Adult Attention-Deficit/Hyperactivity Disorder: Diagnosis, Treatment, and Implications for Drug Development: Proceedings of a Workshop (2024)
Chapter: 5 Balancing Risks and Benefits of ADHD Treatment for Adults
5
Balancing Risks and Benefits of ADHD Treatment for Adults
Highlights of Key Points Made by Individual Speakers*
- Stimulants have one of the highest effect sizes (or magnitude of the difference) of all treatments, not just in psychiatry, but in all of medicine. (Goodman)
- Medical treatment for adults living with ADHD confers psychological, social, academic, and occupational benefits while reducing the risk of other negative health and social outcomes, even premature death. (Goodman, Gordon, Mahome)
- All existing medications for ADHD carry significant risks. Medical treatment requires a risk-benefit calculation, that may be different at the individual level than at the population level. (Sokolowska)
- The long-term effects of using prescription stimulants in adulthood are not well understood, and there is little information on the comparative safety and efficacy of ADHD medications. (Sokolowska, Surman)
- Insurance can interfere with ethical prescribing of drugs by requiring prior authorizations for extended-release stimulants and making patients try stimulants before they can receive nonstimulant drugs to treat their ADHD. (Childress, Rubin)
- Medication alone is not enough to treat ADHD. Cognitive behavioral interventions amplify the effects of medication. (Olfson, Solanto)
*This list is the rapporteurs’ summary of points made by the individual speakers identified, and the statements have not been endorsed or verified by the National Academies of Sciences, Engineering, and Medicine. They are not intended to reflect a consensus among workshop participants.
Presentations and discussions on risks and benefits of ADHD treatment focused on what is known and unknown about ADHD medication use in adult populations; barriers (e.g., legal, regulatory, social, cultural) that patients face accessing equitable treatment; the public health implications for potential overprescribing of Schedule II stimulants; and exploring alternative treatment options (e.g., nonpharmacological interventions, retooling of existing medications, new drug development) that may reduce the risk of harm to patients while considering social and cultural factors.
CURRENT PHARMACOLOGIC AND NONPHARMACOLOGIC TREATMENTS
Pharmacologic Treatments
Based on data from 2020 (IQVIA, 2023), 61 percent of all ADHD prescriptions are for adults, said Goodman. Among these, 79 percent are for amphetamines, 13 percent for methylphenidate, and 8 percent for nonstimulants. Importantly, the prevalence of amphetamines is not because they work better in adults. Rather, he said, it is the result of marketing and education clinicians received after Adderall XR was approved as the first adult ADHD medication in 2000 (Heal et al., 2013). Goodman noted that most adult psychiatrists are not trained in child psychiatry or ADHD, and that nearly half of ADHD prescriptions are written by general practitioners or nurse practitioners (IQVIA, 2023), who know far less about the disorder than child psychiatrists or pediatricians. “You move into adulthood, and it is . . . the wild, wild west of psychiatry,” he said.
There are currently more than 30 preparations for stimulant medication on the market, which is “mind-boggling,” said Goodman. These comprise 7 stimulant compounds that can be grouped into 2 broad classes: 3 methylphenidates (racemic MPH, D-MPH, and Ser-dMPH) and 4 amphetamines (racemic amphetamine, mixed amphetamine salts, D-amphetamine, and Lis-D-Amphetamine). These 7 compounds are packaged into a variety of delivery systems, including beads (which may combine immediate-release and extended-release drugs at various ratios), osmotic release, microparticles (liquid, dissolvable tablet, or
chewable), and transdermal patches. The delivery systems vary in terms of onset, duration, and side effects. Among the nonstimulant medications, 2 (atomoxetine and viloxazine ER) are approved for adults, and 2 (guanfacine ER and clonidine ER) are approved for children and adolescents but not adults, although they are frequently used off-label for adults, said Goodman (Iwanami et al., 2020). Nonstimulants may be used alone or in combination with stimulant medications, he added.
A positive response to stimulant medication does not confirm the diagnosis of ADHD, and failure to respond does not negate the diagnosis, said Goodman, noting that about 30 percent of patients do not respond well to the first stimulant and 15 percent do not respond well to the second, but this does not mean that they do not have ADHD (Rapoport et al., 1980; Zametkin and Ernst, 1999).
New Drugs in the Pipeline
Childress mentioned several promising new drugs for adults with ADHD. Centanafadine is a norepinephrine, dopamine, and serotonin reuptake inhibitor that has shown positive results in children, adolescents, and adults (Adler et al., 2022). Solriamfetol, which is being used to treat sleep disorders, had positive results in a double-blind placebo-controlled pilot study for treatment of adult ADHD (Surman et al., 2023). L-threonic acid magnesium salt may enhance synaptic plasticity in mice and has shown promising effects in a pilot study of adults with ADHD (Surman et al., 2021).
Nonpharmacologic Treatments
Some emerging companies are developing nonpharmacological treatments for people with ADHD, said Baker. The FDA recently approved an external trigeminal nerve stimulation device for children with ADHD (NeuroSigma, 2022). There is also an FDA-approved therapeutic video game (Akili Interactive Labs, 2024). Other modalities include ADHD coaching (Kubik, 2010) and CBT (Sprich et al., 2012). Each of these represents an alternative or complementary way to manage ADHD, said Baker.
This meeting underscores the need for nonmedical approaches to ADHD, said a workshop participant. Although the utility of coaching, CBT, and digital therapeutics has been suggested for decades, “you can’t get the same level of treatment in the community . . . because it’s not regulated, it’s not delivered in the same manner,” and it becomes a problem of access, he said.
Treating Adult ADHD with Medication
Before receiving an ADHD diagnosis, Goodman’s patients blame their troubles on faults in their character, intelligence, and motivation. Diagnosis and treatment resurrect self-esteem, function, relationships, and sense of possibility, enabling them to “find a new direction in life, one that you never imagined you could undertake,” he said. Goodman told the story of Maria, a 35-year-old Hispanic woman who came to see him for anxiety and depression. After a comprehensive psychiatric evaluation, Goodman diagnosed Maria with ADHD and treated her with long-acting stimulant medication and psychotherapy. Visiting Goodman three months later, Maria reported that she realized she was not mentally inept like her family had told her for 30 years. Obeng similarly shared that when he was diagnosed “it was a wonderful thing . . . being able to take medication opened up a whole new world.” Treating ADHD “is unlike depression, where we return people back to their typical state. This is returning a person back to a state they never knew was possible,” Goodman said.
