A New Vision for Women's Health Research: Transformative Change at the National Institutes of Health (2025)
Chapter: 6 Women, Health, and Society
6
Women, Health, and Society
INTRODUCTION
The previous chapter illustrates the role that biological factors, such as chromosomes and hormones, have on women’s health. Biological sex shapes health in many ways, potentially offering vulnerability or resilience to various health conditions (NASEM, 2024a). However, women’s health is also strongly shaped by the social and structural context of their lives, including their income and wealth, education, employment, location, family structure, and larger structural and policy forces. The social factors that contribute to gendered differences in men’s and women’s lives can also interact with each other and with biological differences, confounding or exacerbating the latter. Consequently, the health differences seen between women and among women compared to men are products of social and biological factors. Moreover, other identities, including gender identity, race, ethnicity,1 and sexual orientation, shape women’s health. These biological and social and structural factors intersect and can be bidirectional.
This chapter provides a high-level overview of how structural and social determinants of health can influence women’s health, illustrating why the national research agenda needs to specifically focus research investments to
___________________
1 As discussed in Chapter 1, this report strives to be consistent in its use of the following terms to describe specific racially and ethnically minoritized populations: “American Indian or Alaska Native,” “Asian,” “Black,” “Hispanic or Latino/a/x/e,” “Native Hawaiian or Pacific Islander,” and “White.” However, when describing data from cited studies, the terminology from source papers is used, introducing differences in language. This is also the case with the report’s use of LGBTQIA+ and similar variations, such as LGBT, LGBTQ, and LGBTQ+. This is especially common in this chapter.
better understand how these factors shape the health of girls and women as it seeks to develop solutions to improve their health and well-being. While the structural and social determinants cover a large range of domains, this chapter offers an overview of select examples.
STRUCTURAL AND SOCIAL DETERMINANTS OF HEALTH
Healthy People 2030 organizes the social determinants of health (SDOH) into five domains: health care access and quality, economic stability, neighborhood and built environment, social and community context, and education access and quality (OASH, n.d.-a). The structural determinants of health are the
macrolevel factors, such as laws, policies, institutional practices, governance processes, and social norms that shape the distribution (or maldistribution) of the SDOH (e.g., housing, income, employment, exposure to environmental toxins, interpersonal discrimination) across and within social groups. Structural determinants of health, also referred to as the ‘determinants of the determinants of health,’ include structural racism and other structural inequities and thus influence not only population health but also health equity. (NASEM, 2023b)
The 2024 National Academies of Sciences, Engineering, and Medicine (National Academies) report Advancing Research on Chronic Conditions in Women provides an overview as well as research gaps on the structural and SDOH as they specifically affect women, including structural sexism and health policy (NASEM, 2024a). See Figure 6-1 for a visualization from that report showing how biological, social, and structural determinants can affect women’s health. As that report highlighted, gender-related social and cultural factors can lead to diverse exposures and experiences within the framework of structural and social determinants of health. These factors, through a range of mechanisms, affect not only preventive behaviors but also the onset, characteristics, and progression of various health conditions (NASEM, 2024a). In addition, women often face unique challenges in the health care system, including differences in clinical practices and patient-centered care, which can further influence their health outcomes. For example, weathering (see Figure 6-1) refers to the cumulative negative effect of chronic stress from social and economic adversity on the physical health of marginalized groups and results in premature biological aging and increased health vulnerability. It can yield adverse health outcomes (Geronimus et al., 2006; Simons et al., 2021).
Women navigate the world in ways distinct from men, and women who are additionally marginalized because of other facets of their identity face unique and additional challenges, making health equity a crucial
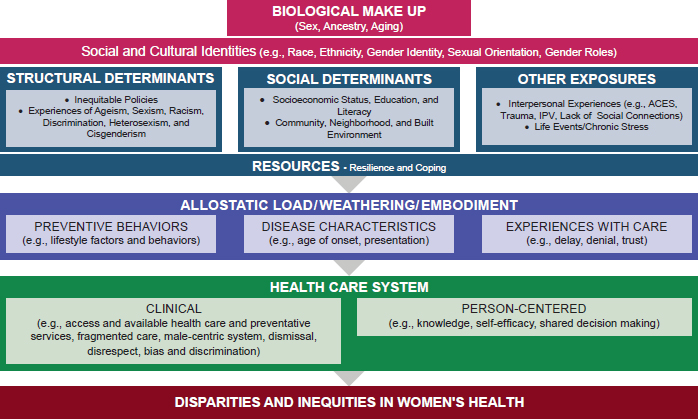
SOURCE: Adapted from NASEM, 2024a.
consideration within women’s health. If equality is defined as treating all individuals in the same manner, it is important to emphasize that equity is not interchangeable. Equality assumes a level playing field for everyone without accounting for historical and current inequities. According to the World Health Organization, “equity is the absence of avoidable or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, [or] geographically” (WHO, n.d.). In other words, equity is the process, and equality is the outcome. Equity focuses on justice (NASEM, 2023b).
In many areas, women experience not only differences in health outcomes compared to men but also inequities in health and health care. Health and health care inequities are driven by structural and social determinants, meaning they are more than just “differences.” For example, the 2020 National Academies report Birth Settings in America: Outcomes, Quality, Access and Choice describes structural inequities and biases, including racism, on the systemic, institutional, and interpersonal levels that underlie SDOH for racially and ethnically minoritized women (NASEM, 2020a). Systematic oppression related to race, sexual orientation, gender identity, age, weight, ability, and more are especially harmful to women, who also experience sexism and misogyny. In addition, laws and policies are important macrolevel factors for consideration (Everett and Agénor, 2023; Jahn et al., 2023; Zubizarreta et al., 2024). These factors combined have contributed to deprioritizing and undervaluing women’s health research (WHR). The remainder of this chapter outlines how social and structural
determinants drive inequities in women’s health and WHR, including consideration and examples of how the intersectional identities of women who are racially and ethnically minoritized, disabled, lesbian, bisexual, transgender, or otherwise marginalized further shape outcomes, and illustrates why these need to be considered in the development of the nation’s research agenda on women’s health.
STRUCTURAL DETERMINANTS OF HEALTH
Discrimination
Sexism
Structural sexism is “systematic gender inequalities between men and women in power and resources, as manifest in institutions, interactions, and individuals” (Homan, 2021). It is reflected in policies and institutions, such as how many women participate in the labor force, the ratio of men’s to women’s median weekly earnings, poverty rates, and percent of state legislative seats occupied by men versus women (Homan, 2019). Researchers have begun to explore how structural and systemic forms of gender-based discrimination affect women’s health (Homan, 2019; Krieger, 2001, 2014; Philbin et al., 2024). For example, data suggest that bias against women in the workplace negatively affects women’s health and, furthermore, that women living in states with high levels of structural sexism have approximately twice as many chronic health conditions compared to women in states with lower levels (Cunningham and Wicker, 2024; Homan, 2019). The health effects are substantial—women exposed to high structural sexism appear to have a health profile about 7 years older than women in low-sexism states (Homan, 2019). Additionally, structural sexism amplifies other forms of discrimination, such as structural racism, ableism, hetero-sexism, and classism, compounding negative health effects for women with multiple marginalized identities (Homan, 2019, 2021; Perry et al., 2013). For example, Everett et al. (2022a, 2024b) have linked structural heteropatriarchy (i.e., the combined impact of structural sexism and discrimination against lesbian, gay, and bisexual populations) to increased risk of preterm birth, decreased birthweight, and maternal cardiovascular morbidities. Moreover, the effects from such discrimination accumulate over time to affect women’s health (Kelley and Gilbert, 2023).
Studies have also shown that structural sexism affects women’s access to health care. For example, researchers examined state-level sexism using state-level indicators of administrative data, such as the ratio of men-to-women earnings, employment, poverty rate, and paid family leave policy,
and their effect on access to health care. Higher state-level sexism was associated with greater barriers to accessing health care and affordability for Black and Hispanic but not White women, illustrating the effect of intersectional structural discrimination that racially and ethnically minoritized women face (Rapp et al., 2021).
Beyond access to health care, studies have examined the effect of structural sexism on the use of preventive health care, cesarean-section rates, breastfeeding, and disordered eating (Balistreri, 2024; Beccia et al., 2022; Dore et al., 2024; Nagle and Samari, 2021; NASEM, 2024a). Gender discrimination is also a major source of stress that directly affects mental health. Women who report experiencing discrimination are more likely to suffer from depression and anxiety (Vigod and Rochon, 2020). Moreover, research suggests there are fewer gender differences in mental illness rates in more gender-equal societies, suggesting discrimination may play a major role in these disparities (Yu, 2018). Future research on measuring structural sexism needs to consider the longitudinal nature of its effects, as most studies are cross-sectional; capture dynamic and complex ways in which systems of oppression affect women’s health; and identify strategies to intervene (Beccia et al., 2024; Homan, 2019).
Racism, Colonialism, and Health Outcomes
A long history of colonialism and racism, reflected in policies, systems, and communities, drive U.S. health inequities (KFF, n.d.; NASEM, 2017, 2023b). The 2023 National Academies report Federal Policy to Advance Racial, Ethnic, and Tribal Health Equity details this history of racism, discrimination, and colonialism; its effect on health outcomes; and the need to address these root causes (NASEM, 2023b); to do so, research needs to account for these underlying structural causes to understand how they affect human biology and the ability to access needed services to prevent, diagnose, and treat health conditions.
Colonialism
Colonialism involves control of “people [and] the context of their lives—control of the economy through land appropriation, labor exploitation, and extraction of natural resources; control of authority through government, normative social institutions, and the military; control of gender and sexuality through oversight of the family and education; and control of subjectivity and knowledge through imposition of an epistemology and the formation of subjectivity” (IOM, 2013, p.13). The American Indian and Alaska Native (AIAN) population is a salient example in which colonialism affects health. To advance health for AIAN women, it is essential to
understand the history of colonialism and how it continues to reverberate through all aspects of health at systems, community, and individual levels.2
The effects of colonialism have created modern health inequities through violence, targeted eradication of AIAN people, erasure of culture, dispossession of land, removal from tribal homelands, forced urbanization, and more (Brown-Rice, 2013; Carroll et al., 2022; Moss, 2019; NASEM, 2023b). AIAN women have been threatened with forcible removal of their children and endured forced sterilization (Newland, 2022; Stern, 2020). The forcible placement of AIAN children in boarding schools and non-AIAN homes has also resulted in cultural eradication (Newland, 2022). These historical events have negatively affected AIAN women’s health, creating inequities in cancer, heart health, mental health, maternal mortality, violence, and more (American Heart Association, 2023; CDC, 2023a; KFF, 2022a; Kwon et al., 2024; Moss, 2019; NASEM, 2017, 2023b; Petrosky et al., 2021; Statista, n.d.; Urban Indian Health Institute, n.d.).
For example, the pregnancy-related death rate among AIAN women is nearly double that in White women (26.2 per 100,000 vs. 13.7) (KFF, 2022a). A review of pregnancy-related deaths among AIAN populations finds that about one in three is attributable to mental health conditions (Trost et al., 2022). Moreover, 2020 data suggest that approximately 92 percent of AIAN maternal mortality is preventable (CDC, 2024).
Like other health disparities affecting AIAN people, mental health outcomes need to be considered in the context of historical trauma resulting from colonialism. Suicide is one of the leading causes of mortality among AIAN people (Statista, n.d.). Although negative mental health outcomes are of great concern for AIAN women, the literature on AIAN mental health research is scant (Kwon et al., 2024). These health inequities exist, but it is important that solutions be framed to include community assets and viewed in terms of attaining balance among the components necessary for health and well-being in alignment with an Indigenous model of health, a concept based on the Medicine Wheel3 (Greer and Lemacks, 2024; National Library of Medicine, n.d.).
When studying SDOH, it is also important to understand the Indigenous SDOH—that is, the factors that impact the health and well-being of Indigenous peoples uniquely. Seven Directions, the first national public health institute in the United States to focus solely on health and wellness for Indigenous people, asserts “[Indigenous SDOH] could include our
___________________
2 The report Federal Policy to Advance Racial, Ethnic, and Tribal Health Equity provides a detailed history of tribal health and how it has led to significant health inequities (NASEM, 2023b).
3 “The Medicine Wheel, sometimes known as the Sacred Hoop, has been used by generations of various Native American tribes for health and healing. It embodies the Four Directions, as well as Father Sky, Mother Earth, and Spirit Tree—all of which symbolize dimensions of health and the cycles of life” (National Library of Medicine, n.d.)
connection to our traditional lands, tribal sovereignty, tribal governance, our unique tribal or urban Indian health care system, the access we have to our traditional lifeways, native languages, traditional foods, ceremonies, relationships, and many more factors. The process of mapping social determinants of health with and for AIAN communities can and should include the factors or conditions that are only found in our tribal or urban Indian settings” (Seven Directions: A Center for Indigenous Public Health, 2023). These are all essential factors to consider not only for research (e.g., including tribal consultation) but also when developing programs, policies, and laws impacting AIAN communities.
Racism
Racism is a structural system resulting from the intersection of social and institutional power and racial prejudice. Policies, practices, and attitudes within this system operate to constrain or enhance access to resources, privileges, and advantages based on race. These privileges disproportionately accrue to some groups and are withheld from others according to social constructions of race and ethnicity (NASEM, 2023b). The psychological toll of racism can directly harm physical and mental health; it increases cortisol levels and weakens the immune system (Berger and Sarnyai, 2015; Chen and Mallory, 2021). In addition, chronic stress from racism is linked to increased risk of hypertension and poorer health at earlier ages (Dolezsar et al., 2014; Geronimus et al., 2006; Hicken et al., 2014).
As discussed in Chapter 2, Black women in the United States experience significant negative health outcomes relative to White women, such as early menopause transition with more severe symptoms, higher fibroid incidence, higher rates of pregnancy-related adverse events, and higher incidence of chronic conditions, such as heart disease and diabetes (Chinn et al., 2021; Harlow et al., 2022; Howell, 2018; Katon et al., 2023). Pregnancy-related mortality is highest among Black women, at 41.4 per 100,000 compared to 13.7, 11.2, 14.1, and 26.2 for White, Hispanic, Asian and Pacific Islander, and AIAN women, respectively (KFF, 2022a). Black, AIAN, Asian, and Pacific Islander women are more likely to experience preterm births, low-birthweight babies, or births after late or no prenatal care compared to White women (KFF, 2022a). Black women are almost two times more likely to experience infertility than White women, and Black, Latina, and Asian women are less likely to receive infertility and fertility preservation treatments (Dongarwar et al., 2022; Weiss and Marsh, 2023). The continuing effects of structural racism, rooted in a history of slavery and colonialism, impede advancing the health of Black women (Bleich et al., 2024), who constantly need to negotiate their identities based on a past entrenched in oppression, which influences their social interactions, mental health, and access to opportunities (Presumey-Leblanc and Sandel, 2024).
Hispanic and Latina women are more likely to be diagnosed with breast cancer at a more advanced stage, experience higher mortality rates from it, and, as breast cancer survivors, face a higher risk of cardiovascular disease (CVD) and related mortality compared to non-Hispanic White women (Gonzalo-Encabo et al., 2023; Paz and Massey, 2016). Black and Hispanic patients are significantly less likely than White patients to have minimally invasive surgery for uterine fibroids and more likely to undergo hysterectomies (Eltoukhi et al., 2014; Katon et al., 2023). These disparities reflect broader issues of racism and discrimination, which contribute to unequal access to health care and SDOH, exacerbating the health inequities faced by these communities.
Furthermore, research on structural determinants of health, including racism, is hampered by shortcomings in data collection and measurement of structural racism and other forms of discrimination (Hing et al., 2024; NASEM, 2023b). In addition, what the research enterprise considers “science” impacts the role of race and ethnicity and the types of studies conducted. For example, community-engaged research—representing a spectrum of approaches where community members and organizations and/or researchers collaborate—can be used to better identify mechanisms to prevent and address complex health issues impacted by bias, racism, and the structural and social determinants of health. These tools are underused and will be important to apply in future WHR (NASEM, 2024a; Wallerstein and Duran, 2006).
