Breastfeeding in the United States: Strategies to Support Families and Achieve National Goals (2025)
Chapter: 2 The Importance of Breastfeeding Across the Life Course
2
The Importance of Breastfeeding Across the Life Course
This chapter highlights the importance of breastfeeding, with a particular focus on its associated health benefits for both mothers and infants. In alignment with its statement of task, which did not call for a novel evidence review, the committee offers a summary of existing research, drawing primarily from meta-analyses and systematic reviews of key health outcomes. The chapter then examines the physiology of breastfeeding and human lactation, explaining the biological processes that enable lactation and the mechanisms through which health benefits may be conferred. Taking a life course perspective, the chapter next identifies critical inflection points, such as prenatal care, birth experiences, and early postpartum support, that can influence breastfeeding initiation and duration, and ultimately, health outcomes. An overview of current breastfeeding rates in the United States follows, identifying trends and differences across populations. Finally, the chapter reviews existing modeling efforts aimed at estimating the economic costs associated with current, suboptimal breastfeeding rates.
THE HEALTH BENEFITS OF BREASTFEEDING
Decades of research show that breastfeeding is associated with short- and long-term benefits for children and mothers. To date, the most comprehensive and widely cited systematic review on the relationship between breastfeeding and infant and maternal health outcomes is a report by Ip et al. (2007). Feltner et al. (2018) partially updated that report but focused only on the maternal health benefits of breastfeeding. Several recent reviews, including those from the Pregnancy and Birth to 24 Months Project
(Güngör et al., 2019a,b,c,d; Obbagy et al., 2019; Stoody et al., 2019) and others (Brown et al., 2019; Dewey et al., 2021; Horta et al., 2015, 2023; Lockyer et al., 2021; Meek et al., 2022; Pathirana et al., 2022; Rollins et al., 2016; Su et al., 2021; Victora et al., 2016) have examined specific infant and child outcomes.
Recently, a systematic review by Patnode et al. (2025) comprehensively updated the evidence from Ip et al. (2007) on the link between breastfeeding and infant and child outcomes. This review advances understanding of the potentially nuanced benefits of breastfeeding for infant- and child-specific health outcomes; the magnitude of those benefits; and how they vary with the intensity, duration, mode of feeding, and source of human milk. However, this review did not include preterm infants or infants requiring intensive care. In the sections that follow, the committee briefly describes the evidence on potential health impacts of breastfeeding for mothers and children, including sick or vulnerable infants and children.
Maternal Health Benefits
In mammalian physiology, discussed later in this chapter, lactation and the practice of breastfeeding1 follow pregnancy. Breastfeeding is also associated with significant health benefits for women over the course of their lives and is a normal part of reproductive physiology and recovery from pregnancy.
In the immediate postpartum period, women who breastfeed experience more rapid uterine involution, decreased postpartum bleeding, and increased child spacing (Louis-Jacques & Stuebe, 2020; Victora et al., 2016). These immediate postpartum benefits are important, as hemorrhage is a leading cause of maternal postpartum morbidity (American College of Obstetricians and Gynecologists [ACOG], 2017; Del Ciampo & Del Ciampo, 2018; Victora et al., 2016). Findings from Feltner et al. (2018) suggest that ever breastfeeding or breastfeeding for longer durations “may be associated with lower rates of breast cancer, ovarian cancer, hypertension, and type 2 diabetes” (p. ix). The authors went on to conclude there were inconsistent findings related to postpartum depression, weight change after birth, and cardiovascular disease (Feltner et al., 2018). Two systematic reviews and a large prospective cohort study published since 2018 have provided additional evidence on the association of breastfeeding duration with reduced maternal risk of cardiovascular disease outcomes (Tschiderer et al., 2022), including among women with diabetes complicating pregnancy
___________________
1 As noted in Chapter 1, breastfeeding refers to the dynamic physiological process and interactions that occur between a mother and infant, including feeding at the breast and/or feeding expressed or pumped human milk.
(Birukov et al., 2024; Field et al., 2025). Chehayeb et al. (2025) also reported that breastfeeding is associated with a lower risk of triple negative breast cancer.
Researchers have also examined whether there is a relationship between breastfeeding and psychosocial outcomes for the breastfeeding dyad, such as attachment, bonding, and maternal mental health. Peñacoba and Catala (2019) conducted a systematic review of the literature related to associations between breastfeeding and mother–infant dyad relationships. The review included 13 studies; most of which were conducted in Europe (46.15%) and were nonexperimental in design (92.3%). The authors found that the relationship indicators most frequently associated with breastfeeding are maternal sensitivity and secure attachment, though the association is complex, and the breastfeeding relationship or method of feeding appears to influence outcomes. Furthermore, a review by Tucker and O’Malley (2022) noted that breastfeeding can have a positive impact on maternal mental health, specifically as it relates to postpartum depression, self-efficacy, and dyad bonding. The authors went on to state that breastfeeding difficulties or early cessation can be a risk factor and could potentially exacerbate perinatal mood and anxiety disorders if proper social support and lactation care are not provided or accessible (Tucker & O’Malley, 2022).
These findings point to the importance of breastfeeding for mothers across the life course. Yet, additional research is needed to further understand the relationship between breastfeeding and maternal physical and mental health.
Health Benefits for Infants and Children
As noted in Chapter 1, human milk provides all the nutrients necessary to support optimal growth and development for nearly all infants for the first six months of life and provides continued essential nutrition and developmental benefits for the duration2 of breastfeeding. As briefly described in Chapter 1, infants who are breastfed “more” versus “less” may have a reduced risk of developing noncommunicable diseases such as asthma, otitis media, obesity in childhood, and childhood leukemia (Patnode et al., 2025). In addition, a protective association of breastfeeding has been found for infant mortality, including sudden infant death, rapid weight gain and growth, systolic blood pressure, severe respiratory and gastrointestinal infections in younger children, allergic rhinitis, malocclusion, inflammatory bowel disease, and type 1 diabetes (Patnode et al., 2025). Breastfeeding can
___________________
2 Professional and public health organizations recommend that, when possible, breastfeeding be continued with appropriate complementary food for two years or as long as mutually desired (ACOG, 2021, 2023; Meek et al., 2022; World Health Organization [WHO], 2023b).
also be lifesaving in humanitarian emergencies, including natural disasters and supply chain disruptions (e.g., Bartick et al., 2024; Cerceo et al., 2024; see Chapters 4 and 5).
Patnode et al. (2025) identified several key findings related to the health effects of breastfeeding for infants, as presented in Table 2-1.
While the Patnode et al. (2025) review did not find associations between breastfeeding and cognitive benefits for infants, other studies have found such relationships (e.g., Belfort et al., 2013; Fitzsimons & Vera-Hernández, 2022; Goldshtein et al., 2025; Horta et al., 2015; Yang et al., 2018). For example, using variation in timing of births at hospitals and likelihood of breastfeeding, Fitzsimons and Vera-Hernández (2022) estimated the effect of breastfeeding on children’s development in the first seven years of life, for a sample of births by low-educated mothers. They found large effects of breastfeeding on children’s cognitive development (Fitzsimons & Vera-Hernández, 2022). Furthermore, a retrospective cohort study from Israel that included more than half a million children reported that longer exclusive and any breastfeeding durations was associated with reduced odds of developmental delays, as well as language or social neurodevelopmental conditions (Goldshtein et al., 2025), which the authors suggest may mediate the relationship between breastfeeding and cognitive development. The study specifically found that children who were breastfed for at least six months versus children breastfed for less than six months had fewer delays in attaining language and social or motor developmental milestones. The corresponding adjusted odd ratios (AORs) were 0.73 (95% Confidence Interval [CI]: 0.7–10.76) for exclusive breastfeeding and 0.86 (95% CI: 0.83–0.88) for nonexclusive breastfeeding). Importantly, among the 37,704 sibling pairs, children who were breastfed for at least six months were less likely—compared with their sibling with less than six months of breastfeeding or no breastfeeding—to demonstrate developmental delays or be diagnosed with neurodevelopmental conditions. The corresponding AORs were 0.91 (95% CI: 0.86–0.97) and 0.73 (95% CI: 0.66–0.82; Goldshtein et al., 2025). Therefore, the current evidence base suggests that some cognitive outcomes may be associated with breastfeeding, but additional research is needed to further elucidate this relationship, including the potential causal pathways and contextual factors that may moderate this relationship. Differences in study design, populations studied, and methods for accounting confounding factors may influence findings.
Health Benefits for Sick or Vulnerable Infants and Children
In the United States, approximately 300,000 infants are admitted to the neonatal intensive care unit (NICU), each year (Pineda et al., 2023). NICU admissions for critically ill infants increased 13% between 2016 and
2023 (Martin & Osterman, 2025). Sick or vulnerable infants, especially those who are born early (before 37 weeks gestation), at low birth weight (less than 5.5 pounds) and very low birth weight (less than 3.3 pounds), have an increased risk of short- or long-term health problems (Boundy et al., 2022). For critically ill infants, human milk has been identified as a lifesaving intervention (Parker et al., 2021; Schanler, 2011; Spatz, 2004; Sullivan et al., 2010; Underwood, 2013; Updegrove, 2004).
Miller et al. (2018) conducted a systematic review and meta-analysis that synthesized literature, started after the 1990s, which examined the effect of human milk on morbidity, specifically necrotizing enterocolitis, late-onset sepsis, retinopathy of prematurity, bronchopulmonary dysplasia, and neurodevelopment in infants born at or before 28 weeks’ gestation; they also reviewed publications with reported infant mean birth weight of 1,500 grams or more. Experimental and observational studies were pooled separately in the meta-analyses. Risk of bias was assessed for each individual study, and the GRADE3 system was used to judge the certainty of the findings. Forty-nine studies (with 56 reports) were included, of which 44 could be included in meta-analyses. Miller et al. (2018) found that human milk was associated with a protective effect against necrotizing enterocolitis, with an approximate 4% reduction in absolute risk.
Parker et al. (2021) also reported that human milk was associated with a reduction in late-onset sepsis, severe retinopathy of prematurity, and severe necrotizing enterocolitis. Particularly for necrotizing enterocolitis, any volume of human milk was found to be better than exclusive preterm formula—the higher the dose, the greater the protection. Altobelli et al. (2020) found that the risk of developing necrotizing enterocolitis is significantly lower when combining mother’s own and pasteurized donor human milk. Improving the intake of mother’s own and/or donor human milk results in small improvements in morbidity in this population (Miller et al., 2018). Parker et al. (2021) described in detail the dose–response relationship when providing mother’s own milk for hospitalized very low birth weight infants; exposures of human milk were variable across the studies, but results point to a strong association between higher doses of mother’s own milk with improved health benefits.
See Chapter 9 for future research needs and priorities, including the need to test the efficacy and effectiveness of strategies for supporting the provision of donor human milk for sick and vulnerable infants, including those who are critically ill.
___________________
3 GRADE is short for Grading of Recommendations Assessment, Development and Evaluation; it is a systematic approach to rating the certainty of evidence in systematic reviews and other evidence syntheses (Cochrane Collaboration, 2025).
| SOE and Direction of Association | Outcome | Number of ESRs (k in newest ESR) (Credibility)a |
Number of Primary Studies by Design (ROB)b |
Key Findings |
|---|---|---|---|---|
| Moderate SOE for reduced risk | Otitis media | 1 ESR (k = 24) (1 High) |
10 cohort (3 Some concerns, 6 High, 1 Very high) |
Reduced risk of otitis media associated with breastfeeding, particularly at younger ages (≤24 months). Pooled analyses showed an approximately 33% reduced risk of otitis media when comparing ever versus never breastfeeding and for longer versus shorter durations of any breastfeeding, and a 43% reduced risk when comparing longer versus shorter durations of exclusive breastfeeding. |
| Asthma | 3 ESRs (k = 42) (1 High, 1 Mod, 1 Low) |
11 cohort (5 Some concerns, 6 High) |
Reduced risk of asthma in childhood (2–12 years) associated with breastfeeding. The magnitude of the relative risk in pooled analyses ranged from approximately a 7 to 31% reduced risk of asthma with longer versus shorter durations of any breastfeeding and a 6 to 30% reduced risk when comparing longer versus shorter durations of exclusive breastfeeding. | |
| Obesity | 3 ESRs (k = 159) (2 Moderate, 1 Low) |
25 cohort (9 Some concerns, 12 High risk, 4 Very high risk) |
Lower risk of overweight and obesity in children two to 12 years old associated with breastfeeding. The magnitude of the association suggests a 15 to 34% reduced odds of having obesity with more versus less breastfeeding and a 4% reduction in the risk of early childhood obesity for every additional month of breastfeeding. |
| Cancer | 2 ESRs (k = 46) (1 High, 1 Moderate) |
2 cohort, 3 case-control (2 Some concerns, 2 High, 1 Very high) |
Reduced risk of childhood leukemia associated with breastfeeding, with pooled analyses suggesting a 10 to 23% reduced risk of childhood leukemia with ever versus never breastfeeding. No clear association for other cancer types. | |
| Low SOE for reduced risk | Respiratory infections | 2 ESRs (k = 16) (2 Low) |
35 cohort (2 Low, 14 Some concerns, 17 High, 2 Very high) |
Potential reduced risk of respiratory infections of greater severity associated with breastfeeding, particularly among infants and children ages 24 months or less. No evidence on COVID-19. |
| Diarrhea and GI infection | 1 ESR (k = 8) (1 Low) |
15 cohort (1 Low, 7 Some concerns, 5 High, 2 Very high) |
Potential reduced risk of moderate-to-severe GI infections and breastfeeding at younger ages, particularly in infants six months or less. No clear association between breastfeeding and GI infection in infants and children of older ages. | |
| Allergic rhinitis | 3 ESRs (k = 23) (2 High, 1 Low) |
4 cohort (2 Some concerns, 2 High) |
Potential reduced risk of allergic rhinitis associated with breastfeeding. | |
| Malocclusion | 2 ESRs (k = 14) (2 Moderate) |
No studies | Potential reduced risk of the development of malocclusion associated with any or exclusive breastfeeding, with inconsistent evidence on breastfeeding duration. | |
| Inflammatory bowel disease | 2 ESRs (k = 42) (1 Moderate, 1 Low) |
1 case-control, 2 cohorts, 1 pooled cohort (1 Low, 1 Some concerns, 1 High, 1 Very high) |
Potential reduced risk of inflammatory bowel disease associated with longer vs. shorter duration of breastfeeding. |
| SOE and Direction of Association | Outcome | Number of ESRs (k in newest ESR) (Credibility)a |
Number of Primary Studies by Design (ROB)b |
Key Findings |
|---|---|---|---|---|
| Type 1 diabetes | 2 ESRs (k = 22) (2 Low) |
1 case-control, 2 cohort (1 Some concerns, 1 High, 1 Very high) |
Potential reduced risk of type 1 diabetes in children 18 years and younger associated with breastfeeding. | |
| Rapid weight gain and growth | 3 ESRs (k = 20) (2 Moderate, 1 Low) |
14 cohort (6 Some concerns, 4 High, 4 Very high) |
Potential lower risk of accelerated growth and rapid weight gain in infancy and early childhood associated with breastfeeding. | |
| Cardiovascular outcomes | 2 ESRs (k = 35) (2 Low) |
14 cohort (4 Some concerns, 10 High) |
Potential reductions in SBP associated with breastfeeding, no clear association for DBP. No clear association between breastfeeding and blood lipid levels or arterial stiffness. Insufficient evidence for CVD endpoint outcomes. | |
| Infant mortality, including SUID | 2 ESRs (k = 18) (2 Moderate) |
2 case-control, 4 cohort (5 High, 1 Very high) |
Potential reduced risk of infant mortality associated with breastfeeding initiation, including risk of late-neonatal mortality and SUID. | |
| Moderate SOE for no association | Cognitive development | 1 ESR (k = 84) (1 Low) |
26 cohort (14 Some concerns, 10 High, 2 Very high) |
No association between breastfeeding and cognitive ability at any age. |
| Low SOE for no association | Atopic dermatitis | 3 ESRs (k = 27) (2 High, 1 Low) |
9 cohort (4 Some concerns, 4 High, 1 Very high) |
No clear association between breastfeeding and the risk of atopic dermatitis at any age. |
| Celiac disease | 2 ESRs (k = 30) (1 Moderate, 1 Low) |
1 cohort (1 High) |
No clear association between breastfeeding and risk of celiac disease. |
| Moderate SOE for increased risk | Dental caries | 1 ESR (k = 31) (1 High) |
2 cohort (1 Low risk, 1 Some concerns) |
Increased risk of dental caries associated with breastfeeding 12 months or longer. Pooled analyses showed an approximately 54% increased risk of caries when breastfeeding for 12 months or longer versus less than 12 months. |
| Insufficient SOE | Food allergy | 2 ESRs (k = 7) (1 High, 1 Low) |
10 cohort (4 Some concerns, 5 High, 1 Very high) |
Insufficient evidence to draw a conclusion on the association between breastfeeding and the risk of food allergies. |
| Type 2 diabetes | 2 ESRs (k = 2) (2 Low) |
4 cohort (2 Some concerns, 2 High) |
Insufficient evidence to draw a conclusion on the association between breastfeeding and risk of type 2 diabetes and intermediate diabetes outcomes at any age. |
a Credibility of ESRs was assessed using an adapted version of the AMSTAR 2 (A MeaSurement Tool to Assess systematic Reviews) tool13,14 (Full Report Appendix D, Table D-1). Overall credibility was rated as: high (zero or one non-critical weakness), moderate (more than one non-critical weakness), low (one critical flaw with or without non-critical weaknesses or more than one non-critical weakness), or critically low (more than one critical flaw with or without non-critical weaknesses).