Stimulants have one of the highest effect sizes (or magnitude of difference between groups) of all treatments, not just in psychiatry but in all of medicine, said Goodman. Individuals with ADHD experience significantly fewer physical injuries, car crashes, substance use disorders, and criminal acts, and improved academic and cognitive functioning, when they are taking MPH than when they are not taking it. “I’m Maria, and I am not alone,” said Gordon. “There are thousands of us at ADDA who have a very, very similar story.”
Medication Changes Patients’ Lives
“ADHD is much worse than you think,” said Gordon, an adult in his sixties with ADHD. “I spent half my life treated, medicated, and half untreated, unmedicated, undiagnosed. The second half was much better,” he said. Before diagnosis and treatment in his mid-thirties, Gordon said, he totaled four cars and ran someone over. “It’s expensive for me and for society to let us [with ADHD] operate heavy machinery unmedicated.” He misused drugs and alcohol, was in trouble with the law, had career and relationship problems, and struggled with obesity and diabetes. “Think about how stressful my life is unmedicated,” he said. “It’s so much easier medicated.”
Gordon described how the effects of medical treatment for ADHD ripple out. “The self-esteem coming back, the ability . . . to apply yourself to learning the different skills that you need to manage your ADHD, to diet, to get to the gym, to sleep better, to follow up with a specialist if you
need to, all start with that initial diagnosis and the medication and treatment.” Goodman agreed, noting that properly medicated patients have improved symptoms and day-to-day functioning, leading to increases in self-esteem and confidence. “It’s an upward spiral,” he said, that he sees in many of his patients.
Although Gordon’s doctor worries about the potential cardiovascular effects of stimulants, Gordon is more concerned about losing access to his ADHD medication. Cardiovascular issues “can be managed medically. . . . I take a whole row of pills already for all the stuff that I have. [Adding] one more for cardiovascular issues scares me a lot less than going unmedicated with ADHD.” He added that coaching and behavioral therapy are also necessary and that it is “not all about the medication.” Nonetheless, weighing the risks and benefits of treating ADHD, he said, “I really want [the audience] to understand how heavy the side of not treating ADHD is. It’s a huge risk.”
“Treating ADHD definitely can save lives,” said Mahome, noting the higher risk of suicide in individuals with ADHD. Describing her own experience during the stimulant shortage, which included rapid weight gain and resigning from her job, she said that when she is off her medication, she is “not the same person that I am when I’m on it.”
The Two Sides of an ADHD Diagnosis and Treatment
Despite the benefits of treatment, there are arguments both for and against receiving an ADHD diagnosis and treatment, noted Goodman. Appropriate treatment for ADHD can be transformational, conferring psychological, social, academic, and occupational benefits while reducing a person’s risk of negative outcomes such as SUD, tobacco use, car accidents, criminal behavior, unwanted pregnancy, financial debt, multiple jobs, and premature death, along with the societal costs they entail. But diagnosis can also have downsides, he noted, sometimes by making a person ineligible for insurance and for certain occupations. Treatment with ADHD drugs can result in testing positive on a drug screen, and the drugs themselves have a range of possible effects and side effects, including psychosis and cardiovascular changes. Use of prescription stimulants also carries the risk of misuse, abuse, or diversion. Additionally, if the diagnosis is incorrect, it may lead the patient to construct a false psychological narrative, he added.
Another potential downside to treatment for ADHD, noted by Higgins, is that some adults like their ADHD symptoms. Adults with ADHD can experience quicker processing and greater passion and drive, he said, and these traits can be advantageous under certain circumstances. Some patients feel that medicating their ADHD robs them of desirable
personality traits. “We don’t pay enough attention to that,” he said; we might think, “It’s a disease, illness, so therefore we must treat it.” Higgins recommended that clinicians be more flexible with both the diagnosis and options for treatment, which “can go a long way towards engaging more people.”
The cardiovascular changes caused by stimulant medications and atomoxetine are statistically significant but clinically small, said Goodman, and the small changes in blood pressure and pulse rate can be medically managed if the patient has hypertension (Cortese and Fava, 2024; Hennissen et al., 2017). Nonetheless, 5 to 15 percent of patients experience larger cardiovascular effects. “These are things that can be mediated by medical monitoring, balanced against the benefit” of treatment, he said.
Behavioral Therapy as a Part of Treatment
One of the first principles for helping adults with ADHD is multimodal treatment that includes nonpharmacological interventions, such as teaching effective coping skills and self-care strategies, said Olfson. Behavioral interventions are typically given in combination with prescription medicine, which often remains “the cornerstone of treatment,” he noted.
CBT is a powerful intervention that complements medical intervention for ADHD by helping the individual develop new habits, ways of thinking, and consequent behaviors, said Solanto (Liu et al., 2023). CBT aims to give people “effective coping skills [and] to identify and challenge their irrational beliefs around their health conditions,” said Olfson. It can help prevent them from catastrophizing and challenge them to build more adaptive functioning, he added. Combining CBT with stimulants has been shown to improve outcomes for patients with ADHD compared to either treatment alone, as was first demonstrated in randomized controlled trials in 2010 and has since been validated by other research (Solanto et al., 2010). In a randomized controlled trial of adults with ADHD who took stimulants, those who also received CBT were twice as likely to experience a reduction in symptom severity as those who received simple relaxation therapy, and the gains in overall function and symptom reduction were maintained a year later, said Olfson (Safren et al., 2010). New behaviors developed through CBT will be maintained, continue to provide reinforcement, and become autonomous for the individual without requiring continued direct coaching and support, added Solanto. “Medications don’t have this sort of persistence,” said Olfson. “After they stop, the benefits stop.”
While stimulants can enhance attention and impulse control, CBT provides skills and strategies to effectively deploy those functions, said
Solanto. To illustrate the importance of this focus, Solanto cited “pivotal” work showing that the estimated lifespan of young adults who were diagnosed with childhood ADHD is 8.4 years shorter than that of young adults who never had ADHD (Barkley and Fischer, 2019). “Thirty percent of the variance in this outcome was explained by the trait of behavioral inhibition,” said Solanto, “associated with lack of conscientiousness with respect to self-care, sleep, exercise, and proper eating habits.” These habits can influence other outcomes like substance abuse, obesity, type 2 diabetes, smoking, accidents, and even suicide.
