Expanding Delivery and Increasing Uptake of Medical Countermeasures Through Public–Private Partnerships: Proceedings of a Workshop—in Brief (2024)
Chapter: Expanding Delivery and Increasing Uptake of Medical Countermeasures Through Public–Private Partnerships: Proceedings of a Workshop Series—in Brief
 |
Proceedings of a Workshop Series—in Brief |
Expanding Delivery and Increasing Uptake of Medical Countermeasures Through Public–Private Partnerships
Proceedings of a Workshop Series—in Brief
To build on the lessons learned from past public health emergency responses, the National Academies of Sciences, Engineering, and Medicine Forum on Medical and Public Health Preparedness for Disasters and Emergencies hosted a virtual workshop series to examine lessons and discuss future opportunities for public–private partnerships (PPPs) to facilitate the distribution, dispensing, acceptance, and uptake of medical countermeasures (MCMs) in a public health emergency. MCMs are medicines and medical supplies that may be used in public health emergency responses to diagnose, prevent, or treat disease. PPPs refer to cross-sector collaborations among government, private for-profit, and nonprofit entities.
The five workshops—held on October 3, 12, 17, 26, and November 2, 2023—featured invited presentations and discussions that were designed to explore (1) lessons learned from PPPs that delivered MCMs during past health emergencies; (2) opportunities to expand and sustain partnerships and capacities between emergencies as well as opportunities to reduce or eliminate barriers that challenge the operationalization, sustainment, and expansion of partnerships; (3) opportunities for addressing the unique needs of disproportionately affected populations through enhanced capacity for MCM distribution and dispensing; and (4) potential paths forward for PPPs to deliver MCMs to the public through threat-agnostic and MCM-agnostic systems. Additionally, two recordings were made available on the project webpages which provided a conceptual background for the workshop series discussions.1
This Proceedings of a Workshop Series—in Brief highlights key points made by workshop participants during the presentations and discussions during the workshop.2
WORKSHOP SERIES OVERVIEW
During the workshop series, Ali S. Khan of the University of Nebraska Medical Center and other speakers referred to prerecorded materials that were made available on the project webpage in advance of the series. The recordings presented the operational, social, and cultural context of public–private partnerships for MCM distribution, dispensing, and uptake. These components of the MCM system are also known as the “last mile.” The MCM system presented during the workshop series can be seen in Figure 1, with the
__________________
1 Pre-recorded background materials available on the project webpage: https://www.nationalacademies.org/our-work/medical-counter-measures-expanding-delivery-and-increasing-uptake-through-public-private-partnerships-a-workshop-series.
2 This Proceedings of a Workshop Series—in Brief is not intended to provide a comprehensive summary of information shared during the workshop. It reflects the knowledge and opinions of individual workshop participants and should not be construed as representing any consensus among the workshop participants.
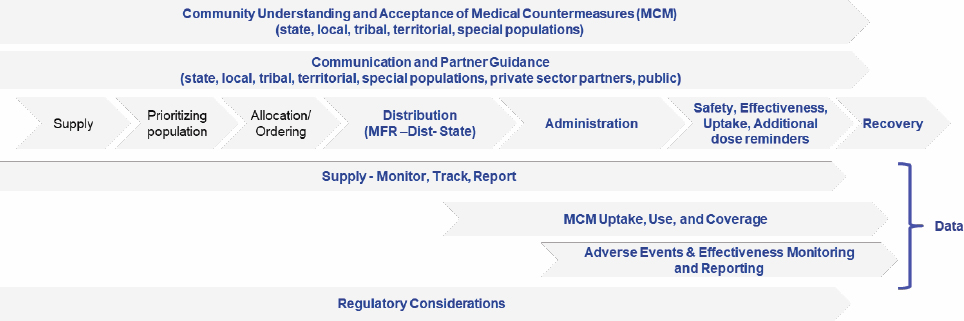
SOURCE: Ali S. Khan presentation, Background Resource: Overview of the U.S. Medical Countermeasures System, October 12, 2023. Original from Anita Patel presentation, From Factory to Frontlines: COVID-19 Vaccine Overview, February 2023, Tufts University, Medford, Massachusetts.
specific components that are relevant for the “last mile” in blue text.