Lesbian, Gay, Bisexual, Transgender, Queer or Questioning, Intersex, and Asexual (LGBTQIA+) Discrimination
Sexual and gender minorities (SGM), including lesbian, bisexual, Two-Spirit, queer, and transgender and nonbinary (TNB) individuals, also experience unique challenges and barriers to health and health care compared to heterosexual cisgender women and men. While the term “TNB” is used throughout this chapter, the focus is on the ways social and structural determinants of health affect transgender women as well as transgender men and nonbinary individuals assigned female sex at birth. SGM are subject to marginalization and stigma that can have a number of downstream effects, such as poorer economic outcomes and increased vulnerability to interpersonal violence (Badgett et al., 2019; Coston, 2023; Flores et al., 2021; Movement Advancement Project and Center for American Progress, 2024; National Coalition of Anti-Violence Programs, 2018; Peitzmeier et al., 2020). On medical and biological dimensions, for example, when seeking gender-affirming care, TNB individuals sometimes need to navigate discrimination from health care providers and barriers to such care. Figure 6-2 shows a framework for multilevel social and structural determinants of health outcomes in SGM populations (Diaz-Thomas et al., 2023). The later sections
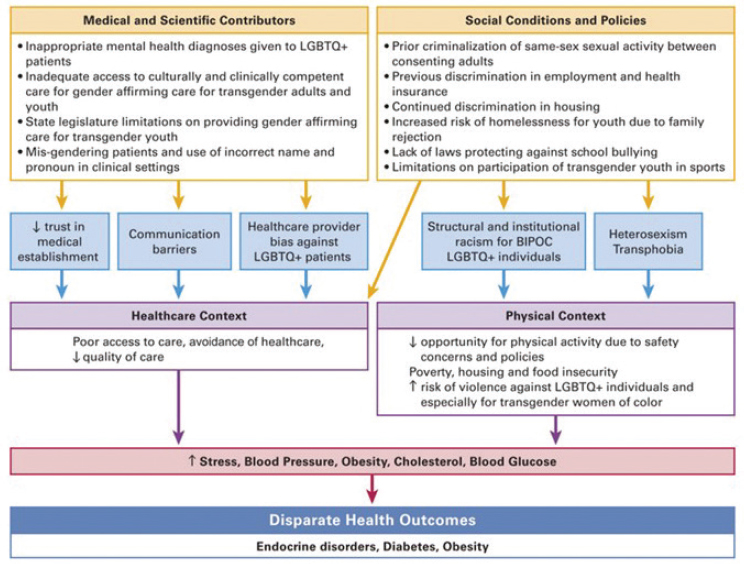
NOTES: LGBTQ+ = lesbian, gay, bisexual, transgender, queer, intersex, and asexual. Although not defined in the figure source, the acronym BIPOC can be used to refer to individuals who are Black, Indigenous, and people of color.
SOURCE: Diaz-Thomas et al., 2023. © Published by Oxford University Press on behalf of the Endocrine Society. All rights reserved.
of this chapter elaborate on several of these challenges and how they can affect health and well-being.
LGBT youth and young adults experience increased stress, labeled “minority stress,” particularly during the pubertal transition (Mason et al., 2023). The minority stress model was introduced by Dr. Virginia R. Brooks (later known as Winn Kelly Brooks) in her 1981 book Minority Stress and Lesbian Women (Brooks, 1981). It proposes that members of minoritized communities experience specific and additional stressors compared to the everyday stress majority populations experience over the life-span (Meyer, 2003). Over time, this can lead to activation of the hypothalamic-pituitary-adrenal axis, one of the body’s stress response systems, affecting physical and mental health (Diaz-Thomas et al., 2023; Hatzenbuehler and McLaughlin, 2014).
Although limited and underfunded, research points to unique sexual and reproductive health barriers among sexual minority women (SMW).
For example, compared to heterosexual women, SMW, including lesbian and bisexual women, may be more likely to experience pregnancy loss, stillbirth, low birthweight, and preterm birth (Charlton et al., 2020) and be at higher risk of developing cervical cancer (American Cancer Society, 2024). Data from Everett et al. suggest that these outcomes may be attenuated by policies that confer protections for SMW (Everett and Agénor, 2023; Everett et al., 2022b, 2024a). Contraceptive access is another area of concern; unintended pregnancy is higher among SMW compared to their heterosexual peers. Research on sexual and reproductive health inequities among racially and ethnically minoritized SMW remains especially limited (Agénor et al., 2021; Higgins et al., 2019).
For AIAN populations, gender is not a dichotomy of male or female. Precolonialism views on gender varied by tribe, with traditional languages including more than two genders. One modern term that applies only to Indigenous people is “Two-Spirit” (NASEM, 2020b; RRC Polytech, 2024). Two-Spirit people often face discrimination and marginalization from multiple directions. For example, they may experience racism and exclusion from non-Native LGBTQ communities, and within Native communities, they may encounter homophobia, transphobia, and rejection of their Two-Spirit identity (Tribal Information Exchange, n.d.). In broader society, Two-Spirit people face intersecting discrimination based on their racial, ethnic, gender, and sexual identities. The National Institutes of Health (NIH) funds little research on health outcomes for this population, with only three current NIH-funded studies with “Two-Spirit” in the title, abstract, or keywords based on a keyword search of RePORTER in October 2024 (NIH, n.d.). However, the limited evidence shows the discrimination Two-Spirit people face may contribute to health disparities, such as high rates of physical and sexual assault victimization, increased risk of mental health issues, such as depression and anxiety, greater likelihood of substance abuse, and elevated suicide risk (Robinson, 2022; Tribal Information Exchange, n.d.).
Weight Bias
Weight bias, also known as weight stigma, “refers to the negative attitudes, beliefs, stereotypes and discriminatory behaviors directed toward individuals based on their body weight or size” (Edwards-Gayfield, n.d.). This can manifest in various forms, including social exclusion and unfair treatment in both personal and professional settings. In health care, weight bias may lead to patients with higher weights receiving inadequate care, being blamed for their health conditions, or facing barriers to accessing necessary services. Weight bias often results in people seeking care later, avoiding it altogether, or receiving suboptimal treatment, which can exacerbate existing health issues and further marginalize this population (Lawrence et al., 2021). Furthermore,
the lack of investment in developing medical technology and resources to care for people along the weight spectrum, such as too few magnetic resonance imaging devices sized for large bodies, creates problems with care and likely affects overall health (Brydon, 2022; Kukielka, 2020; Ordway, 2023).
Some research indicates that weight bias is more prominent for women than men, and women report more internalization of it than men, meaning they are more likely to have self-disparaging thoughts and feelings because of their weight (Sattler et al., 2018). Women, particularly those with higher weights, often face greater societal pressure regarding body image and are more likely to experience weight-related stigma in various aspects of life, including health care (Puhl and Heuer, 2010; Voges et al., 2022). Furthermore, Black and Hispanic women are, on average, heavier than White women, indicating a likely intersectional component to the experience of racialized weight stigma in society and health care (OMH, 2024a, 2024b; Strings, 2019).
Despite growing awareness of weight bias and its impact, a significant gap remains in research on how it mediates and moderates adverse health outcomes, particularly for individuals with higher weights. This gap is particularly critical given that weight bias can exacerbate disparities in health care access and treatment, compounding the challenges faced by those with higher weights and potentially leading to worse health outcomes. Addressing this gap is essential to comprehensively understanding and mitigating the effects of weight bias on overall health.
Disability
Disability4 is an important consideration when undertaking research on women’s health—across all ages, women have slightly higher rates of disability compared to men, and this gap widens with age (Office of Disability Employment Policy, 2021). Women with disabilities experience significant employment barriers compared to both nondisabled women and men with disabilities. Their employment rate (20.5 percent in 2023) is lower than both disabled men (24.8 percent) and nondisabled women (60.3 percent). Women with disabilities also earn less than men with disabilities (Ives-Rublee and Neal, 2024). This economic disparity leads to limited access to the positive SDOH (Friedman, 2024).
In general, women with disabilities have difficulty affording health care, medications, and other health-related needs (CDC, 2023b); those who face poverty, unemployment, and unmet health care needs because of financial
___________________
4 Disability can be defined differently across the relevant literature, with some relying on individuals with disabilities to self-report and others relying on questions about diagnosed conditions or functional capacity.
constraints are also more likely to suffer from heightened mental distress (Cree et al., 2020). Women with physical, intellectual, or sensory disabilities face a wide range of sociocultural and structural factors that negatively affect their access to health care services, including reproductive health services, such as sexual education, contraceptive care, and pregnancy-related care, but this research is limited (Biggs et al., 2023; CDC, 2023b; Matin et al., 2021; Ransohoff et al., 2022).
Laws and Policies
Laws and policies are critical structural determinants of women’s health. The following discussion provides a few examples focused on reproductive rights and rights for SGM.
Reproductive Rights and Justice
Reproductive justice, which encompasses the right to access reproductive health care and the socioeconomic and racial factors that influence health outcomes, is an important example for understanding the effect of structural determinants on women’s health (SisterSong, n.d.). Addressing reproductive rights and health through this lens provides a comprehensive approach to improving women’s overall health and well-being.
Regarding laws and policies, reproductive health and rights frameworks tend to focus on rights to abortion and contraception access. For example, the Supreme Court’s ruling in Dobbs v. Jackson Women’s Health Organization,5 which struck down decisions guaranteeing abortion care access at the federal level, has resulted in abortion bans and early gestational restrictions with direct effects on those seeking abortion care in nearly half the country (KFF, 2024; NASEM, 2023b). This case is a defining moment regarding women’s health and rights to bodily autonomy, and research has already identified numerous negative effects on women’s health care access and health outcomes (Ahmed et al., 2023; Thornburg et al., 2024; Zhao et al., 2024; Zhu et al., 2024). These laws also interact with broader structural determinants to shape women’s and girls’ sexual and reproductive health outcomes. For example, restrictive abortion laws are linked to higher levels of preterm birth and low birthweight among Black people compared to non-Black people (Redd et al., 2021).
However, a reproductive justice framework extends the work of reproductive rights and health by identifying and addressing a set of gendered, racialized, and economically determined structural determinants of health. The term “reproductive justice” was coined in the 1990s as a Black feminist
___________________
5 Dobbs v. Jackson Women’s Health Organization, No. 19–1392, 597 U.S. 215 (2022).
response to White feminist movement approaches to reproductive health and rights (SisterSong, n.d.). It was intentionally intersectional, meaning that the goal was to include the myriad ways Black, Latina, AIAN, and other racially and ethnically minoritized women, as well low-income White women, in particular experienced threats to bodily autonomy and reproductive dignity, something largely excluded from early feminist movements that centered on middle class and wealthy White women. Reproductive justice as a movement and conceptual framework made more explicit that true reproductive freedom had to include rights to have a child under the condition of one’s choosing (SisterSong, n.d.). This was responsive to injustices faced by Black, Latina, AIAN, and other racially and ethnically minoritized women, as well as women in poverty, including forced sterilization and medical experimentation with the first birth control pill on Puerto Rican women (Larson, 2021; NASEM, 2023b; Novak et al., 2018; Pendergrass and Raji, 2017; Stern, 2020; Washington, 2006). It is important to consider the evolution of NIH within this broader context and the effect this may have had on WHR.
Reproductive justice also includes as a central tenet that parents have a right to raise and care for their children in safe and healthy environments (SisterSong, n.d.). This final component focused on safe and healthy birthing and parental rights and has helped expand what it meant to advocate for reproductive justice and not just simply rights to reproductive control (Daniel, 2021). In this way, reproductive justice as a framework indicates that laws and policies that have allowed for forced sterilization of racially and ethnically minoritized women, unethical experimentation with the birth control pill on women, and other policies, such as the Indian Adoption Project, that have taken away parenting rights, fall under the rubric of gendered policies affecting women’s health (Adoption History Project, n.d.; Larson, 2021; Lawrence, 2000; Lopez, 2008; Pendergrass and Raji, 2017; Price and Darity, 2010; Stern, 2005).
The reproductive justice framework can be further expanded to a queer-inclusive lens. It is crucial to acknowledge that many of the issues Black feminists identified in the early 1990s are still prominent in the lives of many cis queer women, trans men, and nonbinary individuals assigned female at birth. An expanded framework is needed to address rights to access alternative insemination, reproductive technologies, gender-affirming care, and rights related to sexual behavior and orientation. Some reproductive justice advocates and scholars assert a fourth tenet—the human right to disassociate sex from reproduction and that healthy sexuality and pleasure are essential to whole and full human life (NASEM, 2021c; Virginia Sexual and Domestic Violence Action Alliance, n.d.; Well Project, 2024; Welleck and Yeung, n.d.).
As a facilitator of health, Medicaid expansion is associated with lower rates of maternal mortality, especially among Black people (Eliason, 2020).
Sexually transmitted infection diagnoses among adolescent SMW are significantly lower in states with lower structural stigma (compared to states with higher structural stigma), and sexual orientation antidiscrimination laws have been linked to lower maternal hypertension among Black and White lesbian and bisexual women (Charlton et al., 2019; Everett and Agénor, 2023). In addition, Earned Income Tax Credit laws are associated with decreased low birthweight, especially among Black people (Komro et al., 2019). These findings underscore how targeted policy interventions can address sexual and reproductive health inequities and the need to research how policy impacts health outcomes.
Rights for SGM
Over the past decade, U.S. legislative and judiciary bodies have set policies that have both affirmed and denied the rights of SGM populations. These legal shifts, and the cultural shifts they represent, are relevant structures that produce needs for health care and manage the contexts in which it is sought. Laws and policies related to gender-affirming care and sexuality rights are the contexts in which women’s health must be navigated. In addition, Supreme Court decisions, such as Obergefell v. Hodges,6 resulting in the federal right to same-sex marriage, and Bostock v. Clayton County,7 affirming that prohibiting sex discrimination in Title VII of the Civil Rights Act of 19648 protects employees against discrimination based on sexual orientation or transgender status, can affect women’s health by reducing stigma and discrimination and increasing access to insurance and economic stability through spouses and employers (National Constitution Center, n.d.; U.S. Equal Employment Opportunity Commission, n.d.). Similarly, the Affordable Care Act Section 1557 names sexual orientation and gender identity as protected in public health insurance coverage (HHS, 2024).
Numerous laws and policies at the federal and state level affect TNB individuals’ health, well-being, and health care quality and access. These include laws and policies that impede or protect TNB people’s ability to participate in sports, use restrooms, update identification documents in accordance with their gender identity, access health care, particularly gender-affirming care, or maintain protection from discrimination in housing or other domains (Hohne, 2023; Movement Advancement Project, n.d.-a,b,c,d,e,f,g,h). Recent years have seen an increase in proposed state legislation aimed at limiting their rights, with over 560 such bills under consideration in 2023 (Hohne, 2023). Numerous bills have banned gender-affirming care for transgender
___________________
6 Obergefell v. Hodges, No. 14–556, 576 U.S. (2015).
7 Bostock v. Clayton County, No. 17–1618, 590 U.S. (2020).
8 Public Law 88-352, 78 Stat. 241 (July 2, 1964).
youth, including banning medication and/or surgical care and sometimes making it a crime for clinicians to provide these (Movement Advancement Project, n.d.-a). Although these legislative efforts primarily restrict care for TNB youth, some state bills are restricting or attempting to restrict gender-affirming care for adults as well (Goldman, 2024). In 10 states, Medicaid policy explicitly excludes coverage of gender-affirming care for individuals of all ages (Movement Advancement Project, n.d.-g).
Conversely, some state laws protect access to health care for TNB people; 14 states and the District of Columbia (DC) have “shield” laws that aim to protect transgender individuals, their families, and medical providers traveling from a state where gender-affirming care is banned to provide or receive it (Movement Advancement Project, n.d.-h). Laws in 24 states and DC prohibit insurers from refusing to cover such care (Movement Advancement Project, n.d.-c). Other protective policies include the prohibition of health insurance discrimination based on gender identity and Medicaid policies that explicitly cover gender-affirming care (Movement Advancement Project, n.d.-c,g).
Summary of Structural Determinants of Health
Structures such as sexism, racism, colonialism, discrimination against SGM individuals, and laws and policies related to reproductive justice and SGM rights have important implications for women’s health. Although many of these themes have traditionally been outside the scope of NIH’s work, NIH is increasingly emphasizing the importance of this knowledge, particularly by creating the National Institute on Minority Health and Health Disparities. To advance health for all women, it is critical to understand how outcomes are affected by sex and gender and the range of additional identities and larger structural and policy contexts that shape women’s experiences.
SDOH
Health Care Quality and Access
In Chapter 1, the committee introduced Heise and colleagues’ (2019) framework on the gender system and health (see Figure 1-3), which reflects considerations that guided the committee. It also illustrates how health inequities and outcomes result from gendered pathways to health, including gendered impacts on care access and gender-biased health systems and health research, institutions, and data collection. Access to and use of the health care system, including insurance coverage and ability to pay, is gendered (Bertakis et al., 2000; KFF, 2023b; Lopes et al., 2024). Reports of negative experiences during health care encounters and with clinicians also
vary by gender (Long et al., 2023). The knowledge with which clinicians and researchers operate to promote health and prevent and treat disease for women is also affected by the gendered health system (Mirin, 2021). Chapter 2 also discusses intersecting barriers to health care with differential effects on women.