b Risk of bias was assessed using adapted versions of the ROBINS-E (Risk Of Bias In Non-randomized Studies of Exposures) tool17,18 or the Newcastle Ottawa Scale for Case Control Studies17 (Full Report Appendix D, Tables D-2 and D-3). Overall risk of bias was rated as low, some concerns, high, or very high risk of bias.
NOTE: CVD = cardiovascular disease; DBP = diastolic blood pressure; ESR = existing systemic review; GI = gastrointestinal; ROB = risk of bias; SBP = systolic blood pressure; SOE = strength of evidence; SUID = sudden unexpected infant death; vs = versus.
SOURCE: Patnode et al., 2025.
HOW BREASTFEEDING WORKS
Breastfeeding is a part of the evolutionary adaptations that play a role in ensuring human survival and ongoing health (Pérez-Escamilla et al., 2023; Quinn et al., 2023). Human infants are born in a highly immature state and experience a long period of postnatal maturation that corresponds with longer brain development compared to other primate species (Pérez-Escamilla et al., 2023). They are particularly vulnerable and cannot survive on their own (Rosenberg, 2021; Rosenberg & Trevathan, 2016). In addition, unlike other primates, human infants are unable to cling to their mothers and must be carried. They are highly dependent on physiological coregulation. Close proximity and frequent breastfeeding help to meet human infants’ nutritional and hydration needs as well as regulate their temperature, breathing, and heart rate (Tomori et al., 2022). The positive health outcomes associated with breastfeeding noted above have long-standing effects that outlast the time frame of breastfeeding and change the life course of the human infant (Meek et al., 2020). In addition to the positive associations with health, breastfeeding may provide psychosocial benefits to the breastfeeding dyad, including opportunities for emotional bonding and the potential to regulate stress and mood (e.g., Alimi et al., 2022; Feltner et al., 2018).
Human milk production is the result of a neuroendocrinological regulated supply–demand process driven by the suckling frequency, duration, and strength of the infant (Geddes et al., 2021). When the infant suckles from the breast, nipple stimulation triggers neural impulses that signal the mother’s hypothalamus to release prolactin-releasing hormone, which then stimulates prolactin release from the anterior pituitary gland and other hormones that are needed for milk synthesis in the mammary gland. The maternal hypothalamus serves a critical regulatory role for prolactin release because it also synthesizes dopamine, which, when released to the anterior pituitary gland, will inhibit prolactin release. In contrast when dopamine levels are lowered, as with certain medications or tumors, increased prolactin secretion results and may lead to overproduction or galactorrhea.
Nipple stimulation also signals the maternal posterior pituitary gland to release oxytocin, which is made in the maternal hypothalamus and stored in the posterior pituitary gland to be released into the maternal bloodstream. Once oxytocin reaches the mammary gland, the gland “squeezes” the myoepithelial cells surrounding the alveoli grape-like structures that contain the epithelial lactocytes where breastmilk is synthesized (Geddes et al., 2021). The squeezing of the myoepithelial cells is what allows the breastmilk to be ejected from the lactocytes into the milk ducts that converge in the nipple to feed the baby (Geddes et al., 2021). When the breasts are not drained, the maternal organism accumulates a substance, sometimes known as the feedback inhibitor of lactation, that slows down milk production in the mammary gland; this is called the autocrine control of milk production.
Thus, any interference with breastfeeding on cue, whether through caregiver-imposed nursing schedules or introduction of foods/fluids other than breastmilk, can interfere with milk establishment and maintenance (Geddes et al., 2021; Pérez-Escamilla et al., 2019, 2023). It is therefore crucial for mothers to breastfeed effectively by having their infants remove the milk from their breasts, or to express milk via another means such as a breast pump, to maintain milk production (Geddes et al., 2021).
Moreover, interactions between the breastfeeding dyad, in the context of their environment, provide the feedback mechanism that shapes the varying composition of milk over the course of the day and over the development of the child (Pérez-Escamilla et al., 2023). These interactions also play a crucial role in psychosocial development and maternal well-being. For example, oxytocin, a neuropeptide, may be inhibited by stress responses, such as release of corticosteroids or conditions of chronic stress, while at the same time, oxytocin has been found to modulate stress responses and may be in part the mechanism for decreased anxiety, improvement of maternal mental health, and increased ability to socially bond during breastfeeding (Hantsoo et al., 2023; Olff et al., 2013). Thus, while human milk is itself a complex system, it needs to be examined in the context of the broader breastfeeding relationship (Pérez-Escamilla et al., 2023; Quinn et al., 2023).
BREASTFEEDING ACROSS THE LIFE COURSE
Part of the committee’s task was to explore contributing factors that impact breastfeeding rates and access to breastfeeding services and supplies. To address this, the committee developed its report using a life course framework in recognition that various exposures across different stages of life can influence future chronic disease risk and other health outcomes (Lynch & Smith, 2005). This framework identifies multiple determinants (i.e., exposures) that may influence individual and community health, including biological and genetic, behavioral, economic, and social factors (Halfon & Hochstein, 2002; see also Chapter 3 for the influence of social ecological factors on breastfeeding differences). In the case of lactation and breastfeeding, an infant and mother’s health trajectories are influenced by exposure to both risk and protective factors, as well as the infant and the mothers early life experiences, which can then influence breastfeeding and associated health outcomes at the population level. With this understanding in mind, the committee recognizes that the breastfeeding dyad progresses through a lactation journey, from preconception to birth to postpartum, return to school and work, and infancy, amid these intersecting influences. The committee identified critical inflection points across the life course that are specific to human lactation, breastfeeding, and the provision of human milk (Figure 2-1). Each of these inflection points presents both challenges
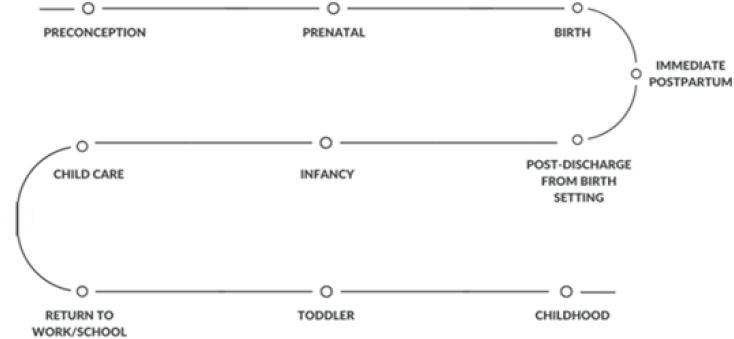
and opportunities. Interventions at these points can create an enabling environment for breastfeeding that provides the best opportunities for women and families to achieve their personal breastfeeding goals. Such interventions can also improve national breastfeeding rates.
This journey map begins with the mother at preconception, then follows her and her infant prenatally, at birth, immediately postpartum, and post-discharge from a birth setting. It continues for both the mother and infant, and identifies critical time points that impact both, including securing childcare and returning to work or school; it includes ongoing child development milestones from toddler to childhood. Protective and risk factors are described by inflection or time point, and additional considerations are presented for the sick or vulnerable breastfeeding dyad.
Preconception
Research demonstrates the importance of fetal health and parents’ preconception health on a child’s health (National Academies of Sciences, Engineering, and Medicine [National Academies], 2019, p. 25466, 2024, p. 27835; Schrott et al., 2022). Recognizing the genetic, epigenetic, and environmental factors that affect health risks for the next generation (Cheng et al., 2016; Hanson & Gluckman, 2014), a growing body of literature documents the intergenerational transmission of health and disease and trans-generational effects of social and environmental exposures and epigenetics on health (Benincasa et al., 2024; Breton et al., 2021; Kioumourtzoglou et al., 2018; Scorza et al., 2019; Tan et al., 2024). As such, the life course perspective prompts consideration of the health of the breastfeeding dyad today, the adults the current infants will become, and the new families they will create.
Opportunities to discuss breastfeeding begin before pregnancy. Education about the importance of breastfeeding for infants and mothers, its value for communities and society, and the developmental stages of breast development can be started in schools or at adolescent health care visits during pubertal changes (Jack et al., 2024). However, education curriculum and studies on their implementation are limited.
Well-women visits during childbearing years, which contain a breast evaluation, present an opportunity to discuss future reproductive plans and the importance of lactation and breastfeeding for a woman’s health and the health of the baby, as well as opportunities for breastfeeding support, supplies, and counseling covered by the Affordable Care Act, if this is needed in the future (Health Resources and Services Administration, 2025).
Prenatal
For the mother, the process of human lactation includes distinct phases and begins during pregnancy (i.e. “lactogenesis stage I”; Geddes et al., 2021). In the first lactation phase, during pregnancy, the mammary glands are stimulated in preparation for breastfeeding the infant at birth. During this time, the placenta produces hormones responsible for the continued growth and differentiation of the tissue of the mammary gland, and the ductal system within the breast expands and branches in response to estrogen (Alex et al., 2020; Lawrence & Lawrence, 2021; Sriraman, 2017). During the prenatal period, progesterone is highly elevated and suppresses, to a large extent, the capacity of the mammary glands to secrete milk.
The prenatal period is a critical time for women to be provided health promotion strategies, including primary and secondary prevention through screening and management of risk factors (see Chapter 6) and related health conditions to promote and sustain a healthy pregnancy, birth, and breastfeeding journey (Howell, 2018). Known maternal or fetal conditions that may impact breastfeeding can also be identified during the prenatal period and appropriate can be counseling provided (Spatz et al., 2024; Stuebe, 2020). Some factors that may put a mother at risk for not meeting her personal breastfeeding goals include anatomic variations of the breast (Cruz & Korchin, 2007, 2010; Neifert et al., 1985; Stuebe et al., 2014), substance use disorders (Harris et al., 2023), mental health conditions (Buck et al., 2018; Dugat et al., 2019; Eagen-Torkko et al., 2017; Kitsantas et al., 2019; Martin-de-Las Heras et al., 2019; Miller-Graff et al., 2018; Wallenborn et al., 2018), diabetes (Mitanchez et al., 2015), and both high and low maternal body mass index (Chapman & Pérez-Escamilla, 1999; Chen et al., 2020; Garcia et al., 2016; Nommsen-Rivers et al., 2022).
Chronic disease prevalence among childbearing women is rising in the United States. From 2005 to 2014, the proportion of women who gave birth with at least one chronic condition increased from 6.7% to 9.2%, with Admon et al. (2017) reporting the highest rates among women living in rural or low-income zip codes and women insured by Medicaid. Some women with chronic health conditions, such as hypertension, endocrine and metabolic diseases, and obesity, for example, may face specific risk factors that make breastfeeding more challenging without additional or specialized clinical lactation support (Arenas et al., 2025; Stuebe, 2022). The management of these conditions may need to be tailored to accommodate the physical and metabolic demands of lactation. These conditions can influence lactation, and in turn, may also be affected by the act of breastfeeding itself (Stuebe, 2022).
Existing evidence-based and supportive policies, as well as best practices in the field, can mitigate these risk factors and support mothers as they prepare to breastfeed their infants (Jack et al., 2024). For example, systematic reviews demonstrate that women who receive breastfeeding prenatal education in health care offices have higher rates of initiation and duration, and are more likely to exclusively breastfeed; this is shown to be particularly effective when education is paired with postpartum support (Kehinde et al., 2023; Olufunlayo et al., 2019; Patnode et al., 2016; Pérez-Escamilla et al., 2023; Rollins et al., 2016; Tomori et al., 2022).
Jack et al. (2024) concluded that prenatal education is most effective and has the greatest impact on breastfeeding outcomes when guidance is focused on the benefits of breastfeeding on infant and maternal health, as well as practices and problem-solving to support early initiation of breastfeeding. In addition, domestic and international evidence demonstrates that educational programs are most effective when they promote breastfeeding self-efficacy in a structured format (Admasu et al., 2022; Araban et al., 2018; Behera & Kumar, 2015; Cangöl & Şahin, 2017; Fauzia et al., 2020; Galipeau et al., 2018; Mizrak et al., 2017; Modi et al., 2019; Öztürk et al., 2022; Sabancı Baransel et al., 2023; You et al., 2020; Zhao et al., 2021).
