Expanding Behavioral Health Care Workforce Participation in Medicare, Medicaid, and Marketplace Plans (2024)
Chapter: 4 Factors Contributing to the Expansion and Recruitment of Behavioral Health Providers Serving Medicare, Medicaid, and Marketplace Beneficiaries
4
Factors Contributing to the Expansion and Recruitment of Behavioral Health Providers Serving Medicare, Medicaid, and Marketplace Beneficiaries
The current system of mental health and substance use treatment in the United States is facing significant challenges, particularly in terms of access to care. As described in Chapter 3, several measures of supply and demand for behavioral health services indicate that many behavioral health care provider types (including psychiatrists, psychologists, and nurse practitioners) are maldistributed, with care providers being unevenly distributed geographically. The result is a critical shortage of behavioral health providers in many areas, particularly among underserved communities (Mauri et al., 2019; Zhu et al., 2022). Services for these high-need populations tend to be densely concentrated in a few areas, creating inequitable geographic accessibility. For other behavioral health care provider types, both maldistribution and outright shortages are a challenge. For example, among child and adolescent psychiatrists, there have been well-documented supply shortages across all areas of the country (McBain et al., 2019). As a consequence, certain high-risk populations, such as children and adolescents, are experiencing an increase in behavioral health distress while facing even more barriers to securing treatment (Harati et al., 2020; Office of the Surgeon General, 2021).
The shortage of behavioral health providers in certain areas has significant consequences for those seeking treatment. Individuals living in areas with limited access to mental health or substance use disorder (SUD) services often face long wait times for appointments—weeks if not months—which can delay or lead to inadequate treatment. This can have serious consequences for those experiencing mental health crises, as they may not access the care they need in a timely manner. Moreover, the lack of
behavioral health providers in certain areas can have a disproportionate effect on marginalized communities. Research has shown that individuals from racial and ethnic minoritized groups and those from low-income backgrounds are less likely to have access to behavioral health services. This can perpetuate health disparities and exacerbate existing social and economic inequalities.
To address these challenges, it is crucial to recruit mental health and SUD providers to areas where they are needed most. Doing so requires a multifaceted approach that includes targeted recruitment efforts, training and education programs, and financial incentives for behavioral health providers to offer care in more locations and to accept more patients facing increased disparities in access, including Medicaid-insured children and adolescents.
Request for Information from Behavioral Health Care Providers
Because of the limited evidence on behavioral health provider barriers to insurance participation in behavioral health, the committee conducted an electronic questionnaire of behavioral health providers across settings and care provider types using a public request for information (RFI). Respondents had access to the public RFI through the National Academies of Sciences, Engineering, and Medicine’s (National Academies) website or may have received an invited link through professional organizations, employers, or directly from the National Academies. To gather additional input from behavioral health clinicians, the questionnaire asked respondents to share their experiences working with Medicare, Medicaid, and Marketplace insurance programs and, if they did not participate in these insurance programs, to explain reasons for not accepting these insurances. The committee collected data in November and December 2023 using Alchemer Survey Software. Responses to the RFI were received from a wide variety of behavioral health professionals, both prescribing and non-prescribing. A total of 1,047 behavioral health professionals completed the questionnaire. Responses from the RFI are discussed later in this chapter.
WORKFORCE EDUCATION PROGRAMS
The Health Resources Services Administration (HRSA) oversees several programs that include innovative strategies to encourage behavioral health practitioners to work with Medicare and Medicaid beneficiaries with complex social, economic, and environmental needs, specifically those in medically underserved areas. HRSA’s Bureau of HealthCare Workforce supports two main behavioral health professions training grants to strengthen the workforce of behavioral health providers. The Behavioral Health Workforce
Education and Training (BHWET) program provides a funding mechanism for institutions to enhance the quality of education and clinical training in behavioral health and increase the number of practicing behavioral health professionals and health support workers. In particular, BHWET emphasizes integrating behavioral health into primary care, and given the acute need for child and adolescent services access, programs focusing on programming for children, adolescents, and transitional-age youth are among those that can apply for BHWET. The graduate psychology education (GPE) training program supports expansion of interprofessional training, with a focus on integrated behavioral health and primary care in doctoral-level health psychology programs.
BHWET and GPE outcomes indicate that the programs have increased the number of behavioral health professionals trained, with a significant number of BHWET and GPE program graduates choosing to practice in high-need areas. From 2014 to 2022, BHWET program awardees supported clinical training of 39,926 graduate-level behavioral health providers, and nearly 70 percent (27,522) graduated and entered the behavioral health workforce. Of the total graduated, 9,892 new health support workers began work as community health workers (CHWs), peer paraprofessionals, and substance use/addictions workers. Of the 17,630 new behavioral health professionals, there were 887 new psychologists; 10,738 new social workers; 1,352 new mental health nurse practitioners; 442 new marriage and family therapists; 4,044 new professional, school, addiction, or mental health counselors; and 80 new psychiatrists.
In the post-graduate employment data collected at one year follow up (2021 to 2022), 46 percent of BHWET graduates and 55 percent of GPE graduates worked in medically underserved communities (HRSA, 2024a). Both BHWET and GPS prioritize programs with a high or increased rate of graduates placed in practice settings focused on serving residents of medically underserved communities (HRSA, 2021). Taken together, outcome data from BHWET and GPE from over the past decade show they are affective at increasing the number of behavioral health professionals working with under-resourced populations. Furthermore, the BHWET and GPE programs have reduced projected behavioral health workforce shortages by 39 percent and are expected to have ongoing positive effects on the behavioral health workforce supply (HRSA, 2022a,b).
HRSA’s National Health Service Corps (NHSC) is another set of programs providing incentives for behavioral health professional to work in geographically underserved areas. NHSC provides scholarship and loan repayment programs for primary care, dental, and behavioral health providers. Health care providers accepted to the program receive loan repayment funding or scholarships in exchange for providing services at participating sites in health professions shortage areas (HPSAs, previously defined
in Chapter 3). NHSC has played a growing role in supporting behavioral health providers in these underserved areas; as of 2017, behavioral health providers accounted for nearly one-third of NHSC providers (Olson et al., 2020). In 2023, NHSC supported over 8,700 behavioral health providers (HHS, 2024b). Particularly relevant to shortages of child and adolescent care providers, child and adolescent psychiatrists (see Box 4-1) are among the physician provider types eligible for NHSC’s loan repayment program (HRSA, 2024b).
Congress has persistently underfunded NHSC, especially when viewed through a behavioral health lens. As of 2020, mandatory funding for NHSC had not increased significantly in a decade (Olson et al., 2020). A 2021
BOX 4-1
Child and Adolescent Psychiatrists
Historically, the United States has had a dearth of child and adolescent psychiatrists. While the number of child psychiatrists has increased in recent years, as of 2016 there were an estimated 9.75 child psychiatrists per 100,000 children; by contrast, the American Academy of Child and Adolescent Psychiatry estimates a need for 47 psychiatrists per 100,0000 children (McBain et al., 2019). Moreover, the existing supply of child and adolescent psychiatrists is concentrated in metropolitan areas, with 70 percent of counties having no behavioral health care providers. Demand far outstrips this supply, as recent data suggests an acute rise in the prevalence of youth diagnosed with depression, attention deficit/hyperactivity disorder, and bipolar disorders. Pediatric emergency visits for mental health conditions have also increased, with high rates of revisits along with low rates of post-emergency department outpatient follow-up. Together, these data underscore the fact that inadequate access to pediatric specialty outpatient care and intervention may play a role in these trends.
There have been multiple proposals to expand the child psychiatry workforce, including early career exposure and enrichment programs, developing alternative and expedited child psychiatry residency programs, and improving coding and billing requirements to account for the complexity of caring for children and adolescents with behavioral health needs. In addition, consultation and integrated, team-based care models that include child psychiatry have been implemented to improve the capacity of present and future specialists.
SOURCES: Bommersbach et al., 2023; Cushing et al., 2023; Hoffmann et al., 2023; McBain et al., 2019; Shapiro, 2022.
Government Accountability Office study found that in fiscal year 2020, 43 percent of behavioral health care providers who newly applied to receive awards from NHSC were denied. NHSC’s largest program, the General Loan Repayment Program, rejected hundreds of applicants despite them having HPSA scores in the upper range that would have received awards per HRSA guidance if more funding had been available. In this same year, relevant to behavioral health, more than 10 percent of treatment sites had unfilled positions for licensed clinical social workers and licensed professional counselors (GAO, 2021).
Finding: HRSA’s Bureau of Health care Workforce Education and Training and Graduate Psychology Education programs have been shown to have ongoing positive impacts on behavioral health workforce supply, including reducing projected behavioral health workforce shortages by 39 percent and increasing the number of behavioral health professionals and support specialists of multiple disciplines working with under-resourced populations. HRSA’s National Health Services Corps program has similarly increased the supply of physicians providing behavioral health services to under-resourced populations. These are populations that disproportionately enroll in Medicare, Medicaid, and the Affordable Care Act Marketplace.
Conclusion 4-1: In addition to short-term improvements in behavioral health care provider participation among the existing workforce, strengthening the pipeline of federally subsidized behavioral health providers would build a workforce more likely to continue serving Medicare and Medicaid populations after the end of their training. Bolstering workforce programs and policies, including successful pathway or pipeline programs, would increase the number of people who want to enter the behavioral health field and support care provider retention over time.
DIVERSE REPRESENTATION IN THE BEHAVIORAL HEALTH WORKFORCE
Racial, ethnic, gender, and sexual minoritized individuals often suffer from poorer mental health outcomes resulting from complex social, economic, and environmental needs, including inaccessibility of high-quality behavioral health care services, cultural stigma surrounding mental health care, discrimination, an overall lack of awareness about mental health, and a lack of access to appropriate care for racially, ethnically, culturally, and linguistically diverse populations. For example, patients of minoritized identity enrolled in Medicaid/Child Health
Insurance Program (CHIP) and in Medicare Advantage experience disparities in mental health and SUD care access and quality; over half of Medicaid/CHIP beneficiaries are of a racial or ethnic minoritized identity, with Hispanic and non-Hispanic Black individuals accounting for a disproportionate share of Medicaid/CHIP beneficiaries (CMS, 2023c; MACPAC, 2021). In addition, the 1.2 million lesbian, gay, bisexual, and transgender Medicaid beneficiaries have higher rates of self-reported unmet mental health and substance use care needs than their non-minoritized counterparts (MACPAC, 2022; Ochieng et al., 2023). It should be noted that relying solely on minority mental health providers to address access disparities for Medicaid-insured patients and those in shortage areas overlooks the need for broader workforce diversity. The concept of racial concordance, pairing non-white providers with patients to reduce health inequities, assumes certain advantages but risks perpetuating segregation in healthcare, reinforcing systemic biases favoring white populations (Boyd, 2019).