PUBLIC–PRIVATE PARTNERSHIPS FOR DATA-INFORMED DECISION MAKING ABOUT MEDICAL COUNTERMEASURES
The first workshop explored ways to bring timely and relevant information to decision makers who inform strategy and operations for MCM distribution, dispensing, and administration.3 Participants presented case studies of novel PPP partnerships that were aimed at improving data-informed decision making to distribute, dispense, administer, and promote acceptance of MCMs (see Box 1). The subsequent discussion focused on successful elements of PPPs and strategies that can be applied to future health emergencies.
__________________
3 The workshop agenda and presentations are available at https://www.nationalacademies.org/event/40843_10-2023_workshop-1-public-private-partnerships-for-data-informed-decision-making-to-distribute-dispense-and-administer-medical-countermeasures_ (accessed January 15, 2024).
Reflecting on the first workshop’s case study presentations and discussion, John Hick of the University of Minnesota said that data serve as a throughline through all MCM issues. In addition to elucidating which types of MCMs are required and where they are needed, data are also important for monitoring the effectiveness of distribution. However, data require vetting, analysis, and interpretation to become actionable for informing public health decisions. Hick described PPPs as a foundational component of data-informed decision making about MCMs because they allow the private sector to contribute innovation and efficiency to problem-solving efforts within the public sector. Moreover, PPPs provide the public sector with access to critical private-sector data for day-to-day surveillance during an emergency event, quantifying the magnitude of the event, and right-sizing the MCM response. Given their value, PPPs supporting robust data ecosystems should be sustained between crises to address day-to-day public health issues while being poised to activate during an emergency, added Ali S. Khan of the University of Nebraska Medical Center.
In effective PPPs, the “right data are shared at the right time,” Hick said. The data should be shared bidirectionally via a standard mechanism through which information can be rapidly integrated to inform decisions about MCM deployment. New platform technologies can help to unify data streams so that the data streams can be effectively operationalized and enable public health action. Because data needs differ in different public health crises, an approach that unifies the public and private sectors can help to identify the essential data elements and engage the appropriate partners for specific events, Hick said.
PPPs work effectively when they provide value to both the public- and private-sector partners, Hick said, but misconceptions that the private sector is motivated solely by profit can undermine the effectiveness of PPPs. Several participants discussed that while a data sharing agreement might exist between a private-sector partner and a government agency, it does not necessarily allow that same agency to share the data with other parts or levels of the government. This compartmentalization can erode trust and transparency. Elaborating further, several participants also highlighted the need to build trust in the public health enterprise among private-sector partners, different levels of government, and the general public—greater levels of trust and transparency can result in more robust data and vice versa.
In conclusion, Khan spoke about the importance of supporting interoperability through a coherent interoperability strategy, infrastructure, and subject matter expertise, implementing standards like widely-recognized data exchange standards, and ensuring patient privacy across public- and private-sector data systems.
He also highlighted the value of flexibility, both in data integration—to overcome interoperability issues—and in the ability to adjust security and governance policies to address equity gaps in distribution.
PUBLIC–PRIVATE PARTNERSHIPS FOR ACCEPTANCE AND UPTAKE OF MEDICAL COUNTERMEASURES
The second workshop focused on how to enable understanding, acceptance, and uptake and administration of MCMs, with a particular focus on at-risk and disproportionately affected populations.4 Public acceptance and uptake of MCMs can significantly affect the health and well-being of affected communities. Highlights from the workshop’s case study presentations are provided in Box 2.