Because of the lack of research on women’s health and female physiology commensurate with that of men, it is not possible for clinicians to provide evidence-based care for women to the same degree. This problem exists across many diseases for which diagnoses and treatments have been fitted to the presentation and disease course in men, ranging from autism to many aspects of CVD, including aortic stenosis (D’Mello et al., 2022; Merone et al., 2022; Tribouilloy et al., 2021; Wenger et al., 2022). The deficit is more stark in diseases and conditions specific to women, which continue to receive comparatively little funding (Mirin, 2021) (see Chapter 4). Thus, the evidence base for diagnosis in women is limited at best. Similarly, more studies are needed on physical health disparities, chronic conditions, and access to preventive care for TNB people to ensure clinicians have the evidence for effective treatment and intervention. Failure to invest in women’s health and sex differences research results in constrained choices for both women and clinicians, suboptimal care, and increased disease burden. Furthermore, studies indicate that the gaps in the knowledge base create an opportunity for high-impact science through funding of research on women’s health (Baird et al., 2021a,b,c, 2022).
Despite the more limited evidence base for women’s health care, women are more likely to use health care services than men and also play a central role in navigating health care services for themselves and their families (Bertakis et al., 2000; KFF, 2022b). This role of family caregiving and increased connectedness with the health care system may be an important facilitating factor for better health outcomes. While women are less likely to lack insurance coverage than men, they are more likely to have Medicaid (KFF, 2023b). Health insurance coverage is not the only indicator of health care access or quality of care. Access is also shaped by availability of care, timely appointments, geographic accessibility, affordable transportation, and health literacy to understand and carry out treatment plans (AHRQ, 2021; Cyr et al., 2019; Levy and Janke, 2016; NASEM, 2023b). The burden of health care costs is disproportionately felt by women, who spend over 18 percent more per year in out-of-pocket medical expenses than men, excluding pregnancy-related care, and more frequently delay medical care because of cost considerations (Deloitte, n.d.; Saad, 2023). Women are also more likely than men to report cost-related barriers to care, trouble paying deductibles, and medical debt (Lopes et al., 2024).
A higher share of women than men report negative experiences with a health care provider, at 38 and 32 percent, respectively (Long et al., 2023).
Among reports from women ages 18–64 who had seen a provider within the past 2 years, 29 percent had their concerns dismissed, 15 percent had a provider not believe them, and 13 percent had their doctor blame them for a health problem. Reports of negative experiences were higher among women who were low income, living with a disability or chronic condition, Black or Hispanic, and covered by Medicaid or uninsured (Long et al., 2023). Mistreatment during childbirth is common, particularly for racially and ethnically minoritized individuals, and may include loss of autonomy and being shouted at, ignored, or refused care (Vedam et al., 2019). Data illustrate significant racial inequities in maternal outcomes, often rooted in discrimination and clinician bias (Fernandez et al., 2024; Gunja et al., 2024; Tucker et al., 2007). For example, research shows that Black birthing people receive worse-quality care than White birthing people, including in measures of care process, outcomes, and perceptions (Gunja et al., 2024). In a 2023 study, 20 percent of those surveyed reported experiences of mistreatment during maternity care, with 30 percent of Black, 29 percent of Hispanic, and 27 percent of multiracial birthing people reporting mistreatment (Mohamoud et al., 2023). The most common types were receiving no response to requests for help, being shouted at or scolded, not having their physical privacy protected, being threatened with withholding treatment, and being made to accept unwanted treatment (Mohamoud et al., 2023).
How sexual orientation and gender identity affect access to care is also a critical consideration. For example, transgender people and cisgender bisexual women are almost twice as likely to report an unmet need for mental health care compared to cisgender heterosexual women (Steele et al., 2017). In addition, as discussed, laws and policies governing health care access for transgender individuals vary across the country, leaving them particularly vulnerable to lack of access to care and inequitable care. Discrimination is also a factor. Based on survey data from Lambda Legal (2010), about 70 percent of transgender and gender-nonconforming people report that they experienced one or more types of discriminatory acts in the health care setting: 26.7 percent were refused care, 20.9 percent were subjected to harsh or abusive language, and 20.3 percent were blamed for their health status (Figure 6-3). In addition, 73.0 percent reported that they believe medical personnel will treat them differently because they are transgender. These realities drive transgender people to delay or avoid care. Citing health care discrimination, more than 25 percent reported delaying or avoiding care when sick or injured, and 33 percent reported delaying preventive care. This can result in poorer health outcomes and increase the possibility of especially serious health consequences, such as late-stage cancer diagnoses, and complications of chronic conditions, such as heart disease and diabetes (Movement Advancement Project and Center for American Progress, 2024).
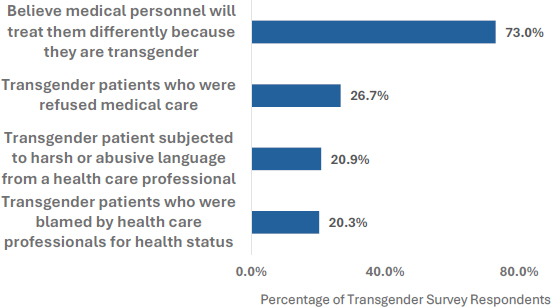
SOURCE: Data from Lambda Legal, 2010. Adapted from Movement Advancement Project and Center for American Progress, 2024.
Data Gaps
While there are many data gaps related to social determinants for women’s health in the health care realm, data gaps in pregnancy-related spheres are one striking example. A lack of robust measurements that help investigators tie community and structural drivers to pregnancy outcomes stymies advancement in understanding the upstream forces responsible for health outcomes inequities. For example, data and measures to capture domains of structural racism remain in their infancy (Headen et al., 2022). Novel approaches that combine qualitative or narrative data, geographic information systems technologies, machine learning, and social “big data” could help to fill data gaps surrounding environmental exposures, neighborhood conditions, and political and social capital that impact pregnancy and abortion outcomes. Understanding upstream social and community factors and their relationship to biological, genetic, and epigenetic processes can provide leverage points for intervention and policy change that could close gaps in pregnancy outcomes by race, ethnicity, income, or geography.
Economic Stability and Employment
Income and Poverty
Women in the United States experience persistent economic inequities that are further exacerbated among racially and ethnically minorized and SGM women (Badgett et al., 2019; Kochhar, 2023; Walker et al., 2021). Sex and gender bias result in systemic differences that leave women overrepresented in certain occupations compared to men, such as caregiving
and low-paid administrative positions (Frank et al., 2023). Poverty is more prevalent among women compared to men across all age groups (Shrider et al., 2023). Despite an overall trend toward narrowing the gender pay gap, White women still earn 83 percent of what their male counterparts do, while Asian, Black, and Hispanic women earn 93, 70, and 65 percent, respectively, of what White men do (Kochhar, 2023). Mothers and parents experience economic disparities most acutely, and 26.8 percent of female head-of-household families live in poverty (Creamer and Mohanty, 2019). Nationally, in 2021, working mothers of children under 18 earned 61.7 cents for every dollar made by working fathers (Institute for Women’s Policy Research, 2023).
Poverty rates also vary by sexual orientation and gender identity. Rates are higher among cisgender bisexual women and transgender individuals, at 29.4 percent each, than cisgender straight or lesbian women, at 17.8 and 17.9 percent, respectively (Badgett et al., 2019). As discussed, Bostock v. Clayton County affirmed that Title VII of the Civil Rights Act of 1964 protects transgender people from employment discrimination (U.S. Equal Employment Opportunity Commission, n.d.). However, it only applies to employers with 15 or more employees. Laws in just 24 states, three territories, and DC provide additional protections, leaving transgender people especially at risk of being unfairly denied employment or forced out of jobs by harassment, mistreatment, or discrimination (Movement Advancement Project, n.d.-b; Movement Advancement Project and Center for American Progress, 2024).
A clear association exists between the effect of poverty on health arising from lack of insurance or access to care. However, poverty also affects physical and mental health through other mechanisms. For example, it can reduce access to other conditions that enable good health, including safe neighborhoods and housing and healthy food (OASH, n.d.-c). These gendered pathways link socioeconomic status and health across the life course, including for conditions such as chronic pain, depression, and cardiometabolic diseases (NASEM, 2024a).
Individuals’ experiences with the criminal-legal system can also affect their economic standing. For example, incarceration is associated with a 52 percent reduction in annual earnings and with employment in low-paying jobs, which affects earnings growth for life (Craigie et al., 2020; NASEM, 2023b). Women face distinct economic challenges during and after incarceration, including specific financial issues that affect their success during reentry; for example, low and stagnant wages are a major financial barrier (Callahan et al., 2016). These data have particularly important implications for transgender individuals, who are overrepresented among incarcerated individuals because of vulnerabilities, such as family rejection and homelessness, unfair school disciplinary policies, and employment and
housing discrimination, and laws and policies such as the criminalization of sex work, drug laws, police profiling, and inaccurate/misgendering identity documents (Center for American Progress, 2016b).
Employment and the Workplace
Workplace factors, such as employer benefits and sex and age discrimination, also affect health (Goodman et al., 2021; Rochon et al., 2021). Age discrimination in the workplace is more prominent for women and can have negative consequences, including on recruitment, access to career opportunities, and pensions. Across the life course, inequity in opportunity and policies such as loss of pension contributions during maternity leave have resulted in women receiving 27 percent fewer annual pension payments than men in Organization for Economic Co-operation and Development countries (Rochon et al., 2021).
Access to workforce support and protection, such as paid sick leave, health insurance, other benefits, and minimum wage and overtime laws, is an important consideration for women’s health. Women are more likely than men to stay home to care for sick children and hold part-time jobs, which are less likely to offer paid sick leave (KFF, 2021). According to the Department of Labor, mothers provide an average of $295,000 of unpaid care for children and adults throughout their lifetime, based on the 2021 U.S. dollar value (DOL, 2023). Paid parental leave offers several economic and health benefits, including reducing the risk of poverty, especially among single mothers with lower income and education (Goodman et al., 2021). In addition, a recent analysis of state-level paid sick leave policies in three states found that it reduced the days that women experienced poor physical and mental health (Slopen, 2023).
There are also racial and ethnic inequities in employment benefits and protections, with non-Hispanic Black and Hispanic women receiving fewer weeks of paid family leave on average and less access to it through both their employers and government programs in comparison to non-Hispanic White and Asian women (Goodman et al., 2021). Racially and ethnically minoritized women are also overrepresented in some low-wage occupations that lack benefits. For example, they make up approximately two-thirds of home health workers (Yearby, 2022). Historically, laws both segregated these women, especially Black women, into these occupations and excluded them from efforts to improve worker conditions (e.g., the Fair Labor Standards Act of 1938 [FLSA]9 and the Social Security Act of 193510). Although FLSA and the Social Security Act were amended to include domestic workers
___________________
9 29 U.S.C. §201 et seq.
10 42 U.S.C. §301 et seq.
in 1974 and 1950, respectively, policies allowing home health workers to be labeled as independent contractors excludes many from FLSA protections (Kijakazi et al., 2019; Yearby, 2022).
Scholars and advocates of law reform and policies to improve economic well-being and justice for women have focused on policies such as wage equity, paid family leave, childcare, and social safety net programs, such as the Supplemental Nutrition Assistance Program, Temporary Assistance for Needy Families, the Children’s Health Insurance Program, and the Earned Income Tax Credit (NASEM, 2019a,b, 2024d). Despite progress, significant financial insecurity remains for many women and families with young children, including lack of support for those who stay home to care for children and a lack of affordable childcare and early childhood education options. In addition, the control of paid family, medical, and sick leave policies at the state and local rather than federal level introduces inequities (Goodman et al., 2021; KFF, 2021; Slopen, 2023). Consideration of factors such as poverty and the workplace in WHR, and how these policies might be improved and expanded, is needed to support the health of working women and their families.
Caregiving
While many workplace family leave policies have improved support for childcare (e.g., childbearing, childrearing), support for informal caregiving and eldercare has lagged. Because many leave policies are structured to require time to be taken consecutively, they do not account for the often acute and unanticipated needs of informal caregiving and eldercare, resulting in lost wages. Informal caregivers provide uncompensated care to ill or disabled family members and friends (Rennels et al., 2024). Women are disproportionately represented, accounting for two of every three caregivers (Sosa and Mangurian, 2023). Based on data from the Behavioral Risk Factor Surveillance System, one in four women are caregivers compared to one in five men. The data also illustrate the physical and emotional toll of caregiving, with 14.5 and 17.6 percent of caregivers reported experiencing 14 or more mentally or physically unhealthy days in the past 30 days, respectively. In addition, 36.7 percent of caregivers reported getting insufficient sleep, defined as fewer than 7 hours in a 24-hour period (CDC, n.d.-c).
Caregiving also has unique effects on racially and ethnically minoritized women. The Centers for Disease Control and Prevention estimates that one-third of AIAN adults are caregivers, and 60 percent of them are women (CDC, n.d.-b). Data from the American Association of Retired Persons shows that non-White caregivers (both men and women) provide more hours of care each week than White caregivers and experience a higher
burden of high-intensity care (AARP and National Alliance for Caregiving, 2020). For example, Black and Hispanic cancer caregivers (both men and women) spend more time, take on more tasks, and face greater financial burdens compared to their non-Hispanic White counterparts. However, they report similar or lower levels of social, emotional, and health-related burdens. Differences in social support and caregiving preparedness between racial groups partially account for the inequities in burden. To address these inequities, research and policy need to focus on alleviating the financial strain experienced by Black and Hispanic caregivers and on the lack of support services (Fenton et al., 2022).
Nurses and other health care providers often take on unpaid caregiving for family members, resulting in negative health consequences, such as shorter sleep duration and poorer sleep quality (DePasquale et al., 2019). Women working in nursing homes also experience higher perceived stress, poorer psychological well-being, and more family–work conflict than those without additional unpaid caregiving responsibilities, whether for children or elders (DePasquale et al., 2016). For conditions with a high caregiving burden, such as dementia, women reduce their work hours or tend to leave the workforce altogether because of the time required, reducing the gross domestic product (Kubendran et al., 2016). Lack of policies to support informal caregiving and eldercare also negatively affects the physician workforce caring for and conducting research on women’s health (see Chapter 8).
Social and Community Context
The social and community context influences women’s health in a number of ways. For example, strong social networks provide emotional support and practical help, such as childcare or transportation, which can alleviate stress and improve health outcomes. Women with robust social ties often experience better mental health and can better manage chronic conditions (NASEM, 2024a).
Safe neighborhoods with supportive community structures contribute to overall well-being. Civic engagement and active participation in community activities and organizations can enhance a sense of belonging and social support, leading to better mental health and overall well-being (NASEM, 2023a,b; Rippel Foundation, n.d.). Social norms and expectations regarding gender roles can affect women’s health by influencing access to health care, autonomy, and opportunities for education and employment. Conversely, norms that restrict women’s choices or access to resources can contribute to poorer health outcomes. Another crucial aspect of the social and community context is violence, which profoundly affects women’s health and is explored next.
Violence Against Women
Violence against women is common worldwide, with over 35 percent of women reporting experiences of domestic violence, abuse, and intimate and non-intimate partner sexual violence. Women experiencing violence are three-, four-, and seven-fold more likely to suffer from depression, anxiety disorders, and post-traumatic stress disorder, respectively (Oram et al., 2017).
Violence and abuse that starts in childhood can have lifelong, negative effects on a woman’s health. Advancing Research on Chronic Conditions in Women describes how early experiences of trauma, also called adverse childhood experiences (ACEs) or early life adversity and which encompass verbal, emotional, physical, and sexual abuse, lead to physiological changes that affect the development of chronic conditions in women (NASEM, 2024a). Research has described associations between such traumatic experiences and seemingly disparate conditions such as endometriosis, vulvodynia, and fibroids, which are female specific, and depression, chronic pain, heart disease, stroke, and autoimmune disease, which occur predominantly or differently in women (Felitti et al., 1998; NASEM, 2024a). Research has identified sex and gender differences in the frequency and type of trauma experienced, with women experiencing more ACEs than men (Haahr-Pedersen et al., 2020). Other studies have reported higher prevalence of ACEs in women compared to men (Haahr-Pedersen et al., 2020; Hurley et al., 2022). Further research is needed to understand precisely how trauma alters women’s mental and physical health across the life course, how gender-related social factors make women vulnerable to trauma, and how to mitigate trauma risks and the later detrimental health consequences in women (NASEM, 2024c).
Intimate partner violence (IPV) is the leading cause of injury among women and is associated with physical injuries (NASEM, 2024b). Furthermore, IPV is associated with adverse outcomes in sexual and reproductive health (including gynecologic infections, HIV/AIDS and other sexually transmitted infections, and unintended pregnancies) and mental health (such as anxiety, post-traumatic stress disorder, depression, substance misuse, suicidality, and eating disorders). Essential health care services for IPV can include universal screening paired with education, enduring safety planning centered on women’s needs, and referrals to care and support services (NASEM, 2024b).
Violence against women and Two-Spirit individuals is of large concern among AIAN people. Homicide is the seventh leading cause of death among AIAN females aged 1–54 (Petrosky et al., 2021). Native women are also 2.5 times more likely to be raped than non-Native women (Urban Indian Health Institute, n.d.). A 2011 study by the National Gay & Lesbian Task Force found that 45 percent of Two-Spirit people reported
family violence, 55 percent were harassed by shelter staff while at a shelter, and 22 percent were sexually assaulted by shelter residents or staff (Tribal Information Exchange, n.d.). Moreover, violence against AIAN women and Two-Spirit individuals is often underreported, given the lack of trust in law enforcement and jurisdictional complexities. The interplay between tribal, federal, and state jurisdictions can complicate legal responses and justice.