Ramsay has been adapting CBT for treating adult ADHD. Medications, he said, are “broadband treatments” that target the core symptoms, which may lead to enough functional improvement to suffice. But since “ADHD is a performance problem,” psychosocial and other nonmedical treatments can address the condition in context, personalizing the treatment to the patient, he added. Solanto has developed and validated a CBT intervention to address executive dysfunction in adults with ADHD that she is currently tailoring for college students. However, although the research shows that CBT can confer enduring benefits, many professionals remain unaware of this, and it can be hard to access therapists who are skilled at delivering this treatment, noted Solanto and Olfson. ADDA members are “huge advocates” of behavioral therapy, said Gordon, noting that until he became educated on how to manage his ADHD, he continued to struggle even after receiving medication. There is an unmet need for behavioral support in addition to drug treatment, he added.
Medication Adherence and Patient Safety and Outcomes
Adherence rates are very low for all ADHD medications, said Baker. In a multinational study on adherence, fewer than 50 percent of adults with ADHD remained on medication a year after they started (Bejerot et al., 2010), said a workshop participant. The two primary reasons patients gave for stopping their medication are that it did not work and that it had negative side effects. Baker questioned the significance of this finding, citing an unpublished drug adherence market research study commissioned by Merck & Co. around 2001 in another therapeutic category in which a third or more of people said they had discontinued the medication because of concerns regarding possible side effects, despite not having experienced them.
“The single most compelling message” to promote adherence, said Baker, is practitioners’ reinforcing to patients that ADHD is a neuro-biological disorder, is well established, and is quite common. But many patients get a different message. “If you have doubts that the condition is real, and . . . other people are telling you it’s not real, it does make you
second-guess,” which can lead to some discontinuing medications despite experiencing symptoms, he said. Many patients tell Solanto that their psychiatrist said to “just take it when you feel like you need it.” She said this is just one example of how many providers are not well-informed about the issue. “When do you not need to pay attention?”
Compared to stimulants, it takes longer for patients to feel the effects of nonstimulants, which many do not have the patience for, said Mahome. Nonstimulants also need to be taken every single day, she said, which itself can be a challenge for individuals with ADHD. Adherence is a problem for all patients, and ADHD’s reduction of executive function makes it all the more challenging, agreed Patel. Schatz has been taking Dexedrine ER since he was a child, and he stays on it because he only needs to visit his provider every six months. “I’ve been tempted to look at some of the longer-duration medication [but] the idea of potentially being referred out to psychiatry . . . and then having to go to monthly appointments . . . is a barrier for me accessing full treatment,” he said.
The words that a physician uses when first communicating the diagnosis to a patient can significantly reduce adherence, said Baker. For example, people are more likely to resist starting a drug if they are told they will have to keep taking it for the rest of their life. But if the physician indicates that the patient will be evaluated on a regular basis to see if the medication is still necessary, the patient may be more willing to accept the drug and stay on it, he said.
Participants with lived experience shared strategies for improving adherence. Joining together with others who have ADHD goes a long way toward encouraging people “to own their ADHD and stick with treatment,” said Obeng. ADDA has multiple support groups where individuals can find supportive communities they can relate to, where “you don’t have to explain your trials and tribulations, people understand automatically . . . being able to find that community and that . . . brings so much empowerment,” said Obeng. ADDA membership more than doubled since the stimulant shortage began, with people seeking resources and a supportive community, he added.
Systematic Barriers to Treatment
Childress said that 84 percent of clinicians who took her survey prescribe short-acting stimulants (Childress, 2023). She continued by saying that insurance “pushes [providers] that way,” despite data showing that long-acting stimulants do not have the same potential for misuse. This is because insurance companies require prior authorization for nonstimulants, she said, which delays treatment. Additionally, prescribers are regularly audited for their notes, which can add hours of extra paper-
work. Roughly half the clinicians in Childress’s survey said that insurance pushed them to prescribe generic short-acting stimulants and refused to cover nonstimulants. Unlike pediatricians, many of whom have switched to using extended-release stimulants, adult prescribers predominantly use immediate-release stimulants. Rubin said these may not be appropriate in all cases, particularly in light of Childress’s finding that most adults on stimulant medicine for ADHD were not completely satisfied with their treatment.
Patients’ insurance and the medications it covers often determine what the prescriber will give, said Mahome. This is because many do not have time to do prior authorizations. For “no other condition . . . not schizophrenia, not bipolar, do I need to validate the diagnosis and go through a set of 15 questions. It’s more restrictive, and that is stigma,” said Schatz.
It is unethical to require patients step through a product that is less efficacious or more harmful than the intended product, said Rubin, but this is what happens when managed care dictates treatment decisions to clinicians and “gets in the way of the patient–physician relationship to . . . determine what is in the patient’s best interest.” Rubin recounted a recent call from a young adult patient who was forced to switch from Supernus’s nonstimulant drug, Qelbree, which he had been using successfully, to a stimulant, despite concerns about side effects. In certain circumstances, the insurer will not approve Qelbree until the patient first steps through other drugs that are not even approved for adult ADHD. “That doesn’t make sense,” he said.
Insurance can also determine what type of provider a patient sees, noted Robinson, citing a preliminary comparison of patients on employer-sponsored insurance with patients on Medicaid using 2021 data obtained from the Merative MarketScan database.1 Robinson analyzed the types of providers seen by individuals who had seen only one outpatient provider type for ADHD in 2021. Among adults with employer-sponsored insurance, 50.4 percent saw a primary care physician, 12.4 percent saw a nurse practitioner, and 29.6 percent saw a psychiatrist, psychologist, or psychiatric nurse for ADHD, “providers who most likely have specialty training in mental health,” she said. In contrast 42.5 percent of Medicaid patients saw a nurse practitioner for ADHD care, 20.9 percent saw a primary care physician, and only 16.9 percent saw a mental health specialist. Robinson noted significant state-level differences in the provider types seen by those with employer-sponsored insurance. Importantly, for both types of insurance, more than half of adult patients received some or all of their ADHD care by telehealth.
