Innovations in Pharmacy Training and Sustainable Practice to Advance Patient Care: Proceedings of a Workshop (2025)
Chapter: 4 Financial Sustainability
4
Financial Sustainability
KEY POINTS*
- Get pharmacists to talk with physicians, patients, and payers to explain and demonstrate the value and role of pharmacists in the system. (Kliethermes)
- Identify efficiencies of pharmacy practice that justify the call for reimbursement, and develop a business model in which practice and reimbursement are commensurate. (Brummel)
- Look at how pharmacy can respond to the needs of today and tomorrow; much change has occurred over the past 30 years, and the time to act is now. (Hanson)
- With shifts in policy, pharmacists would be able to realize their full potential for positively impacting patient care. (McDonough)
- Getting pharmacists recognized as providers by Medicare is an important step in getting adequate reimbursement for their services. (Kraus)
- Pharmacists are essential components of team-based care, but the current fee-for-service payment models are not sustainable for this type of care. (Rodgers)
__________________
*These points were made by the individual workshop speakers/participants identified above. They are not intended to reflect a consensus among workshop participants.
As other speakers discussed, said Mary Ann Kliethermes, American Society of Health-System Pharmacists (ASHP), financial sustainability is critical for pharmacies and their pharmacists. Otherwise, pharmacies close, pharmacists and other providers are overworked and burned out, and patients don’t get the care they need. To have a financially sustainable system, she said, change is desired in three areas: laws and regulations, payments, and standardization in services. For the first, pharmacists would have to be designated as a legal health care provider; this has improved dramatically over the last few decades, said Kliethermes, but room for improvement remains. In addition, state scope of practice laws vary considerably. This makes it challenging for national payers to make consistent decisions about which services are covered. Finally, pharmacists would have to be included in state insurance codes, which outline what services must be provided and who must be paid for them; only some states have made changes to make it clear that if a pharmacist, working within their scope of practice, provides a state-approved benefit, they must be paid for the service.
Getting reimbursed for patient care services is complex, said Kliethermes. Medicare, Medicaid, and commercial payers all have different structures and procedures; Medicare has the biggest impact on payment, as other systems often rely on its decision making. Despite codes in Medicare for pharmacists for patient care, the payments are often inadequate to cover the service and cost of doing business, and reimbursements vary depending on the work setting. A lot of rules and regulations make Medicare reimbursement difficult, Kliethermes noted, and it is challenging to get national-level data about what is actually happening on the ground. Within the Medicaid system, 84 percent of states have designated pharmacists as providers. However, 30 percent of them restrict pharmacists to specified services. Commercial payers complicate the picture further, said Kliethermes. About 25 percent of states have commercial coverage for any service within scope of practice, and 12 percent only cover specified services.
The lack of standardization makes payment for pharmacist-provided services challenging. Billing codes generally cover specific procedures or processes; at a new patient exam, for example, a physician can get paid for taking a history, doing a physical exam, and making decisions. Pharmacists would greatly benefit from a similar standardized process for patient care services, said Kliethermes, that could demonstrate value and receive adequate payment.
FINANCIALLY SUPPORTED ROLES FOR PHARMACISTS
Speakers and participants explored and evaluated model programs where pharmacists are—or could be—financially supported in expanded
roles. Chisholm-Burns moderated the session; each speaker shared details about the models used at their own organizations.
Fairview Pharmacy Service
The Fairview Health System is based in the Minneapolis/St. Paul area, said Amanda Brummel, Fairview Pharmacy Service. It employs over 34,000 staff and operates 12 hospitals, offering comprehensive services, including retail, specialty, infusion, and compounding. The comprehensive medication management (CMM) program has been in place for nearly 30 years, with 70 pharmacists in 65 locations. It involves assessing a patient’s medication therapy, identifying any medication-related problems, developing a care plan, evaluating outcomes, and continuously following up. In 2024, these pharmacists saw over 25,000 patients and had over 57,000 patient encounters. While the program began in 1998, said Brummel, Medicaid and Medicare did not begin paying for the services until 2006. Minnesota Medicaid began covering services in 2006, which set the foundation for the payment model, said Brummel. After securing Medicaid and Medicare coverage, Fairview explored other avenues, including employer benefits, accountable care models, and direct service through Medicare Part D. Brummel noted the fewer barriers to payment when pharmacists are embedded into the health system as part of a team providing consistent service.