In addition, evidence demonstrates that midwives, lactation consultants, other lactation support providers, and doulas can positively affect breastfeeding initiation and duration, particularly in low-income, racially minoritized communities (see Chapters 3 and 6; Bonuck et al., 2014; Hartman et al., 2012; Kehinde et al., 2023; Louis-Jacques et al., 2020; Reno, 2018). Research also shows that support from peer counselors and community health workers during the prenatal period is effective in improving breastfeeding outcomes in community-based settings (Khatib et al., 2023; Louis-Jacques et al., 2020; Reno, 2018; Sobczak et al., 2023; see also Chapter 3).
Birth
Following birth and delivery of the placenta, the sharp decline in progesterone triggers secretory activation of the mammary glands (Geddes et al., 2021; Pérez-Escamilla & Chapman, 2001). This stage of lactation, still considered to be part of lactogenesis stage I, involves the secretion of strongly immune-active colostrum, or first milk, in small amounts (Geddes et al., 2021; Pérez-Escamilla & Chapman, 2001). The conditions and supports available during childbirth can set the stage for early breastfeeding. Andrew et al. (2022) reported that breastfeeding outcomes are better for women who have uncomplicated, full term, vaginal births of vigorous, healthy babies.
Protective and Risk Factors
The Academy of Breastfeeding Medicine (ABM) has identified several characteristics of the birth experience and process that can be either protective or risk factors for breastfeeding (Holmes et al., 2013). For example, during labor and delivery, the continuous presence of a close companion, such as a spouse, partner, or other family member, is beneficial for the mother (Holmes et al., 2013). In addition, Kozhimannil et al. (2013) reported that the presence of a doula is associated with increased initiation and duration of breastfeeding and may mitigate risk factors associated with early cessation of breastfeeding, including surgical and pain-reducing interventions (see also Hodnett et al., 2013; Mottl-Santiago et al., 2008; Nommsen-Rivers et al., 2009). Risk factors for not initiating breastfeeding include birth complications and associated interventions, such as intrapartum analgesia, exogenous oxytocin, and ergometrine (Holmes et al., 2013; see also Beilin et al., 2005; Gizzo et al., 2012; Jordan et al., 2009; Montgomery et al., 2012).
Regarding birth attendants and settings, Vedam et al. (2018) found breastfeeding rates to be higher in states with laws and regulations that support midwifery integration in care. A National Academies committee examining maternal and newborn care in the United States found consistent correlations between birth setting and breastfeeding rates, with low-risk home and birth center deliveries associated with higher rates of breastfeeding initiation and exclusive breastfeeding 6–8 weeks after birth (National Academies, 2020). Less than 1% of women give birth at home and 0.52% in free-standing birth centers (MacDorman & Declercq, 2019). While the report acknowledges that variation in breastfeeding outcomes by birth setting is at least partially attributable to selection bias, as individuals choosing home or birth center births are often highly committed to breastfeeding, the report also suggests that the “wellness-oriented, individualized,
relationship-centered approach of midwifery care across home, birth center, and hospital settings” is a contributing factor for differential outcomes (National Academies, 2020, p. 207). Interestingly, Gregory et al. (2021), analyzed data from the National Vital Statistics System and reported an increase in home births during the COVID-19 pandemic. They report that in 2020, the rate of home births increased by 19% (Gregory et al., 2021) and interest in home birth searches spiked significantly after declaration of the COVID-19 pandemic occurred (Cheng et al., 2022).
Complicated Deliveries
In the United States, 31.8% of women underwent induction of labor in 2020 (Simpson, 2022), and 32.3% birthed by C-section in 2023 (National Center for Health Statistics, 2025).
A population-based study in Australia of infants born at or before 37 weeks found that interventions in labor, such as C-section, epidural anesthesia, and infusion of oxytocin, were associated with higher rates of formula supplementation in the hospital and lower rates of breastfeeding at three and six months postpartum (Andrew et al., 2022). Of note, this study did not include information on maternal health conditions, such as diabetes and hypertension, that can both require induction of labor and affect breastfeeding outcomes.
More difficult labors are associated with early breastfeeding difficulties. In a study among low-risk mothers in northern California (Dewey et al., 2003), longer labor and longer intervals without sleep were associated with later onset of lactogenesis II, the transition from colostrum to milk production. In adjusted models, stage II of labor longer than one hour was associated with delayed onset of milk production and suboptimal infant breastfeeding behavior. As noted above, support from companions and doulas may help mitigate against some of these risk factors (Kozhimannil et al., 2013).
Cesarean birth is associated with lower rates of early initiation of breastfeeding; exclusive breastfeeding at hospital discharge; and exclusive breastfeeding at one, three, and six months postpartum (Ulfa et al., 2023). Promising practices for improving maternal experience and breastfeeding outcomes following cesarean birth include additional support (Beake et al., 2017) and skin-to-skin care in the operating room following C-section (Frederick et al., 2020).
As previously mentioned, postpartum hemorrhage is a leading cause of maternal morbidity, and higher blood loss at delivery is associated with lower rates of fully breastfeeding in the first postpartum week and at both two and four months postpartum (ACOG, 2017; Del Ciampo & Del Ciampo, 2018; Thompson et al., 2010; Victora et al., 2016). U.S. birth
certificate data from 2016 to 2023 shows an association between maternal transfusion and lower rates of breastfeeding at discharge (69.9% vs. 74.8%). An analysis of the ARRIVE trial conducted by Roberts et al. (2025) found that postpartum hemorrhage with transfusion was associated with lower odds of exclusive or any breastfeeding at 4–8 weeks postpartum. For example, a cohort study of women with postpartum hemorrhage, defined as more than 1500 mL of blood loss, found that higher blood loss and longer delays in initiation predicted lower full breastfeeding rates at one week postpartum (Thompson et al., 2010). Additional lactation support in the intrapartum period and beyond have been recommended to address breastfeeding challenges among those experiencing postpartum hemorrhage (Roig et al., 2024; Thompson et al., 2010).
In summary, more difficult labor, C-section, and heavy bleeding after birth predict more breastfeeding difficulties and earlier weaning. Judicious use of interventions in labor, as well as opportunities for early skin-to-skin contact and breastfeeding initiation, and more support for breastfeeding dyads with difficult births, can help more women achieve their infant feeding goals. Chapter 6 describes best practices for clinicians and health care systems to support the breastfeeding dyad in the ambulatory or hospital setting.
Immediate Postpartum
Lactogenesis stage II, or the secretory stage, begins around 48–72 hours after birth, with the onset of lactation or coming to volume. In this stage, more copious amounts of milk secretion begin, although there is wide variability among women (Geddes et al., 2021; Pérez-Escamilla & Chapman, 2001).
Risk and Protective Factors
Postpartum care provides an opportunity to identify and potentially mitigate additional birth- and neonatal-related risk factors for inadequate milk production, delay in the secretory stage, and early breastfeeding cessation. These risk factors include
- low birth weight,
- lower gestational age,
- stressful or prolonged labor and birth,
- unscheduled C-section,
- postpartum hemorrhage,
- delayed first breastfeeding episode,
- breastfeeding or pumping fewer than eight times in 24 hours,
- formula supplementation within the first 48 hours, and
- separation of the dyad at birth.
(See Brown & Jordan, 2013; Chapman & Pérez-Escamilla, 1999, 2012; Dewey et al., 2003; Furman et al., 2002; Grajeda & Pérez-Escamilla, 2002; Hobbs et al., 2016; Huang et al., 2020; McCoy & Heggie, 2020; Meier et al., 2017; Parker et al., 2021; Salariya et al., 1978; Scheeren et al., 2022; Thompson et al., 2010).
A significant number of women experience a delayed onset of lactation (>72 hours after birth), which is a risk factor for shorter exclusive and any breastfeeding durations (Feldman-Winter et al., 2020; Pérez-Escamilla et al., 2019). This is especially the case for mothers of preterm or critically ill infants requiring specialized care in neonatal intensive care units (Hoban et al., 2018; Juntereal, 2024; Mago-Shah et al., 2023; Parker et al., 2021). However, many factors associated with delayed lactation can be prevented or mitigated.
Rooming In
During the hospital stay, mother–infant rooming-in on a 24-hour basis is associated with optimal breastfeeding initiation (Holmes et al., 2013). Health care providers may need to assist mothers with positioning and attaching their babies at the breast, and those who delivered by C-section may need additional help to attain comfortable positioning. Holmes et al. (2013) recommend that at least once every 8–12 hours after delivery a trained lactation support provider assess and document breastfeeding effectiveness until the breastfeeding dyad is discharged. This clinical protocol notes that “peripartum care of the dyad should address and document infant positioning, latch, milk transfer, baby’s weight, clinical jaundice, and any problems raised by the mother, such as nipple pain or the perception of an inadequate breastmilk supply” (Holmes et al., 2013, p. 270; see also Feldman-Winter et al., 2020).
Today, rooming in is the predominate norm in hospital settings (Centers for Disease Control and Prevention [CDC], 2024; see Chapter 6). However, the CDC (2024) reports that early separation remains a practice in 10% of hospitals, and 16% of hospitals have not implemented rooming in. Flacking et al. (2012) noted that infants who are preterm or require additional care may face more significant separation while they are cared for by a pediatric team; the mother may be recovering in the postpartum unit or discharged while the infant is still hospitalized. For neonatal intensive care, family-centered, single-family room design is an opportunity to ensure that mothers and infants are kept together, facilitating more connected models of care, better breastfeeding outcomes, and better outcomes for parents (e.g., European Standards of Care for Newborn Health, 2019; van Veenendaal et al., 2019, 2020). While promising, and although efforts to maintain proximity in the neonatal intensive care unit have increased, the committee notes that the United States has not yet adopted models of family-centered, single-family room design on a large scale.
Skin-to-Skin Care
The ABM advises that healthy newborns should be given directly to the mother for skin-to-skin contact until after the first feeding. The infant may be dried and assigned Apgar scores, and the initial physical assessment may be performed as the infant is placed with the mother. [. . .] Delaying procedures such as weighing, measuring, administering eye prophylaxis as well as vitamin K, up to six hours after birth, and the initial bath enhances early parent–infant interaction. Infants are to be put close to the breast, as soon after birth as is feasible for both mother and infant, to allow for a latch and feeding, ideally within an hour of birth. (Holmes et al., 2013, p. 470)
There is substantial evidence that early skin-to-skin contact facilitates early breastfeeding initiation and is associated with increased duration of any and exclusive breastfeeding (see Bramson et al. 2010; DiGirolamo et al., 2008; Hung & Berg, 2011; Mahmood et al., 2011; Mikiel-Kostyra et al., 2002; Moore et al., 2016; Murray et al., 2007; Thukral et al., 2012).
Uninterrupted skin-to-skin care immediately following birth improves breastfeeding outcomes. A meta-analysis of randomized controlled trials by Moore et al. (2016) found that placing infants with the mother skin to skin for the first 60–90 minutes following birth increased breastfeeding duration by 64 days. In addition, skin-to-skin care and early initiation of breastfeeding are a core tenet of the Ten Steps to Successful Breastfeeding (World Health Organization & United Nations Children’s Fund, 2018). The AAP has delineated key aspects of safe implementation of skin-to-skin care in the delivery setting, including continual observational monitoring by trained staff so that sudden changes to maternal or newborn status can be addressed immediately (Feldman-Winter et al., 2016). In addition, CDC monitors hospital implementation of skin-to-skin care as part of the Maternity Practices in Infant Nutrition and Care (mPINC) Survey (see Chapter 4 for additional surveillance measures).
In 2007, 40.4% of hospitals reported that most patients experienced mother–infant skin-to-skin contact for at least 30 minutes within one hour of an uncomplicated vaginal birth (see Figure 2-2). The prevalence of this practice increased to 83% in 2015 (Boundy et al., 2022). After 2017, mPINC revised the survey to assess skin-to-skin contact for at least one hour after vaginal birth; on the most recent survey, 70% of hospitals reported that this was their standard of care (Boundy et al., 2022).
Severe Maternal Morbidity
Mothers experiencing severe maternal morbidity require interdisciplinary care to address acute, life-threatening conditions (Bingham et al., 2011). Severe maternal morbidity and mortality is a composite measure of 20 unexpected outcomes of labor and delivery, quantified using maternal
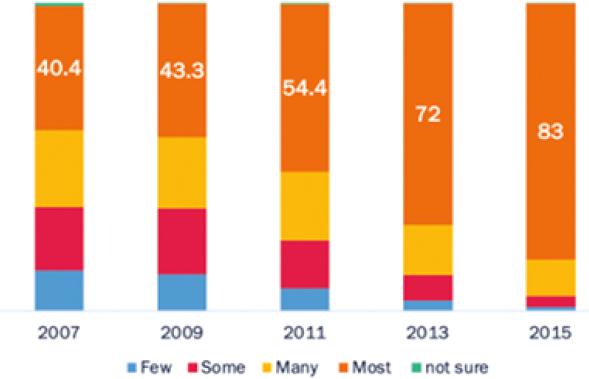
SOURCE: Adapted from Boundy et al., 2018.
diagnosis codes from the birth hospitalization. Rates of severe maternal morbidity and mortality in the United States have continued to rise. According to Reid (2024), rates increased 40% overall from 2016 to 2021 and by 20% when excluding delivery stays with COVID-19.
Often, a mother with severe maternal morbidity is transferred from maternity care to an intensive care unit (ICU), where she is separated from her infant and may be intubated or sedated. This separation can present challenges for breastfeeding (Bartick et al., 2021). ICU staff may not be familiar with lactation physiology and may require assistance to express milk to prevent engorgement and/or mastitis. By regularly expressing milk until the mother is awake and alert, the critical care team can protect her right to decide whether to breastfeed her infant. Facilitating breastfeeding can be an important part of easing the psychological trauma of a maternal ICU admission (Hinton et al., 2015; Intensive Care Society, 2018).
Academy of Breastfeeding Medicine guidelines on supporting breastfeeding for hospitalized mothers include allowing the infant to room in with the mother, providing equipment for milk expression, and ensuring that the care team has access to evidence-based information on medications in lactation (Bartick et al., 2021).
Infant Loss
When a mother is pregnant, her body is typically biologically prepared to lactate. Secretory differentiation begins in the second trimester with
lactogenesis stage I. Thus, even if a mother experiences a second trimester pregnancy loss, an intrauterine fetal death, or the death of a child immediately post birth, the physiologic process of lactation will occur normally (Carroll et al., 2020). With the delivery of the placenta and the associated hormonal impact, the body will likely begin converting to lactogenesis stage II. This process of secretory activation will occur even without an infant suckling at the breast.
