How can you tell if you have COVID-19, RSV, or the flu?
Based on Science
Without a diagnostic test, it can be difficult to tell which virus is the cause of a respiratory illness, especially if all three are circulating in a community at the same time.
Last update December 30, 2022
COVID-19, RSV, and the seasonal flu have some symptoms in common.
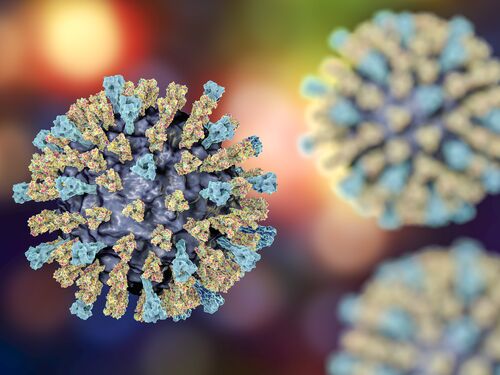
COVID-19, RSV, and the seasonal flu are all respiratory infections, but they are caused by different viruses. COVID-19 is caused by the coronavirus SARS-CoV-2. RSV is short for respiratory syncytial virus, a type of pneumovirus. Influenza viruses cause the flu.
Fever, cough, and runny nose are symptoms common to all three illnesses, although not everyone gets a fever. Certain symptoms are more common with some of the viruses. For example, tiredness and achiness are more likely with COVID-19 and the flu. RSV and COVID-19 can cause shortness of breath or difficulty breathing, particularly in more severe cases. Other symptoms, such as decrease in appetite, tiredness, and irritability can be seen in babies under the age of 6 months with RSV infections.
Because these illnesses and others (including common colds caused by other viruses) have many symptoms in common, health care providers often make a diagnosis based on their knowledge about what virus is most common in a community at the time the patient is sick. When all three viruses are causing illness in a community at the same time, a diagnostic test can be used to identify which virus is the cause. This is typically done by testing body fluids collected with a nasal or mouth swab. If needed to support care, diagnostic tests are available in health care settings for all three viruses. Recently, at-home diagnostic tests have become available for flu and COVID-19.
All three viruses are more likely to cause severe illness in the very young and in older adults.
In most cases, COVID-19, RSV, and the seasonal flu cause mild, cold-like illnesses that clear up within 2 weeks. However, they can require hospitalization and even cause death, particularly in higher risk groups.
Children under the age of 5 are vulnerable to all three illness. Children who were born prematurely or have a chronic health condition are more vulnerable than children in this age group who are otherwise healthy, but all small children are at higher risk because of the size of their lungs and airways. Their small size means inflammation of the airways caused by respiratory illness can more easily cause breathing problems and lead to more serious complications, like pneumonia. In the flu seasons from 2016 to 2020, between 16,000 and 27,000 children under the age of 5 in the U.S. were hospitalized and between 100 and 330 died of flu each year. Studies in the U.S. looking at children under the age of 18 hospitalized for COVID-19 found that infants (that is, children under the age of 1) accounted for more than 20% of these cases. Premature birth is associated with hospitalization for COVID-19 in infants. And RSV is a leading cause of hospitalization for small children. Prior to the COVID-19 pandemic, more than 57,000 children under the age of 5 were hospitalized each year for complications from RSV infections in the United States. In 2019, more than 3.6 million small children were hospitalized for RSV around the world. RSV infections are the most common cause of bronchiolitis, which is inflammation of tiny airways in the lungs, and pneumonia in infants.
People 65 years of age and older are also at higher risk for severe disease from COVID-19 and the seasonal flu. Older adults are more likely to be hospitalized or die from either disease, especially if they are unvaccinated. Adults 65 and older make up less than 17% of the U.S. population, but they have accounted for more than 40% of COVID-19 hospitalizations since the start of the pandemic and more than 75% of COVID-19 deaths. In the flu seasons from 2016 to 2020, between 44% to 67% of hospitalizations and 63% to 86% of deaths in the U.S. were in older adults.
Like COVID-19 and the flu, people can be infected with RSV more than once. As with the other two viruses, RSV presents a risk to adults 65 years of age and older and people with compromised immune systems or those with chronic heart or lung disease. Roughly 14,000 adults over the age of 65 die in the United States each year from RSV. It is likely that the true risk of RSV to older adults is not fully appreciated. There is less information on the risk of RSV in adult populations, as compared to children, because testing to confirm the virus in adults has not been common. As more testing is done to confirm that a respiratory infection is caused by RSV, the risk the virus presents to adults will become clearer.
Vaccines and medicines exist for COVID-19 and the seasonal flu. RSV vaccines for some populations were recently approved.
Vaccines to protect against COVID-19 and the seasonal flu are available for all people 6 months of age and older. There are also antiviral drugs available to treat COVID-19 and the flu.
Several vaccines have been in development for RSV, and two were approved by the U.S. Food and Drug Administration (FDA) for use in some adult populations in 2023. Both vaccines can be used in adults 60 years of age and older. One of the vaccines is also approved for use in women 32–36 weeks pregnant to pass immune protection on to their babies.
Monoclonal antibody treatments for RSV provide antibodies against the virus, which can prevent severe illness should an RSV infection occur. One such drug is approved for use in the most vulnerable populations, such as premature infants. In 2023, FDA approved another monoclonal antibody drug for use in all babies under 8 months of age.
There is currently no medicine that specifically treats an RSV infection. Children who are hospitalized for RSV may receive additional oxygen and IV fluids to make sure they get enough oxygen and stay hydrated while they fight the infection. In the most severe cases, a child may need the help of a ventilator to breathe. Most hospital stays only last a few days. However, in places where access to medical care is limited, RSV can be deadly. Scientists estimate that, worldwide, RSV caused more than 100,000 deaths in 2019 in children under the age of 5. Two-thirds of those deaths were in children less than 1 year old, and 97% of deaths occurred in low-income and middle-income countries, where adequate medical care is less available or does not exist.
There are ways to protect yourself from these respiratory illnesses.
RSV, SARS-CoV-2, and influenza viruses are mainly spread by respiratory droplets and aerosols, which can be released when an infected person coughs, sneezes, talks, sings, or breathes. You can also get RSV through contact with a surface that has the virus on it or by coming into contact with infected body fluids (for example, from wiping mucus from a child’s nose), followed by touching your eyes, nose, or mouth.
Therefore, you can decrease your risk of a respiratory infection by washing your hands often, covering coughs and sneezes, cleaning frequently touched objects, and minimizing time in crowds and poorly ventilated indoor spaces, if possible. Also, get your annual flu shot, get vaccinated against COVID-19, talk to your doctor about the RSV vaccine if eligible and stay up-to-date with all other vaccinations. If you do get sick, stay home to avoid spreading a virus to others.
ADDITIONAL RESOURCES
COVID-19 Responses and Resources – National Academies of Sciences, Engineering, and Medicine
National Academies of Sciences, Engineering, and Medicine – Health and Medicine | Topic
RSV: When It's More Than Just a Cold – American Academy of Pediatrics
Respiratory Syncytial Virus Infection (RSV) – Centers for Disease Control and Prevention
More like this
Events
Right Now & Next Up
Stay in the loop with can’t-miss sessions, live events, and activities happening over the next two days.
TRB Annual Meeting | January 11 - 15, 2026
January 11 - 15, 2026 | The TRB Annual Meeting brings together thousands of transportation professionals worldwide for sessions across all modes and sectors.