___________________
1 Available at https://www.merative.com/documents/brief/marketscan-explainer-general (accessed April 30, 2024).
BALANCING RISKS AND BENEFITS OF USING ADHD MEDICATIONS
All existing medications for ADHD, both stimulant and nonstimulant, carry significant risks, noted Sokolowska. “The central theme here is risk-benefit assessment,” said Winterstein. Risk-benefit assessments may be different at the population level than at the individual level, and the individual risks associated with a drug could render it favorable for some individuals but not others. Balancing these individual risks with population risks can be difficult when making regulatory decisions, said Winterstein. Risk-benefit assessments need to consider lack of response to treatment, minor symptoms that could be managed with nondrug interventions, or a predisposition that increases the risk of a particularly bad adverse effect. Furthermore, the assessment of risk-benefit or personal preferences when considering alleviated symptoms compared to adverse effects is critical.
Overall, said Childress, medications for ADHD lead to improvement in a variety of symptoms in adults, including driving, injuries, depression, suicidality, criminality, and SUD (Chang et al., 2019). ADHD drugs worsen bipolar disorder because stimulants can make people manic, so the bipolar needs to be treated first, said Childress. However, psychosis and seizure disorders do not appear to worsen.
Winterstein spoke about the two major safety risks associated with stimulant use for ADHD: risk of developing SUD and cardiovascular risk. On the risk of SUD, she said, more research is needed to separate the effects of ADHD itself from the effects of stimulants, as well as the relative impact of variables like stimulant type, dosage, form, duration of use, and patient-specific factors. Winterstein and colleagues found that “concomitant long-term stimulant and prescription opioid use is quite common, and opioid use is more common among ADHD patients who use stimulants than those who don’t,” raising “important hypotheses” that need addressing (Wei et al., 2018). Still, she noted, “it remains difficult to identify those patients whose ADHD treatment might result in [SUD].”
Regarding the cardiovascular risk, stimulants affect heart rate and blood pressure as a result of both dopaminergic and adrenergic effects, said Winterstein. In the worst case, this could lead to ventricular arrythmia and sudden cardiac death. Winterstein and colleagues were able to rule out this risk in children (Winterstein et al., 2012). “There may still be subtle effects, but . . . this would result in a huge number needed to harm,” she said. However, a recent study that evaluated the effects of long-term stimulant use in both children and adults from a large Swedish population found a 50 to 70 percent increased risk of hypertension and arterial disease, though there was no association with arrythmias, heart failure, or cerebro--
vascular disease (Zhang et al., 2024). “This is not minor,” said Winterstein, noting that “blood pressure targets keep being lowered, as measures that used to be considered normal are now linked to heart disease.” She also noted that about 10 percent of adults taking stimulants had preexisting heart disease (Gerhard et al., 2010), “and we know very little about the risk of stimulant use in those populations.” Unlike previous studies that failed to detect this cardiovascular risk, the Swedish study followed a very large, higher-risk population over multiple years, with a median of four years. Winterstein’s study, which followed a million children for an average of two years, failed to detect any effect because the risk for cardiovascular disease in children is so low to begin with (Winterstein et al., 2012).
Providers need more data to make patient-centered treatment decisions, “that’s very clear,” said Winterstein, emphasizing the need to compare multiple options, including nondrug treatments and combinations. Given the risks associated with stimulant use, she said, “we need to think about tapering approaches” as well as alternatives for patients with cardiometabolic risk factors or patients who develop hypertension. Patients themselves need to decide “what their preference is, regarding an increased risk for stroke or myocardial infarction versus uncontrolled ADHD.” Making these difficult treatment decisions will require “more subtle and really very specific comparative studies that allow patients, providers, and regulatory agencies to make informed decisions,” she concluded.
“When we evaluate the risk-benefit ratio of treatment for ADHD, I’d say we’ve had an experiment this past year,” said Greg Mattingly, president of APSARD and co-chair of U.S. Psych Congress, referring to the struggles of ADHD patients due to the stimulant shortage. At the U.S. Psych Congress (HMP Global, n.d.), he said, “it’s the number one public mental health issue we hear about. Not depression, not schizophrenia, not anything else. It’s not having access to appropriate ADHD care.”
Long-Term Effects and Efficacy of ADHD Medications
The long-term impact of using prescription stimulants in adulthood is not well understood. Sokolowska noted that assessments of ADHD treatments are typically based on studies that last less than 12 weeks. The efficacy of Adderall, a mixed amphetamine salt, was not systematically evaluated for long-term use in clinical trials before its approval, and the efficacy of Adderall XR, an extended-release mixed amphetamine salt, was established separately for children, adolescents, and adults in studies lasting only three to four weeks (Cortese et al., 2018). Sokolowska emphasized the need for more long-term studies on both safety and effectiveness of the various treatment options, including their impacts on behavior,
cardiovascular effects, and the risk of progression to nonmedical use or SUD. The FDA published new guidance for clinical trials of stimulant medications in 2019 (FDA, 2019), recommending randomized, double-blind, placebo-controlled trials and at least one fixed-dose trial, without dose optimization before randomization, to get a better readout of safety, she said.
Studies rarely involve head-to-head comparison of drugs that would enable providers and patients to make informed choices based on comparative effectiveness and safety of the treatments, said Surman. He also noted the importance of placebo controls and postmarket surveillance. Additional knowledge gaps exist regarding the impact of telemedicine and best approaches to improve access to treatment, added Sokolowska.
Medication Management of Adults with ADHD
Overprescription and Nonmedical Use of Prescription Stimulants
Although two nonstimulants have been approved by the FDA for use in adults with ADHD and additional nonstimulants approved for use in children are sometimes used in adults, “the overwhelming majority” of adults with ADHD who are treated with medication receive amphetamine-based or methylphenidate-based stimulants as first-line treatments (Soreff, 2022), said Olfson. These are Drug Enforcement Administration (DEA) Schedule II drugs with a high potential for abuse and a black box warning about prescribing them to individuals with a history of SUD, but they remain the first choice for treatment because “there’s stronger evidence for more robust efficacy,” he said. Olfson illustrated this with data from two randomized double-blind studies (Nasser et al., 2022; Spencer et al., 2005) that compared either MPH or the nonstimulant viloxazine to placebo (Figure 5-1). Over six weeks, the group receiving MPH showed greater symptom reduction than the group receiving viloxazine.