In the CMM practice model, each clinic site has its own schedule, and each pharmacist cares for 600–700 patients. They provide both in-person and telemedicine appointments and manage over 20 conditions. Patients are referred by their providers, health plans, or automated criteria that identify at-risk patients or specialty medications. Services are supported through fee-for-service billing (CPT1 codes 99605, 99606, 99607), per member per month (PMPM)/Care Management Payments,2 value-based contracting3/quality metric payments, and prescription margins. Brummel noted that CMM has a business office that focuses on coding and claims submission, which ensures that people who understand the system submit the proper claims for proper reimbursement. The financial stability of the CMM program is in large part due to the robust evidence supporting its effectiveness, said Brummel. Studies have found significant clinical, economic, and humanistic impacts, including reduced readmissions, improved medication
___________________
1 Current Procedural Terminology procedural terminology codes are used to pay health care professionals for services.
2 This is the per member per month cost calculated by health care insurance payers.
3 Value-based contracting ties payment to quality rather than volume of services (Bailey, 2021).
adherence, reduction in annual health expenditures, and high satisfaction from patients and providers (Tripicchio et al., 2020).
Looking to the future of the CMM program, Brummel identified three requirements. The first is to continue maintaining payment sustainability by ensuring that payment rates keep up with costs, increasing opportunities for pharmacists to be reimbursed for services, and advocating for changes to legislation to recognize pharmacists as care providers. Second is to improve productivity and efficiency by ensuring that pharmacists have full schedules and maximize their time with patients. Brummel noted, however, that this must be done in a way that ensures adherence to the original practice model, as it is responsible for the positive impacts of the program. The third requirement, she said, would be to optimize the population of patients who are seen. Because the CMM program cannot serve every patient, Brummel felt it is essential to prioritize those who need financial assistance the most.
Geisinger
Geisinger is one of the largest integrated health system in Pennsylvania, said Adriene Zook, its pharmacy manager, with over 550,000 health plan members across 46 counties in Pennsylvania. Pharmacy services are integrated across the system rather than siloed, she said, ranging from antimicrobial stewardship to mail order pharmacy to investigational drug services. The Medication Therapy Disease Management (MTDM) program started in 1996, with a telephone-based program for patients on anticoagulation drugs (Jones et al., 2017). Other condition-specific programs were added over the years, including chronic disease management, and recent additions have been specialized programs for “high-touch, high-dollar” medications. The ambulatory MTDM program has three subsections, said Zook: primary care, specialty care, and nontraditional. Primary care pharmacists provide comprehensive, high-value, high-touch, longitudinal disease management for conditions such as chronic pain, diabetes, and hypertension. Specialty care pharmacists provide high-value, low–moderate-touch, highly specialized interventions for services such as rheumatology, neurology, and pulmonology. Nontraditional MTDM is focused on a comprehensive, high-value, high-touch hybrid of specialized interventions and disease management aimed at the geriatric population. These pharmacists work with patients on issues including osteoporosis, smoking cessation, and behavioral health.
The Geisinger model of pharmacy care has driven clinical, operational, and financial value, said Zook. Clinical outcomes include reduction in mortality for diabetic patients, reduction in dangerous combination of opioids, and increases in drug coverage for Medicare patients. Operationally, MTDM has resulted in fewer acute care visits for diabetic patients and an
improved Centers for Medicare & Medicaid Services (CMS) rating. Financial outcomes include reduced insulin costs and PMPM costs for diabetic patients. Zook identified key priorities for future growth of the pharmacy program:
- Define, track, and report out clinical, operational, and financial impacts.
- Optimize revenue generating opportunities without losing focus on patient outcomes.
- Explore and address organizational value opportunities (physician access needs, quality scores, and HEIDS Metrics4).
- Pursue opportunities for value-based agreements or payor partnerships.
- Implement efficient programs by optimizing technology and targeting the right patients.
- Promote and publish program outcomes.
- Advocate at the state and federal levels for provider status and enhanced reimbursement.