Physician acceptance of Medicaid is lower in areas with higher concentrations of racial and ethnic minoritized individuals (Daly and Mellor, 2020; Greene et al., 2006). Medicaid-insured individuals of Black or African American identity have less access to substance use disorder (SUD) treatment (Heflinger et al., 2006; Stein et al., 2018). An analysis of six Medicaid programs found that Black or African American and Hispanic Medicaid beneficiaries were less likely to receive behavioral health services in community-based settings than their White counterparts and that Black or African American beneficiaries were more likely to receive services in inpatient and emergency room settings than their White counterparts (Samnaliev et al., 2009). Medicaid-insured Black or African American and Hispanic children are less likely to receive behavioral health services than their White counterparts (MACPAC, 2022).
Enrollment in Medicare Advantage has increased more rapidly among racial and ethnic minoritized Medicare beneficiaries than among their White counterparts, and as of 2021 more than half of Black, Hispanic, and Asian/Pacific Islander Medicare beneficiaries were enrolled in a Medicare Advantage plan (Ochieng et al., 2023). A 2023 review from the Kaiser Family Foundation examined disparities in quality-of-care metrics by race and ethnicity in the Medicare Advantage program, finding that racial and ethnic minoritized individuals fared poorly compared with White enrollees on most metrics, including access to medication and appropriate follow-up care (Ochieng et al., 2023).
As the 2023 National Academies’ report Federal Policy to Advance Racial, Ethnic, and Tribal Health Equity (NASEM, 2023) noted, cultural congruency between patient and health care professional (e.g.,
concordance in race, ethnicity, and language) improves patient satisfaction and affects outcomes for racial and ethnic minoritized patients (Diamond et al., 2019; Jones et al., 2017; Ku and Vichare, 2023). Indeed, race concordance between behavioral health care provider and patient has been associated with higher self-report of satisfaction with care and self-report of receiving better quality care among Black and Hispanic patients (Cooper et al., 2003; Saha et al., 1999). A 2023 study provides a recent compelling example, finding that higher Black representation in the primary care physician workforce was associated with higher life expectancy and lower all-cause mortality among Black patients (Snyder et al., 2023).
A 2011 meta-analysis of the literature on this phenomenon specific to behavioral health care examined three variables regrading racial and ethnic match between patient and therapist: patient preference, the patient’s positive versus negative perception of therapist, and treatment outcome (Cabral and Smith, 2011). The meta-analysis revealed that patients preferred receiving treatment from therapists who were racially and ethnically concordant and that racial and ethnic minoritized patients had positive perceptions of race- and ethnicity-matched therapists. For Black or African American patients, these associations were particularly strong, and there was also an association between racial and ethnicity match and positive treatment outcome (Cabral and Smith, 2011. Thus, as the above-cited 2023 National Academies report concluded, “A lack of inclusion and representation in the health care workforce may perpetuate health inequities, given the evidence that suggests better health outcomes when there is identity concordance between patients and providers” (NASEM, 2023, p.118).
Beyond the benefit of specifically addressing disparities for historically marginalized communities, there are data suggesting that increased representation of racial and ethnic minoritized identity in the behavioral health care provider workforce could more broadly improve access to the Medicaid program. Research examining the self-reported practice characteristics of minorized and non-minoritized physician graduates of seven California medical schools found that minoritized physicians saw a higher percentage of Medicaid-insured patients than their non-minoritized counterparts. In addition, a higher proportion of minoritized physicians reported practicing in an area with a shortage of health care providers (Davidson and Montoya, 1987). A 2019 survey of physicians, nurse practitioners, and physician assistants on Medicaid acceptance following the Medicaid expansion found that racially minoritized care providers were more likely to report accepting new Medicaid patients, with Black-identifying physicians exhibiting the highest likelihood (Tipirneni et al., 2019). An analysis of data
from the 2010 Medical Expenditure Panel Survey found that Medicaid-insured adults were more likely to receive care from care providers of racial or ethnic minoritized identity than from White physicians (Marrast et al., 2014). These data suggest that efforts to increase representation of racial or ethnic minoritized health care providers in the behavioral health care workforce could benefit all Medicaid beneficiaries by increasing access to care.
Additional study of best practice for increasing representation of individuals with minoritized identities in the health care workforce is needed, though some existing literature highlights promising directions and approaches. A report from the National Council on Mental Health Wellbeing addressed the factors affecting the recruitment and retention of staff of color, particularly Black or African American men (National Council for Mental Wellbeing, 2022). The report provides findings from two focus groups conducted with Black and African American male mental health and SUD professionals. Focus group participants highlighted the lack of diversity at the leadership and executive level of health care organizations as well as the stigma and historical mistrust of health care institutions in Black and African American communities as factors deterring Black and African American men from pursuing behavioral health careers. The participants also highlighted issues related to pay, noting that African Americans face race-based pay inequities, further complicating issues related to salary and wages. This report’s recommendations to address recruitment barriers include increasing community education to address stigma; increasing partnerships with community-based organizations, particularly faith-based organizations, to address historical mistrust; and providing higher wages and flexible financial support options such as loan repayment, housing stipends, and retirement plans to address the pay barriers. The report further recommends increasing technical assistance resources for mental health and SUD treatment organizations to enhance their understanding of recruitment strategies and establishing learning communities across organizations to share ideas on recruitment strategies and mentorship programs (National Council for Mental Wellbeing, 2022).
HRSA’s NHSC program has proven to increase diversity in the workforce and increase the workforce serving the underserved–largely Medicaid patients. The demographics of the NHSC workforce compared with the national workforce reflects NHSC’s effect on health care provider workforce diversity. A 2020 study reported that among the NHSC workforce, 13 percent of health care providers identified as Black or African American, 10 percent as Hispanic, 7 percent as Asian or Pacific Islander, and 2 percent as American Indian or Alaska Native. Data from 2016 show that 17 percent of NHSC physicians identified as Black or African American compared
with the 4 percent of physicians who identify as Black or African American nationally (Olson et al., 2020).
Several decades of evidence support the association between participation in pathway or pipeline programs—programs that support and increase educational opportunities for systematically and structurally excluded students, including from underrepresented racial and ethnically minoritized populations—and increased matriculation in medical school (Taylor et al., 2022) and health professions in general (HHS, 2009) among students of these backgrounds. Federal pipeline and pathway programs with a proven track record of success include the HRSA’s Health Careers Opportunity Program (HCOP) (HRSA, 2022c), Centers of Excellence Program (COE) (HRSA, 2023a), and Nursing Workforce Diversity Program (NWD) (HRSA, 2023b). HCOP and COE provide grants to health profession schools, including medical schools and behavioral health graduate programs. HCOP grantees provide social and educational supports to increase matriculation of high school and undergraduate students from disadvantaged backgrounds, while COE grantees enhance education resources in health professions schools to support increased diversity and address minority health. NWD aims to increase nursing education opportunities for individuals from disadvantaged backgrounds.
Between 2015 and 2020, 6,856 students participated in HCOP, over 70 percent of whom were from underrepresented racial and ethnic minoritized backgrounds. Their graduation rates from high school or secondary school met or exceeded national averages, and a significant proportion indicated that they intended to continue on to health professions school (HRSA, 2022c). Over 16,000 individuals completed COE programs between 2015 and 2020, with 96 percent of the participants from an underrepresented racial and ethnic minoritized background and 58 percent of those who completed a graduate-level program intending to work or train in a medically underserved community (HRSA, 2023a). Between 2014 and 2019, over 15,000 trainees graduated from NWD programs. Black and African American and Hispanic and Latino representation among NWD nurses was two to five times higher than national averages, and more than half of NWD training sites provided services to individuals with complex needs, including those with lower income, older adults, and individuals with disabilities (HRSA, 2023b).
Finding: Patients of racial/ethnic minoritized identity experience disparities in behavioral health care, including poorer quality of care and lesser access to care, and are over-represented among Medicaid beneficiaries. They also constitute a rapidly growing proportion of Medicare Advantage beneficiaries.
Finding: Evidence supports improved satisfaction and outcomes for racial and ethnic minoritized patients when there is racial and ethnic concordance between patient and health care provider. Data also suggests that health care providers of racial and ethnic minoritized identity are more likely than behavioral health care providers of other racial or ethnic identities to participate in Medicaid.
Finding: Participation in pathway or pipeline programs is consistently associated with increasing the matriculation of students of minoritized racial/ethnic identity in some health professions schools.
Conclusion 4-2: The behavioral health workforce does not reflect the diversity of the population it serves. Increasing historically underrepresented racial and ethnic identities, as well as language and cultural representation, in the behavioral health workforce is one mechanism to address disparities in access to care facing Medicaid and Medicare programs. Within Medicaid specifically, increased representation of historically underrepresented racial and ethnic identities in the health care workforce could expand access to care for beneficiaries more broadly, regardless of identity.
Conclusion 4-3: Efforts to decrease stigma, dispel historical mistrust, and provide financial incentives associated with behavioral health professions may address recruitment barriers, particularly those affecting communities of color.
GRADUATE MEDICAL EDUCATION FUNDING
The committee considered the current structure and distribution of graduate medical education (GME) funding, given the role that Medicare and Medicaid play in supporting GME as well as the potential for training environment to be a factor in incentivizing or disincentivizing future participation in Medicare, and Marketplace programs among health care providers-in-training. A 2014 Institute of Medicine report, Graduate Medical Education That Meets the Nation’s Health Needs, stated that “Medicare GME payments are based on statutory formulas that were developed at a time when hospitals were the central—if not exclusive—site for physician training” (p. 61). The rules, codified in 1997, continue to reflect that era (IOM, 2014). Most GME funding continues to be paid to hospitals, even though inpatient care is decreasing, outpatient care is increasing, and the training of physicians has not shifted to reflect this reality.