Hospitals or birth settings may not adequately prepare mothers for this experience and how to navigate these physical symptoms and suppress lactation (see Britz & Henry, 2013; Carroll et al., 2020; Redshaw et al., 2014). Carroll et al. (2020) described examples of advice and techniques for milk suppression, including nonpharmacological means to relieve symptoms, as well as pharmacological pain relief options. In addition, they present a framework based on supporting evidence for online health information, including acknowledging lactation after infant loss, describing breast changes associated with the production of human milk, advice on alleviating symptoms, suppression options, and sustained milk expression options (Caroll et al., 2020).
Not all families may wish to suppress lactation following a pregnancy loss or death of a child. For example, some mothers may wish to initiate milk expression after a second trimester loss, an intrauterine fetal demise, or immediate death of a child, as part of the grieving process (Paraszczuk et al., 2022). Cole et al. (2018) found that parents are not generally given information about milk donation and navigating the grief journey and the lactation journey following a loss. Families may need to determine how to get a breast pump, as insurance may not provide one if there is not a living child. Because of the challenges that bereaved parents may go through to continue their lactation journeys, additional research in this population would be helpful to better support families’ differing experiences.
Inducing Lactation
Some parents may desire to induce lactation even in the absence of a pregnancy. Inducing lactation, though possible for some nonbirth parents, requires significant time, effort, and financial investment, in addition to the desire and commitment to make it possible. Parents must plan far in advance and seek out support from qualified medical professionals. Those who are inducing lactation need medication and technology to support their lactation journey. A scoping review found limited evidence regarding how best to induce lactation (Cazorla-Ortiz et al., 2020). The ABM provides recommendations for nonbirth parents who wish to induce lactation, as well as an overview of the use of galactagogues in initiating or augmenting maternal milk production (Brodribb & ABM, 2018; Ferri et al., 2020).
Additional Considerations for the Sick or Vulnerable Infant
About 7.5% of infants are hospitalized in the first year of life (Weiss et al., 2022), most commonly for acute respiratory conditions. Although hospitalization can disrupt breastfeeding, interventions to promote ongoing lactation and ensure evidence-based staff support can reduce unwanted weaning (Ben Gueriba et al., 2021). Moreover, pediatric critical care units can develop breastfeeding and breastmilk storage policies to support the breastfeeding dyad (Bartick et al., 2021).
Breastfeeding medically complex children presents multiple challenges. In a narrative synthesis, Hookway et al. (2021) reported that when an infant is hospitalized, mothers must navigate the logistics of expressing, storing, and delivering milk, as well as the psychological stress of separation and anxiety. The infant’s acute condition can affect their ability to feed, as can an underlying chronic condition. Lack of specialized breastfeeding support, inadequate knowledge of health team members, and uneven access to specialized equipment were additional barriers identified by the authors (Hookway et al., 2021). There are multiple levels of neonatal care, and the availability of breastfeeding support and donor human milk4 varies by level (Anstey et al., 2024).
Donor Human Milk
In the United States, donor human milk is primarily regulated through nonprofit milk banks that follow strict safety guidelines. Human Milk Banking Association of North America (HMBANA) is a not-for-profit milk bank that provides standards for donor human milk banking. For example, potential donors may undergo health screenings, and donated milk is pasteurized and tested for contaminants. Most donor human milk is provided to preterm and critically ill infants who are in the hospital NICU. Currently, demand for donor human milk exceeds the available supply in the United States (see Bai & Kuscin, 2021; Hamilton & Middlestadt, 2024). In 2024, HMBANA-affiliated milk banks dispensed 11 million ounces of pasteurized donor human milk, a 10% increase from 2023 (Human Milk Banking
___________________
4 Donor human milk is pasteurized human milk provided by lactating parents who donate their surplus milk to milk banks. It is primarily used for medically fragile infants, especially preterm babies in NICUs, when a mother’s own milk is unavailable or insufficient. As described earlier in the chapter, donor human milk confers protection from necrotizing enterocolitis, a life-threatening condition, to preterm infants. At the time of this report, the U.S. Food and Drug Administration (2018) advises against informal milk sharing; however, the practice continues in the United States (Bressler et al., 2020; Martino & Spatz, 2014; McNally & Spatz, 2020; Spatz, 2016). Health care providers can help parents make informed decisions, informed by position statements and guidance from the ABM and the American Academy of Nursing and Academy of Breastfeeding Medicine (Sriraman et al., 2018).
Association of North America, 2025). State Medicaid programs and other insurers may pay for donor human milk when medically necessary.
It is important to note that donor milk is not a replacement for a mother’s own milk but can serve as a bridge to allow milk supply to be established, if the parent is able to lactate. Encouraging direct breastfeeding before discharge from the NICU may help prolong breastfeeding duration. As discharge approaches, health care providers must decide on the most suitable post-discharge feeding plan to ensure continued nutrition and support for the infant (Noble et al., 2018).
Post-Discharge from Birth Setting
The management of lactation during the first few weeks postpartum is essential for establishing a milk supply (Institute of Medicine, 1991). Through a biologically complex process, women increase their human milk production to about 750 millileters daily on average by three months after birth (Geddes et al., 2021). Most women with multiple births have the capacity to produce enough milk for all their offspring (Flidel-Rimo & Shinwell, 2006), highlighting the enormous plasticity of the human lactation process.
The ABM recommends that breastfed infants see a health care provider within 24–72 hours following discharge from the hospital or at 3–5 days old to assess the infant’s well-being and whether breastfeeding has been established successfully (Holmes et al., 2013; see also Committee on Fetus and Newborn, 2010; Hoyt-Austin et al., 2022; Labarere et al., 2005; Section on Breastfeeding, 2012).
However, reflecting the current fragmentation of care and the need for coordination, most mothers in the United States receive postpartum care from an obstetrician, family physician, midwife, or nurse practitioner, while their infant is cared for by a pediatrician who works in a different office, which may use a different electronic health record system. This can create challenges for the breastfeeding dyad. Lactation is a complex, two-person biosocial system, ultimately involving maternal milk production and infant milk extraction and ingestion usually through close bodily interaction (see Chapter 6).
Lactation problems post-discharge from the birth hospital are common and often reflect the challenges and structural barriers to lactation encountered within the health care system (see Chapter 6). This may result in problem-oriented visits to a doctor or a lactation support professional who may inappropriately recommend supplementation or weaning—outcomes that can often be prevented with effective care. Effective management by a mother’s physician, advanced practice professional, or lactation support provider is necessary to protect breastfeeding, especially exclusive breastfeeding. Currently, no universal structure supports payment of lactation care for problem-oriented visits if they are not provided by a physician
or advanced practice professional. Some, but not all, insurance companies reimburse a certain number of visits to lactation consultants; only certain states offer Medicaid payment for lactation consultants (see Chapter 7).
During the first two weeks after birth, breastfeeding 8–12 times during a 24-hour period is associated with establishment of adequate milk production (Geddes et al., 2021; Hill et al., 2005). However, infants usually feed more frequently than this; close contact with frequent opportunities to breastfeed also helps establish successful breastfeeding (Zimmerman et al., 2023). Additionally, peer support has been found to promote breastfeeding success (Holmes et al., 2013; Renfrew et al., 2012; Sudfeld et al., 2012; see Chapter 3).
ACOG examined factors that can interfere with women achieving their breastfeeding goals (American College of Obstetricians and Gynecologists, 2021). One factor that can lead to early and undesired weaning includes nipple injury or persistent pain during breastfeeding. There are many possible contributors to pain during breastfeeding, and obstetrician-gynecologists or other obstetric care professionals that women see for post-birth care can play an important role in diagnosing and treating the causes of pain to foster continued breastfeeding (American College of Obstetricians and Gynecologists, 2021). As pain during breastfeeding can be associated with postpartum depression, screening for postpartum depression is an important component of assessment for these patients (American College of Obstetricians and Gynecologists, 2021; see also ACOG, 2016; Amir, 1996; Watkins et al., 2011).
Self-reported insufficient milk supply is another risk factor for early weaning (Segura-Pérez et al., 2022). For mothers concerned about having adequate milk supply, providers and clinicians need to evaluate whether underlying physiologic or psychosocial issues are contributing to the perception of inadequate supply. Mothers can be reassured that indicators of adequate milk supply include feeding frequency of 8–12 times per day on average, steady weight gain after the infant is 4–5 days old, and an average of 6–8 wet diapers per day (American College of Obstetricians and Gynecologists, 2021). Infants typically gain back normal post-birth weight loss by 10–14 days after birth; care providers need to alleviate mothers’ concerns that the infant being below their birth weight is an indicator of inadequate milk supply if the infant is not yet two weeks old. Clinicians can use standardized tools, such as the Newborn Weight Tool, to assess growth trajectories and take into consideration birth factors such as fluids administered to the mother before and during birth, and cesarean delivery, that may yield greater weight-loss patterns in infants (Flaherman et al., 2015). Also, feedings more frequent than 8–12 times per day are not necessarily an indicator of insufficient milk supply, as human milk is easily digested (American College of Obstetricians and Gynecologists, 2021). When low milk supply occurs, supporting mothers in more frequent direct breastfeeding or milk expression (e.g., pumping) can often help to increase supply (American College of Obstetricians and Gynecologists, 2021).
Infancy
A critical element of successful breastfeeding relates to the mother’s ability to interpret infant behavior and to respond to their child’s needs, which creates feedback loops of coordination between the dyad (Pérez-Escamilla et al., 2023). For instance, responding to babies’ need to be close and to be fed frequently simultaneously provides reassurance, soothing, and security, and is a major determinant of early breastfeeding success, which also plays a role in exclusive breastfeeding and breastfeeding duration (see Box 2-1).
BOX 2-1
Physiological Infant Care
Young infants require frequent contact and feedings day and night. This box provides a protocol for managing normal physiology for the breastfeeding dyad.
Normal Infant Feeding Patterns
Newborn infants breastfeed approximately 8–12 times per 24 hours; this does not always occur at regular intervals. Responsive feeding is advised, as feeding according to infant cues can ensure that they receive their needed daily nutrition. Infants can self-regulate their nutritional intake by nonnutritive and nutritive suckling. Continuous proximity and skin-to-skin contact with mothers or parents help with infant temperature, breathing, and heart rate regulation.
Normal Infant Sleep Patterns
Newborn infants are born without a functional circadian clock; melatonin passed through human milk can help establish an infant’s circadian rhythm, as can exposure to daytime activities and differentiating them from nighttime (e.g., avoiding artificially darkening rooms for daytime sleep). Expectations of prolonged infant sleep periods are unrealistic, and sleep training infants younger than six months of age can cause significant infant stress and parental distress, and it can impact breastfeeding because of the physical separation of a mother and her infant during the night. The Academy of Breastfeeding Medicine’s protocol is focused on infant sleep patterns as they relate to breastfeeding, which may differ from existing American Academy of Pediatrics recommendations on sleep training.
Supporting Physiological Infant Care
At times, cultural expectations of typical infant behavior and normal physiology are misaligned. Strategies for reducing such misalignment may include addressing expectations that infants sleep through the night, or that solitary sleep without breastfeeding for infants is typical or desirable. In reality, infant sleep is fragmented and breastfeeding infants tend to sleep as well as or better than their formula-fed counterparts. Strategies that support this care and help mothers maximize their recovery, rest, and sleep, include support from fathers, partners, and family members; paid family and medical leave; and accessible and affordable child care.
SOURCE: Zimmerman et al., 2023.
Infants must be permitted to feed on cue, as limiting the time that an infant is at the breast can be detrimental to establishing adequate milk supply. Infants usually release the breast spontaneously or fall asleep when they are satiated (Holmes et al., 2013). Proper postnatal care can be protective for breastfeeding. As noted in Box 1-3, parental expectations of prolonged infant sleep periods may be unrealistic and can be a risk factor for breastfeeding success, particularly if such beliefs lead parents to engage in sleep training for infants younger than six months of age (Zimmerman et al., 2023).
As noted in the box above, community support plays a critical role in shaping breastfeeding success by influencing the environments in which families live, work, and seek care. While clinical and workplace supports are essential, community-based efforts help ensure that breastfeeding is normalized, socially supported, and practically feasible across diverse settings (e.g., Rhodes et al., 2024; see Chapter 4 for additional discussion).
Childcare
For many families, attempting to secure childcare before returning to work or school can produce increased feelings of stress and anxiety, as well as increased reporting of depressive symptoms (Armstrong et al., 2022; Ceballos et al., 2017; Heck, 2021; Laughlin, 2013). Previous research by Armstrong et al. (2022) and Beck (2001) has shown that access to childcare may help mitigate negative effects of sleep deprivation and childcare stress, and support maternal mental health. In a series developed for the Center for American Progress, Malik et al. (2018) reported that approximately 50% of Americans live in childcare deserts. The authors defined childcare desert as an area or community with an inadequate number of licensed childcare providers and facilities (Malik et al., 2018). Given the dearth of accessible and affordable childcare options, newly postpartum mothers and families may spend a large amount of time and resources trying to identify a childcare provider who best fits their infants and families’ needs.
Reliable and affordable childcare is critical for supporting breastfeeding outcomes, particularly as families navigate the postpartum period. Childcare plays a dual role: it supports children’s early development and enables parents to remain engaged in the workforce (Schneider & Gibbs, 2023). However, the high cost of care and financial instability of providers pose significant challenges (U.S. Department of Labor, 2024). Childcare settings can either support or hinder breastfeeding, depending on their practices. Breastfeeding-friendly environments that store and handle breastmilk safely, feed infants responsively, delay solid food until six months, communicate supportively, and provide lactation spaces for parents help
protect breastfeeding continuity. Conversely, when these elements are absent, families are at greater risk of not achieving their breastfeeding goals. Chapter 8 further examines the intersection of childcare and the return to work or school, a critical transition period for lactating parents.
Return to Work or School
Given the need for consistent contact between mothers and children to support and sustain breastfeeding journeys, the transition for women back to the workforce or school presents a significant challenge. In the United States, the absence of a national paid family leave policy means that many mothers return to work within weeks of giving birth (see Chapter 8).
Maternal employment has been identified as a structural determinant of infant feeding decisions across the globe (Baker et al., 2023; Perez-Escamilla et al., 2023). Low-wage workers experience more pronounced differences related to workplace accommodations and policies (California WIC Association, 2025).
The process of returning to work or school after pregnancy varies widely depending on individual circumstances, employer policies, and institutional support systems. For many, this transition requires flexibility and support to ensure a smooth adjustment to new routines.
Working mothers encounter distinct challenges in breastfeeding, resulting in lower rates of initiation and shorter durations than those for nonworking mothers (Chatterji & Frick, 2005; Duthei et al., 2021). These challenges persist despite evidence highlighting the health advantages of breastfeeding for both mother and child (see Chapter 1), as well as the diverse strategies available for supporting breastfeeding women in the workplace (e.g., Litwan et al., 2021).