Virginia Mason Franciscan Health
Laura Hanson, Virginia Mason Franciscan Health, said that like at other organizations, pharmacists began working in primary care in the mid-1990s, focused on anticoagulation management and refill management; services expanded to other chronic diseases, clinic visits, and opioid therapy management. In 2015, Washington became the first state to allow provider billing for pharmacists with prescriptive authority. The implementation of billing did not change the day-to-day work, said Hanson, but created a revenue stream that allowed for pharmacy programs to grow.
The practice model includes three pillars, each with specific activities. Embedded clinic pharmacists focus on patient-facing visits, both in person and virtual. They help with disease state management for conditions including diabetes, chronic pain, hypertension, and specific specialties. Hanson noted that this team evolved during the COVID-19 pandemic. Before that, pharmacists spent 60 percent of their time with patients and 40 percent on indirect care. The pandemic gave the centralized team an opportunity to reassess their workflow and make room for more patients to be seen each day. The second pillar, centralized pharmacy services, has a centralized pharmacist consult pool, offers phone or portal visits, and focuses on anticoagulation management and refill and prior authorizations. Finally,
___________________
4 The Healthcare Effectiveness Data and Information Set is a tool used to measure and improve health care quality (NCQA, 2025).
the population health pillar conducts patient and provider outreach and implements quality initiatives and internal dashboard review.
The ambulatory pharmacy program has 17 full-time embedded clinic pharmacists; nine are in primary care and eight in specialty care clinics. All are residency trained and board certified. It has two postgraduate residents; Hanson said this provides additional support for projects and also serves as a pipeline for talent recruitment. The centralized team clinic is staffed with three pharmacists and two technicians, who, Hanson said, are invaluable for all the nonclinical work they take off the pharmacists’ plates. The primary and specialty clinics have about 32,000 annual patient visits, with $7.5 million in gross charges. The billing method is the same as for other clinic providers, said Hanson, with a target of 8–12 patient visits per clinic day.
Virginia Mason’s pharmacy practice model has many demonstrated benefits, said Hanson. Pharmacists free up time for other clinicians, who can then spend more time with patients, and financial impacts, patient outcomes, and quality metrics improved. The pharmacists are supported by the billing and coding teams, just like other providers, and the mixed model of clinic-based pharmacists and centralized services (CS) makes patient care efficient, flexible, and accessible. Despite these benefits, said Hanson, sustainability faces numerous barriers. In a fee-for-service model, it can be difficult to show a positive outcome for pharmacists, said Hanson. Pharmacists on the care team do not generate as much revenue as others, with limited Medicare codes for their services. In value-based care, their contribution can be difficult to separate out and measure. Other barriers include increasing health care costs, stagnant reimbursement rates, and increased scrutiny of the return on investment after billing was implemented.
Despite challenges to sustainability, said Hanson, there are also always new opportunities. Looking forward, Hanson identified requirements she felt could capitalize on these, starting with a need to improve clinic efficiency with template use and accurate scheduling. She also identified other conditions, including maintaining and improving billing practices, having a vision to reimagine the potential roles for pharmacy technicians and pharmacy learners, and leveraging technology to improve workflows and identify patients who could benefit from pharmacist services and programs.
Community-Based Pharmacy Solutions for All
Community pharmacies are the greatest untapped and underleveraged setting of care in the health care system, with the greatest unrealized potential, said Troy Trygstad, CPESN USA. They cover a large area of the country, he said, making it possible to provide care to many people. For example, as mentioned, during the COVID-19 pandemic, an estimated 350 million interventions occurred across roughly 50,000 community-based
locations. Now, 90 percent of all adult vaccinations are in a community pharmacy; these have great potential, he said, but the business model prevents them from fulfilling it. Specifically, Trygstad argued that the lack of ability to differentiate impedes evolution. Not all pharmacist–practitioner encounters would need to be the same, he said. There are different medical providers, from the emergency room to dermatology, and pharmacy should have similar differentiation.