Throughout the second workshop, participants highlighted the importance of putting communities at the center of planning activities—both in emergency response efforts and in PPPs to support those efforts—to help promote the acceptance and uptake of MCMs, said Monica Schoch-Spana of the Johns Hopkins Center for Health Security. Schoch-Spana continued that community and faith-based organizations should be recognized as true partners in
__________________
4 The workshop agenda and presentations are available at https://www.nationalacademies.org/event/40844_10-2023_workshop-2-public-private-partnerships-for-acceptance-and-uptake-of-medical-countermeasures (accessed January 15, 2024).
a public health response. Community-level partners have distinctive assets, such as proximity, established connections, and insights related to communities that mainstream institutions may not necessarily have the will or the capacity to serve, she added. Schoch-Spana concluded that, for these reasons, PPPs that engage community partners can more effectively reach communities that are vulnerable, underserved, and consequently at a heightened risk of experiencing disproportionately adverse impacts during a public health emergency. PPPs can most effectively deliver MCMs to communities in an emergency when the partners already have a history of collaborating, Schoch-Spana said.
Local governments need sustained funding to support investments in these community relationships, networks, and touchpoints so that can be activated in times of emergencies and also provide value on an everyday basis, Schoch-Spana said. Thus, she continued, these PPPs should not be started up and then demobilized after a crisis period. Additionally, she said, hyperlocal community partners need support to be “paper ready” for PPPs through actions that promote administrative preparedness, and strategies for getting MCMs to end users should ensure that partners are paper-ready through mechanisms such as memorandums-of-understanding, pre-standing contracts, and nimble financing structures.
From the perspectives of communities and community partners, the MCM delivery system provides more than clinically valuable interventions, Schoch-Spana said; “it delivers proof that the lives of community members matter.” This approach provides an opportunity to foster collective efficacy by applying community assets and enabling a community to achieve its own priorities, she concluded.
PUBLIC–PRIVATE PARTNERSHIPS FOR DISPENSING AND ADMINISTERING MEDICAL COUNTERMEASURES
The third workshop examined strategies to deliver and administer significant volumes of MCMs to the public.5 Mass dispensing of MCMs is a complex effort because of the diversity of public health emergencies (e.g., chemical, biological, radiological, or nuclear events) and the fact that such emergencies can have very tight time constraints for delivering and administering significant volumes of medical countermeasures to the public. Through case studies and discussions, this workshop explored how PPPs can contribute to equitable access to and the efficient dispensing and administration of MCMs, with a particular focus on pharmacies and other nontraditional partners and points of access. Box 3 presents highlights from the workshop’s case study presentations.
Anita Patel of Walgreens opened the third workshop’s discussion by sketching a general approach for strengthening the system for dispensing and administering MCMs: (1) identify the end state of needs to be addressed, (2) map the landscape of partners that could contribute, (3) determine where missions are aligned, and (4) adjust the system to meet the needs (e.g., by using regulatory and policy levers to help mobilize partners). She emphasized that the system should be guided by strong, centralized leadership with decision-making authority and should be buttressed by a system of coordination that is understood by and representative of all actors. Knowing what needs to be true to activate partners was the foundation of starting up community-level testing and immunization during the COVID-19 pandemic, she said. Ideally, the infrastructure built for the COVID-19 pandemic would be maintained to support day-to-day public health activities that can adapt to future emergency responses, she added.
Patel highlighted the role of facilitative regulatory, legal, and legislative pathways in broadening access to MCMs during the COVID-19 pandemic, and Bernstein provided an overview of several key pathways pertaining to pharmacies. The Federal Retail Pharmacy Program (FRPP), a PPP launched in 2021, eventually included 21 retail pharmacy partners representing more than 40,000 pharmacies nationwide. Pharmacy partners signed agreements with the government promising to abide by specific measures; in turn, they were able to readily order vaccines from federal government supplies to meet the needs of their patient populations. These pharmacies then provided information back to the federal
__________________
5 The workshop agenda and presentations are available at https://www.nationalacademies.org/event/40845_10-2023_workshop-3-public-private-partnerships-for-dispensing-of-medical-countermeasures (accessed January 15, 2024).