Return to work or school can be a difficult experience for women, as they must learn to blend breastfeeding and/or pumping into the work or school environment (e.g., Gabriel et al., 2020; Little & Masterson, 2021). Many workplaces lack adequate facilities for expressing milk or policies that accommodate breastfeeding needs (Kozhimannil et al., 2016; Lowenfels et al., 2024). Health insurance and paid leave can significantly impact how a new parent manages their physical and mental health and financial well-being during pregnancy and postpartum. Additionally, understanding whether paid leave is available—and for how long—can make a significant difference in planning for the postpartum period and balancing work or educational obligations with caregiving responsibilities.
Given these challenges associated with reentering the workforce (or school), this period for working mothers has been described as an “emotional whirlwind” (Spiteri & Xuereb, 2012, p. 206) and dubbed
the fifth trimester (Brody, 2018), during which “the working mother is born” (Chawla et al., 2024, p. 2); she must navigate how her professional and caregiving (i.e., childcare, family) roles work together (i.e., enrich) or conflict (Gabriel et al., 2020). Working mothers may also be grappling with mental health challenges associated with motherhood, such as postpartum depression (Chawla et al., 2024; Gabriel et al., 2023), which can be compounded by difficulties transitioning back to school or work. Indeed, during this time, mothers who are employed may feel as though they are violating both “ideal worker norms” and “ideal mother norms,” not being fully available to either their work role or their motherhood role (Ladge et al., 2015; Little & Masterson et al., 2023).
Toddler
The Meek et al. (2022) and WHO (2023a) recommend continuing breastfeeding after introducing solid foods as long as mutually desired for up to two years or beyond (Meek et al., 2022). Protective factors for continuing breastfeeding into toddlerhood include flexibility to accommodate the toddler’s variable desire for breastfeeding, such as seeking more frequent feeding during times of stress or transition (e.g., La Leche League, 2020). Risk factors for earlier-than-desired weaning may include poor or inadequate support during birth and in the postnatal period, the demands of returning to work, as well as the influence of commercial milk formula and toddler milk marketing (Pérez-Escamilla et al., 2023). It may also result from disrupted lactation, which may be attributed to untreated risk factors (e.g., see Stuebe et al., 2014) or other structural influences.
Weaning can also be a personal decision, and it differs by mother and family (CDC, 2024). Children and parents may be ready to wean from breastfeeding at different times; some children gradually lose interest as they eat more solids, while others stop suddenly; parents’ readiness can vary as well. Weaning may be a gradual process, conducted with or before the introduction of complementary foods. Consultation with a health care provider is essential to ensure that a child’s nutritional needs are adequately met.
Childhood
Physical development related to lactation begins during childhood. One of the earliest signs is breast development, known as thelarche, which typically starts around ages 9–10 years but can begin as early as eight years (Geddes et al., 2021). This process includes increased pigmentation of the areola and the formation of a small mound of tissue under the nipple
called the breast bud. Breast development usually unfolds over a span of 3–3.5 years and begins approximately 1–2 years before the onset of menstruation (Geddes et al., 2021). During puberty, the mammary ducts begin to grow into the mammary fat pads. Once menstruation begins and ovulation occurs, the hormone progesterone stimulates some development of the lobuloalveolar structures (i.e., the milk-producing components of the breast). These alveolar clusters enlarge during the luteal phase of the menstrual cycle and regress at the start of menses (Geddes et al., 2021). This cyclical development lays the groundwork for the breast’s ability to produce milk in response to pregnancy and childbirth later in life.
Attitudes toward breastfeeding begin to form early in life, often during childhood. The 2003 WHO/United Nations Children’s Fund Global Strategy for Infant and Young Child Feeding highlighted the importance of engaging school aged children and adolescents to positively improve perceptions and raise awareness about breastfeeding (World Health Organization & United Nations Children’s Fund, 2003). Children’s perceptions of infant feeding are shaped by what they observe in their homes, communities, and especially in media, where bottle feeding is often more visible than breastfeeding (see Chapter 4). These early exposures help establish what children view as “normal” or socially acceptable. As such, integrating breastfeeding into school-based education on human development, such as health or life sciences, can help promote more informed and positive attitudes toward breastfeeding (Angell et al., 2011). Educational efforts that include realistic portrayals of breastfeeding can also challenge stigma and reinforce the role of breastfeeding as a natural and beneficial practice. Broader sociocultural factors, including family norms, cultural beliefs, and public attitudes, further shape how individuals view and experience breastfeeding. For an in-depth discussion of these influences, see Brown (2018) and Tomori et al. (2018).
Adulthood
In adulthood, community-level and interpersonal influences affect an individual’s views about breastfeeding. As discussed in greater detail in Chapter 3, cultural influences, community attitudes, family norms, and traditions can influence the extent to which individuals hold a positive attitude toward breastfeeding (see also Brown, 2018; Quinn et al., 2023; Tomori et al., 2018). As described above, breastfeeding is associated with a reduced risk of mothers developing certain chronic diseases as well as improvements in postpartum recovery.
Conclusion 2-1: Human lactation is a multifaceted physiological process that is influenced by a range of factors operating across the life
course. The capacity to breastfeed, and the outcomes associated with breastfeeding, are determined by a combination of biocultural mechanisms and external factors, including clinical practices; health system structures; and social, structural, and environmental conditions experienced throughout an individual’s and family’s life. Preconception health, prenatal care, birth experience, postpartum recovery, and the return to work or school each represent critical windows in which the foundations for optimal breastfeeding can be laid.
There are numerous challenges to breastfeeding across the life course, but each inflection point identified above also presents opportunities to create an enabling environment for breastfeeding. The scientific literature reveals opportunities for timely and effective intervention or support. For example, prenatal breastfeeding education, continuity of lactation support providers, family-centered care at birth, paid leave, and supportive return-to-work or school policies have all been shown to increase breastfeeding initiation and duration (see Chapters 3, 6, 7, and 8). Special considerations are warranted for vulnerable breastfeeding dyads, including those affected by infant and maternal morbidity and mortality, as well as those pursuing induced lactation.
CURRENT STATUS OF BREASTFEEDING IN THE UNITED STATES
As noted in Chapter 1, the United States has been unable to meet the modest breastfeeding targets set by Healthy People 2030. This section presents data on breastfeeding initiation in the United States and trends in breastfeeding duration and exclusivity between 2014 and 2021. It then explores differences in breastfeeding by population group and discusses protective and risk factors across the life course. Chapter 3 focuses on structural determinants that influence these community-level differences, as well as historical shifts in the cultural perception of breastfeeding.
Breastfeeding Initiation
Breastfeeding initiation, or the percentage of live infants “receiving any breast milk or colostrum between delivery and discharge from the birth facility or birth certificate completion for home births,” varies by county and state, and ranges from 22% to 90% (CDC, 2024a, para. 3). The national average of breastfeeding initiation, using birth certificate data from the National Vital Statistic System (NVSS), is estimated to be 83.2% (CDC, 2022; see Figure 2-3).
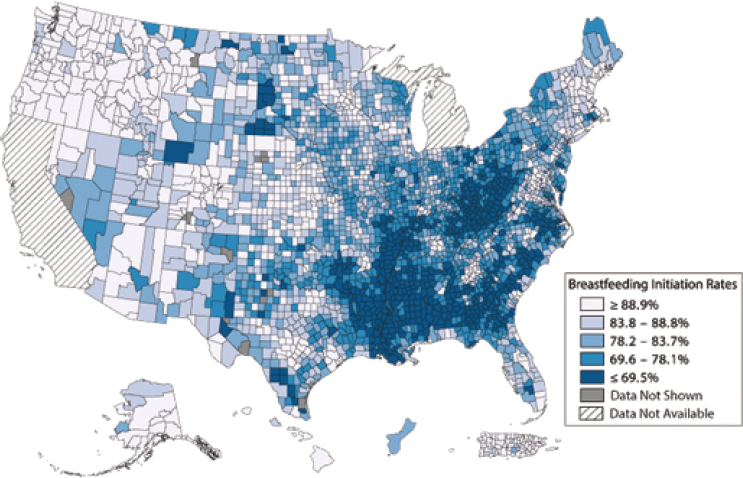
NOTE: Birth certificate breastfeeding initiation data were not available for California, Michigan, American Samoa, or the U.S. Virgin Islands. In addition, to prevent identification of individuals, data are not shown for counties or county equivalents if the total number of infants or the number of infants initiating breastfeeding is fewer than 10; the exact breastfeeding rate is not displayed if it is greater than or equal to 90.0% and the total number of infants is fewer than 50.
SOURCE: CDC, 2025a.
Breastfeeding Exclusivity and Duration
In addition to the NVSS data on initiation, the National Immunization Survey-Child gathers information on breastfeeding initiation, exclusivity, and duration (CDC, 2024b). According to CDC, 84.1% of infants born in 2021 were ever breastfed or initiated breastfeeding. However, by six months, only 59.8% of infants were still breastfeeding or receiving human milk, and at 12 months, this number dropped to 39.5% (CDC, 2025b; Figure 2-4). Sixty percent of mothers who begin breastfeeding report that they stop sooner than they planned (Diaz et al., 2023; Odom et al., 2013). These figures demonstrate that while most mothers initiate breastfeeding, many face barriers that prevent them from meeting national breastfeeding recommendations or their own breastfeeding intentions.
Exclusive breastfeeding falls sharply each month postpartum; in 2021, 46.5% of mothers reported exclusive breastfeeding at three months, and
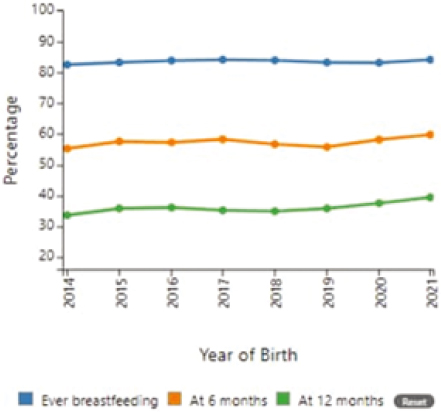
SOURCE: CDC, 2025b.
27.2% at six months (see Figure 2-5; CDC, 2024). Over the last seven years, these rates have remained relatively stagnant.
Variances in Breastfeeding Rates
Breastfeeding rates in the United States have shown improvement over the last 50 years, but significant variances persist across racial, ethnic,
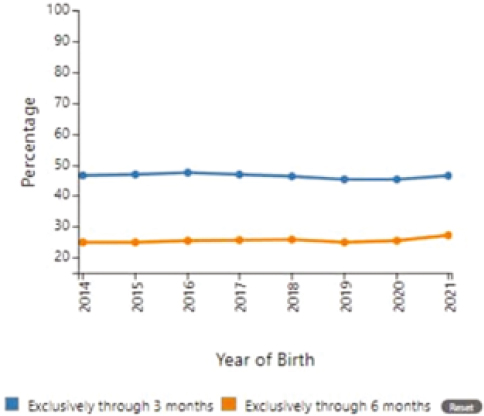
SOURCE: CDC, 2025b.
geographic, and socioeconomic lines (CDC, 2022; Chiang et al., 2021; Diaz et al., 2023).
Race and Ethnicity
Data from CDC (n.d.) reveal that racial/ethnic variances in breastfeeding rates are particularly pronounced. While the overall prevalence of breastfeeding initiation is 84% (Marks et al., 2023), fewer non-Hispanic Black infants (75.4%) are ever breastfed compared with Asian (92.7%), non-Hispanic White (86.2%), and Hispanic infants (83.4%). However, due to greater investments and community-led interventions, increases in breastfeeding initiation and duration of Black infants have been observed over the last 10 or more years (Asiodu et al., 2021).
Two other racial subgroups also had prevalence estimates of less than 80% initiation: American Indian or Alaskan Native (77.7%) and Other Pacific Islanders (79.4%; Marks et al., 2023). These variances persist and often widen at six and 12 months postpartum (CDC, n.d.).
Marks et al. (2023) disaggregated breastfeeding initiation data by subgroups, revealing significant variations within broader racial/ethnic categories. For instance, among Asian mothers, Japanese women had the highest breastfeeding initiation rate at 94%, while Filipino women had a rate of 91.3%. Among Hispanic mothers, Cuban women had the highest initiation rate (90.0%), while Puerto Rican mothers had the lowest (82.2%; Marks et al., 2023). This granular analysis highlights the importance of considering cultural and ethnic subgroups when addressing breastfeeding variances.
Geography
Geographic inequalities in breastfeeding rates are also evident in the data, with significant variations across states and between urban and rural areas. The CDC (2022) Breastfeeding Report Card shows that the percentage of infants breastfed at six months ranges from 31.7% in West Virginia to 73.2% in Vermont. Figure 2-6 illustrates regional differences, with Southeastern states generally having lower breastfeeding rates than Western and Northeastern states (CDC, 2024). Rural areas tend to have lower breastfeeding rates than urban areas, which may be attributed to factors such as limited access to lactation support services and cultural norms (Aschbrenner & Cornish, 2017; Chiang et al., 2021). Chiang et al. (2021) and Raju et al. (2022) noted that because outcomes vary by state, it may be necessary to implement targeted efforts to address the unique needs of each state. The authors suggested that policies and practices in maternity care that promote breastfeeding, along with programs aimed at high-risk populations, could enhance initiation rates, lessen variances, and improve nutrition for infants (Chiang et al., 2021).
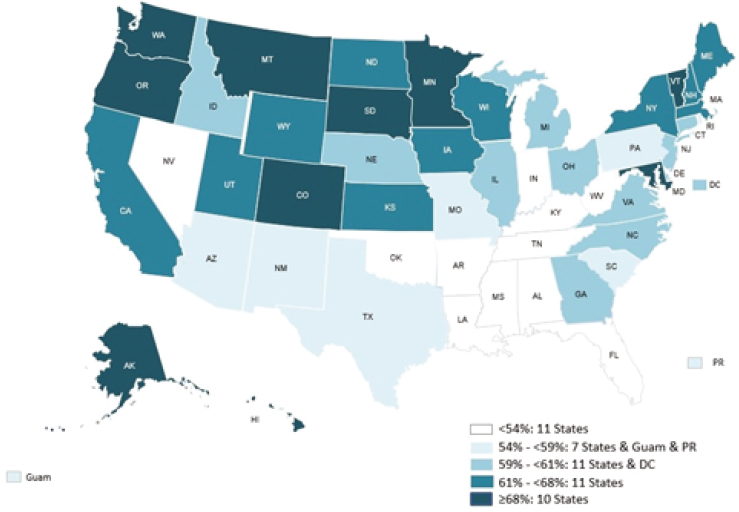
SOURCE: CDC, 2025b.
Socioeconomic Status
Breastfeeding outcomes also vary by socioeconomic status. Mothers with lower education levels and lower household incomes are less likely to initiate and continue breastfeeding than their more affluent counterparts (Seoane Estruel & Andreyeva, 2025). Notably, the relationship between participation in WIC and breastfeeding rates is complex. While WIC provides breastfeeding support and education, studies have shown that WIC participants have lower breastfeeding rates compared with eligible nonparticipants (Ryan & Zhou, 2006; Zhang et al., 2021). Additionally, a study analyzing data from the 2016–2018 National Survey of Children’s Health found that WIC participants had lower breastfeeding rates than the general U.S. population (Parasuraman et al., 2020).