The prescription of stimulants to adults has increased over the past decade, particularly to individuals in the 31–40 age range, said Olfson (Figure 5-2). The number of prescriptions to people in this age range rose from fewer than 6 million in 2012 to nearly 16 million in 2021 (IQVIA, 2023). Olfson questions if this was because that age group had been undertreated “and we’re playing catch-up,” or if it was because of misuse.
A study from southern France (Pauly et al., 2018) found that adults ages 25–49 were prescribed “dramatically higher” doses of MPH than younger adults or adolescents, said Olfson. These older adults saw, on average, four different prescribers and four different pharmacists; 60 percent were also prescribed benzodiazepines; another 14 percent non-benzodiazepine anxiolytics; and 39 percent were filling opioid prescriptions. Thirty percent
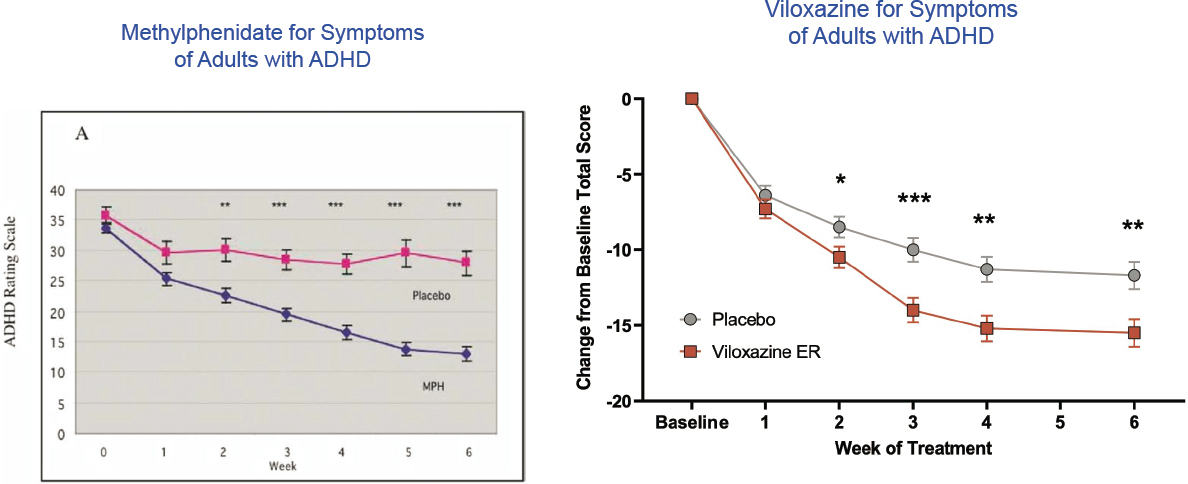
NOTE: * indicate significant levels. On the left, * = p< 0.01; ** = p< 0.001; *** = p< 0.0001. On the right, * = p< 0.05; ** = p< 0.01; *** = p< 0.001.
SOURCES: As presented by Mark Olfson on December 13, 2023; Spencer et al., 2005. Copyright with permission from Elsevier; Nasser et al., 2022, CC BY 4.0.
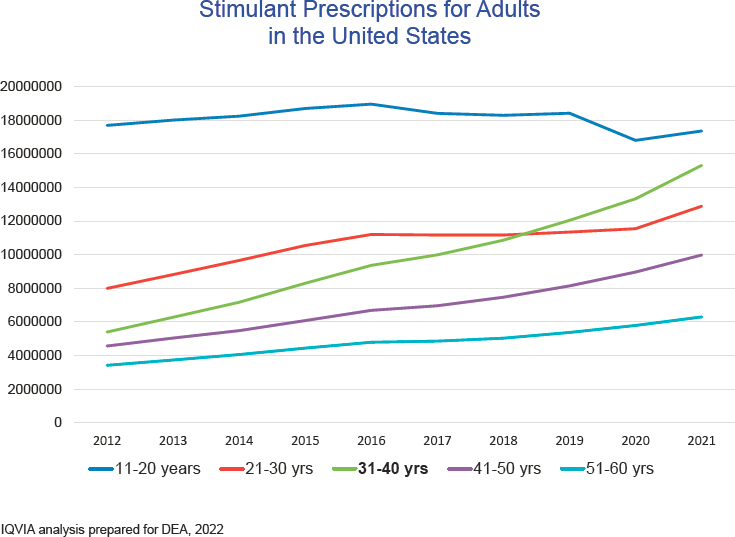
SOURCES: As presented by Mark Olfson on December 13, 2023; figure created based on data provided in IQVIA, 2023.
of these individuals were filling prescriptions for methadone or buprenorphine, “suggesting that they have opioid use disorder,” he said. A Danish study (Rasmussen et al., 2015) obtained similar results when it identified groups of patients who were being prescribed methylphenidate at doses “three times higher than what they call the defined daily dose. . . . I call it suspicious methylphenidate prescribing,” said Olfson. The risk of being in this group was much higher for individuals in the 25–49 age bracket than for older or younger adults. Additional predictors for being in the high-dose-stimulant group included getting the prescription from a general practitioner or hospital doctor rather than a specialist, being prescribed benzodiazepines or opioids, and being prescribed medications for addictive disorders, such as buprenorphine. “Again, it’s a concerning pattern that we see in opioid prescribing in this group,” said Olfson.
Olfson emphasized the distinctions between abuse (using medication to get high), misuse (using medication in a way that is not prescribed), and nonindicated use (using it for purposes other than treatment of ADHD). One possible explanation for some of the increased volume of stimulant
prescriptions, he said, is diversion: selling or giving away drugs outside legal channels.
One nonindicated use of concern, said Olfson, is when college students take stimulants as a study aid, or adults working in intellectually demanding professions take them as neuroenhancers. Studies of healthy volunteers offer some evidence that a single dose of methylphenidate can improve working memory, processing speed, verbal and learning memory, and (to a lesser degree) attention (Linssen et al., 2014). However, there is “very little evidence that these medications actually help with problem solving or reasoning . . . and no evidence that they help with visual learning and memory,” suggesting that they might not offer the benefits students are after, he said. Nonetheless, he noted, “in some dimensions . . . these effects could be viewed and experienced as beneficial.”