The base pharmacy is historically the only model in the market. These pharmacies meet minimum regulatory standards, dispense pills, and provide basic patient counseling, drug use review, and other legally mandated services. The “pharmacy-plus” model, said Trygstad, adds services such as vaccines, medication synchronization, and comprehensive medication reviews. “Pharmacy-plus-plus” would add things like pharmacist prescribing, medication administration, care coordination, behavioral health support, blood pressure monitoring, and opioid management, and “pharmacy-plus-plus-plus” would add services like clinical home visits, lifestyle coaching, wellness visits, and chronic care management. Given the utility of each of these models, Trygstad said there would be no need to transition all pharmacies up to the highest model to add value to the system; all such models have room and value.
Pharmacies are relatively inexpensive to the health care system when considering their wide accessibility and number of patient encounters, said Trygstad. Of the entire roughly $3.6 trillion spent on health care, community pharmacies cost the system 0.86 percent to operate based on the margin between what they bought medications for against what they sold them for plus a dispensing fee, or about $31 billion (IQVIA, 2018). To transition pharmacies to a new sustainable model that provides the care that patients need, it would require a yearly opportunity for services billing of between $2 and $8 billion, comprising 6-25 percent of their operating margin. This represents only about 0.08 percent to 0.27 percent of national health care expenditure and would create enough scale for widespread adoption of a services-based community pharmacy model, preserving more than 50,000 locations for patients to access frontline health care services. While the system spends a relatively large amount of money for the medications dispensed by pharmacies, the system spends very little on the optimal use of those medications and practice of pharmacy itself.
Trygstad identified common barriers to expanding and improving community pharmacy practice. Workflow friction is the biggest and the hardest to overcome, he said. However, he noted that technology and new practices may mitigate some of it, such as with central fill or appointment scheduling. Another barrier is the resources consumed by administrative tasks and costs, along with the lack of scale. The cost of care delivery is relatively fixed, said Trygstad, but administrative costs per transaction go down as
transactions go up. The pandemic demonstrated how scaled-up services could be financially sustainable for community pharmacies. Other barriers, he said, include a lack of evidence pairing outcomes with services, and a lack of clinical training or knowledge. The latter, however, is the smallest and can be overcome quickly.
POLICIES FOR FINANCIALLY SUPPORTED ROLES FOR PHARMACISTS
In this session, moderated by Lockman, speakers and participants explored the question of how government, industry, and health systems can assist in advancing sustainable, financially supported roles for pharmacists.
Setting the Stage
Randy P. McDonough, Towncrest Pharmacy Corp, set the stage with an overview of relevant policies. He noted major challenges in health care. The provider side has shortages, particularly in primary care, community-based pharmacies are closing, and many vulnerable patients live in health care and pharmacy deserts. Within the health care system itself, challenges include siloed practice; lack of collaboration, consistent reimbursement, and payment models to support team-based care; and multiple stakeholders with different priorities. However, said McDonough, challenges offer opportunities to make changes and positively impact the system.
Prescription drugs account for almost 10 percent of annual health care expenditures, or about $405 billion (AMA, 2025). Unfortunately, he said, issues with medication actually cost more than the medications themselves. In 2016, the cost of nonoptimized medication therapy was estimated at $528 billion, with over 275,000 associated deaths; McDonough explained that it includes nonadherence, underprescribing, adverse effects, and new medical problems and that “inexpensive drugs can cause costly adverse events and even death if not appropriately monitored.” Pharmacists are uniquely educated and trained as drug therapy experts, but the system does not recognize them as such. McDonough argued that acknowledging and paying pharmacists for their services adds value to the health care system.
McDonough shared a story of his experience with the Wellmark Value-Based Pharmacy Program, where he challenged the biggest payer in Iowa to think differently about community pharmacy; it transferred 600 commercial patients to the program. After 12 months, the program resulted in $300 savings PMPM, or about $2.4 million. McDonough said that they found 114 drug therapy problems, thanks to open communication and partnership among pharmacists and providers. He wondered, “What are we missing when we are not communicating?” Pharmacists can improve
patient care, reduce unnecessary use of health care resources, and reduce costs, he said, but a need remains to be able to fully use the training and education pharmacy students receive, and a full understanding of how to collaborate with other health professionals.