However, recent research suggests that WIC participation may be associated with improvements in breastfeeding rates among certain populations (U.S. Department of Agriculture, 2024). A study analyzing data from 2009 to 2017 found that breastfeeding initiation increased for low-income women in all racial/ethnic groups, with gaps narrowing between WIC participants and eligible nonparticipants within some racial/ethnic groups (Shetler et al., 2023). This trend indicates that WIC’s efforts to promote
breastfeeding may be having a positive impact, particularly among populations with historically lower breastfeeding rates (Metallinos-Katsaras et al., 2015; Segura-Pérez et al., 2021).
Factors contributing to breastfeeding variances are multifaceted and include lack of paid family leave, unsupportive workplace policies, limited access to quality health care and lactation support, cultural norms, and aggressive marketing of commercial milk formula (Office of the Surgeon General et al., 2011; Petit et al., 2021). Additionally, scholars have found associations between historical and system-level factors, such as racism and discrimination and lower breastfeeding rates among certain racial/ethnic groups (Griswold et al., 2019; Johnson et al., 2016; Robinson et al., 2019).
The COVID-19 pandemic and subsequent infant formula shortage in 2022 highlighted the vulnerability of formula-dependent families and led to an increase in breastfeeding initiation rates (Asiodu, 2022; Tomori & Palmquist, 2022). This increase was particularly pronounced among populations with historically lower breastfeeding rates, including mothers with lower education levels, WIC participants, and Black mothers (Marino et al., 2023; Seoane Estruel & Andreyeva, 2025). This unexpected event demonstrated the potential for addressing breastfeeding variances through targeted interventions and support.
THE COST OF INACTION
As part of their charge, the committee was tasked with exploring the ‘macroeconomic, health, and social costs of current U.S. breastfeeding rates’ (see Box 1-1 in Chapter 1). Existing economic literature measures the overall costs of current, suboptimal U.S. breastfeeding rates, as well as the value of benefits that could be gained by raising breastfeeding rates to optimal levels. See Box 2-2 for a detailed discussion of the methodological approaches used to measure the costs of current breastfeeding rates. Although current cost estimation models are impacted by uncertainty, existing evidence consistently shows large annual costs of suboptimal breastfeeding rates in the United States. Increasing U.S. breastfeeding rates would avoid these short- and long-term costs, resulting in economic benefits.
A scoping study by Jegier et al. (2024) offers a comprehensive review of studies of the economic cost consequences of suboptimal breastfeeding reaching back to the 1990s. The authors identified four approaches used by researchers to estimate costs: microcosting (‘bottom-up’ approach), static modeling (‘top-down’ approach), dynamic modeling (‘top-down’ simulation approach), and macroeconomic (‘replacement cost; foregone value’ approach; see Table 2-2). The earlier microcosting approach, which focused on using cost-accounting data to measure the direct impacts of low
BOX 2-2
Measuring the Costs of Current Suboptimal Breastfeeding Rates
Approaches to measuring the macroeconomic, or overall costs, of current breastfeeding rates are framed by comparing current, lower rates with rates such as those recommended by the World Health Organization (2021) and United Nations Children’s Fund, which call for nearly universal (in practice, usually set at 90%) early initiation of breastfeeding, exclusive breastfeeding at six months, and introduction of nutritionally adequate and safe complementary (solid) foods at six months, together with continued breastfeeding through two years of age and beyond as mutually desired. These rates are referred to as optimal, with current, lower rates labeled suboptimal.
The studies then measure the costs associated with suboptimal breastfeeding. For example, if 27.2% of infants are exclusively breastfed to six months, as was the rate in the United States in 2021, and the optimal rate is 90%, then the difference of 62.8% indicates the percentage of infants and parents who may experience the impacts of suboptimal breastfeeding and the costs that could be avoided (benefits that could be attained) if current rates rose to meet the optimal level. While most studies compare current breastfeeding rates to an optimal rate, some studies compare current rates to lower target rates, such as the U.S. Healthy People 2030 goal of 42.4% (a difference of 15.2%).
Studies identify major categories of the impacts of lower rates and quantify the range and size of those impacts. They then estimate the economic value of the impacts and aggregate those values into an overall estimate of the costs of current breastfeeding rates, again compared with optimal or other target rates. Several studies on the overall burden of current breastfeeding rates have been presented in the format of cost calculators that allow users to estimate costs for different geographical areas or populations. These costs (benefits that could be achieved) can then be compared with the cost of investments that could result in higher breastfeeding rates.
Approaches to measuring the macroeconomic, or overall, costs of current breastfeeding rates identify, based on evidence in the medical literature, the health impacts on full-term infants, sick or vulnerable (including preterm) infants, and mothers that result from lower-than-recommended breastfeeding levels. The cost studies make judgments, based on the literature, about which of these impacts on health and development to include in their analyses. They also consider the economic costs of the outcomes per case for individuals, families, and society, and the sizes of the populations affected. Studies may also include related costs, such as the costs of parental time needed to care for infants or children with higher incidence of negative outcomes due to lower breastfeeding rates. The studies then aggregate costs over time to calculate annual costs.
SOURCE: Committee generated; WHO, 2021.
TABLE 2-2 Definition and Description of Costing Approaches
| Approach | Common Methods of Measurement | Limitations to Method | Examples of This Type of Study |
|---|---|---|---|
| Micro-costing (‘bottom up’ approach) | Direct measurement of actual financial costs using cost-accounting data. | Relies on risk ratios which may not accurately define infant feeding exposure. Does not have proscriptive, universally accepted methodological approach to defining or measuring costs. May use insurance payment or provider charge data, but neither may represent actual costs. Rarely encompasses costs of mother’s time. |
Ball & Wright, 1999; Jegier et al., 2010 |
| Static modelling (‘top down’ approach) | Costs are extrapolated over a fixed period of time covering finite episodes of illness using epidemiologic risk ratios for illness or disease by type of infant feeding exposure. | Relies on risk ratios which may not accurately define infant feeding exposure. Not tracking cost impacts probabilistically over time so less accurate. Costing of episodes rather than total disease costs over a period. Limited by multiple assumptions on disease incidence in the case of chronic diseases, and wide variability in cost assumptions. Only accounts for health costs, not for mother’s time. |
Drane, 1997; Bartick & Reinhold, 2010; Colchero et al., 2015; Rollins et al., 2016; Walters et al., 2019 |
| Approach | Common Methods of Measurement | Limitations to Method | Examples of This Type of Study |
|---|---|---|---|
| Dynamic modelling (‘top down’ simulation approach) | Builds on the static modelling but using a dynamic probabilistic (e.g., Markov chain) computer simulation (e.g. Monte Carlo) model. Usually measures cost impacts of multiple diseases in large hypothetical population of women and/or their offspring over long periods of time, such as from birth to age 70. | As above for static computation. Relies on probabilistic assumptions about risk ratios by age. Discounting rate choices more influential on cost outcomes. |
Bartick et al., 2013; Bartick et al., 2017; Unar-Munguia et al., 2017 |
| Macroeconomic (‘Replacement cost; foregone value’) | Cost to a country of replacing maternal human milk at contemporary breastfeeding rates with breastmilk substitutes or donor human milk. Suboptimal breastfeeding cost may be calculated by subtracting this cost from the cost at an ideal or target breastfeeding rate, which would be the value of ‘lost’ milk due to low breastfeeding rates. | Relies accurately defining infant feeding exposure. Willingness to pay as a measure of value may not capture utility or social value. Prices and valuation based on willingness to pay may understate the economic value of breastmilk due to imperfect scientific knowledge of the health impacts of formula feeding. The cost of women’s time to breastfeed or express donor milk is not accounted for so it measures gross not net value-added. |
Aguayo & Ross, 2002; Smith & Forester, 2013, Lee, 2013, Lee, 2015 |
NOTE: See source for full example reference entries.
SOURCE: Jegier et al., 2024, licensed under CC BY-ND 4.0.
breastfeeding rates, has been supplanted by static and dynamic modeling approaches that allow a broader range of impacts and longer time frames to be included in the analyses (Jegier et al., 2024).
Stuebe et al. (2017) used a dynamic model to simulate population-level changes in disease burdens and costs for several pediatric and maternal
health outcomes based on different marginal increases in breastfeeding rates. They found that a 5% increase in U.S. breastfeeding rates was associated with statistically significant reductions in child infectious morbidity for two outcomes (otitis media and gastrointestinal infection) in the first year of life, with a total medical cost reduction of $44 million (Stuebe et al., 2017). Bartick et al. (2017) used dynamic modeling to measure the outcomes of suboptimal breastfeeding in the United States for nine pediatric and five maternal diseases, with estimated excess deaths of 721 children and 2,619 women due to suboptimal breastfeeding. They estimate the medical costs of pediatric and maternal diseases at $3 billion annually and the costs of premature deaths at $14.2 billion, for a total of $17.2 billion (Bartick et al., 2017).
Rollins et al. (2016) use static modeling to estimate the economic costs of lower cognitive development of children and of increased child morbidity related to suboptimal breastfeeding rates. Based on estimates of cognitive development impacts from a systematic analysis by Horta et al. (2015), Rollins et al. (2016) reported annual losses due to lower cognitive development of $302 billion worldwide, with high-income country losses of $231.4 billion and those of the United States at $84 billion. They estimated that the costs of child morbidity would be reduced by $2.45 billion annually in the United States at optimal breastfeeding rates (Rollins et al., 2016).
Walters et al. (2019) used static modeling to analyze a broader range of impacts in their tool to estimate the global cost of not breastfeeding, including health care system costs for two pediatric illnesses and one maternal illness, potential lower earnings due to lost IQ points for children, and potential earnings losses due to premature mortality for children and mothers. Overall, Walters et al. (2019) estimated that the annual costs of not breastfeeding globally are $341 billion. The estimated cost for North America is $115 billion annually, made up almost entirely of costs due to cognitive losses, as limited data were available for the other costs. Walters et al. (2019) note,
The estimates are likely to be conservative since the economic costs of increased household caregiving time, which are mainly borne by women, transportation costs, and several child and maternal diseases that can be prevented in part by breastfeeding are not included in the model due to the data availability. (p. 409)
The committee recognizes that there is uncertainty in the estimates of the costs of suboptimal breastfeeding. For example, costs may be overestimated if the extent of health and cognitive impacts from low breastfeeding rates are overestimated. Costs may be underestimated if a range of impacts and cost categories are excluded or incompletely included in estimates, reflecting evidence that may be incomplete or missing on the impacts, size of impacts, or disagreement on what to count.
The estimated total costs of suboptimal breastfeeding depend, as noted above, on the impacts that are included in the studies and the costing methodology. For example, Bartick et al. (2016) focused on a wide range of pediatric and maternal diseases, estimating related medical costs and costs of premature death to be $17.2 billion annually for the United States. In their scoping article, Jegier et al. (2024) noted that “the optimal infant feeding practice of breastfeeding requires maternal time. Yet almost all studies, even those from a ‘societal’ perspective neglect the time costs to mothers” (p. 916). In the cost analyses reviewed here, this neglect is a result of not including the indirect costs to households of caring for sick children associated with not breastfeeding (Jegier et al., 2024, p. 941). They noted that, “Costs varied depending on methodology and perspective. Medical costs were dwarfed by cognitive losses and the economic costs of premature death” (Jegier et al., 2024, p. 940). That said, Jegier et al. (2024) concluded that the body of studies available consistently estimate the total costs of suboptimal breastfeeding to exceed $100 billion annually for the United States.
Conclusion 2-2: Suboptimal breastfeeding rates in the United States result in preventable costs. While cost estimates vary depending on methodology, the existing evidence points to annual national losses between $17 billion and over $100 billion. These figures may underestimate the full burden, because preventable costs from the full range of negative health outcomes from suboptimal breastfeeding, as well as indirect costs, such as caregiver time and transportation, are not captured because of data limitations. There is also potential to overestimate the burden, if the extent of health and cognitive impacts upon which cost estimates are built are overestimated.
Chapter 3 of this report explores breastfeeding in the community context, including the influence of intersecting systems and social ecological factors across settings (e.g., public health policies and programs; media, marketing, and messaging; health care and payment for services and supplies; employers and schools). The following chapters will explore leverage points across these settings and describe best practices, investments, and promising approaches to increasing overall breastfeeding initiation, exclusivity, and duration in the United States and to reducing differences in breastfeeding rates between mothers from different populations and for those experiencing poverty.