Increase in ADHD Prescriptions
The number of ADHD prescriptions in the United States increased from 50 million in 2012 to 80 million in 2022, according to DEA data presented by Sokolowska (IQVIA, 2023). In 2022, 90 percent of prescriptions were for stimulants and 10 percent for nonstimulants. Stimulant prescriptions increased over that decade by 58 percent, and nonstimulant prescriptions by 70 percent. This increase was driven by prescriptions to adults, predominantly females, in the 31–50 age range. The absence of adult ADHD clinical practice guidelines, coupled with the rise in both telemedicine and social media advertising of ADHD treatments during this decade, has raised concerns that some of this increase may reflect inappropriate prescribing, said Sokolowska. The COVID-19 pandemic may have also contributed to this increase, she noted.
Perhaps surprisingly, given the rise in U.S. stimulant prescriptions, studies have turned up no evidence of a corresponding increase in misuse, noted Sokolowska and Olfson (SAMHSA, 2023). According to the annual National Survey of Drug Use and Health conducted by SAMHSA, the proportion of people ages 18–25 in the general U.S. population who reported misusing stimulants actually decreased from 2015 to 2022. This level was lower for individuals aged 26 and up, with only 1 percent of that population reporting the misuse of stimulants. Nonetheless, in 2022, 4.3 million people in the United States aged 12 or older reported misusing prescription stimulants in the past year, and 1.3 million of those reported misusing prescription stimulants together with other stimulants, such as cocaine or methamphetamine. Looking more narrowly at SUDs, the national prevalence of prescription stimulant use disorder is about 1.5 percent of people ages 18–25 and 0.5 percent of those age 26 and up. “It’s not a large number, but it’s not trivial either,” said Olfson, noting
that in adults it’s a fraction of the prevalence of prescription opioid use disorder.
“We still need to learn a lot more regarding the impact of nonmedical use of stimulants in adulthood,” said Sokolowska, noting that plenty of data exist regarding the consequences of nonmedical use in adolescents but little in adults. A recent study (McCabe et al., 2022) found that the pattern of nonmedical stimulant use among individuals ages 18–50 follows one of six trajectories over time, with peaks occurring around age 18, 19/20, 25/26, 40, 45, and 50 (Figure 5-3). All misuse trajectories showed increased odds of developing SUD symptoms in middle adulthood. Based on their data, the study authors recommended screening for prescription stimulant misuse and SUD in adolescence and adulthood, said Sokolowska.
FDA is acting to curb stimulant overprescription and nonmedical use while at the same time trying to address the drug shortage, said Sokolowska, noting that label warnings have been updated to emphasize the serious risks related to drug misuse, abuse, addiction, and sharing. FDA and DEA are working in tandem to combat counterfeit prescription stimulants and to crack down on online pharmacies that sell Adderall illegally and pharmaceutical companies that do not identify the risks of taking stimulant medications in their advertisements, she said. FDA is also funding research to better understand the nonmedical use of prescription stimulants, she added.
Robinson presented information from a 2023 CDC Morbidity and Mortality Weekly Report on prescription stimulant fills using Merative MarketScan employer-sponsored insurance claims (Danielson et al., 2023), which was based on insurance claims data. The report showed a “sharp increase” in the percentage of adults receiving prescription stimulant medications during the first year of the COVID-19 pandemic (2020–2021). While there was an overall increase in the number of people receiving stimulant medication, from 3.8 percent to 4.1 percent of all individuals ages five to 64, the increase was particularly notable (i.e., more than a 10 percent increase) among adolescent and adult females as well as among adult males. It rose 17 percent and 12 percent, respectively, for women and men in the 25–29 age group. This kind of increase had not been seen prior to the pandemic, she added.
DIVERSION AND MISUSE OF ADHD MEDICATION
The treatment of adult ADHD creates several dialectics that need to be carefully thought through, said Patel. There is a tension between the need to prescribe stimulants where appropriate and the risk of diversion; between use of detailed, thorough screening tools that patients are unlikely
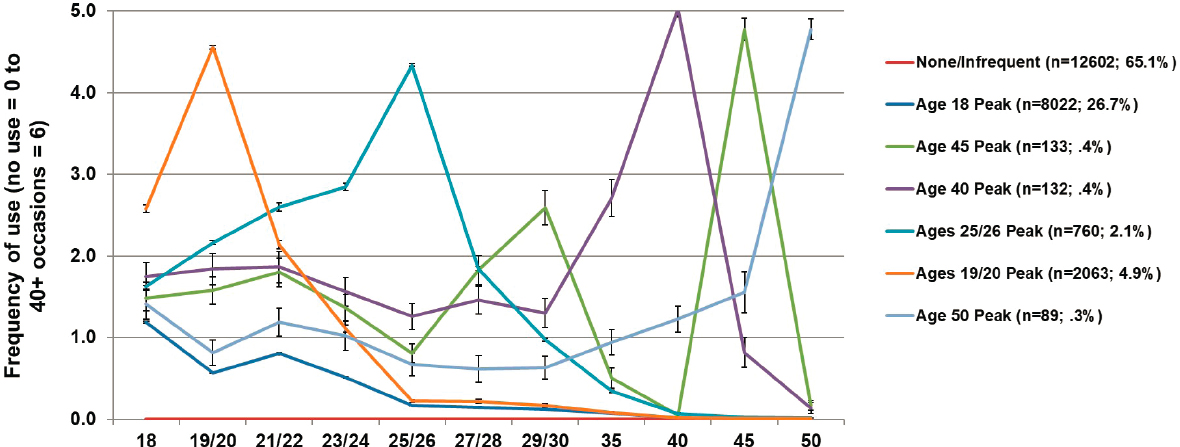
SOURCES: As presented by Marta Sokolowska on December 12, 2023; McCabe et al., 2022, CC BY.
to complete in full or return and those that are more succinct but might not provide a full picture; between underdiagnosis and overdiagnosis, which vary based on population and setting; and between treating ADHD to prevent the emergence of comorbid SUD and the potential increase in SUD risk with treatment. Trends related to telehealth and online platforms for prescribing stimulants raise additional concerns. However, ADHD has serious adverse consequences, ranging from impaired academic performance to an increased risk of SUD, criminality, and death, as noted by Childress and many others. Therefore, Patel said, “individuals with adult ADHD need help, and these trends . . . should not preclude appropriate and adequate treatment.”
Carlos Blanco, director of the Division of Epidemiology, Services, and Prevention Research at the National Institute on Drug Abuse, noted that this dilemma involves a risk-benefit calculation that requires balancing the individual’s benefit of taking a stimulant against the community cost of its misuse or diversion. “How do we provide regulations and incentives so we achieve, if not optimal, at least second-best solutions?” he asked. This requires understanding how stimulants are actually misused and diverted.