Transgender individuals also face high rates of violence victimization, including IPV and bias-motivated murder and violence, which has important implications for their health and well-being (Coston, 2023). Data from the 2017 and 2018 National Crime Victimization Survey demonstrate that transgender people experience nearly four times more violence than cisgender people at 86.2 victimizations per 1,000 persons compared to 21.7, and households with a transgender person have higher rates of property victimization than cisgender households at 214.1 per 1,000 households versus 108 (Flores et al., 2021). Of reported hate violence in 2017, 17 percent involved anti-transgender bias. Of 52 reports of hate violence homicides in 2017, 52 percent were against transgender or gender-nonconforming people (National Coalition of Anti-Violence Programs, 2018). Furthermore, a 2020 systematic review and meta-analysis found that transgender individuals were 2.2 and 2.5 times more likely to experience physical and sexual IPV, respectively (Peitzmeier et al., 2020). Factors such as social isolation and economic vulnerability can leave them dependent on abusive partners. The National Coalition of Anti-Violence Programs found that 33 percent of violence reported as IPV, rather than as bias motivated, involved anti-transgender bias (Coston, 2023; National Coalition of Anti-Violence Programs, 2018). It is also common for transgender individuals to experience discrimination when seeking assistance from domestic violence shelters, police, or health care providers (Center for American Progress, 2016a; Peitzmeier et al., 2020).
Women with a disability are more likely to experience IPV, including sexual and physical violence, stalking, psychological aggression, and control of reproductive or sexual health, compared to women without a disability (CDC, 2023b). Disabilities can lead to social isolation, limiting women’s access to supportive networks or resources. This isolation can make it harder for them to seek help or escape abusive situations (Anyango et al., 2023).
Violence against women profoundly affects their health outcomes, leading to both immediate and long-term consequences. The resulting physical injuries and psychological trauma contribute to a range of health issues, including chronic pain, mental health disorders, and increased susceptibility to other illnesses (Uvelli et al., 2023; Wuest et al., 2009, 2010). Systemic barriers, such as limited access to health care, stigma, and discrimination, exacerbate the effects. Addressing these challenges requires a comprehensive
approach that includes improving access to support services, enhancing legal protections, and addressing the broader SDOH that contribute to the vulnerability of affected individuals (Arcaya et al., 2024; Gehris et al., 2023; Robinette et al., 2021).
Neighborhood and Built Environment
The neighborhood and built environment significantly affect women’s health outcomes through a variety of mechanisms, encompassing both physical and social aspects (OASH, n.d.-d). For example, neighborhoods with closer proximity to health care services have improved access to preventive care, screenings, and treatment and more specialized services, such as maternal care, mental health support, or reproductive health services, and this can greatly affect women’s health (OASH, n.d.-b). In general, people in unsafe neighborhoods may experience higher levels of anxiety and stress, and the perception of safety may affect women’s willingness to engage in physical activity, seek health care, or use community resources (Gehris et al., 2023; Robinette et al., 2021). Environmental exposures and geography are additional factors with critical impacts on women’s health and will be further explored in the following sections.
Geography
Geographic location can have critical impacts on women’s health. For example, as discussed, laws and policies that affect TNB people’s health, such as those that impede or protect their ability to participate in sports, use restrooms, update identification documents in accordance with their gender identity, access health care, particularly gender-affirming care, or maintain protection from discrimination in housing or other domains, vary by state (Hohne, 2023; Movement Advancement Project, n.d.-a,b,c,d,e,f,g,h). Other examples include the effects of state-level structural sexism and variability in the expansion of Medicaid and access to abortion services on women’s health (Homan, 2019; KFF, 2023a; Margerison et al., 2020) (see Chapter 7 for more information).
In considering the impact of geography on women’s health, rurality in particular is an important factor. For rural residents, high poverty and lack of opportunity can create challenges to staying healthy, causing difficulty accessing housing, education, jobs, health care, transportation, and healthy food. Low physician density and the small scale, limited staff, and limited resources of health systems pose challenges to the management of chronic conditions, access to timely care, and access to subspecialists. Furthermore, transportation challenges can create difficulties accessing even this limited available health care (NASEM, 2017, 2021b). Data suggest that fewer rural
residents participate in clinical trials than urban residents, and they travel further to do so (Bharucha et al., 2021).
Rural women experience significant inequities compared to urban women, including higher rates of fair or poor self-reported health, unintentional injury and motor vehicle–related deaths, cerebrovascular disease deaths, suicide, cigarette smoking, obesity, difficulty with basic actions or limitation of complex activities, and incidence of cervical cancer. Additionally, fewer rural women receive recommended preventive screenings for breast and cervical cancer (ACOG Committee on Health Care for Underserved Women, 2014). In addressing gaps in women’s health, it is critical to consider these and other ways they are affected by place.
Environmental Factors and Women’s Health
Women may be at increased risk for some diseases associated with environmental exposures because of biological or behavioral differences. Health conditions such as endometriosis and uterine fibroids, reproductive health outcomes, female-specific cancers, and autoimmune diseases all have links to environmental causes (Corbett et al., 2022; Giudice, 2021; Haggerty et al., 2021; Hassan et al., 2024; Katz et al., 2016; Mallozzi et al., 2017; McCue and DeNicola, 2019; Rickard et al., 2022; Rudel et al., 2014; Stiel et al., 2016; Vallée et al., 2024; Van Loveren et al., 2001; Zlatnik, 2016).
Physiological differences between women and men significantly affect exposure, uptake, metabolism, and retention of toxic chemicals. Women’s higher body fat content facilitates the accumulation of lipophilic chemicals, which can be released during weight fluctuations or lactation. Gender-specific metabolic pathways and enzyme activity differences can result in varying internal doses and toxic chemical responses (Silbergeld and Flaws, 2002). In addition, hormonal variations influence metabolic pathways and bone physiology, altering chemical processing and storage. For example, women’s reproductive stages affect enzyme activity and bone mineral metabolism, influencing the body’s interaction with toxic substances, such as lead and mercury. These factors underscore the crucial importance of gender-specific considerations in toxicology research and risk assessment, a complexity that is often overlooked (Silbergeld and Flaws, 2002).
As a result of socioeconomic factors and traditional gender roles, women experience environmental health risks disproportionately and uniquely (Moss, 2002). For example, exposure to air pollution increases the risk of adverse outcomes in pregnancy, such as preterm birth, low birthweight, and stillbirth. Moreover, data illustrate that racially and ethnically minoritized individuals are exposed to disproportionately high levels of air pollution, including Hispanic, African American, and Asian/Pacific Islander mothers, with more adverse pregnancy outcomes related to such
exposure among Black and Hispanic people than Non-Hispanic White people (Dzekem et al., 2024). Additionally, while Black people are overall 40 percent more likely to have asthma than White people, Black women are 84 percent more likely to have asthma than Black men (NHLBI, 2023).
Additionally, spending more time at home can increase women’s exposure to contaminants in drinking water (Silbergeld and Flaws, 2002). Despite evolving gender roles, women are still more likely to be primary caregivers and homemakers, placing them at risk of exposure to indoor pollutants from various sources, including household products, building materials, and outdoor air infiltration (Folletti et al., 2017; Rousseau et al., 2022). Cooking can increase exposure to particulate matter and gases (Kashtan et al., 2024). Hobbies such as arts and crafts can also increase women’s exposure to metals in paints or jewelry-making materials (Silbergeld and Flaws, 2002).
Beauty and personal care products are known sources of potential exposure to toxic chemicals, and understanding the exposure pathway and disease risks requires further elucidation. For example, a study found toxic chemicals, such as lead and arsenic, in tampons, though some researchers have stated that these cannot leach out during use (Shearston et al., 2024). Phthalates and talc in vaginal douches and other feminine care products are associated with gynecological cancers (Zota and Shamasunder, 2017). Others have also documented the potentially carcinogenic effects of cosmetics, highlighting the need for additional research, particularly per- and polyfluoroalkyl substances in cosmetics (Balwierz et al., 2023; FDA, n.d.).
Products marketed to women for beauty, feminine hygiene, or other aspects of personal care may also contribute to racial and ethnic health disparities. Colorism, hair texture preferences, and odor discrimination can increase toxicant exposure (Zota and Shamasunder, 2017). For example, mercury in skin-lightening creams is associated with poisoning, neurotoxicity, and kidney damage. Parabens, a common ingredient in hair relaxers, are associated with precocious puberty and fibroids. Chemicals in hair relaxers marketed to Black women appear to be associated with both harmful exposures and disease risks (Zota and Shamasunder, 2017). One study that measured chemicals in hair products marketed to Black women found that root stimulators, hair lotions, and relaxers frequently contained nonylphenols and parabens, which were not always listed on the product label (Helm et al., 2018). Studies have shown a correlation between frequent and long-term use of these products and an increased risk of uterine cancer, an increased risk of breast cancer with lye-based relaxers, and increased risk of earlier menarche (Chang et al., 2022; Coogan et al., 2021; James-Todd et al., 2011; Wise et al., 2023).
Occupational hazards experienced by women include repetitive stress, exposure to violence, and exposure to solvents used in cleaning and
sterilization. Women may be at increased risk for workplace-related musculoskeletal disorders such as sprains, strains, carpal tunnel syndrome, and tendonitis (CDC, n.d.-e). In addition, in 2020, 73 percent of victims who experienced trauma from nonfatal workplace violence were women (CDC, n.d.-a). Some occupational exposures linked to jobs with a higher percentage of women are also associated with cancers that are female specific or more common in women. For example, hospital workers who sterilize medical equipment may be exposed to ethylene oxide, which is associated with breast cancer. Perchloroethylene, the main solvent in dry cleaning, may increase cervical cancer risk (CDC, n.d.-e). Women may also be less protected when they participate in traditionally male-dominated fields because of ill-fitting personal protective equipment and can face additional stressors, such as sexual harassment (CDC, n.d.-e).
Despite growing evidence linking environmental exposures to women’s health issues, significant gaps remain in understanding these complex relationships. While epidemiological studies suggest associations between environmental exposures and various health conditions in women, more research is needed to establish causal links. Multiple factors are associated with most outcomes, and the timing of the exposure, intensity, and duration also contribute. A deeper understanding of how environmental exposures at different life stages (prenatal, puberty, pregnancy, menopause transition) affect women’s health across the life-span is needed. This includes investigating potential long-term consequences of exposures during critical developmental windows. Research also needs to explore how interactions between chemicals and pollutants influence women’s health outcomes; NIH could fund this type of research.
Gaps also exist concerning the specific vulnerabilities faced by racially and ethnically minoritized, low-income, and immigrant women. These groups may experience heightened risks arising from factors such as residential segregation near pollution sources, limited access to health care, and cultural practices that increase exposure (NASEM, 2023b).
Developing and promoting safer alternatives to potentially harmful chemicals in consumer products, building materials, and personal care items is crucial to reduce women’s exposure risks. Although many are marketed as safer or greening cleaning products, few studies have confirmed that they effectively reduce exposure to toxic chemicals (Sieck et al., 2024).
Education Access and Quality
Education, as an SDOH, has an effect on health in a number of ways, including improving health literacy, access to health care, economic stability, and health behaviors. Education can drive opportunity and reproduce inequality (Zajacova and Lawrence, 2018). For example, individuals with
higher education levels generally have greater health literacy, leading to a better understanding of health information and more informed medical choices (Coughlin et al., 2020; NASEM, 2021a). Higher levels of education often correlate with increased use of preventive health services, such as screenings and vaccinations, which can lead to earlier detection and better management of conditions, better employment opportunities, and access to health insurance, improving overall health outcomes (NASEM, 2017). Conversely, poor health not only results from lower educational attainment but also can cause educational setbacks and diminished success because of recurrent absences and difficulty concentrating in class.
Associations between education and health and survival are well documented, but whether their strength depends on gender is not, with few studies on U.S. populations (Montez and Cheng, 2022; NASEM, 2017, 2019b; Raghupathi and Raghupathi, 2020). A study found that effects of education on perceived health and survival vary by gender but in contrasting ways: it significantly improves women’s self-rated health more than men’s, yet it has a greater effect on reducing men’s mortality rates (Ross et al., 2012). Some studies have pointed to important health outcomes correlated with education for women. Globally, women with higher levels of education are more likely to have better mental and physical health, including lower rates of anxiety and depression (Kondirolli and Sunder, 2022). Studies have found that enhancing women’s education leads to a decrease in their short- and long-term likelihood of psychological, physical, and sexual violence. It also reduced their chances of encountering any form of IPV and multiple forms of victimization (Villardón-Gallego et al., 2023; Weitzman, 2018).
In the United States, women are more likely than men to hold a bachelor’s degree or higher. In 2022, 39 percent of women aged 25 and older had a bachelor’s degree, compared to 36.2 percent of men in the same age group. Women also have a higher graduation rate from 4-year institutions, with 66.4 percent graduating within 4–6 years between 2015 and 2021, compared to 60.4 percent of men (WIA Report, 2022). Nevertheless, men continue to have an edge in certain professional fields, such as law, medicine, and dentistry (Nguyen Le et al., 2017). In 2022, men earned 1,869,000 professional degrees, while women earned 1,584,000 (Census Bureau, 2023). In addition, women with bachelor’s degrees in social science or business earn over $1 million less than their male counterparts over their lifetimes. This gap widens to $1.6 million for business majors with graduate degrees and exceeds $1 million for women in law and public policy with advanced degrees (Carnevale et al., 2018).
Research is required to elucidate the specific pathways and mechanisms through which education influences women’s health outcomes, including how it interacts with other SDOH and demographic factors, such as race, ethnicity, socioeconomic status, and geography.
Health Behaviors and SDOH
Another important consideration for women’s health is the interaction of SDOH and health behaviors. SDOH create the conditions that shape health behaviors, and these behaviors can influence overall health outcomes. For example, poverty can limit access to healthful food, making eating less about an individual’s choices and more about what choices are available. In addition, poverty restricts access to safe neighborhoods, potentially limiting the ability to be physically active (OASH, n.d.-c). Additionally, the built environment can significantly influence healthy behaviors and adherence to disease prevention guidelines. Factors such as access to supermarkets or grocery stores and to safe, walkable spaces for physical activity can facilitate or hinder healthy practices (Feskens et al., 2022). These challenges often disproportionately affect racially and ethnically minoritized women (Hilmers et al., 2012; NASEM, 2017; Pichardo et al., 2023). Health behaviors such as lack of physical inactivity, smoking, alcohol consumption, and poor diet can increase the risk of chronic conditions, such as diabetes, heart disease, and lung disease, thereby accounting for a significant portion of the country’s burden of chronic illness (American Public Health Association, n.d.).
There are clear differences in health behaviors between men and women. Although women have lower rates of smoking, they engage in less regular physical activity, defined as more than 75 minutes per week. In the United States, 10.1 percent of women versus 13.1 percent of men smoke tobacco, 28.3 percent of women versus 38.9 percent of men engage regularly in vigorous physical activity, and 5.2 percent of women versus 8.1 percent of men report a moderate to severe alcohol use disorder in their lifetime (CDC, n.d.-d; Grant et al., 2016; Ji et al., 2024). Although the prevalence of alcohol use disorder is lower in women, alcohol-associated liver disease is often more severe in women, and they tend to develop it with less exposure to alcohol (Kezer et al., 2021). Moreover, data suggest that SMW may exhibit poorer health behaviors, such as heavy drinking and smoking, compared to heterosexual women (Baptiste-Roberts et al., 2017).
Societal factors can heavily affect women’s health-promoting behaviors. For example, gender norms and cultural expectations uniquely shape women’s health behaviors. As noted, caregiving responsibilities often fall more heavily on women, limiting time for self-care and health-promoting activities, such as exercise, and women in lower-wage jobs often have less access to workplace wellness programs and paid sick leave, impacting health behaviors (Kelley and Gilbert, 2023). Lower education levels have been linked to higher rates of obesity and smoking in women specifically (Baheiraei et al., 2015).
In general, the effects of health behaviors and programs to modify lifestyles in women have been understudied; as noted in Chapter 5, sex differences in the levels at which specific health behaviors are most beneficial
remain understudied as well. More attention to understanding the crucial role of modifiable behaviors among women is needed within WHR. Integrating the structural and social determinants of health when studying mechanisms to improve health behaviors is needed to identify actionable interventions to improve health outcomes for women. At NIH, work on women’s health would benefit from coordination with the NIH Office of Behavioral and Social Sciences Research.
Summary of SDOH
Social factors, such as health care quality and access, economic stability and employment, violence, and environment, all uniquely impact women’s health outcomes. Without examining these factors and understanding the mechanisms by which they do so, the nation’s WHR agenda will not be adequately prepared to achieve health equity for women.