government about the patients and the populations who received the vaccine. Bernstein shared an example of the Bridge Access Program, a PPP between the Centers for Disease Control and Prevention, federal health centers, and participating pharmacies to provide coverage for COVID-19 vaccines for uninsured and underinsured patients. The Public Readiness and Emergency Preparedness Act (PREP Act) served as a powerful tool to take advantage of the value of pharmacy teams while it was in place during the COVID-19 pandemic, Bernstein
said. The PREP Act addressed statewide variability in scope of practice by enabling pharmacists to administer vaccines, allowing for license portability across states, and providing pharmacists with immunity from liability.
Several participants discussed strategies to maintain a “warm base” for PPPs that can help to ensure continuity from one response to another. Patel illustrated an example of a missed opportunity to maintain meaningful infrastructure that was built during COVID-19. COVID-19 testing and vaccination programs established entirely new core competencies for PPPs, but neither type of program was used during the mpox outbreak, she said. Proactive efforts to put in place pre-positioned agreements and contracts between public and private-sector actors can help maintain this “warm base,” Patel said. To maintain a warm base from pharmacies’ perspective, Bernstein suggested (1) pre-positioning contracts, protocols, and dispensing authorities; (2) establishing sustainable and fair payment pathways for pharmacists that cover public and private insurance plans as well as the uninsured; (3) maintaining the reporting, database, and ordering systems between events; (4) developing a “response playbook” for different scenarios; and (5) conducting table-top exercises.
Patel commented on the need to monitor the implementation and performance of systems for dispensing and administering MCMs, while considering the social determinants of health and having a clear understanding of what equity means in this context. In all emergency responses, federal authorities need to work closely with state and local authorities to ensure that national distribution strategies are well aligned with population needs and to incorporate equity from the ground level, she said.
PUBLIC–PRIVATE PARTNERSHIPS FOR DISTRIBUTION OF MEDICAL COUNTERMEASURES
To address the challenge of readying MCMs for timely distribution and delivery to points of dispensing in a public health emergency, the fourth workshop focused on the use of PPPs to ensure the equitable and efficient allocation and distribution of MCMs to affected populations.6 Through the presentation of case studies (see Box 4) and the subsequent discussion, participants shared examples of how PPPs can increase access to MCMs through coordinated distribution strategies; they also discussed barriers, facilitators, and opportunities to strengthen distribution.
Nicolette Louissaint of the Healthcare Distribution Alliance said that MCM distribution should adopt a patient-centered approach—accounting for where patients will actually receive MCMs during an emergency—and ensure that MCM distributors have sufficient lead time. This will often require adjustment to normal distribution plans and systems regarding the allocation of products. Louissant said that in successful PPPs for MCM distribution, partners will have clear roles and responsibilities that optimize their respective strengths. For example, the private sector has greater expertise in distribution than the public sector; thus, liaising with downstream private-sector distribution partners can improve the design of product packaging, ordering platforms, and account and customer management systems.
During the COVID-19 pandemic, PPPs between the federal government and private-sector distributors enabled greater speed, access, and efficiency in the distribution of MCMs, Louissaint said. In addition to facilitating the flow of information about supply and demand, PPPs allowed for sharing tactical, technical, and logistical expertise about MCM distribution. Louissant remarked on the need to recognize and mitigate variability in access to MCMs based on organizational size and previous purchasing practices that can lead to inequities in distribution and subsequently in administration, dispensing, and uptake.
Establishing clear, ongoing channels of communication with downstream partners is essential to maintaining trust and ensuring continuity in the flow of distribution across the evolving phases of a response, Louissaint said. This includes communication about an unfolding event as well as communication about how changes
__________________
6 The workshop agenda and presentations are available at https://www.nationalacademies.org/event/40846_10-2023_workshop-4-public-private-partnerships-for-distribution-of-medical-countermeasures (accessed January 15, 2024).
in operational realities may shift expectations for downstream partners (e.g., about when and where products will be received).