The Centers for Medicare & Medicaid Services (CMS) has the opportunity to influence the supply of the nation’s physicians. Medicare is the largest source of federal GME funding, and Medicaid is the second largest source of support for GME. In addition, the federal government shares payment for Medicaid expenses through federal matching funds (Heisler et al., 2018; Mitchell et al., 2023).
While GME funding has not changed, the country’s health care delivery system continues to undergo dramatic changes. A 2018 report illustrates the growing role of outpatient settings in health care delivery. Per this report, while hospital inpatient stays declined by 6.6 percent between 2005 and 2015, outpatient visit increased by 14 percent, and gross outpatient revenue per visit increased by 45 percent (Abrams et al., 2018). A figure from this report (Figure 4-1) demonstrates the increasing proportion of hospital revenue generated by outpatient care.
Despite this ongoing change, CMS has not changed the basic formulas and processes it uses to fund residency training, nor has CMS accounted for
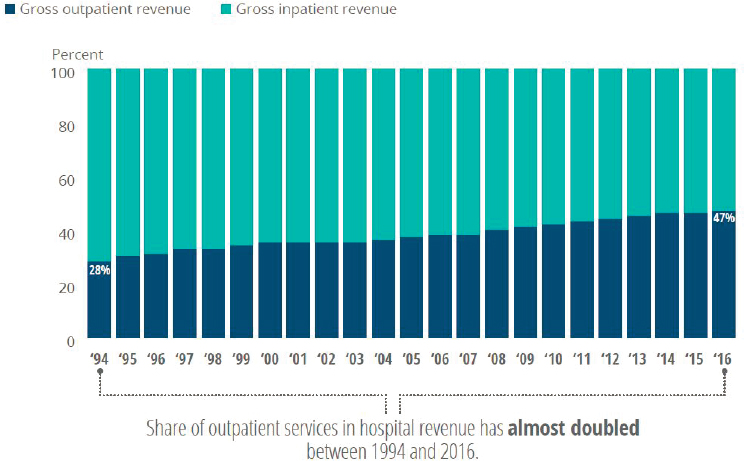
NOTE: The figure is based on Deloitte analyses, using data from the American Hospital Association annual survey and Medicare cost reports via Truven Health Analytics.
SOURCE: Abrams et al., 2018.
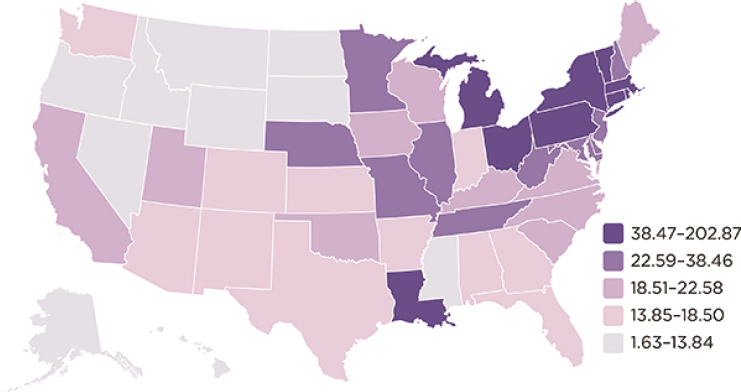
SOURCE: Mullan et al., 2013.
geographic maldistribution of residency slots which are currently concentrated in the Northeastern states (Figure 4-2). While Congress passed legislation calling for CMS to add 1,000 Medicare-funded residency training slots over 5 years, with a focus on geographic needs—the first such increase since 1997 (Schleiter Hitchell and Johnson, 2022)—adding 200 physician slots across the country per year will not align the country’s physician supply with the needs of the country, particularly in the case of psychiatrists. Even if all 1,000 residency slots were solely for training psychiatrists, psychiatrists are the physician specialty with the lowest acceptance of Medicare and Medicaid. In addition, other than the ongoing addition of 1,000 residency training that began in 2023, Medicare-supported training slots are essentially frozen where they existed almost two decades ago, perpetuating inequities in the geographic distribution of training slots and ignoring changes in the geography and demography of the U.S. population (GAO, 2017).
When initially legislated, CMS calculated Medicare Graduate Medical Education (GME) payments to teaching hospitals based solely on hospitals’ costs. In 1983, CMS established two GME funding streams for teaching hospitals: (1) Direct Graduate Medical Education (DGME) funding to cover the direct expenses associated with residency training (e.g., residents’ and faculty salaries and benefits and certain administrative and overhead costs); and (2) Indirect Medical Education (IME) funding, an adjustment to individual teaching hospitals to help defray the additional costs of providing patient care associated with sponsoring residency programs. Of the more
than $15 billion CMS pays annually to hospitals, approximately one-third is paid as DGME and two-thirds as IME. Physicians who train in Medicare or Medicaid-supported residencies are under no obligation to accept Medicare or Medicaid patients when they enter practice, nor are they required to provide any other services to these programs, despite CMS largely paying for their training (IOM, 2014).
Medicare GME funding is formula-driven and does not take into account national health care needs or priorities. The GME financing system offers little incentive to improve the quality or efficiency of physician training and no incentive for institutions to align residency slots with local or national health care needs. It does incentivize adding residency slots to training programs that allow hospitals to care for higher-cost, often procedure-based specialty care, as opposed to primary care or behavioral health care (IOM, 2014). In addition, because the Medicare formulas are linked to Medicare patient volume, the system disadvantages children’s hospitals, safety net hospitals, and other training sites that care for mostly non-elderly patients (IOM, 2014).
Research has shown that psychiatric mental health nurse practitioners (PMHNPs) have begun to provide an increasingly large percentage of necessary care to Medicare-insured behavioral health patients. A recent analysis of Medicare claims for office visits demonstrated a 162 percent increase in PMHNPs serving Medicare patients from 2011 to 2019, while the number of psychiatrists billing Medicare dropped 6 percent during this same period. Over the same period, the growth in the PMHNP workforce mitigated losses in mental health specialist visits—while psychiatrist-provided visits dropped by 30 percent, the net decrease in behavioral health specialist visits was just over 10 percent because of the increase in PMHNP-provided visits (Cai et al., 2022).
However, Medicare does not support training programs beyond those for physicians even though non-physicians treat a growing percentage of Medicare beneficiaries in higher-need specialties. Aside from primary care physicians and psychiatrists, Medicare does not financially support the training of the behavioral health workforce needed to deliver services to those covered by Medicare. It does not support advanced practice registered nurses (APRNs), social workers, or psychologists despite both a national mental health crisis and national SUD crisis. The need continues to grow, but CMS has not redistributed the dollars to support the workforce in a way that reflects this current reality. Even among physicians and in the midst of an ongoing opioid crisis. In the CY 2024 PFS (Physician Fee Schedule) final rule, CMS finalized addiction counselors or drug and alcohol counselors who meet the applicable requirements to be a mental health counselor (MHC), could enroll in Medicare as MHCs (CMS 2023a).
HRSA has used funding to create the Teaching Health Center Graduate Medical Education (THCGME) program, which helps communities grow their health workforces by training physicians and dentists in community-based settings, with a focus on rural and underserved communities. The THCGME program funds the majority of training in the community-based outpatient settings where most people receive their health care, such as community health centers. Teaching health centers receive a payment for each resident they train to cover the training costs, including the resident’s salary and benefits. In many ways, THCGME resembles CMS’ Medicare IME and DGME funding.
An analysis of the THCGME program shows significant retention of the workforce serving these communities. Patients seen in these settings are largely Medicare and Medicaid beneficiaries. THCGME graduates were significantly more likely than other graduates to practice in a rural location, to practice within 5 miles of their residency program, and to care for medically underserved populations. Their scope of practice was wider than other graduates and more likely to include services such as buprenorphine prescribing and behavioral health care (Davis et al., 2022), even though this program supports medical training, not behavioral health training.
Given this success, the committee believes that both the Substance Abuse and Mental Health Services Administration (SAMHSA) and CMS have an opportunity to increase funding for such programs. As the 2014 National Academies report Graduate Medical Education That Meets the Nation’s Health Needs (IOM, 2014) suggests, CMS can create one Medicare GME fund with two subsidiary funds:
- A GME operational fund to distribute ongoing support for residency training positions that are currently approved and funded.
- A GME transformation fund to finance initiatives to develop and evaluate innovative GME programs, determine and validate GME performance measures, pilot alternative GME payment methods, and award new Medicare-funded GME training positions in priority disciplines and geographic areas (see Figure 4-3). This could include changes and enhancements both from the Center for Medicare and Medicaid Innovation and Section 1115 waiver authorities1 to states to increase the federal medical assistance percentage matching funds to support state-based investments in behavioral health workforce training.
___________________
1 Section 1115 waiver authorities allow states to test new approaches to administering Medicaid and CHIP programs beyond what is required by federal statute.
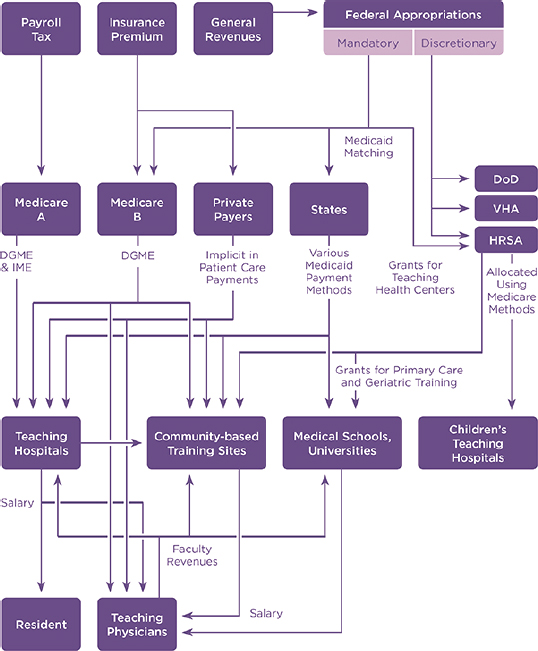
SOURCE: IOM, 2014.