RESILIENCE
Despite the barriers that inequities pose, women have worked to improve their social and health outcomes. Resilience among women, including racially and ethnically minoritized, transgender, and SGM individuals, often manifests in various ways. For example, many racially and ethnically minoritized and LGBTQIA+ women build and rely on strong community networks that provide emotional support, advocacy, and practical resources. These networks often help individuals navigate health care systems, access services, and share information about health resources (Ceatha et al., 2021; Hudson and Romanelli, 2020). Women from minoritized communities frequently engage in advocacy and activism to address health care disparities and push for policy changes (Kumanyika et al., 2001). For example, LGBTQ activists have fought for rights such as access to gender-affirming care and protection from discrimination (Center for American Progress, 2021). Transgender and gender minority individuals often develop coping strategies and resilience through mental health support groups, therapy, and peer support (DeBower, 2024). These resources help them manage the stress of discrimination and navigate the complexities of gender-affirming care. Moreover, data suggest that SMW in states with policy protections for lesbian, gay, and bisexual individuals may have better outcomes even relative to heterosexual women (Everett et al., 2022b, 2024a).
Culture as protection for health conditions is a concept gaining widespread traction in Western research, although it has always been known to AIAN people. If colonialism is at the root of negative health outcomes, then culture is needed to heal (University of Arizona Health Sciences, n.d.). Indigenous women and communities often draw on cultural traditions and
practices to maintain health and resilience. This can include traditional healing practices, community-based health initiatives, and cultural ceremonies that promote mental and physical well-being. For example, the connection to traditional foods can be an important aspect of cultural identity and resilience (Britwum and Demont, 2022; Wehi et al., 2023). Indigenous and other researchers have pointed to asset models in research and health care that emphasize the importance of community strengths and traditional health practices as vital components of well-being (Kennedy et al., 2022; O’Keefe et al., 2023). By focusing on these assets, researchers and practitioners can leverage existing resources, cultural knowledge, and community networks to enhance health outcomes. This approach recognizes the value of traditional health practices and local expertise, fostering more inclusive and effective health care solutions that build on the resilience and resources within communities. Integrating these strengths into health research and practice at NIH can lead to more culturally relevant and sustainable interventions.
Many individuals from minoritized communities share their personal stories of overcoming health barriers through platforms such as social media, advocacy groups, and public speaking (Endometriosis Coalition, n.d.; Fibroid Foundation, n.d.; National Menopause Foundation, n.d.; PCOS Challenge, n.d.; Tight Lipped, n.d.). These stories highlight the strength and resilience within these communities.
These examples underscore the diverse and resourceful ways women demonstrate resilience in overcoming barriers to health and not only illustrate successful strategies for advancing women’s health despite adversity but also offer valuable insights for research to further enhance efforts to improve women’s health.
CONCLUDING OBSERVATIONS
The interplay among women, health, and society highlights the intricate ways social structures, cultural norms, and systemic inequalities shape women’s health outcomes. Understanding it is essential for developing evidence-based, effective interventions and policies that address not only individual health needs but also the broader societal factors that influence health. By recognizing and addressing these interconnected issues—ranging from gender-based discrimination and economic disparities to access to health care and social support—society can work toward creating structures that support women’s health needs, including filling the many research gaps highlighted in this chapter. Understanding these underlying mechanisms and how they affect health will increase the ability to achieve health equity for women. The committee’s recommendations for priority research areas, including social and structural determinants of women’s health, are in Chapter 9—see Recommendation 8.
REFERENCES
AARP (American Association of Retired Persons) and National Alliance for Caregiving. 2020. Caregiving in the United States 2020. Washington, DC: American Association of Retired Persons.
ACOG (American College of Obstetricians and Gynecologists) Committee on Health Care for Underserved Women. 2014. ACOG committee opinion no. 586: Health disparities in rural women. Obstetrics & Gynecology 123(2 Pt 1):384–388.
Adoption History Project. n.d. Indian Adoption Project. https://pages.uoregon.edu/adoption/topics/IAP.html (accessed August 23, 2024).
Agénor, M., A. E. Pérez, A. Wilhoit, F. Almeda, B. M. Charlton, M. L. Evans, S. Borrero, and S. B. Austin. 2021. Contraceptive care disparities among sexual orientation identity and racial/ethnic subgroups of U.S. women: A national probability sample study. Journal of Women’s Health 30(10):1406–1415.
Ahmed, A., D. P. Evans, J. Jackson, B. M. Meier, and C. Tomori. 2023. Dobbs v. Jackson Women’s Health: Undermining public health, facilitating reproductive coercion. Journal of Law, Medicine, & Ethics 51(3):485–489.
AHRQ (Agency for Healthcare Research and Quality). 2021. National healthcare quality & disparities reports 2021. Rockville, MD: Agency for Healthcare Research and Quality.
American Cancer Society. 2024. Cancer Facts for Lesbian and Bisexual Women. https://www.cancer.org/cancer/risk-prevention/understanding-cancer-risk/cancer-facts/cancer-facts-for-lesbian-and-bisexual-women.html (accessed August 26, 2024).
American Heart Association. 2023. Heart Health Is Sub-Optimal Among American Indian/Alaska Native Women, Supports Needed. https://newsroom.heart.org/news/heart-health-is-sub-optimal-among-american-indianalaska-native-women-supports-needed (accessed August 26, 2024).
American Public Health Association. n.d. Encourage Healthy Behaviors and Choices. https://www.apha.org/what-is-public-health/generation-public-health/our-work/healthy-choices (accessed August 26, 2024).
Anyango, C., I. Goicolea, and F. Namatovu. 2023. Women with disabilities’ experiences of intimate partner violence: A qualitative study from Sweden. BMC Women’s Health 23(1):381.
Arcaya, M. C., I. G. Ellen, and J. Steil. 2024. Neighborhoods and health: Interventions at the neighborhood level could help advance health equity. Health Affairs 43(2):156–163.
Badgett, M., S. K. Choi, and B. D. Wilson. 2019. LGBT poverty in the United States: A study of differences between sexual orientation and gender identity groups. Los Angeles, CA: Williams Institute.
Baheiraei, A., F. Bakouei, E. Mohammadi, A. Montazeri, and M. Hosseni. 2015. The social determinants of health in association with women’s health status of reproductive age: A population-based study. Iranian Journal of Public Health 44(1):119–129.
Baird, M. D., M. A. Zaber, A. Chen, A. W. Dick, C. E. Bird, M. Waymouth, G. Gahlon, D. D. Quigley, H. Al-Ibrahim, and L. Frank. 2021a. The WHAM report: The case to fund women’s health research: An economic and societal impact analysis. Santa Monica, CA: RAND Corporation.
Baird, M. D., M. A. Zaber, A. W. Dick, C. E. Bird, A. Chen, M. Waymouth, G. Gahlon, D. D. Quigley, H. Al-Ibrahim, and L. Frank. 2021b. Societal impact of research funding for women’s health in Alzheimer’s disease and Alzheimer’s disease-related dementias. Santa Monica, CA: RAND Corporation.
Baird, M. D., M. A. Zaber, A. W. Dick, C. E. Bird, A. Chen, M. Waymouth, G. Gahlon, D. D. Quigley, H. Al-Ibrahim, and L. Frank. 2021c. Societal impact of research funding for women’s health in coronary artery disease. Santa Monica, CA: RAND Corporation.
Baird, M. D., M. A. Zaber, A. Chen, A. W. Dick, C. E. Bird, M. Waymouth, G. Gahlon, D. D. Quigley, H. Al-Ibrahim, and L. Frank. 2022. Societal impact of research funding for women’s health in rheumatoid arthritis. Santa Monica, CA: RAND Corporation.
Balistreri, K. S. 2024. Structural sexism and breastfeeding in the United States, 2016–2021. Maternal and Child Health Journal 28(3):431–437.
Balwierz, R., P. Biernat, A. Jasińska-Balwierz, D. Siodłak, A. Kusakiewicz-Dawid, A. Kurek-Górecka, P. Olczyk, and W. Ochędzan-Siodłak. 2023. Potential carcinogens in makeup cosmetics. International Journal of Environmental Research and Public Health 20(6).
Baptiste-Roberts, K., E. Oranuba, N. Werts, and L. V. Edwards. 2017. Addressing health care disparities among sexual minorities. Obstetrics and Gynecology Clinics of North America 44(1):71–80.
Beccia, A. L., S. B. Austin, J. Baek, M. Agénor, S. Forrester, E. Y. Ding, W. M. Jesdale, and K. L. Lapane. 2022. Cumulative exposure to state-level structural sexism and risk of disordered eating: Results from a 20-year prospective cohort study. Social Science & Medicine 301:114956.
Beccia, A. L., M. Agénor, J. Baek, E. Y. Ding, K. L. Lapane, and S. B. Austin. 2024. Methods for structural sexism and population health research: Introducing a novel analytic framework to capture life-course and intersectional effects. Social Science & Medicine 351:116804.
Berger, M., and Z. Sarnyai. 2015. “More than skin deep”: Stress neurobiology and mental health consequences of racial discrimination. Stress 18(1):1–10.
Bertakis, K. D., R. Azari, L. J. Helms, E. J. Callahan, and J. A. Robbins. 2000. Gender differences in the utilization of health care services. Journal of Family Practice 49(2):147–152.
Bharucha, A. E., C. I. Wi, S. G. Srinivasan, H. Choi, P. H. Wheeler, J. R. Stavlund, D. A. Keller, K. R. Bailey, and Y. J. Juhn. 2021. Participation of rural patients in clinical trials at a multisite academic medical center. Journal of Clinical and Translational Science 5(1):e190.
Biggs, M. A., R. Schroeder, M. T. Casebolt, B. I. Laureano, R. L. Wilson-Beattie, L. J. Ralph, S. Kaller, A. Adler, and M. W. Gichane. 2023. Access to reproductive health services among people with disabilities. JAMA Network Open 6(11):e2344877.
Bleich, S. N., J. F. Figueroa, and M. Minow. 2024. Institutional efforts to address legacies of slavery—implications for the health care system. JAMA Health Forum 5(3):e240785.
Britwum, K., and M. Demont. 2022. Food security and the cultural heritage missing link. Global Food Security 35:100660.
Brooks, V. R. 1981. Minority stress and lesbian women. Lexington, MA: Lexington Books.
Brown-Rice, K. 2013. Examining the theory of historical trauma among Native Americans. Professional Counselor 3(3):117–130.
Brydon, M. 2022. Weight bias: A consideration for medical radiation sciences. Journal of Medical Imaging and Radiation Sciences 53(4):534–537.
Callahan, S., L. A. Jason, and L. Robinson. 2016. Reducing economic disparities for female offenders: The Oxford House model. Alcoholism Treatment Quarterly 34(3):292–302.
Carnevale, A. P., N. Smith, and A. Gulish. 2018. Women can’t win: Despite making educational gains and pursuing high-wage majors, women still earn less than men. Washington, DC: Georgetown University McCourt School of Public Policy.
Carroll, S. R., M. Suina, M. B. Jäger, J. Black, S. Cornell, A. A. Gonzales, M. Jorgensen, N. L. Palmanteer-Holder, J. S. De La Rosa, and N. I. Teufel-Shone. 2022. Reclaiming Indigenous health in the U.S.: Moving beyond the social determinants of health. International Journal of Environmental Research and Public Health 19(12).
CDC (Centers for Disease Control and Prevention). n.d.-a. About Workplace Violence. https://www.cdc.gov/niosh/violence/about/index.html (accessed October 21, 2024).
CDC. n.d.-b. Caregiving Among American Indian/Alaska Native Adults. https://www.cdc.gov/aging/data/infographic/2018/american-indian-adults-caregiving.html (accessed August 23, 2024).
CDC. n.d.-c. Caregiving for Family and Friends—A Public Health Issue. https://www.cdc.gov/aging/caregiving/pdf/caregiver-brief-508.pdf (accessed August 9, 2024).
CDC. n.d.-d. Current Cigarette Smoking Among Adults in the United States. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm (accessed August 26, 2024).
CDC. n.d.-e. Women’s Safety and Health Issues at Work. https://www.cdc.gov/niosh/docs/2001-123/default.html (accessed August 26, 2024).
CDC. 2023a. Cancer in American Indian and Alaska Native people. https://www.cdc.gov/cancer/research/cancer-in-american-indian-and-alaska-native-people.html (accessed August 26, 2024).
CDC. 2023b. Supporting Women with Disabilities to Achieve Optimal Health. https://www.cdc.gov/womens-health/features/women-disabilities.html (accessed August 26, 2024).
CDC. 2024. Pregnancy-Related Deaths Among American Indian or Alaska Native Persons: Data from Maternal Mortality Review Committees in 38 U.S. States, 2020. https://www.cdc.gov/maternal-mortality/php/data-research/aian-mmrc/index.html (accessed August 22, 2024).
Ceatha, N., A. C. C. Koay, C. Buggy, O. James, L. Tully, M. Bustillo, and D. Crowley. 2021. Protective factors for LGBTI+ youth wellbeing: A scoping review underpinned by recognition theory. International Journal of Environmental Research and Public Health 18(21).
Census Bureau. 2023. Educational Attainment in the United States: 2022, Table 2. https://www.census.gov/data/tables/2022/demo/educational-attainment/cps-detailed-tables.html (accessed August 26, 2024).
Center for American Progress. 2016a. Discrimination Against Transgender Women Seeking Access to Homeless Shelters. https://www.americanprogress.org/article/discrimination-against-transgender-women-seeking-access-to-homeless-shelters/ (accessed August 23, 2024).
Center for American Progress. 2016b. Unjust: How the broken criminal justice system fails LGBT people of color. Washington, DC: Center for American Progress.
Center for American Progress. 2021. Improving the lives and rights of LGBTQ people in America: A road map for the Biden administration. Washington, DC: Center for American Progress.
Chang, C.-J., K. M. O’Brien, A. P. Keil, S. A. Gaston, C. L. Jackson, D. P. Sandler, and A. J. White. 2022. Use of straighteners and other hair products and incident uterine cancer. Journal of the National Cancer Institute 114(12):1636–1645.
Charlton, B. M., M. L. Hatzenbuehler, H. J. Jun, V. Sarda, A. R. Gordon, J. R. G. Raifman, and S. B. Austin. 2019. Structural stigma and sexual orientation-related reproductive health disparities in a longitudinal cohort study of female adolescents. Journal of Adolescence 74:183–187.
Charlton, B. M., B. G. Everett, A. Light, R. K. Jones, E. Janiak, A. J. Gaskins, J. E. Chavarro, H. Moseson, V. Sarda, and S. B. Austin. 2020. Sexual orientation differences in pregnancy and abortion across the lifecourse. Women’s Health Issues 30(2):65–72.
Chen, S., and A. B. Mallory. 2021. The effect of racial discrimination on mental and physical health: A propensity score weighting approach. Social Science & Medicine 285:114308.
Chinn, J. J., I. K. Martin, and N. Redmond. 2021. Health equity among Black women in the United States. Journal of Women’s Health 30(2):212–219.
Coogan, P. F., L. Rosenberg, J. R. Palmer, Y. C. Cozier, Y. M. Lenzy, and K. A. Bertrand. 2021. Hair product use and breast cancer incidence in the Black Women’s Health study. Carcinogenesis 42(7):924–930.
Corbett, G. A., S. Lee, T. J. Woodruff, M. Hanson, M. Hod, A. M. Charlesworth, L. Giudice, J. Conry, and F. M. McAuliffe. 2022. Nutritional interventions to ameliorate the effect of endocrine disruptors on human reproductive health: A semi-structured review from FIGO. International Journal of Gynecology & Obstetrics 157(3):489–501.
Coston, B. E. 2023. Looking back: Intimate partner violence in transgender populations. American Journal of Public Health 113(5):474–476.
Coughlin, S. S., M. Vernon, C. Hatzigeorgiou, and V. George. 2020. Health literacy, social determinants of health, and disease prevention and control. Journal of Environmental Health Science 6(1).
Craigie, T. A., A. Grawert, and C. Kimble. 2020. Conviction, imprisonment, and lost earnings: How involvement with the criminal justice system deepens inequality. New York: Brennan Center for Justice.
Creamer, J., and A. Mohanty. 2019. Poverty Rate for People in Female-Householder Families Lowest on Record—U.S. Poverty Rate Drops to 11.8% in 2018. https://www.census.gov/library/stories/2019/09/poverty-rate-for-people-in-female-householder-families-lowest-on-record.html (accessed August 23, 2024).
Cree, R. A., C. A. Okoro, M. M. Zack, and E. Carbone. 2020. Frequent mental distress among adults, by disability status, disability type, and selected characteristics—United States, 2018. MMWR 69(36):1238–1243.
Cunningham, G. B., and P. Wicker. 2024. Sexual harassment and implicit gender-career biases negatively impact women’s life expectancy in the U.S.: A state-level analysis, 2011–2019. BMC Public Health 24(1):1115.