End-to-end visibility into the MCM supply chain requires large volumes of data, so PPPs should proactively aggregate such data ahead of the next crisis, said Jason Roos of ASPR. He emphasized that the data infrastructure created during the pandemic offered unprecedented insight into operations and distribution patterns; this infrastructure should be maintained between crises so partnerships do not have to be rebuilt during the next emergency. However, in using data to monitor and track equitable distribution of MCMs, a balance should be struck between obtaining sufficient information and overburdening the management of day-to-day operations with data reporting requests, Louissaint said.
Several participants spoke about opportunities to build the capacity to distribute MCMs during future events by investing in, creating, and maintaining PPPs. Khan called for elevating the focus on MCM distribution to match that placed on dispensing and administration, which warrants deliberative planning and prioritized investment. A range of different PPPs need to be sustained at multiple levels to support MCM distribution, said Onora Lien of the Northwest Healthcare Response Network. She suggested that the federal government should use incentives and allocate resources to build local, regional, and state-level capacities for engagement. Moving forward, Roos suggested (1)
enhancing and formalizing PPPs to ensure synchronized, synergistic modernization; (2) innovating on distribution to enable rapid development and dissemination of critical MCM-specific information; and (3) maintaining open communication channels with real-time feedback to eliminate logistical barriers as they surface.
LEVERS AND SYSTEMS FOR SUCCESSFUL PUBLIC-PRIVATE PARTNERSHIPS FOR MEDICAL COUNTERMEASURES DELIVERY
The fifth and final workshop focused on understanding the systems and conditions to enable successful PPPs for MCM distribution, dispensing, administration, and acceptance.7 Panelists shared regulatory perspectives, private sector health care perspectives, federal government perspectives, and state and local perspectives.
Will Chang of UpStream Healthcare spoke about legislative and regulatory pathways that would bolster the nation’s capacity to deploy MCMs in a public health emergency response. Underscoring the valuable yet underused role of pharmacists as a public health resource, he emphasized the need to provide Medicare status recognition to pharmacists. Two bills that have already been introduced to do so are the Equitable Community Access to Pharmacist Services Act8 and the Pharmacy and Medically Underserved Areas Enhancement Act9. Both bills share a key feature: when the HHS secretary declares a public health emergency in which pharmacists and pharmacy staff are essential in the response, the secretary can automatically turn on Medicare reimbursement for those services, thereby providing a reliable stream to reach the most vulnerable citizens. To facilitate information sharing by and with the government, Chang suggested expanding the scope of liability protection for all claims that might arise from any actions taken by private participants as a result of voluntary agreement under Section 708 of the Defense Production Act. This would protect against legal liability at the state and federal levels which could deter participation in a response, and it would help ensure that data are shared in a timely fashion across stakeholders so that resources can be effectively mobilized.
Marcus Coleman of the Center for Faith-Based and Neighborhood Partnerships offered examples of how the COVID-19 pandemic response demonstrated the ability to effectively scale different kinds and levels of PPPs. At the outset of the pandemic, the National Association for the Advancement of Colored People (NAACP) was among the first organizations to look for opportunities—based on existing social determinants of health and communities’ mistrust of the medical and government establishments—to rapidly collaborate with trusted partners to reach community members with MCMs. Coleman went on to further describe the historically black colleges and universities (HBCU) Emergency Management Workforce Consortium’s work in helping to build people’s confidence in taking protective measures as an illustration of the importance of working with trusted collaborators to build and sustain effective messaging through both formal and informal channels. In another example of the power of communication, Healthcare Ready started up substantial efforts to communicate evidence-based and data-informed messaging in a way that was easy to comprehend and share, in parallel to official health sector channels. Finally, Coleman spotlighted partnerships with national voluntary organizations active in disasters as providing continuing opportunities for collaboration between the emergency management and public health communities.