With shifts in policy, pharmacists would be able to realize their full potential for positively impacting patient care. McDonough listed actions that he believed could facilitate this:
- Sufficient reimbursement for products and services;
- Pharmacists recognized and paid as providers of primary care services, medication management, and care coordination activities;
- Standards of care regulations for pharmacy practice in all states;
- Shared electronic health records; and
- Better payment models that recognize the contributions of each member of the health care team, including pharmacists.
Panel Discussion
As other speakers mentioned, said Tom Kraus, ASHP, getting pharmacists recognized as providers by Medicare is an important step to adequate reimbursement. Given that this change is not immediately likely, Kraus offered three other solutions that could improve financial sustainability. First, he encouraged action on the state level, saying that most progress has been in the states. Over the past decade, several states have changed their laws to require commercial and/or Medicaid payers to cover certain pharmacist services (see Figure 4-1). Kraus encouraged stakeholders to “pour fuel on this fire” by putting resources into advocacy in states that do not require payment for all pharmacist services from public and commercial payers, which may also pay off on the federal level. It makes for a “totally different conversation” with federal representatives if a constituent points out that the lack of federal recognition of pharmacists as providers means that seniors are the only ones in the state who cannot access pharmacy services.
The second opportunity, said Kraus, is the mechanism of “incident-to-billing.” It allows physicians to bill Medicare for services provided by a pharmacist on the care team. However, the $22.64 reimbursement for pharmacists using the 99211 code is not sustainable (FC Billing, 2025). Increasing this rate through federal legislative changes is not a substitute for Medicare provider status, he said, but is an important separate opportunity for advocacy.
Finally, Kraus emphasized the importance of focusing advocacy on Medicare Advantage (MA) plans. These cover more beneficiaries than traditional Medicare and already can recognize pharmacists as providers. Getting
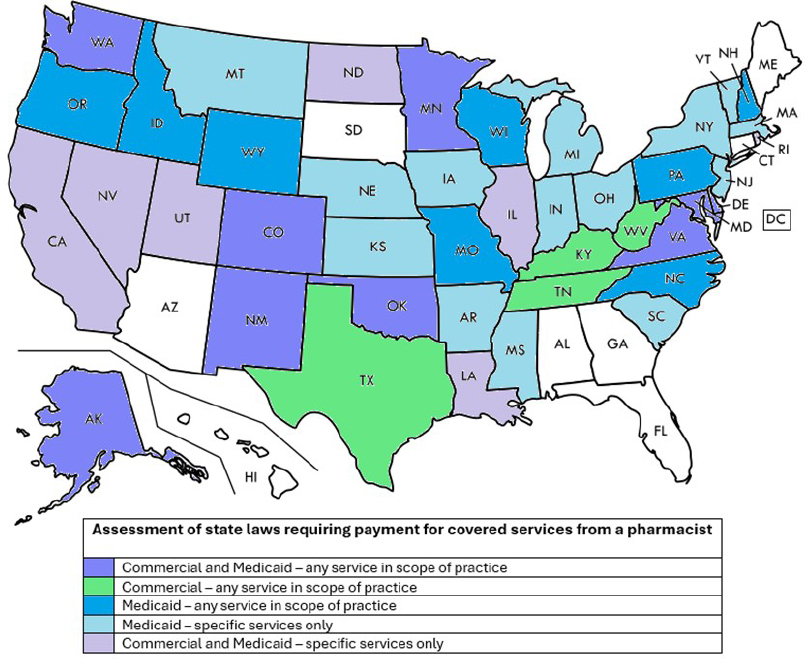
SOURCE: Presented by Tom Kraus on May 29, 2025. Created by and used with permission from the American Society of Health-System Pharmacists.
MA plans to recognize and pay pharmacists is a matter of contracting, he said, and making arguments about the benefits of coverage; for example, pharmacists could help payers satisfy network adequacy requirements.
Mark Atalla, formerly at CMS, said that the big question is how to make pharmacy financially viable not just today but in the future. With advances in health technology and workforce changes that will result in less primary care availability, current pharmacy policy and payment incentives would need to evolve to match the level of care and services that pharmacy will be called on to provide.
To better align policies with the needs of pharmacy, there are two questions to answer. First, what is the value of pharmacy, and how is that value reflected in policy? Second, where are the key gaps in the future, and how can pharmacists close those gaps with the right incentives and policies?