Cyr, M. E., A. G. Etchin, B. J. Guthrie, and J. C. Benneyan. 2019. Access to specialty healthcare in urban versus rural U.S. populations: A systematic literature review. BMC Health Services Research 19(1):974.
D’Mello, A. M., I. R. Frosch, C. E. Li, A. L. Cardinaux, and J. D. E. Gabrieli. 2022. Exclusion of females in autism research: Empirical evidence for a “leaky” recruitment-to-research pipeline. Autism Research 15(10):1929–1940.
Daniel, M. 2021. The social movement for reproductive justice: Emergence, intersectional strategies, and theory building. Sociology Compass 15(8):e12907.
DeBower, J. 2024. Worldbuilding: A theory of resilience in transgender and gender expansive young people. New York: Social Welfare, City University of New York.
Deloitte. n.d. Closing the Cost Gap: Strategies to Advance Women’s Health Equity. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/womens-health-equity-disparities.html?utm_source=newsletter&utm_medium=email&utm_campaign=newsletter_axiosvitals&stream=top (accessed August 23, 2024).
DePasquale, N., K. D. Davis, S. H. Zarit, P. Moen, L. B. Hammer, and D. M. Almeida. 2016. Combining formal and informal caregiving roles: The psychosocial implications of double- and triple-duty care. Journals of Gerontology: Psychological Sciences 71(2):201–211.
DePasquale, N., M. J. Sliwinski, S. H. Zarit, O. M. Buxton, and D. M. Almeida. 2019. Unpaid caregiving roles and sleep among women working in nursing homes: A longitudinal study. Gerontologist 59(3):474–485.
Diaz-Thomas, A. M., S. H. Golden, D. M. Dabelea, A. Grimberg, S. N. Magge, J. D. Safer, D. E. Shumer, and F. C. Stanford. 2023. Endocrine health and health care disparities in the pediatric and sexual and gender minority populations: An Endocrine Society scientific statement. Journal of Clinical Endocrinology & Metabolism 108(7):1533–1584.
DOL (Department of Labor). 2023. Readout: U.S. Department of Labor Report Finds Impact of Caregiving on Mother’s Wages Reduces Lifetime Earnings by 15 Percent. https://www.dol.gov/newsroom/releases/wb/wb20230511#:~:text=The%20estimated%20employment-related%20costs%20for%20mothers%20providing%20unpaid,which%20also%20creates%20a%20reduction%20in%20retirement%20income. (accessed August 23, 2024).
Dolezsar, C. M., J. J. McGrath, A. J. M. Herzig, and S. B. Miller. 2014. Perceived racial discrimination and hypertension: A comprehensive systematic review. Health Psychology 33(1):20–34.
Dongarwar, D., V. Mercado-Evans, S. Adu-Gyamfi, M.-L. Laracuente, and H. M. Salihu. 2022. Racial/ethnic disparities in infertility treatment utilization in the U.S., 2011–2019. Systems Biology in Reproductive Medicine 68(3):180–189.
Dore, E. C., S. Shrivastava, and P. Homan. 2024. Structural sexism and preventive health care use in the United States. Journal of Health and Social Behavior 65(1):2–19.
Dzekem, B. S., B. Aschebrook-Kilfoy, and C. O. Olopade. 2024. Air pollution and racial disparities in pregnancy outcomes in the United States: A systematic review. Journal of Racial and Ethnic Health Disparities 11(1):535–544.
Edwards-Gayfield, P. n.d. Weight Stigma. https://www.nationaleatingdisorders.org/weight-stigma/ (accessed October 20, 2024).
Eliason, E. L. 2020. Adoption of Medicaid expansion is associated with lower maternal mortality. Women’s Health Issues 30(3):147–152.
Eltoukhi, H. M., M. N. Modi, M. Weston, A. Y. Armstrong, and E. A. Stewart. 2014. The health disparities of uterine fibroid tumors for African American women: A public health issue. American Journal of Obstetrics & Gynecology 210(3):194–199.
Endometriosis Coalition. n.d. The Endo Co: What We Do. https://www.theendo.co/what-we-do (accessed August 27, 2024).
Everett, B. G., and M. Agénor. 2023. Sexual orientation-related nondiscrimination laws and maternal hypertension among Black and White U.S. Women. Journal of Women’s Health 32(1):118–124.
Everett, B. G., M. A. Kominiarek, S. Mollborn, D. E. Adkins, and T. L. Hughes. 2019. Sexual orientation disparities in pregnancy and infant outcomes. Maternal and Child Health Journal 23(1):72–81.
Everett, B. G., A. Limburg, P. Homan, and M. M. Philbin. 2022a. Structural heteropatriarchy and birth outcomes in the United States. Demography 59(1):89–110.
Everett, B. G., A. Limburg, S. McKetta, and M. L. Hatzenbuehler. 2022b. State-level regulations regarding the protection of sexual minorities and birth outcomes: Results from a population-based cohort study. Psychosomatic Medicine 84(6):658–668.
Everett, B. G., Z. Bergman, B. M. Charlton, and V. Barcelona. 2024a. Sexual orientation-specific policies are associated with prenatal care use in the first trimester among sexual minority women: Results from a prospective cohort study. Annals of Behavioral Medicine 58(9):594–602.
Everett, B. G., M. M. Philbin, and P. Homan. 2024b. Structural heteropatriarchy and maternal cardiovascular morbidities. Social Science & Medicine 351:116434.
FDA (Food and Drug Administration). n.d. Per and Polyfluoroalkyl Substances (PFAS) in Cosmetics. https://www.fda.gov/cosmetics/cosmetic-ingredients/and-polyfluoroalkyl-substances-pfas-cosmetics (accessed August 26, 2024).
Felitti, V. J., R. F. Anda, D. Nordenberg, D. F. Williamson, A. M. Spitz, V. Edwards, M. P. Koss, and J. S. Marks. 1998. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine 14(4):245–258.
Fenton, A., K. A. Ornstein, P. Dilworth-Anderson, N. L. Keating, E. E. Kent, K. Litzelman, A. C. Enzinger, J. H. Rowland, and A. A. Wright. 2022. Racial and ethnic disparities in cancer caregiver burden and potential sociocultural mediators. Supportive Care in Cancer 30(11):9625–9633.
Fernandez, H., M. Ayo-Vaughan, L. C. Zephyrin, and R. Block, Jr. 2024. Revealing disparities: Health care workers’ observations of discrimination against patients. New York: The Commonwealth Fund.
Feskens, E. J. M., R. Bailey, Z. Bhutta, H. K. Biesalski, H. Eicher-Miller, K. Krämer, W. H. Pan, and J. C. Griffiths. 2022. Women’s health: Optimal nutrition throughout the lifecycle. European Journal of Nutrition 61(Suppl 1):1–23.
Fibroid Foundation. n.d. Fibroid Foundation: About Us. https://www.fibroidfoundation.org/about/ (accessed August 27, 2024).
Flores, A. R., I. H. Meyer, L. Langton, and J. L. Herman. 2021. Gender identity disparities in criminal victimization: National crime victimization survey, 2017–2018. American Journal of Public Health 111(4):726–729.
Folletti, I., A. Siracusa, and G. Paolocci. 2017. Update on asthma and cleaning agents. Current Opinion in Allergy and Clinical Immunology 17(2):90–95.
Frank, J., C. Mustard, P. Smith, A. Siddiqi, Y. Cheng, A. Burdorf, and R. Rugulies. 2023. Work as a social determinant of health in high-income countries: Past, present, and future. Lancet 402(10410):1357–1367.
Friedman, C. 2024. Disparities in social determinants of health amongst people with disabilities. International Journal of Disability, Development and Education 71(1):101–117.
Gehris, J. S., A. L. Oyeyemi, M. L. Baishya, S. C. Roth, and M. Stoutenberg. 2023. The role of physical activity in the relationship between exposure to community violence and mental health: A systematic review. Preventive Medicine Reports 36:102509.
Geronimus, A. T., M. Hicken, D. Keene, and J. Bound. 2006. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health 96(5):826–833.
Giudice, L. C. 2021. Environmental impact on reproductive health and risk mitigating strategies. Current Opinion in Obstetrics and Gynecology 33(4):343–349.
Goldman, M. 2024. States Are Limiting Gender-Affirming Care for Adults, Too. https://www.axios.com/2024/01/10/trans-care-adults-red-states (accessed August 23, 2024).
Gonzalo-Encabo, P., N. Sami, R. L. Wilson, D. W. Kang, S. Ficarra, and C. M. Dieli-Conwright. 2023. Exercise as medicine in cardio-oncology: Reducing health disparities in Hispanic and Latina breast cancer survivors. Current Oncology Reports 25(11):1237–1245.
Goodman, J. M., C. Williams, and W. H. Dow. 2021. Racial/ethnic inequities in paid parental leave access. Health Equity 5(1):738–749.
Grant, B. F., T. D. Saha, W. J. Ruan, R. B. Goldstein, S. P. Chou, J. Jung, H. Zhang, S. M. Smith, R. P. Pickering, B. Huang, and D. S. Hasin. 2016. Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions—III. JAMA Psychiatry 73(1):39–47.
Greer, T., and J. L. Lemacks. 2024. The medicine wheel as a public health approach to lifestyle management interventions for indigenous populations in North America. Frontiers in Public Health 12:1392517.
Gunja, M. Z., E. D. Gumas, R. Masitha, and L. C. Zephyrin. 2024. Insights into the U.S. maternal mortality crisis: An international comparison. New York: The Commonwealth Fund.
Haahr-Pedersen, I., C. Perera, P. Hyland, F. Vallières, D. Murphy, M. Hansen, P. Spitz, P. Hansen, and M. Cloitre. 2020. Females have more complex patterns of childhood adversity: Implications for mental, social, and emotional outcomes in adulthood. European Journal of Psychotraumatology 11(1):1708618.
Haggerty, D. K., K. Upson, D. C. Pacyga, J. E. Franko, J. M. Braun, and R. S. Strakovsky. 2021. Reproductive toxicology: Pregnancy exposure to endocrine disrupting chemicals: Implications for women’s health. Reproduction 162(5):F169–F180.
Harlow, S. D., S.-A. M. Burnett-Bowie, G. A. Greendale, N. E. Avis, A. N. Reeves, T. R. Richards, and T. T. Lewis. 2022. Disparities in reproductive aging and midlife health between Black and White women: The study of Women’s Health Across the Nation (SWAN). Women’s Midlife Health 8(1):3.
Hassan, S., A. Thacharodi, A. Priya, R. Meenatchi, T. A. Hegde, T. R, H. T. Nguyen, and A. Pugazhendhi. 2024. Endocrine disruptors: Unravelling the link between chemical exposure and women’s reproductive health. Environmental Research 241:117385.
Hatzenbuehler, M. L., and K. A. McLaughlin. 2014. Structural stigma and hypothalamic-pituitary-adrenocortical axis reactivity in lesbian, gay, and bisexual young adults. Annals of Behavioral Medicine 47(1):39–47.
Headen, I. E., M. A. Elovitz, A. N. Battarbee, J. O. Lo, and M. P. Debbink. 2022. Racism and perinatal health inequities research: Where we have been and where we should go. American Journal of Obstetrics & Gynecology 227(4):560–570.
Heise, L., M. E. Greene, N. Opper, M. Stavropoulou, C. Harper, M. Nascimento, D. Zewdie, G. L. Darmstadt, M. E. Greene, S. Hawkes, L. Heise, S. Henry, J. Heymann, J. Klugman, R. Levine, A. Raj, and G. Rao Gupta. 2019. Gender inequality and restrictive gender norms: Framing the challenges to health. Lancet 393(10189):2440–2454.
Helm, J. S., M. Nishioka, J. G. Brody, R. A. Rudel, and R. E. Dodson. 2018. Measurement of endocrine disrupting and asthma-associated chemicals in hair products used by Black women. Environmental Research 165:448–458.
HHS (Department of Health and Human Services). 2024. Section 1557 of the Patient Protection and Affordable Care Act. https://www.hhs.gov/civil-rights/for-individuals/section-1557/index.html (accessed August 27, 2024).
Hicken, M. T., H. Lee, J. Morenoff, J. S. House, and D. R. Williams. 2014. Racial/ethnic disparities in hypertension prevalence: Reconsidering the role of chronic stress. American Journal of Public Health 104(1):117–123.
Higgins, J. A., E. Carpenter, B. G. Everett, M. Z. Greene, S. Haider, and C. E. Hendrick. 2019. Sexual minority women and contraceptive use: Complex pathways between sexual orientation and health outcomes. American Journal of Public Health 109(12):1680–1686.
Hilmers, A., D. C. Hilmers, and J. Dave. 2012. Neighborhood disparities in access to healthy foods and their effects on environmental justice. American Journal of Public Health 102(9):1644–1654.
Hing, A. K., T. Chantarat, S. Fashaw-Walters, S. L. Hunt, and R. R. Hardeman. 2024. Instruments for racial health equity: A scoping review of structural racism measurement, 2019–2021. Epidemiologic Reviews 46(1):1–26.
Hohne, S. 2023. How to win the war on 100 fronts: What caused the rise of anti-trans bills and how to defeat them. Georgetown Journal of Gender and the Law XXV(1).
Homan, P. 2019. Structural sexism and health in the United States: A new perspective on health inequality and the gender system. American Sociological Review 84(3):486–516.
Homan, P. 2021. Sexism and health: Advancing knowledge through structural and intersectional approaches. American Journal of Public Health 111(10):1725–1727.
Howell, E. A. 2018. Reducing disparities in severe maternal morbidity and mortality. Clinical Obstetrics and Gynecology 61(2):387–399.
Hudson, K. D., and M. Romanelli. 2020. “We are powerful people”: Health-promoting strengths of LGBTQ communities of color. Qualitative Health Research 30(8):1156–1170.
Hurley, L., A. Stillerman, J. Feinglass, and C. Percheski. 2022. Adverse childhood experiences among reproductive age women: Findings from the 2019 Behavioral Risk Factor Surveillance System. Women’s Health Issues 32(5):517–525.
Institute for Women’s Policy Research. 2023. State by state, mothers are paid much less than fathers: The gender wage gap between mothers and fathers by state and by race and ethnicity. Washington, DC: Institute for Women’s Policy Research.
IOM (Institute of Medicine). 2013. Leveraging culture to address health inequalities: Examples from Native communities: Workshop summary. Edited by K. M. Anderson and S. Olson. Washington, DC: The National Academies Press.
Ives-Rublee, M., and A. Neal. 2024. Eliminating Barriers to Employment for Disabled Women. https://www.americanprogress.org/article/playbook-for-the-advancement-of-women-in-the-economy/eliminating-barriers-to-employment-for-disabled-women/#:~:text=Disabled%20women%20face%20employment%20gaps,disabled%20men%2C%20at%2024.8%20percent (accessed August 26, 2024).
Jahn, J. L., D. Zubizarreta, J. T. Chen, B. L. Needham, G. Samari, A. J. McGregor, M. Daugherty, Douglas, S. B. Austin, and M. Agénor. 2023. Legislating inequity: Structural racism in groups of state laws and associations with premature mortality rates. Health Affairs 42(10):1325–1333.
James-Todd, T., M. B. Terry, J. Rich-Edwards, A. Deierlein, and R. Senie. 2011. Childhood hair product use and earlier age at menarche in a racially diverse study population: A pilot study. Annals of Epidemiology 21(6):461–465.
Ji, H., M. Gulati, T. Y. Huang, A. C. Kwan, D. Ouyang, J. E. Ebinger, K. Casaletto, K. L. Moreau, H. Skali, and S. Cheng. 2024. Sex differences in association of physical activity with all-cause and cardiovascular mortality. Journal of the American College of Cardiology 83(8):783–793.
Kashtan, Y., M. Nicholson, C. J. Finnegan, Z. Ouyang, A. Garg, E. D. Lebel, S. T. Rowland, D. R. Michanowicz, J. Herrera, K. C. Nadeau, and R. B. Jackson. 2024. Nitrogen dioxide exposure, health outcomes, and associated demographic disparities due to gas and propane combustion by U.S. stoves. Science Advances 10(18):eadm8680.
Katon, J. G., T. C. Plowden, and E. E. Marsh. 2023. Racial disparities in uterine fibroids and endometriosis: A systematic review and application of social, structural, and political context. Fertility and Sterility 119(3):355–363.
Katz, T. A., Q. Yang, L. S. Treviño, C. L. Walker, and A. Al-Hendy. 2016. Endocrine-disrupting chemicals and uterine fibroids. Fertility and Sterility 106(4):967–977.
Kelley, J. A., and M. Gilbert. 2023. Structural sexism across the life course: How social inequality shapes women’s later-life health. In A Life Course Approach to Women’s Health, edited by G. Mishra, R. Hardy, and D. Kuh. Oxford, UK: Oxford University Press. Pp. 327–342.
Kennedy, A., A. Sehgal, J. Szabo, K. McGowan, G. Lindstrom, P. Roach, L. L. Crowshoe, and C. Barnabe. 2022. Indigenous strengths-based approaches to healthcare and health professions education—recognising the value of elders’ teachings. Health Education Journal 81(4):423–438.