REFERENCES
Admasu, J., Egata, G., Bassore, D. G., & Feleke, F. W. (2022). Effect of maternal nutrition education on early initiation and exclusive breast-feeding practices in south Ethiopia: A cluster randomised control trial. Journal of Nutritional Science, 11, e37. https://doi.org/10.1017/jns.2022.36
Admon, L. K., Winkelman, T. N. A., Moniz, M. H., Davis, M. M., Heisler, M., & Dalton, V. K. (2017). Disparities in chronic conditions among women hospitalized for delivery in the United States, 2005–2014. Obstetrics and Gynecology, 130(6), 1319–1326. https://doi.org/10.1097/AOG.0000000000002357
Alex, A., Bhandary, E., & McGuire, K. P. (2020). Anatomy and physiology of the breast during pregnancy and lactation. Advances in Experimental Medicine and Biology, 1252, 3–7. https://doi.org/10.1007/978-3-030-41596-9_1
Alimi, R., Azmoude, E., Moradi, M., & Zamani, M. (2022). The association of breastfeeding with a reduced risk of postpartum depression: A systematic review and meta-analysis. Breastfeeding Medicine, 17(4), 290–296. https://doi.org/10.1089/bfm.2021.0183
Altobelli, E., Angeletti, P. M., Verrotti, A., & Petrocelli, R. (2020). The impact of human milk on necrotizing enterocolitis: A systematic review and meta-analysis. Nutrients, 12(5), 1322. https://doi.org/10.3390/nu12051322
American College of Obstetricians and Gynecologists (ACOG). (2016). Committee Opinion No. 658: Optimizing support for breastfeeding as part of obstetric practice. Obstetrics & Gynecology, 127(2), e86–e92. https://doi.org/10.1097/AOG.0000000000001318
———. (2017). Postpartum hemorrhage. Practice bulletin 183. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2017/10/postpartum-hemorrhage
———. (2021). Breastfeeding challenges: ACOG Committee Opinion, Number 820. Obstetrics & Gynecology, 137(2), e42–e53. https://doi.org/10.1097/AOG.0000000000004253
———. (2023). Practice advisory to update the duration of breastfeeding [Practice Advisory]. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2023/02/duration-of-breastfeeding-update
Amir, L. H., Dennerstein, L., Garland, S. M., Fisher, J., & Farish, S. J. (1996). Psychological aspects of nipple pain in lactating women. Journal of Psychosomatic Obstetrics and Gynaecology, 17(1), 53–58. https://doi.org/10.3109/01674829609025664
Andrew, M. S., Selvaratnam, R. J., Davies-Tuck, M., Howland, K., & Davey, M.-A. (2022). The association between intrapartum interventions and immediate and ongoing breastfeeding outcomes: An Australian retrospective population-based cohort study. International Breastfeeding Journal, 17(1), Article 1. https://doi.org/10.1186/s13006-022-00492-7
Angell, C., Alexander, J., & Hunt, J. A. (2011). How are babies fed? A pilot study exploring primary school children’s perceptions of infant feeding. Birth, 38(4), 346–353. https://doi.org/10.1111/j.1523-536X.2011.00484.x
Anstey, E., Noiman, A., Boundy, E., & Nelson, J. (2024). Maternity care practices supportive of breastfeeding in U.S. advanced neonatal care units, United States, 2022. Journal of Perinatology, 44, 1560–1566. https://doi.org/10.1038/s41372-024-02139-3
Araban, M., Karimian, Z., Karimian Kakolaki, Z., McQueen, K. A., & Dennis, C.-L. (2018). Randomized controlled trial of a prenatal breastfeeding self-efficacy intervention in primiparous women in Iran. Journal of Obstetric, Gynecologic & Neonatal Nursing, 47(2), 173–183. https://doi.org/10.1016/j.jogn.2018.01.005
Arenas, G., Barrera, M. J., & Contreras-Duarte, S. (2025). The impact of maternal chronic inflammatory conditions on breast milk composition: Possible influence on offspring metabolic programming. Nutrients, 17(3), 387. https://doi.org/10.3390/nu17030387
Armstrong, B., Weaver, R. G., Beets, M. W., Østbye, T., Kravitz, R. M., & Benjamin-Neelon, S. E. (2022). Use of child care attenuates the link between decreased maternal sleep and increased depressive symptoms. Journal of Developmental and Behavioral Pediatrics, 43(5), e330–e338. https://doi.org/10.1097/DBP.0000000000001048
Aschbrenner, K., & Cornish, D. L. (2017). Barriers to breastfeeding among rural women in the United States. UNIversitas: Journal of Research, Scholarship, and Creative Activity, 12(1), Article 12. https://scholarworks.uni.edu/universitas/vol12/iss1/12/
Asiodu, I. V. (2022). Infant formula shortage: This should not be our reality. The Journal of Perinatal & Neonatal Nursing, 36(4), 340–343. https://doi.org/10.1097/JPN.0000000000000690
Asiodu, I. V., Bugg, K., & Palmquist, A. E. L. (2021). Achieving breastfeeding equity and justice in black communities: Past, present, and future. Breastfeeding Medicine, 16(6), 447–451. https://doi.org/10.1089/bfm.2020.0314
Bai, Y., & Kuscin, J. (2021). The current state of donor human milk use and practice. Journal of Midwifery & Women’s Health, 66(4), 478–485. https://doi.org/10.1111/jmwh.13244
Baker, P., Smith, J. P., Garde, A., Grummer-Strawn, L. M., Wood, B., Sen, G., Hastings, G., Pérez-Escamilla, R., Ling, C. Y., Rollins, N., McCoy, D., & 2023 Lancet Breastfeeding Series Group. (2023). The political economy of infant and young child feeding: Confronting corporate power, overcoming structural barriers, and accelerating progress. Lancet, 401(10375), 503–524. https://doi.org/10.1016/S0140-6736(22)01933-X
Bartick, M., Hernández-Aguilar, M. T., Wight, N., Mitchell, K. B., Simon, L., Hanley, L., Meltzer-Brody, S., & Lawrence, R. M. (2021). ABM Clinical Protocol No. 35: Supporting breastfeeding during maternal or child hospitalization. Breastfeeding Medicine, 16(9), 664–674. https://doi.org/10.1089/bfm.2021.29190.mba
Bartick, M. C., Schwarz, E. B., Green, B. D., Jegier, B. J., Reinhold, A. G., Colaizy, T. T., Bogen, D. L., & Stuebe, A. M. (2016). Suboptimal breastfeeding in the United States: Maternal and pediatric health outcomes and costs. Maternal & Child Nutrition. https://doi.org/10.1111/mcn.12366
Bartick, M., Zimmerman, D. R., Sulaiman, Z., Taweel, A. E., AlHreasy, F., Barska, L., Fadieieva, A., Massry, S., Dahlquist, N., Mansovsky, M., & Gribble, K. (2024). Academy of Breastfeeding medicine position statement: Breastfeeding in emergencies. Breastfeeding Medicine, 19(9), 666–682. https://doi.org/10.1089/bfm.2024.84219.bess
Beake, S., Bick, D., Narracott, C., & Chang, Y.-S. (2017). Interventions for women who have a caesarean birth to increase uptake and duration of breastfeeding: A systematic review. Maternal & Child Nutrition, 13(4), e12390. https://doi.org/10.1111/mcn.12390
Beck C. T. (2001). Predictors of postpartum depression: An update. Nursing Research, 50(5), 275–285. https://doi.org/10.1097/00006199-200109000-00004
Behera, D., & Kumar, A. (2015). Predictors of exclusive breastfeeding intention among rural pregnant women in India: A study using theory of planned behaviour. Rural and Remote Health, 15(3405). http://www.rrh.org.au
Beilin, Y., Bodian, C. A., Weiser, J., Hossain, S., Arnold, I., Feierman, D. E., Martin, G., & Holzman, I. (2005). Effect of labor epidural analgesia with and without fentanyl on infant breastfeeding: A prospective, randomized, double-blind study. Anesthesiology, 103, 1211–1217.
Belfort, M. B., Rifas-Shiman, S. L., Kleinman, K. P., Guthrie, L. B., Bellinger, D. C., Taveras, E. M., Gillman, M. W., & Oken, E. (2013). Infant feeding and childhood cognition at ages 3 and 7 years: Effects of breastfeeding duration and exclusivity. JAMA Pediatrics, 167(9), 836–844. https://doi.org/10.1001/jamapediatrics.2013.455
Ben Gueriba, K., Heilbronner, C., Grimaud, M., Roy, E., Hadchouel, A., Hachem, T., de Barbeyrac, C., Murmu, M., Renolleau, S., & Rigourd, V. (2021). Simple actions to support breastfeeding can avoid unwanted weaning in infants younger than 6 months hospitalized for bronchiolitis: A before/after study (Bronchilact II). Archives De Pediatrie: Organe Officiel De La Societe Francaise De Pediatrie, 28(1), 53–58. https://doi.org/10.1016/j.arcped.2020.10.004
Benincasa, G., Napoli, C., & DeMeo, D. L. (2024). Transgenerational epigenetic inheritance of cardiovascular diseases: A network medicine perspective. Maternal and Child Health Journal, 28(4), 617–630. https://doi.org/10.1007/s10995-023-03886-z
Bingham, D., Lyndon, A., Lagrew, D., & Main, E. K. (2011). A state-wide obstetric hemorrhage quality improvement initiative. The American Journal of Maternal/Child Nursing, 36(5), 297–304. https://doi.org/10.1097/NMC.0b013e318227c75f
Birukov, A., Guasch-Ferré, M., Ley, S. H., Tobias, D. K., Wang, F., Wittenbecher, C., Yang, J., Manson, J. E., Chavarro, J. E., Hu, F. B., & Zhang, C. (2024). Lifetime duration of breastfeeding and cardiovascular risk in women with type 2 diabetes or a history of gestational diabetes: Findings from two large prospective cohorts. Diabetes Care, 47(4), 720–728. https://doi.org/10.2337/dc23-1494
Bonuck, K., Stuebe, A., Barnett, J., Labbok, M. H., Fletcher, J., & Bernstein, P. S. (2014). Effect of primary care intervention on breastfeeding duration and intensity. American Journal of Public Health, 104(Suppl 1), S119–127. https://doi.org/10.2105/AJPH.2013.301360
Boundy, E. O., Anstey, E. H., & Nelson, J. M. (2022). Donor human milk use in advanced neonatal care units—United States, 2020. MMWR. Morbidity and Mortality Weekly Report, 71(33), 1037–1041. https://doi.org/10.15585/mmwr.mm7133a1
Boundy, E. O., Perrine, C. G., Barrera, C. M., Li, R., & Hamner, H. C. (2018). Trends in maternity care practice skin-to-skin contact indicators: United States, 2007–2015. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 13(5), 381–387. https://doi.org/10.1089/bfm.2018.0035
Bramson, L., Lee, J. W., Moore, E., Montgomery, S., Neish, C., Bahjri, K., & Melcher, C. L. (2010). Effect of early skin-to-skin mother—infant contact during the first 3 hours following birth on exclusive breastfeeding during the maternity hospital stay. Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 26(2), 130–137. https://doi.org/10.1177/0890334409355779
Bressler, T., Dambra-Candelaria, L. M., & Spatz, D. L. (2020). Informal milk sharing for the hospitalized at-risk infant in the Ultra-Orthodox-Haredi Jewish community in the United States. Breastfeeding Medicine, 15(5), 357–364. https://doi.org/10.1089/bfm.2019.0216
Breton, C. V., Landon, R., Kahn, L. G., Enlow, M. B., Peterson, A. K., Bastain, T., Braun, J., Comstock, S. S., Duarte, C. S., Hipwell, A., Ji, H., LaSalle, J. M., Miller, R. L., Musci, R., Posner, J., Schmidt, R., Suglia, S. F., Tung, I., Weisenberger, D., Zhu, Y., & Fry, R. (2021). Exploring the evidence for epigenetic regulation of environmental influences on child health across generations. Communications Biology, 4(1), 769. https://doi.org/10.1038/s42003-021-02316-6
Britz, S. P., & Henry, L. (2013). Supporting the lactation needs of mothers facing perinatal and neonatal loss. Journal of Obstetric, Gynecologic & Neonatal Nursing, 42(Suppl 1), S105–S106. https://doi.org/10.1111/1552-6909.12207
Brodribb W., & the Academy of Breastfeeding Medicine. (2018). ABM Clinical Protocol #9: Use of galactogogues in initiating or augmenting maternal milk production, second revision 2018. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 13(5), 307–314. https://doi.org/10.1089/bfm.2018.29092.wjb
Brody, L. S. (2018). The fifth trimester: The working mom’s guide to style, sanity, and success after baby. Anchor.
Brown, A. (2018). Sociological and cultural influences upon breastfeeding. In Breastfeeding and Breast Milk – from Biochemistry to Impact (pp. 149–158). Georg Thieme Verlag. https://doi.org/10.21428/3d48c34a.2a0f254a
Brown, A., & Jordan, S. (2013). Impact of birth complications on breastfeeding duration: An internet survey. Journal of Advanced Nursing, 69(4), 828–839. https://doi.org/10.1111/j.1365-2648.2012.06067.x
Brown, J. V. E., Walsh, V., & McGuire, W. (2019). Formula versus maternal breast milk for feeding preterm or low birth weight infants. The Cochrane Database of Systematic Reviews, 8(8), CD002972. https://doi.org/10.1002/14651858.CD002972.pub3
Buck, C. O., Gjelsvik, A., Vivier, P. M., Monteiro, K., & Amanullah, S. (2018). Prenatal exposure to stressful life events and infant breastfeeding. Breastfeeding Medicine, 13(6), 426–432. https://doi.org/10.1089/bfm.2017.0200
California WIC Association. (2020). Lactation support for low-wage workers [Issue brief]. https://calwic.org/maternal-care/lactation-support-for-low-wage-workers/
Cangöl, E., & Şahin, N. H. (2017). The effect of a breastfeeding motivation program maintained during pregnancy on supporting breastfeeding: A randomized controlled trial. Breastfeeding Medicine, 12(4), 218–226. https://doi.org/10.1089/bfm.2016.0190
Carroll, K., Noble-Carr, D., Sweeney, L., & Waldby, C. (2020). The “Lactation After Infant Death (AID) Framework”: A guide for online health information provision about lactation after stillbirth and infant death. Journal of Human Lactation, 36(3), 480–491. https://doi.org/10.1177/0890334420926946
Cazorla-Ortiz, G., Obregón-Gutiérrez, N., Rozas-García, M. R., & Goberna-Tricas, J. (2020). Methods and success factors of induced lactation: A scoping review. Journal of Human Lactation, 36(4), 739–749. https://doi.org/10.1177/0890334420950321
Ceballos, M., Wallace, G., & Goodwin, G. (2017). Postpartum depression among African American and Latina mothers living in small cities, towns, and rural communities. Journal of Racial and Ethnic Health Disparities, 4(6), 916–927. https://doi.org/10.1007/s40615-016-0295-z
Centers for Disease Control and Prevention (CDC). (n.d.). Infant Feeding Practices Study II: Table data, chapter 2. https://www.cdc.gov/breastfeeding/pdf/ifps/data/ifps2_tables_ch2.pdf
———. (2022). Breastfeeding Report Card: United States, 2022. U.S. Department of Health and Human Services. https://www.cdc.gov/breastfeeding-data/media/pdfs/2024/06/2022-Breastfeeding-Report-Card-508.pdf
———. (2024a). Breastfeeding initiation rates by county and state—United States, 2018–2019 [Data tables]. U.S. Department of Health and Human Services. https://www.cdc.gov/breastfeeding-data/county-initiation/index.html
———. (2024b). NIS-Child data analysis: Breastfeeding initiation, duration & exclusivity. U.S. Department of Health & Human Services. https://www.cdc.gov/breastfeeding-data/survey/analysis.html