At a macro level, policies reflect our values as a society, said Atalla. Society largely views pharmacy as a model for medication dispensing, so payment policies reflect that limited, outdated view, rather than the professional care services pharmacists have been taught to provide. Evolving this view could help shift the profession toward a services model, although this would mean educating federal policy makers on what such a service model means and what value pharmacists contribute to the health care system. One way to do that is by highlighting examples on the state level that show pharmacists serving as providers, how that can improve access to care, and that federal reimbursement does not match the level of care. The second issue, said Atalla, is considering how to mitigate future gaps and needs across the population. Primary care shortages are projected to get worse. The early 2030s will see 80 million seniors and $2 trillion spent annually on Medicare alone (Board of Trustees, 2024; Washington Times, 2018). Artificial intelligence (AI) is rapidly evolving, both in general and within the health care system. Looking toward the future optimistically, Atalla said that he could see pharmacy filling the gaps by leading the way on at-home diagnostics, devices, and drug therapy. However, for this to happen, pharmacists would have to be able to practice at the top of their license and be recognized and paid for their services.
Pharmacists are essential components of team-based care, said Rodgers, but the current fee-for-service payment models are not sustainable. By advocating for other models, it could be possible to recognize the value of team-based care. Rodgers pointed to examples in pharmacy and other areas, such as palliative care. He noted the enormous power in partnerships to improve patient care and make it more efficient and effective. For example, he and his colleagues created a program in which physicians trained community pharmacists on hypertension management and allowed patients to schedule follow-ups with a pharmacist instead. Pharmacists had full access to the electronic health record and were able to send blood
pressure readings and other information to the physician. This model made appointments far more flexible and convenient for patients, he said, and facilitated pharmacists and physicians working together to optimize care. Rodgers noted that any physician who has had a chance to partner with a pharmacist has found it to be an “incredibly valuable experience.” He encouraged everyone, from payers to providers, to move outside of their own silos and work together to advocate for change.
DISCUSSION
Tom Bateman, Rutgers, the State University of New Jersey, facilitated a discussion among panelists and participants.
Value-Based vs. Fee-for-Service Models
Magaly Rodriguez de Bittner, University of Maryland School of Pharmacy, asked panelists how they balance the dual worlds of fee-for-service and value-based models and whether they would immediately switch to a value-based system if they had a “magic wand.” Hanson said that many health systems are in value-based contracts, with both incentives for exceeding targets and penalties for falling short (upside and downside contracts). Despite the room for both models, Hanson said that many providers find it challenging to make ends meet with fee-for-service models. Alternate payment models are likely the “way of the future.” Brummel added that not all value-based models are equal. From a health system perspective, consistent fee-for-service payments may help offset the less reliable finances of the value-based model. Trygstad agreed, saying that health systems need fee-for-service payments to make payroll. Zook added that it can be difficult to find outcomes to support the shift to value-based care. As a profession, pharmacy would have to gather evidence about its value and outcomes to support this. One concern specifically for pharmacy, said Kliethermes, is that pharmacists are not always on the radar as a key person in a value-based model. Depending on how the model is structured, a value-based system might actually be detrimental to pharmacy.
Credentialing
Lucinda Maine, CEO emeritus of the American Association of Colleges of Pharmacy, observed that it can be difficult for community pharmacists to get credentialed to deliver and be paid for their services. She asked panelists for their thoughts on what can be done to build legitimate credentialing models that will work in the marketplace. Zook noted that “credentialing” means different things to different people. At Geisinger, an effort to credential pharmacy residents required a “big conversation” with people who
were saying the same words but not “speaking the same language.” This was a big barrier, she said. Brummel added that some Minnesota health plans credential and enroll pharmacists for services such as CMM. New legislation has added additional codes that pharmacists can use for billing, and Brummel mentioned a “little bit of panic” around how or whether pharmacists will be credentialed or enrolled for these services. If hundreds of pharmacists want to be credentialed under the new codes, she said, it would be an enormous effort.