Kezer, C. A., D. A. Simonetto, and V. H. Shah. 2021. Sex differences in alcohol consumption and alcohol-associated liver disease. Mayo Clinic Proceedings 96(4):1006–1016.
KFF. n.d. How History Has Shaped Racial and Ethnic Health Disparities. https://www.kff.org/how-history-has-shaped-racial-and-ethnic-health-disparities-a-timeline-of-policies-and-events/ (accessed August 25, 2024).
KFF. 2021. Paid Leave in the U.S. https://www.kff.org/womens-health-policy/fact-sheet/paid-leave-in-u-s/ (accessed August 23, 2024).
KFF. 2022a. Racial Disparities in Maternal and Infant Health: Current Status and Efforts to Address Them. https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-disparities-in-maternal-and-infant-health-current-status-and-efforts-to-address-them/ (accessed August 22, 2024).
KFF. 2022b. Workplace Benefits and Family Health Care Responsibilities: Key Findings from the 2022 KFF Women’s Health Survey. https://www.kff.org/womens-health-policy/issue-brief/workplace-benefits-and-family-health-care-responsibilities-key-findings-from-the-2022-kff-womens-health-survey/ (accessed August 25, 2024).
KFF. 2023a. What Does the Recent Literature Say About Medicaid Expansion?: Impacts on Sexual and Reproductive Health. https://www.kff.org/medicaid/issue-brief/what-does-the-recent-literature-say-about-medicaid-expansion-impacts-on-sexual-and-reproductive-health/ (accessed October 17, 2024).
KFF. 2023b. Women’s Health Insurance Coverage. https://www.kff.org/womens-health-policy/fact-sheet/womens-health-insurance-coverage/ (accessed August 25, 2024).
KFF. 2024. Abortion in the United States Dashboard. https://www.kff.org/womens-health-policy/dashboard/abortion-in-the-u-s-dashboard/ (accessed August 15, 2024).
Kijakazi, K., K. Smith, and C. Runes. 2019. African American economic security and the role of Social Security. Washington, DC: Urban Institute.
Kochhar, R. 2023. The Enduring Grip of the Gender Pay Gap. https://www.pewresearch.org/social-trends/2023/03/01/the-enduring-grip-of-the-gender-pay-gap/%23:~:text=Gender%20pay%20gap%20differs%20widely%20by%20race%20and%20ethnicity,-Looking%20across%20racial&text=In%202022%2C%20Black%20women%20earned,%2C%20making%2 (accessed August 23, 2024).
Komro, K. A., S. Markowitz, M. D. Livingston, and A. C. Wagenaar. 2019. Effects of state-level earned income tax credit laws on birth outcomes by race and ethnicity. Health Equity 3(1):61–67.
Kondirolli, F., and N. Sunder. 2022. Mental health effects of education. Health Economics 31(Suppl 2):22–39.
Krieger, N. 2001. Theories for social epidemiology in the 21st century: An ecosocial perspective. International Journal of Epidemiology 30(4):668–677.
Krieger, N. 2014. Discrimination and health inequities. International Journal of Social Determinants of Health and Health Services 44(4):643–710.
Kubendran, S., R. DeVol, and A. Chatterjee. 2016. The price women pay for dementia: Strategies to ease gender disparity and economic costs. Santa Monica, CA: Milken Institute.
Kukielka, E. 2020. How safety is compromised when hospital equipment is a poor fit for patients who are obese. Patient Safety 2(1):48–56.
Kumanyika, S. K., C. B. Morssink, and M. Nestle. 2001. Minority women and advocacy for women’s health. American Journal of Public Health 91(9):1383–1388.
Kwon, S. C., R. Kabir, and A. Saadabadi. 2024. Mental health challenges in caring for American Indians and Alaska Natives. In Statpearls. Treasure Island, FL: StatPearls Publishing.
Lambda Legal. 2010. When Health Care Isn’t Caring: Lambda Legal’s Survey of Discrimination Against LGBT People and People with HIV. http://www.lambdalegal.org/sites/default/files/publications/downloads/whcic-report_when-health-care-isnt-caring.pdf (accessed November 18, 2024).
Larson, K. C. 2021. Mississippi appendectomy. In Walk with me: A biography of Fannie Lou Hamer. Oxford, UK: Oxford University Press. Pp. 35–49.
Lawrence, B. J., D. Kerr, C. M. Pollard, M. Theophilus, E. Alexander, D. Haywood, and M. O’Connor. 2021. Weight bias among health care professionals: A systematic review and meta-analysis. Obesity 29(11):1802–1812.
Lawrence, J. 2000. The Indian Health Service and the sterilization of Native American women. American Indian Quarterly 24(3):400–419.
Levy, H., and A. Janke. 2016. Health literacy and access to care. Journal of Health Communication 21(Suppl 1):43–50.
Long, M., B. Frederiksen, U. Ranji, K. Diep, and A. Salganicoff. 2023. Women’s Experiences with Provider Communication and Interactions in Health Care Settings: Findings from the 2022 KFF Women’s Health Survey. https://www.kff.org/womens-health-policy/issue-brief/womens-experiences-with-provider-communication-interactions-health-care-settings-findings-from-2022-kff-womens-health-survey/ (accessed August 20, 2024).
Lopes, L., A. Montero, M. Presiado, and L. Hamel. 2024. Americans’ Challenges with Health Care Costs. https://www.kff.org/health-costs/issue-brief/americans-challenges-with-health-care-costs/ (accessed August 8, 2024).
Lopez, I. 2008. Matters of choice: Puerto Rican women’s struggle for reproductive freedom. New Brunswick, NJ and London: Rutgers University Press.
Mallozzi, M., C. Leone, F. Manurita, F. Bellati, and D. Caserta. 2017. Endocrine disrupting chemicals and endometrial cancer: An overview of recent laboratory evidence and epidemiological studies. International Journal of Environmental Research and Public Health 14(3).
Margerison, C. E., C. L. MacCallum, J. Chen, Y. Zamani-Hank, and R. Kaestner. 2020. Impacts of Medicaid expansion on health among women of reproductive age. American Journal of Preventive Medicine 58(1):1–11.
Mason, A., E. Crowe, B. Haragan, S. Smith, and A. Kyriakou. 2023. Gender dysphoria in young people: A model of chronic stress. Hormone Research in Paediatrics 96(1): 54–65.
Matin, B. K., H. J. Williamson, A. K. Karyani, S. Rezaei, M. Soofi, and S. Soltani. 2021. Barriers in access to healthcare for women with disabilities: A systematic review in qualitative studies. BMC Women’s Health 21(1):44.
McCue, K., and N. DeNicola. 2019. Environmental exposures in reproductive health. Obstetrics & Gynecology Clinics of North America 46(3):455–468.
Merone, L., K. Tsey, D. Russell, and C. Nagle. 2022. Sex inequalities in medical research: A systematic scoping review of the literature. Women’s Health Reports 3(1):49–59.
Meyer, I. H. 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin 129(5):674–697.
Mirin, A. A. 2021. Gender disparity in the funding of diseases by the U.S. National Institutes of Health. Journal of Women’s Health 30(7):956–963.
Mohamoud, Y. A., E. Cassidy, E. Fuchs, L. S. Womack, L. Romero, L. Kipling, R. Oza-Frank, K. Baca, R. R. Galang, A. Stewart, S. Carrigan, J. Mullen, A. Busacker, B. Behm, L. M. Hollier, C. Kroelinger, T. Mueller, W. D. Barfield, and S. Cox. 2023. Vital signs: Maternity care experiences—United States, April 2023. MMWR 72(35):961–967.
Montez, J. K., and K. J. Cheng. 2022. Educational disparities in adult health across U.S. states: Larger disparities reflect economic factors. Frontiers in Public Health 10:966434.
Moss, M. 2019. Trauma Lives on in Native Americans by Making Us Sick—While the U.S. Looks Away. https://www.theguardian.com/commentisfree/2019/may/09/trauma-lives-on-in-native-americans-while-the-us-looks-away (accessed March 6, 2023).
Moss, N. E. 2002. Gender equity and socioeconomic inequality: A framework for the patterning of women’s health. Social Science & Medicine 54(5):649–661.
Movement Advancement Project. n.d.-a. Bans on Best Practice Medical Care for Transgender Youth. https://www.lgbtmap.org/equality-maps/healthcare/youth_medical_care_bans (accessed August 23, 2024).
Movement Advancement Project. n.d.-b. Equality Maps: Employment Nondiscrimination Laws. https://www.lgbtmap.org/equality_maps/employment_non_discrimination_laws (accessed August 25, 2024).
Movement Advancement Project. n.d.-c. Healthcare Laws and Policies. https://www.lgbtmap.org/equality-maps/healthcare_laws_and_policies (accessed August 23, 2024).
Movement Advancement Project. n.d.-d. Identity Document Laws and Policies—Birth Certificate. https://www.lgbtmap.org/equality-maps/identity_documents/birth_certificate (accessed August 23, 2024).
Movement Advancement Project. n.d.-e. Identity Document Laws and Policies—Driver’s License. https://www.lgbtmap.org/equality-maps/identity_documents (accessed August 23, 2024).
Movement Advancement Project. n.d.-f. Identity Document Laws and Policies—Name Change. https://www.lgbtmap.org/equality-maps/identity_documents/name_change (accessed August 23, 2024).
Movement Advancement Project. n.d.-g. Medicaid Coverage of Transgender-Related Health Care. https://www.lgbtmap.org/equality-maps/healthcare/medicaid (accessed August 23, 2024).
Movement Advancement Project. n.d.-h. Transgender Healthcare “Shield” Laws. https://www.lgbtmap.org/equality-maps/healthcare/trans_shield_laws (accessed August 23, 2024).
Movement Advancement Project and Center for American Progress. 2024. Paying an Unfair Price: The Financial Penalty for Being Transgender in America. Washington, DC: Center for American Progress.
Nagle, A., and G. Samari. 2021. State-level structural sexism and cesarean sections in the United States. Social Science & Medicine 289:114406.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2017. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press.
NASEM. 2019a. A roadmap to reducing child poverty. Washington, DC: The National Academies Press.
NASEM. 2019b. Vibrant and healthy kids: Aligning science, practice, and policy to advance health equity. Washington, DC: The National Academies Press.
NASEM. 2020a. Birth settings in America: Outcomes, quality, access, and choice. Washington, DC: The National Academies Press.
NASEM. 2020b. Understanding the well-being of LGBTQI+ populations. Washington, DC: The National Academies Press.
NASEM. 2021a. Exploring the role of critical health literacy in addressing the social determinants of health: Proceedings of a workshop—in brief. Edited by R. M. Martinez and K. McHugh. Washington, DC: The National Academies Press.
NASEM. 2021b. Population health in rural America in 2020: Proceedings of a workshop. Edited by A. Nicholson. Washington, DC: The National Academies Press.
NASEM. 2021c. Sexually transmitted infections: Adopting a sexual health paradigm. Washington, DC: The National Academies Press.
NASEM. 2023a. Civic engagement and civic infrastructure to advance health equity: Proceedings of a workshop. Edited by A. Baciu and A. Andrada. Washington, DC: The National Academies Press.
NASEM. 2023b. Federal policy to advance racial, ethnic, and tribal health equity. Washington, DC: The National Academies Press.
NASEM. 2024a. Advancing research on chronic conditions in women. Washington, DC: The National Academies Press.
NASEM. 2024b. Essential health care services addressing intimate partner violence. Washington, DC: The National Academies Press.
NASEM. 2024c. Overview of research gaps for selected conditions in women’s health research at the National Institutes of Health: Proceedings of a workshop—in brief. Washington, DC: The National Academies Press.
NASEM. 2024d. Reducing intergenerational poverty. Washington, DC: The National Academies Press.
National Coalition of Anti-Violence Programs. 2018. Lesbian, gay, bisexual, transgender, queer and HIV-affected hate and intimate partner violence in 2017. New York: National Coalition of Anti-Violence Programs.
National Constitution Center. n.d. Obergefell v. Hodges (2015). https://constitutioncenter.org/the-constitution/supreme-court-case-library/obergefell-v-hodges (accessed August 27, 2024).
National Library of Medicine. n.d. Medicine Ways: Traditional Healers and Healing. https://www.nlm.nih.gov/nativevoices/exhibition/healing-ways/medicine-ways/medicine-wheel.html (accessed August 26, 2024).
National Menopause Foundation. n.d. National Menopause Foundation: About Us. https://nationalmenopausefoundation.org/about/ (accessed August 27, 2024).
Newland, B. 2022. Federal Indian Boarding School Initiative investigative report. Washington, DC: The Office of the Assistant Secretary—Indian Affairs.
Nguyen Le, T. A., A. T. Lo Sasso, and M. Vujicic. 2017. Trends in the earnings gender gap among dentists, physicians, and lawyers. Journal of the American Dental Association 148(4):257–262.e252.
NHLBI (National Heart, Lung, and Blood Institute). 2023. Asthma in the Black Community. https://www.nhlbi.nih.gov/sites/default/files/publications/asthma_in_black_community_fact_sheet.pdf (accessed October 21).
NIH (National Institutes of Health). n.d. Reporter Search Results for “Two-Spirit.” https://reporter.nih.gov/search/WnMXFzqBiEa88HOf_3lrpw/projects (accessed October 22, 2024).
Novak, N. L., N. Lira, K. E. O’Connor, S. D. Harlow, S. L. R. Kardia, and A. M. Stern. 2018. Disproportionate sterilization of Latinos under California’s eugenic sterilization program, 1920–1945. American Journal of Public Health 108(5):611–613.
O’Keefe, V. M., T. L. Maudrie, A. B. Cole, J. S. Ullrich, J. Fish, K. X. Hill, L. A. White, N. Redvers, V. B. B. Jernigan, J. P. Lewis, A. E. West, C. A. Apok, E. J. White, J. D. Ivanich, K. Schultz, M. E. Lewis, M. C. Sarche, M. B. Gonzalez, M. Parker, S. E. Neuner Weinstein, C. J. McCray, D. Warne, J. C. Black, J. R. Richards, and M. L. Walls. 2023. Conceptualizing Indigenous strengths-based health and wellness research using group concept mapping. Archives of Public Health 81(1):71.
OASH (Office of the Assistant Secretary for Health). n.d.-a. Healthy People 2030. https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed July 18, 2024).
OASH. n.d.-b. Healthy People 2030—Access to Health Services. https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/access-health-services (accessed August 26, 2024).
OASH. n.d.-c. Healthy People 2030—Poverty. https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/poverty (accessed August 23, 2024).
OASH. n.d.-d. Healthy People 2030: Neighborhood and Built Environment. https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/neighborhood-and-built-environment (accessed October 21, 2024).
Office of Disability Employment Policy. 2021. Spotlight on women with disabilities. Washington, DC: Department of Labor.
OMH (Office of Minority Health). 2024a. Obesity and African Americans. https://minority-health.hhs.gov/obesity-and-african-americans (accessed October 22, 2024).
OMH. 2024b. Obesity and Hispanic Americans. https://minorityhealth.hhs.gov/obesity-and-hispanic-americans (accessed October 22, 2024).
Oram, S., H. Khalifeh, and L. M. Howard. 2017. Violence against women and mental health. Lancet Psychiatry 4(2):159–170.
Ordway, D.-M. 2023. Weight Bias, Common in Health Care, Can Drive Weight Gain and Prompt People with Obesity to Avoid Doctors, Research Finds. https://journalistsresource.org/health/weight-bias-health-care-obesity-research/ (accessed August 26, 2024).
Paz, K., and K. P. Massey. 2016. Health disparity among Latina women: Comparison with non-Latina women. Clinical Medical Insights: Women’s Health 9(Suppl 1):71–74.
PCOS Challenge. n.d. About PCOS Challenge. https://pcoschallenge.org/about-pcos-challenge/ (accessed August 27, 2024).
Peitzmeier, S. M., M. Malik, S. K. Kattari, E. Marrow, R. Stephenson, M. Agénor, and S. L. Reisner. 2020. Intimate partner violence in transgender populations: Systematic review and meta-analysis of prevalence and correlates. American Journal of Public Health 110(9):e1–e14.
Pendergrass, D. C., and M. Y. Raji. 2017. The Bitter Pill: Harvard and the Dark History of Birth Control. https://www.thecrimson.com/article/2017/9/28/the-bitter-pill/ (accessed October 21, 2024).
Perry, B. L., K. L. Harp, and C. B. Oser. 2013. Racial and gender discrimination in the stress process: Implications for African American women’s health and well-being. Sociological Perspectives 56(1):25–48.
Petrosky, E., L. M. Mercer Kollar, M. C. Kearns, S. G. Smith, C. J. Betz, K. A. Fowler, and D. E. Satter. 2021. Homicides of American Indians/Alaska Natives—National Violent Death Reporting System, United States, 2003–2018. MMWR Surveillance Summaries 70(8):1–19.