While the 2014 National Academies report recommendations were specific to CMS, SAMHSA, with a necessary and appropriate focus on the behavioral health workforce beyond physicians, can:
- Either work in partnership with HRSA to develop integrated training programs for both primary care and behavioral health, or
- Use discreet and directed grant funding to create a behavioral health teaching health center—or other specific setting—to train the behavioral health workforce. This grant funding should be multi-year funding to both establish and continue training programs for the life of the training period, which would avoid trainees not completing their training because of a lack of funding. Modeling this largely after the THCGME training program, if done de novo, would allow for a successful blueprint for many aspects of initial implementation and ongoing evaluation, assessment, and impact.
Finding: CMS provides significant funding to support physician training; SAMHSA likewise provides significant funding to support training and care delivery. These funding streams do not require recipient institutions to report on long-term outcomes regarding career choice, practice environment, or service provision to Medicare and Medicaid beneficiaries.
Finding: Teaching Health Center Graduate Medical Education (THCGME) Programs support significant retention of workforce serving the communities where these programs are in place. Patients seen in these settings are largely Medicare and Medicaid beneficiaries.
Conclusion 4-4: There is a demonstrated inconsistency between the primary source of GME program funding (e.g., Medicare and Medicaid) and participation in public insurance programs among health care providers whose training is funded by GME. While GME program funding primarily comes from Medicare and Medicaid, many trainees do not subsequently participate in these programs.
BILLING CAPABILITY FOR BEHAVIORAL HEALTH CARE PROVIDERS-IN-TRAINING IN MEDICARE, MEDICAID, AND ACA MARKETPLACE INSURANCES
Because CMS has long permitted those in medical residency training programs to bill Medicare and Medicaid under the supervision of an attending physician, the committee considered billing capability for behavioral health care providers-in-training as a potential factor that might incentivize those in training to participate in Medicare, Medicaid, and Marketplace programs after completing their training. The access and availability of high-quality supervised training opportunities for behavioral health trainees remains one of the most critical issues in behavioral health workforce development and behavioral health care provider participation in public health insurance programs.
There is a shortage of clinical training sites across behavioral health professions (BHWAC, 2022). Increasing the availability of training sites, which can provide supervised training toward licensure, certification, or other requisite credential to practice, requires sustainable funding. Such funding can be severely lacking for many behavioral health clinical training sites. CMS allows reimbursement for teaching physicians, interns, and residents in certain approved settings and training programs (CMS, 2023b), but there is no corresponding comprehensive guide or policy for non-physician behavioral health trainees. Similarly, these trainees are not eligible for funding through GME that would help subsidize the cost of required residency training (APA, 2022a).
Existing mechanisms for billing by supervised trainees can vary greatly by state, profession, insurance plan, and practice setting. For example, some states allow psychology trainee billing under various mechanisms, such as trainee license, registration, or under the “incident to” billing provision (APA, 2014). Such practices are not permissible under Medicare, however (APA, 2022b). The American Psychological Association, for example, has stated that not allowing billing for services provided by trainees “presents a significant challenge to training programs that offer needed services to the public yet must find other ways to support the costs associated with running a quality training program” (APA, 2014).
Responders to the committee’s RFI raised many of these training and billing issues (see Table 4-1 for a selection of relevant quotes from RFI responders).
While various solutions and workarounds have been implemented, including apprenticeship programs and grant funding for training sites (i.e., BHWET and GPE grant programs discussed earlier), allowing billing for services provided by trainees under an approved supervisor or preceptor might be a more comprehensive, equitable, and scalable approach to this problem. One proposal, for example, calls for Congress to create a billing modifier that Medicare, Medicaid, and commercial payers would use to bill for services performed by trainees under supervision (Gajewski et al., 2022). This proposal would include “an additional 10 percent of the base code’s Medicare fee, compensating training sites for the time clinicians spend teaching” (Gajewski et al., 2022). Under this policy, a teaching practice would generate 10 percent more reimbursement revenue than a private practice clinician for providing any mental health service involving a resident. The proposed policy would offset the cost of supervision and enable teaching practices to offer more competitive salaries to prospective clinical educators. The policy should apply to all payers if it is to create a reliable revenue stream that encourages practices to treat every patient equitably.
Creating a pathway in which all mental health and SUD trainees can provide reimbursable services with Medicare, Medicaid, and Marketplace plans would not just increase the supply of workers. It would help build a pipeline of behavioral health care providers who would be more likely to continue serving these populations after their training ends. Research has linked health care provider retention to training programs and training (Bazemore et al., 2015; Dahal and Skillman, 2022). In other words, creating such a pathway would make it feasible to develop training sites across different practice settings where public insurance beneficiaries receive services, thereby covering the cost of training and increasing the odds of more behavioral health providers “staying where they train” and providing services to these populations long-term, post-graduation, in permanent, non-training positions.
TABLE 4-1 RFI Selected Quotes: Trainee Issues
| “As a trainee in Florida, I was unable to work with any Medicaid populations, which left a major gap in my training.” |
| “As a trainee, I am unable to work with Medicare patients, which feels arbitrary, means that our Medicare patients may have to wait longer for services, and limits my training since I rarely if ever see older adults.” |
| “My primary concern is that Medicare doesn’t allow trainees (neuropsychology interns and fellows) to see patients. This is a huge problem, as it impedes the ability of our trainees to gain experience with the aging population.” |
| “Our training clinic is a community mental health center, and most patients have Medicare/Medicaid. Without our clinic, access to services would be limited, and we would not be able to train future clinicians on campus.” |
| “It’s difficult as a CSWI [clinical social work intern] to work with Medicaid. Medicaid makes it very difficult for CSWIs to be credentialed because they have to apply for a different provider type. This limits access to care and makes more hurdles for patients. Interns should be able to bill Medicaid just as easily as we can bill private insurance.” |
| “Our Behavioral Health Clinic (Illinois) is able to bill for intern and extern therapy services, which is a huge factor in having sufficient providers and sustaining our training program’s budget. However, there isn’t a good mechanism for billing testing (e.g., no equivalent in Medicaid for 96138). This has led to a lack of available staff and huge waitlists (over a year).” |
| “Currently, I’m in leadership in an FQHC [federally qualified health center]. In NV, licensed MH [mental health] interns (of any licensure) and LCPCs [licensed clinical professional counselors] cannot bill Medicaid under the FQHC provider type. This is a huge barrier in a state with a significant provider shortage.” |
| “At our institution, all providers are enrolled with Medicare and Medicaid, and I see many patients who are covered by Medicaid in particular. One significant barrier is that, at least in NC where I practice, psychology trainees (such as students in psychology Ph.D. programs who are completing practicum experiences or predoctoral psychology interns) cannot bill for services they provide to patients with Medicaid. This is an unnecessary barrier to care for patients with Medicaid, since psychology trainees provide services under the close supervision of a licensed psychologist and can certainly provide high-quality services.” |
| “I am grateful for the mental health coverage my patients have with Medicare; however, with the aging population, our clinic receives more referrals than can be accommodated by licensed psychologists. The restrictions on trainees seeing government pay sources places undue barriers to care for our patients. In addition, our patients with Medicaid are unable to receive mental health services at our facility as psychologists in the state of Georgia are not reimbursed by Medicaid. We would be able to serve more patients if psychologists in the state of Georgia were reimbursed by Medicaid and if my trainees could see patients independently.” |
| “It is pretty easy for me as a provider—my institution accepts versions of all 3. The challenge is my trainees cannot see Medicare patients, nor most privately insured patients, so I don’t take the patients.” |
| “I am a licensed clinical social worker, licensed at the highest level possible in the state. Medicare and Medicaid do not reimburse for my services or those provided by my trainees. This is a disservice to underserved patients who need treatment.” |
| “We accept Medicaid in our clinic, but it’s been a challenge since unlike some other insurance companies that allow psychology doctoral trainees to bill under their licensed and credentialed supervisor (the way medical residents do), Medicaid does not. This limits our ability to serve this population and leads to our Medicaid waitlist of over a year, probably more like two years for psychological assessment services. In our small rural area that lacks providers, especially those who take Medicaid, this is a huge disservice.” |
| “There are many students/trainees who would enter this field if Medicare reimbursement rates provided a full income or at least enough of a full income to allow medical centers to easily hire them.” |
NOTE: 96318 = CPT code 96138 is used to bill for the first 30 minutes spent by a technician administering and scoring psychological or neuropsychological tests. This includes situations where at least two tests are administered, whether they are paper-based, verbal, or electronic.
Finding: While CMS allows for physicians-in-training to bill for services under the supervision and license of a preceptor, similar parity does not exist for other behavioral health professionals. This limits non-physician behavioral health trainee exposure to caring for Medicare and Medicaid beneficiaries and has a strong potential to influence which patients these health care providers serve when they finish training.
Conclusion 4-5: The lack of billing for services provided by trainees in Medicare and Medicaid is a major barrier to expanding training opportunities for behavioral health specialists more likely to participate in the Medicare and Medicaid programs.
BILLING COVERAGE OF NON-LICENSED BEHAVIORAL HEALTH PROVIDERS AND SERVICES
A substantial body of evidence, encompassing over 100 randomized, controlled trials, underscores the viability, feasibility, and clinical efficacy of behavioral health care delivery by non-specialist care providers, including CHWs, peers, lay individuals, and nurses (Barbui et al., 2020). These interventions are rooted in community contexts and require sustained collaboration, funding, training, support, and monitoring. Known throughout the literature as “task sharing,” this approach entails community-driven identification and delivery of behavioral health care, also called community-initiated care (CIC). CIC involves empowering local communities to implement evidence-informed programs for behavioral health prevention and intervention. This departs significantly from the predominant focus on specialist-delivered care, acknowledging the pivotal role that caregivers and frontline workers can play in addressing community behavioral health needs.