Prescription Stimulant Misuse:
Health Risks and Association with Later SUD
The risks associated with nonmedical use, also called misuse, of prescription stimulants vary with the route of administration, said Goodman (Faraone et al., 2024). The nasal route is associated with a higher risk of medical admission, oral with an increased risk of suicide attempts, and intravenous injection with a more than 20-fold increased risk of death; these data do not account for cofactors (such as comorbid psychological disorders) and therefore do not demonstrate causality, he noted.
The literature does not provide a clear link between early prescription stimulant use and later SUD, said Goodman (Chang et al., 2019). Animal studies demonstrated that exposure to stimulants during adolescence was associated with long-term risk of substance abuse (Kantak and Dwoskin, 2016), but more recent clinical studies found that ADHD medication neither raises nor lowers the risk of later SUD (Humphreys et al., 2013; Molina et al., 2013). Pharmacoepidemiologic studies drawn from a prescription database found that “ADHD medication was associated with a lower risk of substance-related events over three years” (Chang et al., 2014; Quinn et al., 2017), he said. Goodman suggested that the discrepancies might reflect differences in how these three very different types of studies were conducted.
Stimulant Misuse
Misuse of prescription stimulants is a serious concern. Among the general population, roughly 10 percent of individuals misuse prescription stimulants over the course of their lifetime, said Goodman, and this should be considered the background rate when studying misuse in patients with ADHD. Data consistently show that extended-release preparations of stimulants have a lower abuse liability than short-acting preparations, and nonstimulants have no potential for misuse (Findling, 2008). Nonetheless, Goodman advised against eliminating short-acting stimulants altogether, which would decrease the flexibility of clinicians and patients to manage ADHD symptoms.
“It’s also important to know that many people who misuse stimulants do it infrequently,” said Brooke Molina, professor of psychiatry, psychology, pediatrics, and clinical and translational science at the University of Pittsburgh. She noted that in the College Prescription Drug Study, 84 percent of the college students who reported misusing stimulants at some time in their life said they had used them zero to nine times in the past year (Kilmer et al., 2021; Phillips, 2018). Most students who misused stimulants were doing it not on a daily basis but during stressful times, such as during midterms and final exams, she said. Misuse is more common in schools that have more stimulant prescriptions, more white students, higher parent education, and more reported substance use. Misuse is also more common among males, white students, and students with ADHD symptoms, lower grades, substance use, or (among young adults) membership in fraternities or sororities; it peaks in the 18-to-25-year age range, added Molina.
Stimulant use among children with ADHD drops precipitously as they age, said Molina, citing her longitudinal study (Molina et al., 2023) that followed stimulant treatment and substance use in children from the Multimodal Treatment of ADHD study (MTA) for 16 years (a 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal treatment study of children with ADHD, 1999). At the study’s outset, the children had a mean age of 10.5 years, with 57 percent taking stimulants for ADHD. The percentage of children on stimulants dropped to 7.4 percent when the study group reached a mean age of 25 (Figure 5-4). This drop is commonly seen in longitudinal studies and suggests that children who are prescribed stimulants will not become addicted to them, said Molina.
As stimulant use among the MTA population declined over time, use of other substances like cigarettes, marijuana, and alcohol tended to rise. Molina found that children with ADHD had an elevated risk for harmful use of other substances, which is “a typical pattern,” but this risk was not
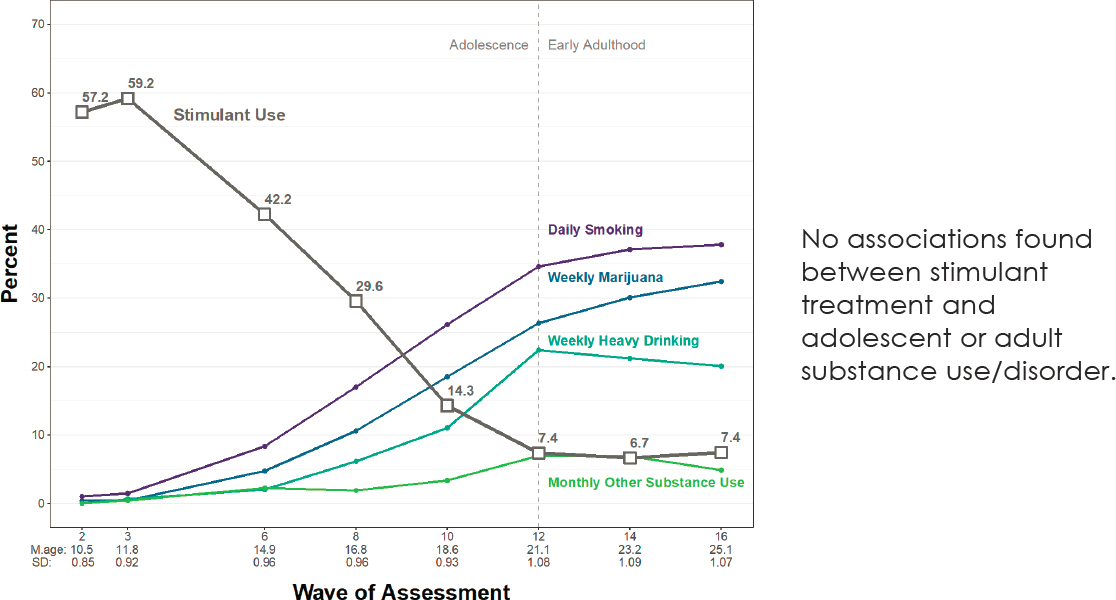
NOTE: M.age = mean age; SD = standard deviation.
SOURCES: As presented by Brooke Molina on December 13, 2023; Molina et al., 2023. Reproduced with permission from JAMA Psychiatry. Copyright © American Medical Association. All rights reserved, including those for text and data mining, AI training, and similar technologies.
associated with stimulant use in childhood, “which was a great find,” she said.
Higgins indicated that many of his patients who attend college report smoking marijuana on a regular basis, behavior patterns supported by the literature (Jean et al., 2022; Rooney et al., 2011). Students stop taking their ADHD medicine and turn to marijuana because they hear that it enhances dopamine. “But the fact is that you blow right past your dopamine levels to inattentiveness because you are dopamine depleted,” he said. Higgins now asks patients whether they smoke marijuana, and how much, as part of his diagnosis.
