Is monkeypox related to chickenpox?
Based on Science
Monkeypox is not related to chickenpox. Both diseases include ‘pox’ in their names because they both cause pockmark skin lesions. But they are different diseases caused by unrelated viruses. Monkeypox, renamed mpox, is an orthopoxvirus and related to the virus that causes smallpox. Chickenpox is caused by a type of herpes virus.
Last update October 25, 2022
Based on Science Banner
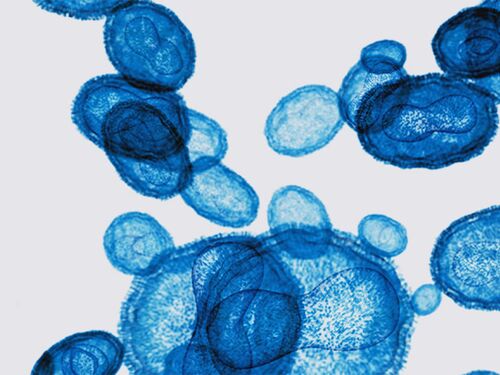
Mpox and chickenpox are different, unrelated types of viruses.
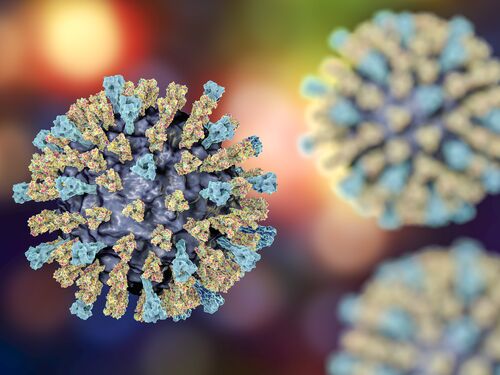
Mpox is an orthopoxvirus. It is related to variola, the orthopoxvirus that causes smallpox. Common symptoms include fever, swollen lymph nodes, and headaches, although these symptoms may not always occur. Usually, a rash also develops. In the 2022 outbreak, the rash most commonly occurred in the oral, anal, or genital area.
Chickenpox is a part of the herpes family of viruses, which is not related to the poxvirus family that includes mpox and smallpox. The same virus that causes chickenpox, the varicella-zoster virus, also causes shingles. The most common symptom of chickenpox is an itchy, blister-like rash. People with chickenpox may also run a fever, be tired, or lose their appetite.
Mpox is much less contagious than chickenpox.
Both viruses are spread through close contact, but chickenpox is much more contagious. It spreads through direct contact with someone who is infected. The chickenpox virus can also spread via the air, either from infected air breathed out by someone who is sick or from aerosols that contain infected fluid from the blisters. If you have not had chickenpox before or have not been vaccinated against chickenpox and you spend time around someone with chickenpox, the chances are extremely high that you will become infected.
Mpox also spreads from person to person through direct contact, including contact with the rash, scabs, or body fluids from someone infected with mpox. Unlike chickenpox, some animals can get mpox, too. Prior to the 2022 outbreak, most cases of mpox were transmitted from an animal to a person.
Mpox does not spread as readily from person to person as chickenpox does. People with mpox can have virus in their saliva and breathe out virus, but the virus does not spread easily long distances through the air. Transmission through respiratory secretions appears to occur through kissing and in other situations with prolonged face-to-face contact. The 2022 outbreak spread primarily through intimate contact.
We have effective vaccines for these diseases.
While most cases are not fatal, mpox and chickenpox can cause serious discomfort or illness and sometimes death. Fortunately, there are vaccines for these diseases. In the United States, a safe and effective vaccine against chickenpox has been a part of routine childhood immunizations since 1996. Cases of chickenpox in the United States have declined from roughly 4 million a year prior to the vaccine’s availability to fewer than 150,000 a year. If you have not already had chickenpox and have not received a vaccine, getting vaccinated is the best way to protect yourself from an infection.
A vaccine originally licensed for smallpox is available for prevention of both smallpox and mpox. Most people are at low risk of getting mpox, and there is currently not enough vaccine available to provide vaccinations to everyone. Therefore, the Centers for Disease Control and Prevention (CDC) currently recommends that people who have had close contact with someone with mpox receive the vaccine. It also recommends vaccination for:
Gay, bisexual, or other men who have sex with men, people who are transgender, and people who are nonbinary or gender-diverse and who, in the last 6 months, have had sex with multiple partners, had sex at a commercial sex venue, or had sex at an event where mpox transmission is occurring.
Gay, bisexual, or other men who have sex with men, people who are transgender, and people who are nonbinary or gender-diverse who have had a new diagnosis of one or more sexually transmitted diseases.
People who work in settings where there is a risk of being exposed to mpox, such as in a laboratory with orthopoxviruses or as part of a health care response team.
While most of the world’s population may be at low risk, mpox has been a public health concern for decades in countries where it is endemic. In August 2024, the World Health Organization declared a public health emergency of international concern after more than 15,000 cases and 500 deaths were reported in the Democratic Republic of Congo so far that year. In the summer of 2024, mpox cases were also reported in many neighboring countries, including four that had not previously reported cases. Making vaccines and drug therapies for mpox available in west and central Africa―along with greater support for health infrastructure and public health resources (including disease surveillance and response capabilities) in this region, particularly in rural areas―would reduce suffering in places where the disease is endemic and lower the risk of mpox outbreaks.
ADDITIONAL RESOURCES
More like this
Discover
Events
Right Now & Next Up
Stay in the loop with can’t-miss sessions, live events, and activities happening over the next two days.
NAS Building Guided Tours Available!
Participate in a one-hour guided tour of the historic National Academy of Sciences building, highlighting its distinctive architecture, renowned artwork, and the intersection of art, science, and culture.