Behavioral health support specialists, such as peer support specialists (PSSs), CHWs, and paraprofessionals, play a crucial role in bridging the gap between individuals and traditional treatment settings and improving outcomes for individuals with complex social, economic, and environmental needs. Research has shown that PSSs significantly improve the overall effectiveness of behavioral health treatment for individuals with serious mental illness by decreasing substance use, decreasing depressive and psychotic symptoms, decreasing emergency department use and admission rates, and reducing costs (Davidson et al., 2012). People living with serious mental illness also report increased self-control, increased self-esteem and confidence, and increased empowerment when working with a PSS (Davidson et al., 2012). The positive benefits of peer support are captured by the following comment from Keris Jän Myrick during the committee’s webinar, Lived Experiences in Accessing Behavioral Health Care Services Through Public Insurance Programs:
The power of peer support was super helpful for me, especially because there are not a lot of providers of color . . . (F)inding a peer who looked like me and has the same cultural background as me, also helped me on my recovery journey.
A growing body of research supports the role of CHWs in improving behavioral health outcomes for lower income and racial/ethnic minority patients across the lifespan (Barnett et al., 2018). A 2021 issue brief from the CMS Office of Minority Health highlights the roles of CHWs in improving outcomes for vulnerable populations, including those with limited English proficiency and those living in rural communities (CMS, 2021). Given the evidence supporting the role of PSSs and CHWs in improving the mental health outcomes of individuals with complex needs, expanding this workforce’s reach within the Medicare and Medicaid-insured population has the potential to improve outcomes for Medicare and Medicaid beneficiaries with such needs. A 2024 SAMHSA report noted the growth in reimbursement opportunities for PSS services in public insurance programs and highlighted persistent challenges in actual use of these billable services on behalf of beneficiaries with behavioral health conditions. Specifically, the report notes that 48 out of 50 state Medicaid plans include PSS-delivered care as a reimbursable service and that the 2023 Consolidated Appropriations Act newly allows for direct reimbursement of PSS services for behavioral health conditions under Medicare (SAMHSA, 2024). Despite the broad availability for billing under Medicaid, a low proportion of Medicaid beneficiaries with behavioral health conditions were found to actually have received these services. The fee-for-service payment model was highlighted as a key barrier; other issues noted as barriers to PSS workforce expansion included low compensation, infrastructure challenges, and an absence of operational content and guidance (SAMHSA, 2024). Similarly, though interest is growing, even fewer states allow Medicaid payment
for services provided by CHWs (Haldar and Hinton, 2023), and allowable services are often limited in scope and target population (MACPAC, 2022).
SAMHSA established core competencies and a National Model Standards for PSS Certification to assist states in establishing a certification framework (SAMHSA, 2023a,b). More extensive use of PSSs and CHWs will require implementing standardized training and competencies to ensure that these important members of the team deliver care in a high-quality and effective way. A 2023 report, Filling the Gaps in the Behavioral Health Workforce, highlights this need and includes several policy recommendations that could support expanding the behavioral health workforce. These recommendations include creating a set of core competencies for behavioral health support specialists (BHSSs) at the federal level, creating pathways for improved coverage of BHSSs within the Medicare and Medicaid programs, and establishing a minimum federal exemption to becoming a BHSS for those convicted of nonviolent crimes (Gilbert et al., 2023). The recognition of Peer Support by Medicare could pave the way for broader adoption by Advantage Plans and other insurance companies, promising widespread integration in the future.
This report also calls for Congress to create a pipeline program to help interested BHSSs become licensed and to expand existing federal funding streams to support CIC programs (Breuer et al., 2023; Kohrt et al., 2023; Siddiqui et al., 2022). The report further called on Congress to help speed and spread the adoption of CIC programs by integrating existing federal funding streams that support CIC-related programs and those that support the work of BHSSs to help distribute the responsibility of behavioral health support into the community.
Finding: The presence of behavioral health support specialists, such as peer support specialists, community health workers, and other community-based paraprofessionals, plays a crucial role in bridging the gap between individuals and traditional treatment settings. These paraprofessionals have been shown to improve behavioral health outcomes for individuals with complex needs.
Finding: Including and using BHSSs in public insurance programs has been hampered by multiple factors, including lack of a standardized set of core competencies across the nation for certification, lack of payment structures that allow BHSSs to operate as part of a team, and federal funding streams that perpetuate the continuation of BHSS services outside of Medicare and Medicaid.
Conclusion 4-6: Expanding the delivery of behavioral health support specialist (BHSS) services in Medicare and Medicaid has the potential to significantly improve access and outcomes, especially for individuals with complex needs, while also augmenting the reach of licensed
behavioral health professionals. Federal intervention is crucial to establish BHSSs through model national certification standards and flexible payment models that facilitate the integration of these services into the full continuum of behavioral health care.
TELEHEALTH AND EXPANDED LICENSURE TO ADDRESS BEHAVIORAL HEALTH PROVIDER MALDISTRIBUTION
Expanding the delivery of behavioral health services via telehealth is one avenue for improving access to care and addressing the maldistribution of the current behavioral health workforce across areas of need (Guth, 2023). The following section considers the evidence on the role that occupational compacts play in expanding the reach of the current behavioral health workforce via telehealth, thereby addressing workforce maldistribution. Chapter 6 addresses other elements of telehealth relevant to expanding access to behavioral health services, including issues of modality, payment parity, and coverage parity.
In March 2020, during the COVID-19 public health emergency, the federal government and individual state governments provided temporary, specific telehealth flexibilities, including temporary licensure waivers to allow for clinicians to deliver telehealth services across state lines and for retired clinicians to reinstate their licenses. While some of these changes remain, much of the flexibility around licensure ended with the public health emergency.
Multiple stakeholders are encouraging states to permanently streamline licensing for all licensed care providers, in particular for licensed telehealth care providers. States approach licensing flexibility using a variety of mechanisms, including interstate compacts, licensure by endorsement or reciprocity, special-purpose telehealth registries or licenses to deliver telehealth services, and exceptions to in-state licensure requirements under certain circumstances and for telehealth services.
Thirty-nine states and the District of Columbia are now members of the Interstate Medical Licensure Compact for physicians. As the Center for Connected Health Policy explains, “When telehealth is used, it is considered to be rendered at the physical location of the patient, and therefore a care provider typically needs to be licensed in the patient’s state. A few states have licenses or telehealth specific exceptions that allow an out-of-state provider to render services via telemedicine in a state where they are not physically located or allow a clinician to provide services via telehealth in a state if certain conditions are met (such as agreeing that they will not open an office in that state). Still other states have laws that do not specifically address telehealth and/or telemedicine licensing, but make allowances for practicing in contiguous states, or in certain situations where a temporary license might be issued provided the specific state’s licensing conditions are met” (CCHP, 2024).
Occupational compacts are one pathway to decreasing the barriers for licensed clinical providers seeking to practice telehealth in a state other than their state of residence and are a facilitator for improving access to care across state lines for Medicare and Medicaid beneficiaries (HHS, 2024a). A license compact is an agreement to streamline the licensing process for physicians who would like to practice in multiple states. This development is a promising replacement for the relaxation of licensure laws that took place during the pandemic emergency orders. There are license compacts in place that include psychiatrists, psychologists, and nurses, but there is no compact for mental health/SUD counselors, including licensed clinical social workers, licensed clinical professional counselor, and licensed addiction counselors, Therefore, the existing licensing compacts are not as helpful as they could be when it comes to expanding the delivery of telehealth for behavioral health services (HHS, 2024a).
Medicare allows billing by health care providers in occupational compacts because the compacts meet the CMS’s federal licensing requirements. Currently the Interstate Medical Licensure Compact explicitly allows for practicing telemedicine across state lines but the Counseling Compact’s allotted privileges authorizing telehealth and in-person practice across state lines are expected to be open in late 2024 or early 2024 (Counseling Compact, 2024b; IMLCC, 2021). Physicians must meet the licensure requirements of the state where they are licensed and any additional licensure or practice requirements of the state where the patient is physically located at the time of the appointments. Compacts differ regarding single- versus multi-state licensing, allowance for telehealth, or exceptions to state licensure in specific circumstances to preserve continuity of care (HHS, 2024c).
There are at least nine health care occupational compacts, of which at least five are relevant to the delivery of longitudinal behavioral health services (see Table 4-2):
- Interstate Medical Licensure Compact: 41 jurisdictions (states and territories)
- Nursing Licensure Compact: 41 jurisdictions (states and territories)
- Psychology Interstate Compact: 41 states
- Counseling Compact: 33 states
- Social Work Compact (24 states have introduced legislation, need seven states to pass legislation for an active compact)
Upon enactment, these compacts are binding agreements that expedite a state’s (or territory’s, used interchangeably henceforth) licensing process and require legislative authorization for an individual state’s participation. A minimum number of states, often at least seven, must enact the model legislation before a compact can be implemented. Compact commissions
TABLE 4-2 Comparison of Common Compact Licenses in the United States
| Name of Compact | Distribution | History | Practitioner Eligibility | Governance | Revenues |
|---|---|---|---|---|---|
| The Counseling Compact Commission (Counseling Compact Commission, 2023, 2024a,b) | 36 States (effective July 1, 2024) | Funded and created by the American Counseling Association and the Council of State Governments, the Counseling Compact was finalized in December 2020. | Applications for Counseling Compact privileges to practice are expected to open in late 2024. The compact applies only to counselors licensed as licensed professional counselors, or whatever designation the state uses. | Each licensing board appoints one current member of its board to serve as a commissioner. | None yet. The American Counseling Association has agreed to cover the initial funds necessary to operationalize the Commission through September 30, 2023. Total initial proposed expenses: $367,500.00. |
| The Interstate Medical Licensure Compact (IMLCC, 2024) | 40 states plus Guam and Washington, DC | In April 2017, the compact became operational. | Physician (M.D. or D.O.). Approximately 80% of U.S. physicians meet the criteria for licensure through the compact. The physician’s primary residence is in the state of primary licensure. Serves as an information share/clearinghouse among states, state license required for all physicians in the compact. | Each participating compact state sends two representatives to the Commission. | Proposed 2025 budget: $7,236,000 |
| The Nurse Licensure Compact (NLC, 2022, 2024) | 41 jurisdictions | Started in 2000. Beginning on Jan. 19, 2018, an updated version of the NLC was implemented in 26 states, replacing the original version that started in 2000. | RN or LPV/VN. Does not include APRNs. Nurses may not currently be a participant in an alternative program and are required to self-disclose current participation in an alternative program if applying. | The Interstate Commission of Nurse Licensure Compact Administrators comprises members from each of the participating NLC jurisdictions. | FY 2022: $192,000.00 |
| The Psychology Interjurisdictional Compact Commission – PSYPACT (PSYPACT, 2024a,b) | 41 states as of July 1, 2024 | PSYPACT was originally created in 2019. | Must hold a full, unrestricted license to practice psychology based off a doctoral-level degree. Psychologists must identify a home state and will be physically located in the home state while providing telepsychology | Bylaws established 2019. Each licensing board appoints one current member or staff member of its board to serve as a commissioner. | Annual 2024 revenue is $275,000.00 |
NOTE: Compacts listed are those with more than 50 percent saturation across the country
SOURCES: Counseling Compact, 2023,2024a,b; IMLCC, 2024; NLC, 2022; PSYPACT, 2024a,b.
are the governing bodies that make sure that states comport to the licensing rules and processes that are established. Compacts do not change a state’s statutory authority regarding the specific scope of practice. Compacts differ regarding single- versus multi-state licensing, allowance for tele-behavioral health, or exceptions to state licensure in specific circumstances to preserve continuity of care (HHS, 2024c).