Melissa Harvey of HCA Healthcare shared a health care system perspective and discussed strategies to create better and more successful partnerships with health systems for MCM distribution. During the COVID-19 pandemic, MCM distribution challenges faced by health systems included confusion regarding the health system’s role in community testing and prophylaxis, a lack of awareness of monoclonal antibody availability at dispensing sites, and a lack of sufficient staff to manage the burden of testing, prophylaxis administration, acute care, and non-acute care. However, she warned, challenges faced during future events could be even
__________________
7 The workshop agenda and presentations are available at https://www.nationalacademies.org/event/40847_11-2023_workshop-5-future-opportunities-levers-and-systems-for-public-private-partnerships-to-distribute-dispense-and-administer-medical-countermeasures (accessed January 15, 2024).
8 H.R. 1770/S. 2477.
9 H.R. 2759/S. 1491.
more complex and difficult. She outlined a set of opportunities for enhancing partnerships to prepare for future complex events, such as: (1) enhancing the health systems’ awareness of federal Strategic National Stockpile (SNS) assets, (2) developing order sets for SNS assets, (3) increasing the visibility of consent forms and other documentation, (4) standardizing indications and administration guidelines, and (5) integrating health systems into planning (e.g., locations for MCM dispensing, supply chain requirements, referral processes, staffing needs, patient follow-up and tracking).
Steve Adams of the Administration for Strategic Preparedness and Response (ASPR) said that PPPs are most effective if they are integrated into the multilevel planning and preparedness cycle before the time of need. Not all public health responses are created equal, he remarked. Thus, it is important that planning accounts for long-term, slowly unfolding scenarios that provide opportunities to bring players to the table over time as well as for emergent public health events (e.g., natural disasters) that require a rapid response with very little time to integrate partners in real-time who were not part of pre-event planning. To illustrate the importance of planning, Adams described a distribution challenge during the 2022 mpox outbreak. The distribution tools that were deployed had been designed for a large-scale smallpox outbreak presuming the full mobilization of society, with a focus on using retailers to ease the distribution burden at the state and local level. Even though the mpox outbreak was a smaller-scale event compared to the COVID-19 pandemic, there was a delay in starting up emergency distribution capabilities. Given the limited resources, many states did not have the capability to move resources to smaller rural communities where people were in greatest need and living further from population centers where care was available. Putting in place distribution capacity to direct the flow of resources to rural areas addressed this gap in collective response capacity.
Paul Petersen of the Tennessee Department of Health spoke about the importance of engaging with state and local partners during response planning and considering the upstream and downstream impact of decisions about MCM deployment. To surmount barriers related to information technology integration and interoperability, he suggested (1) using existing tools for daily use cases before creating systems anew, (2) ensuring transparent communication, (3) investing in sustainable data modernization, and (4) engaging states in the development of reporting system strategies. To address challenges in the transition to the commercialization of MCMs, strategies include facilitating the payer transition—which is a major barrier to partners’ staying at the table—and mitigating the impact on disproportionately affected populations, such as individuals who cannot pay for services. Petersen described the federal pharmacy partnerships established during the COVID-19 pandemic as a resounding success because they used a national systems approach. To prepare for future threats, he encouraged continued investment in that type of federal coordination, coupled with building daily systems that can scale during emergencies. He also highlighted ASPR’s role in effective command and control for MCM management and coordination with private partners.
WORKSHOP SERIES CLOSING REMARKS
At the end of the final workshop, Brooke Courtney of the U.S. Food and Drug Administration asked for reflections on policies and practices that can create and sustain PPPs, and panelists offered the suggestions listed in Box 5. Khan emphasized that diverse private-sector involvement was a success of the COVID-19 pandemic. PPPs across the public health system are now at a unique point in time, he continued, with the alignment, structures, and engagement in place that can and should be maintained and used both for day-to-day practice and future emergencies. Suzet McKinney of Sterling Bay said that the COVID-19 pandemic underscored the extent to which efforts to distribute, deliver, and monitor the uptake of MCMs during a public health emergency are critical to the resilience and the recovery of individuals, families, and communities. “A medical countermeasure is only of value if it is used when it is needed by our communities,” McKinney said.