Diversion and Misuse of Stimulants by Students
Misuse of stimulants is common among students, said Molina. In the 2018 College Prescription Drug Study (Faraone et al., 2020; Phillips, 2018), which surveyed 19,000 college students, 15.9 percent reported stimulant misuse at some point in the past, and 10 percent reported misuse in the last year. The Monitoring the Future Study (McCabe et al., 2023; Teter et al., 2020) sampled 230,000 secondary school students across the United States between 2005 and 2020 and found that 3.6 percent of 8th graders, 6.5 percent of 10th graders, and 7.2 percent of 12th graders reported misusing stimulants in the past year. This increase in misuse with age is “relevant . . . particularly with respect to prevention,” said Molina. Nonprescribed use of stimulants varies widely across schools, ranging from 0 to more than 25 percent of students, “so one school is not the same as the next,” she added.
The most common reason why individuals misuse stimulant medications is to improve academic performance, said Molina. Students take them to stay “awake longer, to pay attention, to have their arousal level increased, thinking that they’re smarter,” she said. However, research does not bear out this effect. In a study where adults with ADHD were asked to perform a complicated cognitive task with and without stimulants (Bowman et al., 2023), the level of effort increased but quality decreased when stimulants were used, said Molina, “so it’s not a smart pill. . . . People often think that it does more than it really does.”
In a longitudinal study of 1,253 college students, Amelia Arria and colleagues found that most nonmedical prescription stimulant use was associated with binge drinking and cannabis use, and these last two were strongly associated with academic disengagement (Arria et al., 2008). Students were using nonmedical prescription stimulants “as a shortcut or a compensatory mechanism” to address the academic fallout from drinking and smoking marijuana, said Arria.
College students constitute the highest-risk group for nonmedical use of stimulants, said Antshel. Citing nine separate surveys of college
students (Advokat et al., 2008; Arria et al., 2008; Cassidy et al., 2015; DeSantis et al., 2010; Faraone et al., 2020; Novak et al., 2007; Rabiner et al., 2009; Verdi et al., 2016), Antshel said the primary motivation for misuse is that students view stimulants as an “academic steroid not as a drug, in contrast to “party drugs” like heroin or other opioids (DeSantis and Hane, 2010). Students also justify the nonmedical use of stimulants by saying they use them strategically and only during periods of high stress; or by minimizing the harm, comparing stimulants to coffee and energy drinks. The strategic nature of stimulant use in colleges was illustrated in a 2013 study, said Antshel, which found a jump in mixed amphetamine salts in campus wastewater in April and December, during exams (Burgard et al., 2013).
Citing another publication of Arria’s that tracked stimulant misuse among college students over a two-year period (Arria et al., 2017), Antshel noted that students’ grade point averages did not rise during the periods when they misused or fall when they stopped misusing, “suggest[ing] it’s not the academic steroid that the average college student believes.”
Diversion and Misuse of Stimulants by Adults
Not all diversion is done by college students, noted El-Sabawi. Diversion and misuse look different “for the adult population, the minoritized populations, disproportionately impacted populations.” Indeed, longstanding work shows that there are moral economies of drug use, said Ryan McNeil, associate professor and director of harm reduction research at Yale School of Medicine, which are structured around sharing resources and supporting one another. Diversion of stimulants is often the result of sharing among friends, he said, “to support gaps in prescribing, lapses in medication . . . meeting gaps in broader systems . . . where we’ve let people down. . . . This doesn’t happen in a vacuum.” Furthermore, when diversion is considered against the background of a volatile drug supply that includes pressed pills, which may contain fentanyl or other adulterants that can amplify the risk of overdose, diversion can be protective, he added. Molina concurred, noting that most individuals who divert are not building up a supply with the intent of getting rich. “By and large [they] end up being approached, and it’s hard to say no.” Molina has worked with practitioners “to help patients anticipate those moments and have . . . a script” to explain why they cannot share their pills.
Terms like “diversion” and “misuse” suggest that drugs are not being used for medical reasons, said McNeil, but this may be a mistaken assumption about many of the adults who take stimulants without a prescription. He noted that “a lot of folks are using nonprescribed opioids for pain,” and “extending that logic, it’s reasonable to expect that similar
dynamics are occurring here,” with barriers to care or a lapse in care driving people to nonprescription use of stimulants.
Public health approaches to substance are “demand-side,” said El-Sabawi. In contrast, the emphasis on diversion takes a “supply-side approach, which is typically focused on by law enforcement.” Framing the problem as diversion, with enforcement as the solution, disproportionately impacts “people of color, people who are poor, people who are systematically targeted by carceral systems,” said McNeil. “If we hope to avoid that, we need to reflect on what we’re . . . constructing as the actual problem here.” McNeil noted that engagement with the carceral system is an “incredible driver of harm at the individual level, at the community level, and society at large.” Approaching the issue through an equity lens, he said, “we need to foreground that [harm] in the discussion so as to not perpetuate these systems that are so devastating to people and communities.” Supporting this, Rubin offered that one option to address issues of misuse, diversion, and abuse of stimulants is to consider the prescription of nonstimulants as a first step when appropriate.
“People who are prescribed controlled substances will tell you that stashing is very important because pharmacies run out, you move, you can’t find a doctor, you might be on a waitlist . . . or there’s a restriction like you only have two days to fill your prescription,” said El-Sabawi. Molina cautioned that doctors should not be “so tight on prescribing that [patients] don’t have enough to carry [them] over from time to time,” particularly in light of the difficulty that adults with ADHD have maintaining their prescriptions and getting to the doctor for refills on a regular basis. The goal of Molina’s harm reduction approach (described in Chapter 7) is for providers to be aware if a patient has a lot of unused medication at home and to adjust the prescription if necessary, but not to prevent patients from having any buffer, she noted.
A public health approach should ask why people are using and stockpiling their drugs, said El-Sabawi. She noted that people of color may be less likely to see a psychiatrist, more likely to blame themselves for their disorder, and less likely to be diagnosed with ADHD, “and so we have over-representation . . . in the population using illicit stimulants who are people of color.”
This page intentionally left blank.























