatment options and the need for individualized assessment of risks and benefits, shared decision making is a good paradigm for treatment of ADHD in adults. (Olfson)
- Social media contains both useful information and misinformation about ADHD that patients may turn to for medical advice. Providers can leverage these platforms by directing their patients toward reputable sources. (Gold, Walker)
- Medication provides a foothold, but it is not sufficient to treat ADHD on its own. Adults with ADHD also need to learn healthy coping strategies. (Barron, Chronis-Tuscano)
- Educating patients, teachers, and medical providers about ADHD in adults will require prioritizing and increasing access to structured, accessible, and trusted information resources. (Arria, Patel, Walker)
- To better track symptoms and monitor patient response to medication, measurement-based care should be used for ADHD in adults. (Cheyette)
*This list is the rapporteurs’ summary of points made by the individual speakers identified, and the statements have not been endorsed or verified by the National Academies of Sciences,
Engineering, and Medicine. They are not intended to reflect a consensus among workshop participants.
Presentations and discussions about shared decision-making involved sharing perspectives and resources for prescribers, clinicians, and patients regarding treatment and management options for adult ADHD; practical approaches to working through barriers (e.g., stigma and misdiagnosis) to appropriately diagnose and treat adults with ADHD; and considering opportunities for shared decision making between patients and their providers.
ADOPTING MEASUREMENT-BASED CARE
Issues of cognition are treated differently than disorders such as hypertension, asthma, and obesity, said Weisenbach. Rosier agreed adding, “If your blood pressure is high when you go into your doctor’s office, they are not going to say, ‘Here, you need a hypertension medication.’ They are going to say, ‘Let’s . . . monitor your blood pressure for a period of time, or come back for another visit so that we can reassess.’ Why aren’t we doing that . . . with ADHD . . . [or] other cognitive disorders?” She compared the care she receives for her asthma, which includes keeping track of symptoms and filling out a checklist at every doctor’s visit, to that for her ADHD, which simply consists of her provider asking how she feels and giving her a prescription.
Providers need to monitor a patient’s response to medication, said Cheyette. Current symptom-tracking measures for ADHD are inadequate, and while the ADHD Quality-of-Life Scale has been validated (Brod et al., 2006), it is long and impractical for clinicians to deliver to their patients before each visit, he said. Some clinicians use the ASRS, which is shorter, but it was validated as a diagnostic screening tool and not for tracking.
Cheyette developed the Hyperactivity, Impulsivity, Inattention Symptom Rating Scale (HII-5)1, which consists of five questions, each scored between 0 and 3. Patients can complete the HII-5 in a minute or two, and they obtain a score from 0 to 15. This enables the provider to monitor a patient and track response to treatment across visits. “It’s not meant to be exhaustive,” said Cheyette, but it provides sufficient information “that you can quickly surmise how their ADHD is responding to your last medication change and make adjustments.” The HII-5 scale
___________________
1 Available at https://www.psychologytoday.com/us/blog/1-2-3-adhd/202306/tracking-symptom-severity-in-adhd (accessed April 26, 2024).
was modeled after similar scales used to routinely screen for depression, such as the Patient Health Questionnaire–9 (PHQ-9), and anxiety, such as the Generalized Anxiety Disorder 7-Item (GAD-7), he added. Cheyette presented tracking data from individual patients demonstrating the responsiveness of the HII-5 score to medical treatment for ADHD, as well as the overall correlation between changes in the scores on HII-5, PHQ-9, and GAD-7 (Figure 4-1). “There is a real need” for this sort of measurement-based care to track the progress of adult ADHD patients over time, said Olfson, noting that “a longitudinal perspective is very helpful in informing clinical decision making.” The HII-5 is available for anyone to use, said Cheyette.
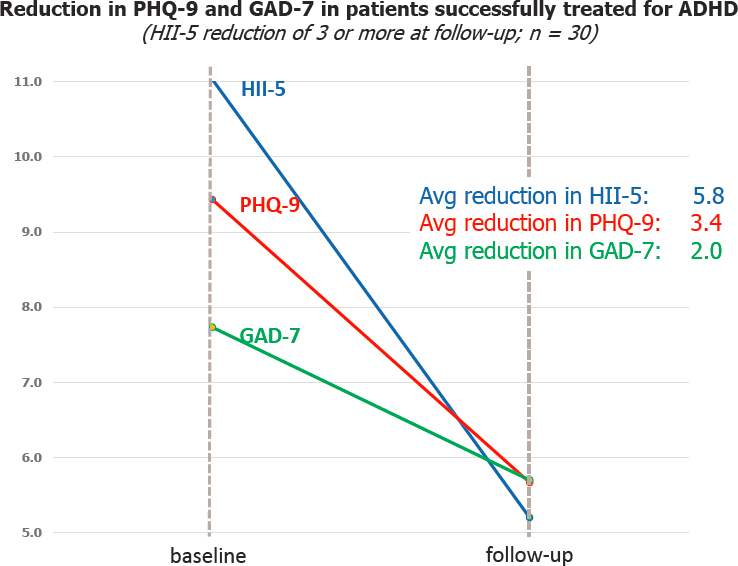
NOTES: Graph shows data from one patent out of a group of 30. Avg = average; GAD-7 = Generalized Anxiety Disorder 7-item; HII-5 = Hyperactivity, Impulsivity, Inattention Symptom Rating Scale; PHQ-9 = Patient Health Questionnaire–9.