The Department of Defense has been partnering with the Council of State Governments to fund and support the development of new interstate compacts for occupational licensure. According to the National Center for Interstate Compacts, over 325 pieces of compact legislation have passed at the state and territorial level since 2016. In addition, 50 states and territories are participating in at least one occupational licensure compact, and 17 professions have occupational licensure compacts (NCIC, 2024). On April 12, 2024, Kansas became the seventh state to pass social work interstate licensing compact legislation, reaching the seven-state threshold creating a compact commission that will govern the compact and ensure coordination between the participating states (NASW, 2024).
Some states participate in only one compact, while others participate in multiple compacts. There are active advocacy efforts at both the federal and state levels to implement compacts for other professions well as to increase adoption by states and jurisdictions to join existing compacts. Despite the national footprint these compacts allow, there remains no federal government influence or oversight on specifics for licensure, standardization, or reimbursement, even though CMS pays more than any other insurer for behavioral health service delivery.
BILLING COVERAGE OF ADDITIONAL CLINICAL BEHAVIORAL HEALTH PROVIDERS AND SERVICES
Widespread shortages of behavioral health providers disproportionally affect beneficiaries and enrollees of the Medicare, Medicaid, and Marketplace plans (Counts, 2023). To mitigate this challenge, various efforts have been underway to expand the workforce pool, such as allowing insurance funding for new types of behavioral health care providers not previously eligible for reimbursement on a consistent basis (Saunders et al., 2023). This effort increasingly includes nonclinical and paraprofessional behavioral health providers and services, such as peer counselors and CHWs, as discussed previously. In addition, other allied health clinical provider types are now also being considered as a viable option to help close the gap in mental health and SUD provider shortages, especially as part of integrated, interdisciplinary health care teams. For example, there is growing evidence for the value of occupational therapy (OT) as a part of an interdisciplinary approach to the treatment of behavioral health conditions (Arbesman et al., 2013; Lannigan and Noyes, 2019) and SUDs (Stoffel and Moyers, 2004).
However, RFI data from OT responders indicated some notable differences in experiences while accessing insurance reimbursement specifically for behavioral health services depending on state of practice or practice setting. While some OT providers reported being able to bill insurance, many others reported having faced considerable difficulty obtaining reimbursement from Medicare, Medicaid, and Marketplace programs specifically for behavioral health services, thus limiting patient access to these vital services. As one OT provider stated: “Occupational therapy is not recognized as a qualified behavioral health provider in every state. This limits reimbursement from these programs.” Other responders remarked on common misconceptions surrounding an OT’s ability to assess and treat behavioral health concerns. For example, one OT provider said, “There seems to be a misperception that occupational therapists only work with people who have primary physical diagnoses. Payment has been denied for OT services provided to people with behavioral health conditions, requiring significant therapist time to complete appeals and payer education.”
Mental health clinical pharmacy specialists are another group that fellow team members and patients are recognizing as making contributions to clinical teams, leading to increased access to care and improvements in workflows and overall quality of care (Gillespie et al., 2022). However, there is considerable variation in the ability of pharmacists to bill for their services. Pharmacists can bill Medicaid and private commercial insurance in some states but not others, depending on whether the specialists have been formally recognized under each respective state’s legal designation of a health care provider (Ali et al., 2023; Hazlet et al., 2017). This group has also not been legally recognized as health care providers at the federal level, under Medicare, Part B (Terrie, 2023). As a result, pharmacists continue to face barriers to providing some important services, including behavioral health services, depending on the state in which the practice is located, the service performed, and payer type. This was exemplified in the following sample of responses from the RFI:
“Currently due to CMS rules, pharmacists cannot bill for services. This is because they are not recognized as providers. Pharmacists have more years of education and training than many other professions who can currently bill for services. This limits our ability to provide services to those in need, especially those with behavioral health needs. This barrier delays access to care.”
“For all 3 programs, clinical pharmacists in general, including psychiatric pharmacists, are not recognized as providers. I therefore cannot submit for reimbursement of services I provide to patients, which are very similar in nature to a psych NP or APRN. I am forced to submit under my supervising psychiatrist’s name to get any kind of reimbursement, and
even then, not all of the FQHC’s submitted claims for my patient visits get reimbursed.”
“Medicare/Medicaid does not recognize pharmacists as providers, therefore limiting reimbursement possibilities and tying pharmacists to provider-based clinics. This fact negates community pharmacists from providing reimbursable behavioral health services when patients are in their pharmacy (medication assessment, metabolic monitoring, side effect/outcome screening/assessment).”
Additional training might sometimes be needed to further support these allied health care providers as members of interdisciplinary behavioral health care teams (El-Den et al., 2021). Nonetheless, advocacy efforts have continued to result in removing or relaxing various scope-of-practice restrictions and billing limitations, which would allow these allied health care professionals to be more widely recognized as behavioral health providers (Read et al., 2024), including more consistent inclusion under definition of a behavioral health provider for all applicable state and federal laws.
Finding: During the COVID-19 pandemic, both the federal government and states waived provisionally specific licensure requirements to maintain health care services, including behavioral health care. This flexibility included the provision of telehealth and provision of treatment across state lines. Several states have taken steps to codify this flexibility either through state policies or legislation.
Finding: The licensing process for behavioral health providers is hampered by a myriad of individual state licensure and scope-of-practice laws and guidelines. Coupled with lengthy and different credentialing processes among individual insurance and managed care companies, these have served as a deterrent for some individuals to participate in or be allowed to participate into insurance networks to provide behavioral health treatment.
Finding: There is evidence that state-based licensure is a barrier to portability across state lines and reciprocity across state lines.
Conclusion 4-7: Occupational licensing compacts can facilitate improved access to care and diminish the maldistribution of the current behavioral health workforce. Revising and updating the interstate licensure agreements or advocating for adjustments in the state law, policy, or regulation could bolster and expand occupational compacts to further ease the provision of telemedicine services across state lines.
CONCLUSIONS
Conclusion 4-1: In addition to making short-term improvements in behavioral health provider participation among the existing workforce, strengthening the pipeline of federally subsidized behavioral health providers would build a workforce more likely to continue serving Medicare and Medicaid populations after completing their training. Bolstering workforce programs and policies, including successful pathway or pipeline programs, would increase the number of people who want to enter the behavioral health field and support behavioral health provider retention.
Conclusion 4-2: The behavioral health workforce does not reflect the diversity of the population it serves. Increasing historically underrepresented racial and ethnic identities, as well as language and cultural representation, in the behavioral health workforce is one mechanism to address disparities in access to care facing Medicare and Medicaid programs. Within Medicaid specifically, increased representation of historically underrepresented racial and ethnic identities in the health care workforce could expand access to care for beneficiaries more broadly, regardless of identity.
Conclusion 4-3: Recruitment barriers, particularly those affecting communities of color, may be addressed through efforts to decrease stigma, dispel historical mistrust, and provide financial incentives associated with behavioral health professions.
Conclusion 4-4: There is a demonstrated inconsistency between the primary source of GME program funding (e.g., Medicare and Medicaid) and participation in public insurance programs among behavioral health providers whose training is funded by GME. While GME program funding primarily comes from Medicare and Medicaid, many trainees do not subsequently participate in these programs.
Conclusion 4-5: The lack of billing for services provided by trainees in Medicare and Medicaid is a major barrier to expanding training opportunities for behavioral health specialists who are more likely to participate in the Medicare and Medicaid programs.
Conclusion 4-6: Expanding the delivery of behavioral health support specialist (BHSS) services in Medicare and Medicaid has the potential to significantly improve access and outcomes, especially for individuals with complex needs, while also augmenting the reach of licensed behavioral health professionals. Federal intervention is crucial to establishing BHSS through model national certification standards and flexible
payment models that facilitate the integration of these services into the full continuum of behavioral health care.
Conclusion 4-7: Occupational licensing compacts can facilitate improved access to care and diminish the maldistribution of the current behavioral health workforce. Revising and updating the interstate licensure agreements or advocating for adjustments in the state law, policy, or regulation could bolster and expand occupational compacts to further ease the provision of telemedicine services across state lines.
REFERENCES
Abrams, K., P. Durbha, and A. Balan-Cohen. 2018. Growth in outpatient care: The role of quality and value incentives. https://www2.deloitte.com/us/en/insights/industry/health-care/outpatient-hospital-services-medicare-incentives-value-quality.html (accessed May 31, 2024).
Ali, U. S., G. M. Hale, M. Santibanez, K. Berger, and K. Baldwin. 2023. Is now our time? History to provider status for allied health professions and the path for pharmacists. Journal of the American Pharmacists Association 63(5):1515–1520.
APA (American Psychological Association). 2014. Medicaid reimbursement for psychology interns’ services: Advocacy toolkit. https://www.apa.org/ed/graduate/about/reimbursement (accessed May 31, 2024).
APA. 2022a. Congress: Reimburse psychology interns and residents for supervised services provided in Medicare. Washington, DC: American Psychological Association.
APA. 2022b. Mental health crisis: CMS issues proposals to help psychologists meet the demand. https://www.apaservices.org/practice/reimbursement/government/help-psychologists-meet-demand (accessed May 31, 2024).