DISCLAIMER This Proceedings of a Workshop—in Brief has been prepared by Anna Nicholson, Shalini Singaravelu, and Lisa Brown as a factual summary of what occurred at the meeting. The statements made are those of the rapporteurs or individual workshop participants and do not necessarily represent the views of all workshop participants, the planning committee, or the National Academies of Sciences, Engineering, and Medicine.
*The National Academies of Sciences, Engineering, and Medicine’s planning committees are solely responsible for organizing the workshop, identifying topics, and choosing speakers. The responsibility for the published Proceedings of a Workshop—in Brief rests with the institution. The planning committee comprised Ali S. Khan (Chair), University of Nebraska Medical Center; Brooke Courtney, U.S. Food and Drug Administration; Nicole Errett, University of Washington; John Hick, Hennepin Healthcare; Christine Kosmos, Centers for Disease Control and Prevention; Nicolette Louissaint, Healthcare Distribution Alliance; Jennifer Martin, Department of Veterans Affairs; Suzet McKinney, Sterling Bay; Anita Patel, Walgreens; Sara Roszak, National Association of Chain Drug Stores; Monica Schoch-Spana, Johns Hopkins Center for Health Security; and Stephen Thomas, University of Maryland.
REVIEWERS To ensure that it meets institutional standards for quality and objectivity, this Proceedings of a Workshop—in Brief was reviewed by Suzet McKinney, Sterling Bay, and Paul Petersen, Tennessee Department of Health. Leslie Sim, National Academies of Sciences, Engineering, and Medicine, served as the review coordinator.
SPONSORS This workshop was partially supported by contracts between the National Academies of Sciences and the Administration for Children and Families, Administration for Strategic Preparedness and Response, American Burn Association, American College of Emergency Physicians, American College of Surgeons—Committee on Trauma, American Hospital Association, Assistant Secretary of Defense for Health Affairs, Association of Public Health Laboratories, Association of State and Territorial Health Officials, Centers for Disease Control and Prevention, Council of State and Territorial Health Officials, Emergency Nurses Association, Healthcare Distribution Alliance, Healthcare Ready, Infectious Diseases Society of America, Mass General Hospital, the MITRE Corporation, National Association of Chain Drug Stores, National Association of County and City Health Officials, National Association of Emergency Medical Technicians, National Fire Protection Association, National Highway Traffic Safety Administration, National Institute of Allergy and Infectious Diseases, Society of Critical Care Medicine, Trauma Center Association of America, U.S. Department of Defense, U.S. Department of Homeland Security, U.S. Food and Drug Administration, Uniformed Services University of the Health Sciences, and University of Nebraska Medical Center. Additionally, this project has been funded in part with federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; National Institute of Environmental Health Sciences; National Institute of Allergy and Infectious Diseases; National Cancer Institute; National Institute on Minority Health and Health Disparities; and the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services, under Contract no. HHSN2632018000291, Task Order no. HHSN26300026.
STAFF Lisa Brown, Scott Wollek, Shalini Singaravelu, Michael Berrios, and Rayane Silva-Curran.
For additional information regarding the workshop, visit https://www.nationalacademies.org/our-work/medical-countermeasures-expanding-delivery-and-increasing-uptake-through-public-private-partnerships-a-workshop-series.
Suggested citation: National Academies of Sciences, Engineering, and Medicine. 2024. Expanding delivery and increasing uptake of medical countermeasures through public–private partnerships: Proceedings of a workshop series—in brief. Washington, DC: The National Academies Press. https://doi.org/10.17226/27594.
|
Health and Medicine Division Copyright 2024 by the National Academy of Sciences. All rights reserved. |
 |