Medicare Provider Status
Lockman asked panelists to comment on the push for Medicare provider status for pharmacists. Atalla replied that if he were at CMS today, he would look at the payment models in states and push to align state policy with federal policy. There are many dually enrolled patients (e.g., Medicaid and Medicare), so it is challenging when payment rules are not aligned and services are covered by Medicaid but not Medicare. Educating CMS on this misalignment seems like a “rational next step,” said Atalla. Kraus repeated his point that Medicare provider status is very important but that other opportunities to advance payment exist in the meantime. Rodgers issued a cautionary note. Medicare Part B is statutorily required to be budget neutral, so any new services added reduce the value of other services. In other words, the pie doesn’t get bigger; everyone billing gets a little less. Furthermore, Part B is not subject to the Medicare economic index for rising costs. Health professionals from all disciplines can work together to advocate for sustainable payments for all professionals, said Rodgers. McDonough countered that giving pharmacists provider status not only would improve access to care but also could have a positive impact on the total cost of care. While paying pharmacists for services would add costs, these could be offset by savings created through more efficient, effective care.
Role of Residents
Lockman asked panelists how pharmacy residents can help support financially sustainable roles for pharmacists. Kraus began by noting that residency programs are critical to building the workforce. Services provided by postgraduate year (PGY) 1 residents in an inpatient setting are reimbursed by Medicare, he said, but services in a community or ambulatory setting or by a PGY2 resident are not reimbursable and provided at a loss. This is a big gap in policy, said Kraus, and advocating for support for these training programs would help train and meet the workforce demands. Across all health care professions, said Rodgers, there are multiple reasons to integrate learners and residents into care teams. Integrating pharmacy
residents can improve quality and safety, with a strong argument to be made that it helps to build a habit of interprofessional practice and teamwork. Furthermore, the implicit business model of academic health centers relies on the work of less expensive learners and residents; despite costs associated with training and supervision, the model brings overall value to the system.
Buy-in From Physicians
In the pursuit of financially sustainable pharmacy practice, asked a participant, how might pharmacists work together with physicians and get buy-in on issues such as payment and provider status? Rodgers replied that health professionals could tell their stories together. There is movement toward a total-cost-of-care model, where pharmacists would demonstrate to their organizations that they can deliver on care, quality, safety, patient experience, and cost containment. Rodgers encouraged pharmacists who work with physicians to sit down with them and ask what problems they can help solve. Starting from the ground up, with physicians and pharmacists collaborating to improve patient care, is one way to generate momentum for change at the top. McDonough added that the only way to gain trust and buy-in from physicians and other health professionals is by demonstrating competence. When pharmacists conduct interventions that make a difference in patient care, other team members see their value.
Telling the Story of Pharmacy
Peter Swan, University of Florida, believed that changing minds and policies could be possible if the story of pharmacy is told in ways that are understandable and relatable. McDonough agreed, recalling that he was abruptly cut off in an interview on a national radio show when he started listing statistics rather than stories. Having learned his lesson, he began with a patient case when he testified to the Senate Judiciary Committee. McDonough noted that even his own family did not recognize his expertise until they personally needed his help making life-and-death decisions. Every pharmacist has a story about connecting with a patient during an emotional time, and “we need to be telling these stories,” he said before adding, “better yet, let patients tell the story for us.” Kraus agreed that patient stories and experiences are what shape the perception of pharmacy. When a person experiences patient care with a pharmacist, they “get it.” Kraus pushed back on the idea that policy makers do not understand the shift in pharmacy toward a model of patient care. He contended that the conversation has changed in the last 5 years and that most policy makers now understand this. He noted only incremental progress toward recognition
and payment, but it is all in the same direction. In the past year, around 20 bills were passed expanding pharmacist scope of practice, and several bills recognized them as providers. Change is happening, he said, and it is important to continue to put resources and advocacy into these areas. A participant commented that while stories are critical to convey the value of pharmacy systematic research is equally important and has a gap on what patients want and how pharmacy can innovate to provide what patients need. He noted that “we never knew we needed iPads until Apple said we did,” and now they are embedded in our everyday lives. Similarly, the profession can go a long way by thinking creatively about how to meet patients’ needs. Atalla noted the fair amount of research demonstrating the value of pharmacy—such as data gathered during the pandemic on the services provided—but much of this research has not been widely discussed. He agreed that stories are often what capture people’s attention.
This page intentionally left blank.