SOURCE: As presented by Benjamin Cheyette on December 13, 2023.
USING SHARED DECISION MAKING
Shared decision making is a model for the clinician–patient interaction in which both parties contribute information that is used in the clinical decision-making process, said Olfson. This includes decisions regarding whether to initiate pharmacotherapy, which medication to use, and what dose to use. Studies of depression have shown that shared decision making improves adherence with medication and improves outcomes (Bauer et al., 2014; Clever et al., 2006; Rossom et al., 2016), suggesting the same would be true in adult ADHD, he said.
Shared decision making can start with clinicians presenting technical information to the patient about the patient’s condition, including the risks and benefits of available options, said Olfson. He noted that, given the information available online, “sometimes that discussion goes both ways. . . . People with ADHD often know more about . . . their condition [and] ADHD [in general] than their clinician.” Patients inform clinicians about their goals and preferences regarding the consequences of treatment. All this information feeds into the decisions that are made, and “hopefully these decisions will reflect the priorities, goals, values, and preferences of the patient,” he said. Obtaining the most robust efficacy may be paramount for some patients, while others may prioritize minimizing the risk of substance abuse. Ideally, Chronis-Tuscano added, providers “could engage in shared decision making regarding whether to begin treatment with stimulants, CBT, organizational skills, or nonstimulants. But limited mental health literacy may make this challenging in some cases.”
Providing her perspective as an adult with ADHD, Kylie Barron described her experience with shared decision making. When she learned that she was pregnant, she stopped taking her ADHD medicine without talking to her doctor, out of concern that it might harm the baby. But after Barron left her car running in the garage and the gas stove on, her own safety became a serious concern. She felt “hopeless. . . . I’ve got to choose between me surviving and this unborn child surviving.” Barron’s doctor met with her to address these concerns. Over the course of a one-and-a-half-hour visit, the two worked together to review guidelines describing the risks of various ADHD medicines to the fetus. “I [was] able to make an informed decision about my own health after that appointment,” she said. Adults with ADHD talk among themselves about self-empowerment and going to the doctor armed with questions, said Gordon.
It is critical for providers, especially general care practitioners, to take the time to talk with their patients and meet them where they are regarding treatment and diagnosis. “When we go to the doctor . . . there’s not a lot of time left to talk about ADHD. I don’t think I’ve ever told my
doctor that I had four car accidents and ran somebody over,” Gordon shared. That might have led to an earlier diagnosis, but it did not come up. If doctors were trained to ask and answer those questions, “there’d be a partnership formed that would lead to positive outcomes all around,” he added. After all, Gordon noted, a person’s ability to access the life-changing benefits of ADHD medication “all starts in that office with the diagnosis.”
Cheyette agreed that poor training of practitioners stands in the way of shared decision making. Shared clinical decision making works best for disorders where there is more than one reasonable treatment option and a need to balance risks and benefits, said Olfson; furthermore, “there’s a lot that we don’t know [regarding] the lives of the individuals who present for care.” For these reasons, he said, “the shared decision-making paradigm fit[s] well with the decisions that are often made in the medication management of adults with ADHD.”
Adult ADHD and Healthy Coping Strategies
“There’s a huge difference between treating someone with medication and actually managing a condition,” said Barron. She compared medication for ADHD to drug treatment for diabetes. If you are on medication for diabetes, but then sit at home eating cake and candy, that’s not managing your condition. With ADHD, she said, “medication isn’t the final treatment. . . . You can use it as a foothold . . . but you can’t expect medication to treat everything.” Chronis-Tuscano agreed, and stressed that “it’s really important to learn skills, like any other chronic condition. . . . It’s not just about medication, but it’s also about lifestyle, using skills, CBT organizational [skills], all of those [approaches].” Kofi Obeng, executive director of ADDA, added that “combining [medication] with things like therapy, group work, [and] behavioral modification . . . became force multipliers for me in terms of just having a better life.”
After Barron moved and found a new provider, she was handed a list of rules, including limited rescheduling chances, no prescription refills if she was late to an appointment, and all her prescription refills must be requested within a week before she runs out. Barron asked herself, “Does she understand that I have ADHD?” Barron’s provider told her that as long as she was taking her medication, “this should be pretty easy for [me] to adhere to.” Taking her medication is the bare minimum. “It just gets me here,” she said. “It doesn’t help me find my keys or show up on time.”
Medication can take the edge off, but it does not help a person manage life, finances, sustain healthy relationships, or deal with sexual promiscuity and substance use, said Walker. “We have people who take
ADHD medication and they’re smoking marijuana every day,” she said. “If they don’t have healthy coping strategies, they will use whatever they’ve been using to get by.” Providers need to make a concerted effort to help patients develop these strategies, she said, “and that is an ongoing conversation” that should encompass broader issues of lifestyle and may involve summoning help from others, like a spouse or coach.