Arbesman, M., S. Bazyk, and S. M. Nochajski. 2013. Systematic review of occupational therapy and mental health promotion, prevention, and intervention for children and youth. American Journal of Occupational Therapy 67(6):e120–e130.
Barbui, C., M. Purgato, J. Abdulmalik, C. Acarturk, J. Eaton, C. Gastaldon, O. Gureje, C. Hanlon, M. Jordans, C. Lund, M. Nosè, G. Ostuzzi, D. Papola, F. Tedeschi, W. Tol, G. Turrini, V. Patel, and G. Thornicroft. 2020. Efficacy of psychosocial interventions for mental health outcomes in low-income and middle-income countries: An umbrella review. The Lancet Psychiatry 7(2):162–172.
Barnett, M. L., A. Gonzalez, J. Miranda, D. A. Chavira, and A. S. Lau. 2018. Mobilizing community health workers to address mental health disparities for underserved populations: A systematic review. Administration and Policy in Mental Health and Mental Health Services Research 45(2):195–211.
Bazemore, A., P. Wingrove, S. Petterson, L. Peterson, M. Raffoul, and R. L. J. Phillips. 2015. Graduates of teaching health centers are more likely to enter practice in the primary care safety net. American Family Physician 15(10):868.
BHWAC (Behavioral Health Workforce Advisory Committee). 2022. 2022 Behavioral Health Workforce Assessment: A report of the Behavioral Health Workforce Advisory Committee. Olympia, WA: Workforce Training and Education Coordinating Board.
Bommersbach, T. J., A. J. McKean, M. Olfson, and T. G. Rhee. 2023. National trends in mental health-related emergency department visits among youth, 2011–2020. JAMA 329(17):1469.
Boyd, R. W. 2019. The case for desegregation. The Lancet 393(10190):2484-2485.
Breuer, E., A. Morris, L. Blanke, M. Pearsall, R. Rodriguez, B. F. Miller, J. A. Naslund, S. Saxena, S. Balsari, and V. Patel. 2023. A theory of change for community-initiated mental health care in the United States. Cambridge Prisms: Global Mental Health 10:1–35.
Cabral, R. R., and T. B. Smith. 2011. Racial/ethnic matching of clients and therapists in mental health services: A meta-analytic review of preferences, perceptions, and outcomes. Journal of Counseling Psychology 58(4):537–554.
Cai, A., A. Mehrotra, H. D. Germack, A. B. Busch, H. A. Huskamp, and M. L. Barnett. 2022. Trends in mental health care delivery by psychiatrists and nurse practitioners in Medicare, 2011–19. Health Affairs 41(9):1222–1230.
CCHP (Center for Connected Health Policy). 2024. Professional requirements: Cross-state licensing. https://www.cchpca.org/topic/cross-state-licensing-professional-requirements/ (accessed May 31, 2024).
CMS (Centers for Medicare & Medicaid Studies). 2021. On the front lines of health equity: Community health workers. Washington, DC: U.S Department of Health and Human Services.
CMS. 2023a. Calendar year (CY) 2024 Medicare physician fee schedule final rule. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2024-medicare-physician-fee-schedule-final-rule (accessed July 5, 2024).
CMS. 2023b. Medicare Learning Network (MLN) booklet: Guidelines for teaching physicians, interns, & residents. Washington, DC: Centers for Medicare & Medicaid Services. Available at https://www.cms.gov/files/document/guidelines-teaching-physicians-interns-and-residents.pdf (accessed May 31, 2024).
CMS. 2023c. Race and ethnicity of the national medicaid and chip population in 2020. Washington, DC: Centers for Medicare and Medicaid Services.
Cooper, L. A., D. L. Roter, R. L. Johnson, D. E. Ford, D. M. Steinwachs, and N. R. Powe. 2003. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine 139(11):907–915.
Counseling Compact. 2023. Counseling compact 2022 annual report. https://counseling-compact.org/wp-content/uploads/2023/09/annual-report-2022-counseling-compact.pdf (accessed May 31, 2024).
Counseling Compact. 2024a. Counseling Compact. https://counselingcompact.org/ (accessed May 31, 2024).
Counseling Compact. 2024b. FAQ for counselors. https://prod761aul1.wpenginepowered.com/faq/ (accessed July 1, 2024).
Counts, N. 2023. Understanding the U.S. behavioral health workforce shortage. https://www.commonwealthfund.org/publications/explainer/2023/may/understanding-us-behavioral-health-workforce-shortage (accessed May 31, 2024).
Cushing, A. M., D. B. Liberman, P. K. Pham, K. A. Michelson, A. Festekjian, T. P. Chang, and P. P. Chaudhari. 2023. Mental health revisits at U.S. pediatric emergency departments. JAMA Pediatrics 177(2):168–176.
Dahal, A., and S. M. Skillman. 2022. Washington State’s physician workforce in 2021. Center for Health Workforce Studies, University of Washington. https://familymedicine.uw.edu/chws/wp-content/uploads/sites/5/2022/08/Washington_Physicians_FR_2022-JULY.pdf (accessed May 31, 2024).
Daly, M. R., and J. M. Mellor. 2020. Racial and ethnic differences in Medicaid acceptance by primary care physicians: A geospatial analysis. Medical Care Research and Review 77(1):85–95.
Davidson, L., C. Bellamy, K. Guy, and R. Miller. 2012. Peer support among persons with severe mental illnesses: A review of evidence and experience. World Psychiatry 11(2): 123–128.
Davidson, R. C., and R. Montoya. 1987. The distribution of services to the underserved. A comparison of minority and majority medical graduates in california. Western Journal of Medicine 146(1):114–117.
Davis, C. S., T. Roy, L. E. Peterson, and A. W. Bazemore. 2022. Evaluating the teaching health center graduate medical education model at 10 years: Practice-based outcomes and opportunities. Journal of Graduate Medical Education 14(5):599–605.
Diamond, L., K. Izquierdo, D. Canfield, K. Matsoukas, and F. Gany. 2019. A systematic review of the impact of patient–physician non-English language concordance on quality of care and outcomes. Journal of General Internal Medicine 34(8):1591–1606.
El-Den, S., J. C. Collins, T. F. Chen, and C. L. O’Reilly. 2021. Pharmacists’ roles in mental healthcare: Past, present and future. Pharmacy Practice 19(3):2545.
Gajewski, A. J., S. M. Starks, and N. T. Aggarwal. 2022. To grow the mental health workforce, pay for care delivered by trainees. Health Affairs Forefront, July 18. https://www.healthaffairs.org/content/forefront/grow-mental-health-workforce-pay-care-delivered-trainees (accessed May 31, 2024).
GAO (U.S. Government Accountability Office). 2017. Physician workforce: Locations and types of graduate training were largely unchanged, and federal efforts may not be sufficient to meet needs. GAO-17-411. Washington, DC: Government Accountability Office. Available at https://www.gao.gov/products/gao-17-411 (accessed May 31, 2024).
GAO. 2021. National Health Service Corps: Program directs funding to areas with greatest provider shortages. GAO-21-323. Washington, DC: U.S. Government Accountability Office. Available at https://www.gao.gov/assets/720/714090.pdf (accessed May 31, 2024).
Gilbert, M., T. Hartnett, G. W. Hoagland, O. J. Kim, M. Serafini, and K. Strong. 2023. Filling the gaps in the behavioral health workforce. Washington, DC: Bipartisan Policy Center.
Gillespie, C., F. Kleinberg, A. Zogas, A. Morreale, H. Ourth, M. Tran, T. Moore, D. Miller, and M. McCullough. 2022. Perceptions of clinical pharmacy specialists’ contributions in mental health clinical teams. Mental Health Clinician 12(1):15–22.
Greene, J., J. Blustein, and B. C. Weitzman. 2006. Race, segregation, and physicians’ participation in Medicaid. The Milbank Quarterly 84(2):239–272.
Guth, M. 2023. Telehealth delivery of behavioral health care in Medicaid: Findings from a survey of state Medicaid programs. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/telehealth-delivery-of-behavioral-health-care-in-medicaid-findings-from-a-survey-of-state-medicaid-programs/ (accessed May 31, 2024).
Haldar, S., and E. Hinton. 2023. State policies for expanding medicaid coverage of community health worker (CHW) services. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/state-policies-for-expanding-medicaid-coverage-of-community-health-worker-chw-services/#footnote-576635-19 (accessed May 31, 2024).
Harati, P. M., J. R. Cummings, and N. Serban. 2020. Provider-level caseload of psychosocial services for Medicaid-insured children. Public Health Reports 135(5):599–610.
Hazlet, T. K., T. E. Karwaki, and D. F. Downing. 2017. Pathway to pharmacist medical provider status in Washington State. Journal of the American Pharmaceutical Association 57(1):116–119.
Heflinger, C. A., J. Chatman, and R. C. Saunders. 2006. Racial and gender differences in utilization of Medicaid substance abuse services among adolescents. Psychiatric Services 57(4):504–511.
Heisler, E. J., B. H. P. Mendez, A. Mitchell, S. Viranga Panangala, and M. A. Villagrana. 2018. Federal support for graduate medical education: An overview
HHS (U.S. Department of Health and Human Services). 2009. Pipeline programs to improve racial and ethnic diversity in the health professions: An inventory of federal programs, assessment of evaluation approaches, and critical review of the research literature. https://sfdph.org/dph/files/SDDTAC/PipelineToImproveDiversityInHealthProfessions.pdf (accessed May 31, 2024).
HHS. 2024a. About telehealth. https://telehealth.hhs.gov/about (accessed May 31, 2024).
HHS. 2024b. HHS roadmap for behavioral health integration fact sheet of accomplishments. https://www.hhs.gov/about/news/2024/01/18/hhs-roadmap-for-behavioral-health-integration-fact-sheet-accomplishments.html (accessed May 31, 2024).
HHS. 2024c. Licensure compacts. https://telehealth.hhs.gov/licensure/licensure-compacts (accessed May 31, 2024).