Philbin, M. M., B. G. Everett, and J. D. Auerbach. 2024. Gender(ed) science: How the institutionalization of gender continues to shape the conduct and content of women’s health research. Social Science & Medicine 351:116456.
Pichardo, M. S., L. M. Ferrucci, Y. Molina, D. A. Esserman, and M. L. Irwin. 2023. Structural racism, lifestyle behaviors, and obesity-related cancers among Black and Hispanic/Latino adults in the United States: A narrative review. Cancer Epidemiology Biomarkers and Prevention 32(11):1498–1507.
Presumey-Leblanc, G., and M. Sandel. 2024. The legacy of slavery and the socialization of Black female health and human services workforce members in addressing social determinants of health. Journal of Racial and Ethnic Health Disparities 11(1):192–202.
Price, G. N., and W. A. Darity. 2010. The economics of race and eugenic sterilization in North Carolina: 1958–1968. Economics & Human Biology 8(2):261–272.
Puhl, R. M., and C. A. Heuer. 2010. Obesity stigma: Important considerations for public health. American Journal of Public Health 100(6):1019–1028.
Raghupathi, V., and W. Raghupathi. 2020. The influence of education on health: An empirical assessment of OECD countries for the period 1995–2015. Archives of Public Health 78:20.
Ransohoff, J. I., P. Sujin Kumar, D. Flynn, and E. Rubenstein. 2022. Reproductive and pregnancy health care for women with intellectual and developmental disabilities: A scoping review. Journal of Applied Research in Intellectual Disabilities 35(3):655–674.
Rapp, K. S., V. V. Volpe, and H. Neukrug. 2021. State-level sexism and women’s health care access in the United States: Differences by race/ethnicity, 2014–2019. American Journal of Public Health 111(10):1796–1805.
Redd, S. K., W. S. Rice, M. S. Aswani, S. Blake, Z. Julian, B. Sen, M. Wingate, and K. S. Hall. 2021. Racial/ethnic and educational inequities in restrictive abortion policy variation and adverse birth outcomes in the United States. BMC Health Services Research 21(1):1139.
Rennels, C., S. G. Murthy, M. A. Handley, M. D. Morris, B. K. Alldredge, P. Dahiya, R. Jagsi, J. L. Kerns, and C. Mangurian. 2024. Informal caregiving among faculty at a large academic health sciences university in the United States: An opportunity for policy changes. Academic Psychiatry 48(4):320–328.
Rickard, B. P., I. Rizvi, and S. E. Fenton. 2022. Per- and poly-fluoroalkyl substances (PFAS) and female reproductive outcomes: PFAS elimination, endocrine-mediated effects, and disease. Toxicology 465:153031.
Rippel Foundation. n.d. Vital Conditions for Health and Well-Being. https://rippel.org/vital-conditions/ (accessed August 26, 2024).
Robinette, J. W., J. R. Piazza, and R. S. Stawski. 2021. Neighborhood safety concerns and daily well-being: A national diary study. Wellbeing, Space, and Society 2: 100047.
Robinson, M. 2022. Recent insights into the mental health needs of Two-Spirit people. Current Opinion in Psychology 48:101494.
Rochon, P. A., S. Kalia, and P. Higgs. 2021. Gendered ageism: Addressing discrimination based on age and sex. Lancet 398(10301):648–649.
Ross, C. E., R. K. Masters, and R. A. Hummer. 2012. Education and the gender gaps in health and mortality. Demography 49(4):1157–1183.
Rousseau, M., C. Rouzeau, J. Bainvel, and F. Pelé. 2022. Domestic exposure to chemicals in household products, building materials, decoration, and pesticides: Guidelines for interventions during the perinatal period from the French National College of Midwives. Journal of Midwifery and Women’s Health 67(Suppl 1):S113–S134.
RRC Polytech. 2024. Gender and Sexual Diversity—Two-Spirit People. https://library.rrc.ca/2SLGBTQIA/2spirit (accessed August 26, 2024).
Rudel, R. A., J. M. Ackerman, K. R. Attfield, and J. G. Brody. 2014. New exposure biomarkers as tools for breast cancer epidemiology, biomonitoring, and prevention: A systematic approach based on animal evidence. Environmental Health Perspectives 122(9):881–895.
Saad, L. 2023. 7 Insights Into Women’s Lives in the U.S. https://news.gallup.com/opinion/gallup/471242/insights-women-lives.aspx (accessed August 23, 2024).
Sattler, K. M., F. P. Deane, L. Tapsell, and P. J. Kelly. 2018. Gender differences in the relationship of weight-based stigmatisation with motivation to exercise and physical activity in overweight individuals. Health Psychology Open 5(1):2055102918759691.
Seven Directions: A Center for Indigenous Public Health. 2023. Indigenous Social Determinants of Health. https://cdn.prod.website-files.com/5d4b3177c03a6439be501a14/65fdf6eea8be02b9051d9a86_Module-Report-Compressed.pdf (accessed October 18, 2024).
Shearston, J. A., K. Upson, M. Gordon, V. Do, O. Balac, K. Nguyen, B. Yan, M.-A. Kioumourtzoglou, and K. Schilling. 2024. Tampons as a source of exposure to metal(loid)s. Environment International:108849.
Shrider, E. A., M. Kollar, F. Chen, and J. Semega. 2023. Income and Poverty in the United States: 2020. https://www.census.gov/library/publications/2021/demo/p60-273.html (accessed August 27, 2024).
Sieck, N. E., M. Bruening, I. v. Woerden, C. Whisner, and D. C. Payne-Sturges. 2024. Effects of behavioral, clinical, and policy interventions in reducing human exposure to bisphenols and phthalates: A scoping review. Environmental Health Perspectives 132(3):036001.
Silbergeld, E. K., and J. A. Flaws. 2002. Environmental exposures and women’s health. Clinical Obstetrics and Gynecology 45(4).
Simons, R. L., M. K. Lei, E. Klopack, Y. Zhang, F. X. Gibbons, and S. R. H. Beach. 2021. Racial discrimination, inflammation, and chronic illness among African American women at midlife: Support for the weathering perspective. Journal of Racial and Ethnic Health Disparities 8(2):339–349.
SisterSong. n.d. Reproductive Justice. https://www.sistersong.net/reproductive-justice/ (accessed August 23, 2024).
Slopen, M. 2023. The impact of paid sick leave mandates on women’s health. Social Science & Medicine 323:115839.
Sosa, J. A., and C. Mangurian. 2023. Addressing eldercare to promote gender equity in academic medicine. JAMA 330(23):2245–2246.
Statista. n.d. Distribution of the Leading Causes of Death for American Indians or Alaska Natives in the United States in 2019, by Gender. https://www.statista.com/statistics/1285749/aian-leading-causes-of-death-by-gender/ (accessed August 22, 2024).
Steele, L. S., A. Daley, D. Curling, M. F. Gibson, D. C. Green, C. C. Williams, and L. E. Ross. 2017. LGBT identity, untreated depression, and unmet need for mental health services by sexual minority women and trans-identified people. Journal of Women’s Health 26(2): 116–127.
Stern, A. M. 2005. Sterilized in the name of public health: Race, immigration, and reproductive control in modern California. American Journal of Public Health 95(7):1128–1138.
Stern, A. M. 2020. Forced Sterilization Policies in the U.S. Targeted Minorities and Those with Disabilities—and Lasted into the 21st Century. https://ihpi.umich.edu/news/forced-sterilization-policies-us-targeted-minorities-and-those-disabilities-and-lasted-21st (accessed March 18, 2023).
Stiel, L., P. B. Adkins-Jackson, P. Clark, E. Mitchell, and S. Montgomery. 2016. A review of hair product use on breast cancer risk in African American women. Cancer Medicine 5(3): 597–604.
Strings, S. 2019. Fearing the Black body: The racial origins of fat phobia. New York: NYU Press.
Thornburg, B., A. Kennedy-Hendricks, J. D. Rosen, and M. D. Eisenberg. 2024. Anxiety and depression symptoms after the Dobbs abortion decision. JAMA 331(4):294–301.
Tight Lipped. n.d. Tight Lipped. https://www.tightlipped.org/ (accessed August 27, 2024).
Tribal Information Exchange. n.d. Walking in Two Worlds: Supporting the Two Spirit and Native LGBTQ Community. https://tribalinformationexchange.org/files/resources/twospiritbrochure.pdf (accessed August 26, 2024).
Tribouilloy, C., Y. Bohbot, D. Rusinaru, K. Belkhir, M. Diouf, A. Altes, Q. Delpierre, S. Serbout, M. Kubala, F. Levy, S. Maréchaux, and M. Enriquez Sarano. 2021. Excess mortality and undertreatment of women with severe aortic stenosis. Journal of the American Heart Association 10(1):e018816.
Trost, S., J. Beauregard, G. Chandra, F. Njie, A. Harvey, J. Berry, and D. A. Goodman. 2022. Pregnancy-related deaths among American Indian or Alaska Native persons: Data from maternal mortality review committees in 36 US states, 2017–2019. Atlanta, GA: Centers for Disease Control and Prevention.
Tucker, M. J., C. J. Berg, W. M. Callaghan, and J. Hsia. 2007. The Black-White disparity in pregnancy-related mortality from 5 conditions: Differences in prevalence and case-fatality rates. American Journal of Public Health 97(2):247–251.
University of Arizona Health Sciences. n.d. “Winter Institute” to Focus on Health and Research Issues Relevant to Native Americans, Feb. 17–20 at UA Health Sciences. https://azpride.uahs.arizona.edu/news/winter-institute%E2%80%99-focus-health-and-research-issues-relevant-native-americans-feb-17-20-ua (accessed August 26, 2024).
Urban Indian Health Institute. n.d. Our bodies, our stories: Sexual violence among native women in Seattle, WA. Washington, DC: Urban Indian Health Institute.
U.S. Equal Employment Opportunity Commission. n.d. Sexual Orientation and Gender Identity (SOGI) Discrimination. https://www.eeoc.gov/sexual-orientation-and-gender-identity-sogi-discrimination (accessed August 23, 2024).
Uvelli, A., C. Duranti, G. Salvo, A. Coluccia, G. Gualtieri, and F. Ferretti. 2023. The risk factors of chronic pain in victims of violence: A scoping review. Healthcare 11(17).
Vallée, A., P. F. Ceccaldi, M. Carbonnel, A. Feki, and J. M. Ayoubi. 2024. Pollution and endometriosis: A deep dive into the environmental impacts on women’s health. BJOG 131(4):401–414.
Van Loveren, H., J. G. Vos, D. Germolec, P. P. Simeonova, G. Eijkemanns, and A. J. McMichael. 2001. Epidemiologic associations between occupational and environmental exposures and autoimmune disease: Report of a meeting to explore current evidence and identify research needs. International Journal of Hygiene and Environmental Health 203(5–6):483–495.
Vedam, S., K. Stoll, T. K. Taiwo, N. Rubashkin, M. Cheyney, N. Strauss, M. McLemore, M. Cadena, E. Nethery, E. Rushton, L. Schummers, and E. Declercq. 2019. The Giving Voice to Mothers study: Inequity and mistreatment during pregnancy and childbirth in the United States. Reproductive Health 16(1):77.
Vigod, S. N., and P. A. Rochon. 2020. The impact of gender discrimination on a woman’s mental health. eClinicalMedicine 20.
Villardón-Gallego, L., A. García-Cid, A. Estévez, and R. García-Carrión. 2023. Early educational interventions to prevent gender-based violence: A systematic review. Healthcare 11(1).
Virginia Sexual and Domestic Violence Action Alliance. n.d. What Is Reproductive Justice? https://vsdvalliance.org/wp-content/uploads/2022/07/Part-1-What-is-Reproductive-Justice.pdf (accessed August 26, 2024).
Voges, M. M., H. L. Quittkat, B. Schöne, and S. Vocks. 2022. Giving a body a different face—how men and women evaluate their own body vs. that of others. Frontiers in Psychology 13:853398.
Walker, R. J., E. Garacci, A. Z. Dawson, J. S. Williams, M. Ozieh, and L. E. Egede. 2021. Trends in food insecurity in the United States from 2011–2017: Disparities by age, sex, race/ethnicity, and income. Populational Health Management 24(4):496–501.
Wallerstein, N. B., and B. Duran. 2006. Using community-based participatory research to address health disparities. Health Promotion Practice 7(3):312–323.
Washington, H. A. 2006. The Black stork: The eugenic control of African American reproduction. In Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. New York: Harlem Moon. Pp. 189–215.
Wehi, P. M., M. P. Cox, H. Whaanga, and T. Roa. 2023. Tradition and change: Celebrating food systems resilience at two Indigenous Māori community events. Ecology and Society 28(1).
Weiss, M. S., and E. E. Marsh. 2023. Navigating unequal paths: Racial disparities in the infertility journey. Obstetrics & Gynecology 142(4):940–947.
Weitzman, A. 2018. Does increasing women’s education reduce their risk of intimate partner violence? Evidence from an education policy reform. Criminology 56(3):574–607.
Well Project. 2024. Sexual and Reproductive Health, Rights, Justice, Pleasure, and HIV. https://www.thewellproject.org/hiv-information/sexual-and-reproductive-health-rights-justice-pleasure-and-hiv (accessed August 26, 2024).
Welleck, A., and M. Yeung. n.d. Reproductive Justice and Lesbian, Gay, Bisexual, and Transgender Liberation. https://www.protectchoice.org/article.php?id=135 (accessed August 26, 2024).
Wenger, N. K., D. M. Lloyd-Jones, M. S. V. Elkind, G. C. Fonarow, J. J. Warner, H. M. Alger, S. Cheng, C. Kinzy, J. L. Hall, V. L. Roger, and American Heart Association. 2022. Call to action for cardiovascular disease in women: Epidemiology, awareness, access, and delivery of equitable health care: A presidential advisory from the American Heart Association. Circulation 145(23):e1059–e1071.
WHO (World Health Organization). n.d. Health Equity. https://www.who.int/health-topics/health-equity#tab=tab_1 (accessed August 25, 2024).
WIA Report. 2022. The Significant Gender Gap in College Graduation Rates. https://www.wiareport.com/2022/11/the-significant-gender-gap-in-college-graduation-rates/ (accessed October 22, 2024).
Wise, L. A., T. R. Wang, C. N. Ncube, S. M. Lovett, J. Abrams, R. Boynton-Jarrett, M. R. Koenig, R. J. Geller, A. K. Wesselink, C. M. Coleman, E. E. Hatch, and T. James-Todd. 2023. Use of chemical hair straighteners and fecundability in a North American preconception cohort. American Journal of Epidemiology 192(7):1066–1080.
Wuest, J., M. Ford-Gilboe, M. Merritt-Gray, C. Varcoe, B. Lent, P. Wilk, and J. Campbell. 2009. Abuse-related injury and symptoms of posttraumatic stress disorder as mechanisms of chronic pain in survivors of intimate partner violence. Pain Medicine 10(4):739–747.
Wuest, J., M. Ford-Gilboe, M. Merritt-Gray, P. Wilk, J. C. Campbell, B. Lent, C. Varcoe, and V. Smye. 2010. Pathways of chronic pain in survivors of intimate partner violence. Journal of Women’s Health 19(9):1665–1674.
Yearby, R. 2022. The social determinants of health, health disparities, and health justice. Journal of Law, Medicine, & Ethics 50(4):641–649.
Yu, S. 2018. Uncovering the hidden impacts of inequality on mental health: A global study. Translational Psychiatry 8(1):98.
Zajacova, A., and E. M. Lawrence. 2018. The relationship between education and health: Reducing disparities through a contextual approach. Annual Review of Public Health 39:273–289.
Zhao, J., A. Zahn, S. C. Pang, T. S. Quang, J. Campbell, and P. N. Halkitis. 2024. Early national trends in non-abortion reproductive care access after Roe. Frontiers in Public Health 12:1309068.
Zhu, D. T., L. Zhao, T. Alzoubi, N. Shenin, T. Baskaran, J. Tikhonov, and C. Wang. 2024. Public health and clinical implications of Dobbs v. Jackson for patients and healthcare providers: A scoping review. PLoS One 19(3):e0288947.
Zlatnik, M. G. 2016. Endocrine-disrupting chemicals and reproductive health. Journal of Midwifery and Women’s Health 61(4):442–455.
Zota, A. R., and B. Shamasunder. 2017. The environmental injustice of beauty: Framing chemical exposures from beauty products as a health disparities concern. American Journal of Obstetrics and Gynecology 217(4):418.e411–418.e416.
Zubizarreta, D., A. L. Beccia, J. T. Chen, J. L. Jahn, S. B. Austin, and M. Agénor. 2024. Structural racism-related state laws and healthcare access among Black, Latine, and White U.S. adults. Journal of Racial and Ethnic Health Disparities [Epub ahead of print].















