“There’s not a single answer here that’s going to be right for everybody,” said Cheyette, further accentuating the need for a broad-based conversation with the patient to determine how best to help that individual. Olfson concurred, noting that medications are tested on groups of people, but there is a lack of information about which medication and at which dose is going to be helpful for whom. “Even at the end of thoughtful and engaged conversations [with patients and providers], there is still an aspect of trial and error involved,” he said, so “having some sort of therapeutic humility” is important.
“I think psychiatry sometimes focuses too much on medication” due to time constraints and insurance reimbursement, said Gold. She cautioned that medications can only do so much and that “there are other things people need to work on at the same time.” Treatment is made even more difficult by comorbidities. “Sometimes medications never work,” she said, referring to a patient who tried “virtually every stimulant . . . and nonstimulant” and never found one that did not worsen their anxiety. Having conversations about nonmedication management is important, she said. She is often able to help patients with referrals to occupational therapy, to learn skills for workplace management. “There are also a lot of apps for that,” she added, and it does not take much time for her to show them to patients.
The U.S. Department of Defense has created “apps that give people access to just-in-time therapy,” which could help supplement the care provided by medical professionals, said Walker. Wearable devices and other technology can also be leveraged for adult ADHD care. However, she added, “the bottom line still comes to resources, and being able to make sure that information gets out, and how practical it is for people.”
ACCESSING RESOURCES
To successfully engage in shared decision making, patients and providers first need access to resources. Walker emphasized the need to standardize resources and help connect people with those resources early in life. “A lot of times that’s not happening, so parents are struggling. And . . . without care, their children grow up to be adults with significant negative trajectories,” said Walker. There need to be systems and processes for delivering these resources “to the people who are touching
the people,” she said: teachers, special education coordinators, and medical providers. Given the high incidence of comorbid conditions such as anxiety, depression, and sleep disorders, and citing her experience working at the intersection of trauma and ADHD, she said, “anybody treating those comorbid conditions should also be aware how the ADHD is undermining that.”
Jonathan Rubin, chief medical officer and senior vice president of research and development at Supernus Pharmaceuticals, emphasized the need for patient education, particularly for adults with ADHD, “who may not completely understand the concept of ADHD as a neuro-developmental disorder that persists throughout the day and evening . . . and potentially throughout their lifetime.” Parents sometimes see ADHD as something that is only an issue during the school year, while adults view it as something that stops after they come home from work. “That framework needs to be reconceptualized, and patients need to be educated about the pervasiveness of ADHD,” he said.
“Trusted messengers are really the key” for reaching individuals, said Patel, and the best messengers are often individuals with lived experience. Patel also emphasized the importance of instilling hope. “If you’re looking for information and getting bombarded with disinformation, individuals who can provide trusted, accurate information that can also instill a feeling of hope are really important,” he said. Following on Patel’s suggestion, Solanto recommended a video made by the World Federation of ADHD that profiles individuals with ADHD (World Federation of ADHD, 2024), which she said would be educational for professionals as well as patients. She also cited the CHADD National Resource Center as a “good, important source of information” that takes “probably thousands of calls a year.” SAMHSA publishes detailed manuals and guidance documents on ADHD, but these need to be turned into shorter documents that the public can use, said Patel.
The FDA could play a public education role by “translating into plain language what treatments are available that are FDA-approved for the management of adult ADHD” and making a concerted effort to educate the public about their importance and explain why medication is important, said Amelia M. Arria, professor in the Department of Behavioral and Community Health and director of the Center on Young Adult Health and Development at the University of Maryland School of Public Health.
LEVERAGING SOCIAL MEDIA TO EDUCATE PATIENTS
Gold primarily treats college students, and ADHD is one of the top three diagnoses that she sees. Many students watch TikTok videos
about ADHD, she said. The TikTok algorithm is designed to offer more videos similar to whatever a person has watched already, so “if you think you have ADHD, you’ll watch 10 more videos that tell you that you probably have ADHD.” This becomes a self-fulfilling prophecy that leads Gold to hearing her patients say, “the internet told me I have ADHD.” This might be correct, she noted. People who have never been diagnosed, including women and people of color, “will feel validated by what they are seeing.” The provider’s job is not to invalidate this experience, said Gold, but to “approach people with kindness [and] provide the information they’re not getting” and offer to talk about it.
Gold shared the results of a cross-sectional study looking at content quality of ADHD videos on TikTok. The analysis of the 100 most popular TikTok videos on ADHD determined that 52 percent were misleading, 27 percent described personal experience, and 21 percent were useful (Yeung et al., 2022), said Gold. The study found that videos made by health care providers were the most useful and least misleading, which could make an argument “for [practitioners] to participate on social media,” she added. Providers can leverage social media to educate patients and put out messaging “that reduces stigma and normalizes challenges with executive function,” said Walker. It can “even [normalize] the concept of neurodiversity and [highlight] the strengths and creativity that come out of a neurodiverse mind.” Some doctors do this very well, agreed Gold, who recommends these doctors’ videos to her patients and encourages others to do so to update patients’ algorithms.