Hoffmann, J. A., P. Krass, J. Rodean, N. S. Bardach, R. Cafferty, T. R. Coker, G. J. Cutler, M. Hall, R. B. Morse, K. A. Nash, K. Parikh, and B. T. Zima. 2023. Follow-up after pediatric mental health emergency visits. Pediatrics 151(3):e2022057383.
HRSA (Health Resources and Services Administration). 2021. FAQ: Behavioral Health Workforce Education and Training (BHWET) program for professionals. https://bhw.hrsa.gov/funding/apply-grant/bhwet-faqs (accessed May 31, 2024).
HRSA. 2022a. Behavioral Health Workforce Education and Training Program academic years 2014–2022. Washington, DC: U.S. Department of Health and Human Services.
HRSA. 2022b. Behavioral health workforce projections, 2020–2035. Washington, DC: U.S. Department of Health and Human Services.
HRSA. 2022c. Health Careers Opportunity Program—Academic years 2015–2020. Washington, DC: U.S. Department of Health and Human Services.
HRSA. 2023a. Centers of excellence—Academic years 2015–2020. Washington, DC: U.S. Department of Health and Human Services.
HRSA. 2023b. Nursing Workforce Diversity (NWD) Program academic years, 2014–2019. Washington, DC: U.S. Department of Health and Human Services.
HRSA. 2024a. Justification of estimates for appropriations committees. Washington, DC: U.S. Department of Health and Human Services.
HRSA. 2024b. NHSC loan repayment program. https://nhsc.hrsa.gov/loan-repayment/nhsc-loan-repayment-program (accessed May 31, 2024).
IMLCC (Interstate Medical Licensure Compact). 2021. https://www.imlcc.org/ (accessed May 31, 2024).
IOM (Institute of Medicine). 2014. Graduate medical education that meets the nation’s health needs. Washington, DC: The National Academies Press.
Jones, E., S. R. Lattof, and E. Coast. 2017. Interventions to provide culturally-appropriate maternity care services: Factors affecting implementation. BMC Pregnancy and Childbirth 17(1):267.
Kohrt, B. A., B. F. Miller, and V. Patel. 2023. Community initiated care: A blue-print for the practical realization of contextual behavioral science. Journal of Contextual Behavioral Science 27:54–60.
Ku, L., and A. Vichare. 2023. The association of racial and ethnic concordance in primary care with patient satisfaction and experience of care. Journal of General Internal Medicine 38(3):727–732.
Lannigan, E. G., and S. Noyes. 2019. Occupational therapy interventions for adults living with serious mental illness. American Journal of Occupational Therapy 73(5):7305395010p1–7305395010p5.
MACPAC (Medicaid and CHIP Payment and Access Commission). 2021. Racial and ethnic disparities in Medicaid: An annotated bibliography. Washington, DC: MACPAC.
MACPAC. 2022. Access in brief: Experiences of lesbian, gay, bisexual, and transgender Medicaid beneficiaries with accessing medical and behavioral health care. Washington, DC: MACPAC. Available at https://www.macpac.gov/publication/access-in-brief-experiences-of-lesbian-gay-bisexual-and-transgender-medicaid-beneficiaries-with-accessing-medical-care-and-behavioral-health-care/ (accessed May 31, 2024).
Marrast, L. M., L. Zallman, S. Woolhandler, D. H. Bor, and D. McCormick. 2014. Minority physicians’ role in the care of underserved patients. JAMA Internal Medicine 174(2):289.
Mauri, A., M. Gaiser, J. Buche, and A. J. Beck. 2019. Behavioral health provider geographic distribution and reimbursement inequities. Ann Arbor, MI: University of Michigan Behavioral Health Workforce Research Center.
McBain, R. K., A. Kofner, B. D. Stein, J. H. Cantor, W. B. Vogt, and H. Yu. 2019. Growth and distribution of child psychiatrists in the United States: 2007–2016. Pediatrics 144(6): e20191576.
Mitchell, A., E. P. Baumrucker, K. J. Colello, A. Napili, C. Binder, and S. K. Braun. 2023. Medicaid: An overview. Washington, DC: Congressional Research Service. Available at https://crsreports.congress.gov/product/pdf/R/R43357 (accessed May 31, 2024).
Mullan, F., C. Chen, and E. Steinmetz. 2013. The geography of graduate medical education: Imbalances signal need for new distribution policies. Health Affairs 32(11): 1914–1921.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2023. Federal policy to advance racial, ethnic, and tribal health equity. Washington, DC: The National Academies Press.
NASW (National Association of Social Workers). 2024. Interstate licensure compact. https://www.socialworkers.org/Advocacy/Interstate-Licensure-Compact-for-Social-Work (accessed May 31, 2024).
National Council for Mental Wellbeing. 2022. View from the field: Recruitment and retention of African American men in the mental health and substance use workforce. Available at https://www.thenationalcouncil.org/resources/baa-focus-group-report/ (accessed May 31, 2024).
NCIC (National Center for Interstate Compacts). 2024. Occupational Licensure Compacts. https://compacts.csg.org/compacts/ (accessed May 29, 2024).
NLC (Nurse Licensure Compact.). 2022. Nurse Licensure Compact Commission annual report. https://www.ncsbn.org/public-files/22-NLCAnnualReport.pdf (accessed May 31, 2024).
NLC. 2024. Home page. https://www.nursecompact.com/ (accessed May 31, 2024).
Ochieng, N., J. Fuglesten Biniek, J. Cubanski, and T. Neuman. 2023. Disparities in health measures by race and ethnicity among beneficiaries in Medicare Advantage: A review of the literature. KFF. https://www.kff.org/report-section/disparities-in-health-measures-by-race-and-ethnicity-among-beneficiaries-in-medicare-advantage-report/ (accessed May 31, 2024).
Office of the Surgeon General. 2021. Protecting youth mental health: The U.S. Surgeon General’s advisory. Washington, DC: U.S. Department of Health and Human Services.
Olson, D. P., F. Nunez, M. Overbeck, J. Hotz, A. Billings, E. Frazier, K. Thomsen, A. P. Kelly, N. Diaz, and V. Little. 2020. The National Health Service Corps at 50: A legacy of impact in partnership with the Association of Clinicians for the Underserved. Journal of Health Care for the Poor and Underserved 31(2):542–548.
PSYPACT. 2024a. Home page. https://psypact.org/ (accessed May 31, 2024).
PSYPACT. 2024b. 2024 Annual Budget and Narrative Report. https://cdn.ymaws.com/psypact.org/resource/resmgr/proposed_budget/proposed_2024_annual_budget.pdf (accessed May 31, 2024).
Read, H., S. Zagorac, N. Neumann, I. Kramer, L. Walker, and E. Thomas. 2024. Occupational therapy: A potential solution to the behavioral health workforce shortage. Psychiatric Services, February 7:appips20230298.
Saha, S., M. Komaromy, T. D. Koepsell, and A. B. Bindman. 1999. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine 159(9):997–1004.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2023a. Core competencies for peer workers. https://www.samhsa.gov/brss-tacs/recovery-support-tools/peers/core-competencies-peer-workers (accessed June 28, 2024).
SAMHSA. 2023b. SAMHSA’s national model standards for peer support certification. https://www.samhsa.gov/about-us/who-we-are/offices-centers/or/model-standards (accessed June 28, 2024).
SAMHSA. 2024. Financing peer recovery support: Opportunities to enhance the substance use disorder peer workforce. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Samnaliev, M., M. P. McGovern, and R. E. Clark. 2009. Racial/ethnic disparities in mental health treatment in six Medicaid programs. Journal of Health Care for the Poor and Underserved 20(1):165–176.
Saunders, H., M. Guth, and G. E. Eckart. 2023. A look at strategies to address behavioral health workforce shortages: Findings from a survey of state medicaid programs. Kaiser Family Foundation. https://www.kff.org/mental-health/issue-brief/a-look-at-strategies-to-address-behavioral-health-workforce-shortages-findings-from-a-survey-of-state-medicaid-programs/ (accessed May 31 2024).
Schleiter Hitchell, K., and L. Johnson. 2022. CMS finalizes rules for distribution of 1,000 new medicare-funded residency positions and changes to rural training track programs. Journal of Graduate Medical Education 14(2):245–249.
Shapiro, D. N. 2022. Increasing interest in child and adolescent psychiatry during medical school: Launching a summer immersion experience for medical students. Academic Psychiatry 46(1):70–74.
Siddiqui, S., A. Morris, D. J. Ikeda, S. Balsari, L. Blanke, M. Pearsall, R. Rodriguez, S. Saxena, B. F. Miller, V. Patel, and J. A. Naslund. 2022. Scaling up community-delivered mental health support and care: A landscape analysis. Frontiers in Public Health 10992222.
Snyder, J. E., R. D. Upton, T. C. Hassett, H. Lee, Z. Nouri, and M. Dill. 2023. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the U.S. JAMA Network Open 6(4):e236687.
Stein, B. D., A. W. Dick, M. Sorbero, A. J. Gordon, R. M. Burns, D. L. Leslie, and R. L. Pacula. 2018. A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees. Substance Abuse 39(4):419–425.
Stoffel, V. C., and P. A. Moyers. 2004. An evidence-based and occupational perspective of interventions for persons with substance-use disorders. American Journal of Occupational Therapy 58(5):570–586.
Taylor, K. J., M. Eldridge, L. Ford, C. Alvarez Caraveo, E. H. Allen, and F. Mitchell. 2022. Improving and expanding programs to support a diverse health care workforce. Washington, DC: Urban Intstitute.
Terrie, Y. 2023. Supporting provider status for pharmacists. U.S. Pharmacist 48(10):39–42.
Tipirneni, R., E. C. Kieffer, J. Z. Ayanian, E. G. Campbell, C. Salman, S. J. Clark, T. Chang, A. N. Haggins, E. Solway, and M. A. Kirch. 2019. Factors influencing primary care providers’ decisions to accept new Medicaid patients under Michigan’s Medicaid expansion. American Journal of Managed Care 25(3):120–127.
Zhu, J. M., C. J. Charlesworth, D. Polsky, and K. J. McConnell. 2022. Phantom networks: Discrepancies between reported and realized mental health care access in oregon medicaid. Health Affairs 41(7):1013–1022.
This page intentionally left blank.



