———. (2025a). Breastfeeding initiation rates. https://www.cdc.gov/breastfeeding-data/county-initiation/index.html
———. (2025b). NIS-Child data results: Breastfeeding among U.S. children born 2014-2021, percentage breastfed by birth year. https://www.cdc.gov/breastfeeding-data/survey/results.html
Cerceo, E., Saxer, K., Grossman, L., Shapley-Quinn, K., & Feldman-Winter, L. (2024). The climate crisis and breastfeeding: Opportunities for resilience. Journal of Human Lactation, 40(1), 33–50. https://doi.org/10.1177/08903344231216726
Chapman, D. J., & Pérez-Escamilla, R. (1999). Identification of risk factors for delayed onset of lactation. Journal of the American Dietetic Association, 99(4), 450–456. https://doi.org/10.1016/S0002-8223(99)00109-1
———. (2012). Breastfeeding among minority women: Moving from risk factors to interventions. Advances in Nutrition, 3(1), 95–104. https://doi.org/10.3945/an.111.001016
Chatterji, P., & Frick, K. D. (2005). Does returning to work after childbirth affect breastfeeding practices? Review of Economics of the Household, 3(3), 315–335. https://doi.org/10.1007/s11150-005-3460-4
Chawla, N., Gabriel, A. S., Prengler, M., Rogers, K., Rogers, B., Tedder-King, A., & Rosen, C. C. (2024). Allyship in the fifth trimester: A multi-method investigation of women’s postpartum return to work. Organizational Behavior and Human Decision Processes, 182, 104330. https://doi.org/10.1016/j.obhdp.2024.104330
Chehayeb, R. J., Odzer, N., Albany, R. A., Ferrucci, L., Sarpong, D., Perez-Escamilla, R., Lewis, J. B., Phipps, A. I., Meisner, A., & Pusztai, L. (2025). Breastfeeding attributable fraction of triple negative breast cancer in the US. NPJ Breast Cancer, 11(1), 40. https://doi.org/10.1038/s41523-025-00755-6
Chen, C.-N., Yu, H.-C., & Chou, A.-K. (2020). Association between maternal pre-pregnancy body mass index and breastfeeding duration in Taiwan: A population-based cohort study. Nutrients, 12(8), 2361. https://doi.org/10.3390/nu12082361
Cheng, R. J., Fisher, A. C., & Nicholson, S. C. (2022). Interest in home birth during the COVID-19 pandemic: Analysis of Google Trends data. Journal of Midwifery & Women’s Health, 67(4), 427–434. https://doi.org/10.1111/jmwh.13341
Cheng, T. L., Johnson, S. B., & Goodman, E. (2016). Breaking the intergenerational cycle of disadvantage: The three generation approach. Pediatrics, 137(6), e20152467. https://doi.org/10.1542/peds.2015-2467
Chiang, K. V., Li, R., Anstey, E. H., & Perrine, C. G. (2021). Racial and Ethnic Disparities in Breastfeeding Initiation—United States, 2019. Morbidity and Mortality Weekly Report, 70(21), 769–774. https://www.cdc.gov/mmwr/volumes/70/wr/mm7021a1.htm
Cochrane Collaboration. (2025). GRADE. https://www.cochrane.org/learn/courses-and-resources/cochrane-methodology/grade
Cole, J. C. M., Schwarz, J., Farmer, M. C., Coursey, A. L., Duren, S., Rowlson, M., Prince, J., Oser, M., & Spatz, D. L. (2018). Facilitating milk donation in the context of perinatal palliative care. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 47(4), 564–570. https://doi.org/10.1016/j.jogn.2017.11.002
Committee on Fetus and Newborn. (2010). Hospital stay for healthy term newborns [Policy statement]. Pediatrics, 125(2), 405–409. https://doi.org/10.1542/peds.2009-3119
Cruz, N. I., & Korchin, L. (2007). Lactational performance after breast reduction with different pedicles. Plastic and Reconstructive Surgery, 120(1), 35–40. https://doi.org/10.1097/01.prs.0000263371.37596.49
———. (2010). Breastfeeding after augmentation mammaplasty with saline implants. Annals of Plastic Surgery, 64(5), 530–533. https://doi.org/10.1097/SAP.0b013e3181c925e4
Del Ciampo, L. A., & Del Ciampo, I. R. L. (2018). Breastfeeding and the benefits of lactation for women’s health. Revista Brasileira de Ginecologia E Obstetricia 40(6), 354–359. https://doi.org/10.1055/s-0038-1657766
Dewey, K. G., Güngör, D., Donovan, S. M., Madan, E. M., Venkatramanan, S., Davis, T. A., Kleinman, R. E., Taveras, E. M., Bailey, R. L., Novotny, R., Terry, N., Butera, G., Obbagy, J., de Jesus, J., & Stoody, E. (2021). Breastfeeding and risk of overweight in childhood and beyond: A systematic review with emphasis on sibling-pair and intervention studies. The American Journal of Clinical Nutrition, 114(5), 1774–1790. https://doi.org/10.1093/ajcn/nqab206
Dewey, K. G., Nommsen-Rivers, L. A., Heinig, M. J., & Cohen, R. J. (2003). Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics, 112(3 Pt 1), 607–619. https://doi.org/10.1542/peds.112.3.607
Diaz, L. E., Yee, L. M., & Feinglass, J. (2023). Rates of breastfeeding initiation and duration in the United States: Data insights from the 2016–2019 Pregnancy Risk Assessment Monitoring System. Frontiers in Public Health, 11, 1256432. https://doi.org/10.3389/fpubh.2023.1256432
DiGirolamo, A. M., Grummer-Strawn, L. M., & Fein, S. B. (2008). Effect of maternity-care practices on breastfeeding. Pediatrics, 122(Suppl 2), S43–S49. https://doi.org/10.1542/peds.2008-1315e
Dugat, V. M., Chertok, I. R. A., & Haile, Z. T. (2019). Association between stressful life events and exclusive breastfeeding among mothers in the United States. Breastfeeding Medicine, 14(7), 475–481. https://doi.org/10.1089/bfm.2019.0058
Dutheil, F., Méchin, G., Vorilhon, P., Benson, A. C., Bottet, A., Clinchamps, M., Barasinski, C., & Navel, V. (2021). Breastfeeding after returning to work: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 18(16), 8631. https://doi.org/10.3390/ijerph18168631
Eagen-Torkko, M., Low, L. K., Zielinski, R., & Seng, J. S. (2017). Prevalence and predictors of breastfeeding after childhood abuse. Journal of Obstetric, Gynecologic & Neonatal Nursing, 46(3), 465–479. https://doi.org/10.1016/j.jogn.2017.01.002
European Standards of Care for Newborn Health. (2019). Standards. https://newborn-health-standards.org/standards/
Fauzia, F., Ekayanthi, N. W. D., & Fudholi, A. (2020). The influence of participative counseling approach on improving breastfeeding self-efficacy among pregnant women in Indonesia. Asian Journal of Pharmaceutical and Clinical Research, 13(1), 85–88. https://doi.org/10.22159/ajpcr.2020.v13i1.36167
Feldman-Winter, L., Goldsmith, J. P., Committee on Fetus and Newborn, & Task Force on Sudden Infant Death Syndrome (2016). Safe sleep and skin-to-skin care in the neonatal period for healthy term newborns. Pediatrics, 138(3), e20161889. https://doi.org/10.1542/peds.2016-1889
Feldman-Winter, L., Kellams, A., Peter-Wohl, S., Taylor, J. S., Lee, K. G., Terrell, M. J., Noble, L., Maynor, A. R., Meek, J. Y., & Stuebe, A. M. (2020). Evidence-based updates on the first week of exclusive breastfeeding among infants ≥35 Weeks. Pediatrics, 145(4), e20183696. https://doi.org/10.1542/peds.2018-3696
Feltner, C., Weber, R. P., Stuebe, A., Grodensky, C. A., Orr, C., & Viswanathan, M. (2018). Breastfeeding programs and policies, breastfeeding uptake, and maternal health outcomes in developed countries. Agency for Healthcare Research and Quality. https://doi.org/10.23970/AHRQEPCCER210
Ferri, R. L., Rosen-Carole, C. B., Jackson, J., Carreno-Rijo, E., Greenberg, K. B., & Academy of Breastfeeding Medicine. (2020). ABM Clinical Protocol #33: Lactation care for lesbian, gay, bisexual, transgender, queer, questioning, plus patients. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 15(5), 284–293. https://doi.org/10.1089/bfm.2020.29152.rlf
Field, C., Grobman, W. A., Wu, J., Palatnik, A., Landon, M. B., Scholtens, D., Lowe, W., Shah, N. S., Josefson, J., Khan, S., & Venkatesh, K. K. (2025). Association between breastfeeding and long-term risk of cardiovascular disease. Obstetrics and Gynecology, 146(1), 11–18. https://doi.org/10.1097/AOG.0000000000005943
Fitzsimons, E., & Vera-Hernández, M. (2022). Breastfeeding and child development. American Economic Journal: Applied Economics, 14(3), 329–366. https://doi.org/10.1257/app.20180385
Flacking, R., Lehtonen, L., Thomson, G., Axelin, A., Ahlqvist, S., Moran, V. H., Ewald, U., Dykes, F., & Separation and Closeness Experiences in the Neonatal Environment (SCENE) group. (2012). Closeness and separation in neonatal intensive care. Acta Paediatrica, 101(10), 1032–1037. https://doi.org/10.1111/j.1651-2227.2012.02787.x
Flaherman, V. J., Schaefer, E. W., Kuzniewicz, M. W., Li, S. X., Walsh, E. M., & Paul, I. M. (2015). Early weight loss nomograms for exclusively breastfed newborns. Pediatrics, 135(1), e16–e23. https://doi.org/10.1542/peds.2014-1532
Flidel-Rimon, O., & Shinwell, E. S. (2006). Breast feeding twins and high multiples. Archives of Disease in Childhood. Fetal and Neonatal Edition, 91(5), F377-380. https://doi.org/10.1136/adc.2005.082305
Frederick, A., Fry, T., & Clowtis, L. (2020). Intraoperative mother and baby skin-to-skin contact during cesarean birth: Systematic review. The American Journal of Maternal Child Nursing, 45(5), 296–305. https://doi.org/10.1097/NMC.0000000000000646
Furman, L., Minich, N., & Hack, M. (2002). Correlates of lactation in mothers of very low birth weight infants. Pediatrics, 109(4), e57–e57. https://doi.org/10.1542/peds.109.4.e57
Gabriel, A. S., Ladge, J. J., Little, L. M., MacGowan, R. L., & Stillwell, E. E. (2023). Sense-making through the storm: How postpartum depression shapes personal work–family narratives. Journal of Applied Psychology, 108(12), 1903–1923. https://doi.org/10.1037/apl0001125
Gabriel, A. S., Volpone, S. D., MacGowan, R. L., Butts, M. M., & Moran, C. M. (2020). When work and family blend together: Examining the daily experiences of breastfeeding mothers at work. Academy of Management Journal, 63(5), 1337–1369. https://doi.org/10.5465/amj.2017.1241
Galipeau, R., Baillot, A., Trottier, A., & Lemire, L. (2018). Effectiveness of interventions on breastfeeding self-efficacy and perceived insufficient milk supply: A systematic review and meta-analysis. Maternal & Child Nutrition, 14(3), e12607. https://doi.org/10.1111/mcn.12607
Garcia, A. H., Voortman, T., Baena, Cristina. P., Chowdhurry, R., Muka, T., Jaspers, L., Warnakula, S., Tielemans, M. J., Troup, J., Bramer, W. M., Franco, O. H., & Van Den Hooven, E. H. (2016). Maternal weight status, diet, and supplement use as determinants of breastfeeding and complementary feeding: A systematic review and meta-analysis. Nutrition Reviews, 74(8), 490–516. https://doi.org/10.1093/nutrit/nuw016
Geddes, D. T., Gridneva, Z., Perrella, S. L., Mitoulas, L. R., Kent, J. C., Stinson, L. F., Lai, C. T., Sakalidis, V., Twigger, A.-J., & Hartmann, P. E. (2021). 25 Years of research in human lactation: From discovery to translation. Nutrients, 13(9), 3071. https://doi.org/10.3390/nu13093071
Gizzo, S., Di Gangi, S., Saccardi, C., Patrelli, T. S., Paccagnella, G., Sansone, L., Barbara, F., D’Antona, D., & Nardelli, G. B. (2012). Epidural analgesia during labor: Impact on delivery outcome, neonatal well-being, and early breastfeeding. Breastfeeding Medicine, 7, 262–268. https://doi.org/10.1089/bfm.2011.0099
Goldshtein, I., Sadaka, Y., Amit, G., Kasir, N., Bourgeron, T., Warrier, V., Akiva, P., Avgil Tsadok, M., & Zimmerman, D. R. (2025). Breastfeeding duration and child development. JAMA Network Open, 8(3), e251540. https://doi.org/10.1001/jamanetworkopen.2025.1540
Grajeda, R., & Pérez-Escamilla, R. (2002). Stress during labor and delivery is associated with delayed onset of lactation among urban Guatemalan women. The Journal of Nutrition, 132(10), 3055–3060. https://doi.org/10.1093/jn/131.10.3055
Gregory, E. C. W., Osterman, M. J. K., & Valenzuela, C. P. (2021). Changes in home births by race and hispanic origin and state of residence of mother: United States, 2018–2019 and 2019–2020. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 70(15), 1–10.
Griswold, M. K., Crawford, S. L., Perry, D. J., Person, S. D., Rosenberg, L., Cozier, Y. C., & Palmer, J. R. (2018). Experiences of racism and breastfeeding initiation and duration among first-time mothers of the Black Women’s Health Study. Journal of Racial and Ethnic Health Disparities, 5(6), 1180–1191. https://doi.org/10.1007/s40615-018-0465-2
Güngör, D., Nadaud, P., Dreibelbis, C., LaPergola, C. C., Wong, Y. P., Terry, N., Abrams, S. A., Beker, L., Jacobovits, T., Järvinen, K. M., Nommsen-Rivers, L. A., O’Brien, K. O., Oken, E., Pérez-Escamilla, R., Ziegler, E. E., & Spahn, J. M. (2019a). Infant milk-feeding practices and childhood leukemia: A systematic review. The American Journal of Clinical Nutrition, 109, 757S–771S. https://doi.org/10.1093/ajcn/nqy306
———. (2019b). Infant milk-feeding practices and cardiovascular disease outcomes in offspring: A systematic review. The American Journal of Clinical Nutrition, 109, 800S–816S. https://doi.org/10.1093/ajcn/nqy332
———. (2019c). Infant milk-feeding practices and diabetes outcomes in offspring: A systematic review. The American Journal of Clinical Nutrition, 109, 817S-837S. https://doi.org/10.1093/ajcn/nqy311
———. (2019d). Infant milk-feeding practices and food allergies, allergic rhinitis, atopic dermatitis, and asthma throughout the life span: A systematic review. The American Journal of Clinical Nutrition, 109, 772S–799S. https://doi.org/10.1093/ajcn/nqy283
Halfon, N., & Hochstein, M. (2002). Life course health development: An integrated framework for developing health, policy, and research. The Milbank Quarterly, 80(3), 433–479. https://doi.org/10.1111/1468-0009.00019
Hamilton, L. J., & Middlestadt, S. (2024). Beliefs about donating human milk to a milk bank: A theory-based salient belief elicitation. Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 40(4), 582–592. https://doi.org/10.1177/08903344241274348
Hanson, M. A., & Gluckman, P. D. (2014). Early developmental conditioning of later health and disease: Physiology or pathophysiology? Physiological Reviews, 94(4), 1027–1076. https://doi.org/10.1152/physrev.00029.2013
Hantsoo, L., Jagodnik, K. M., Novick, A. M., Baweja, R., di Scalea, T. L., Ozerdem, A., McGlade, E. C., Simeonova, D. I., Dekel, S., Kornfield, S. L., Nazareth, M., & Weiss, S. J. (2023). The role of the hypothalamic-pituitary-adrenal axis in depression across the female reproductive lifecycle: Current knowledge and future directions. Frontiers in Endocrinology, 14, 1295261. https://doi.org/10.3389/fendo.2023.1295261
Harris, M., Schiff, D. M., Saia, K., Muftu, S., Standish, K. R., & Wachman, E. M. (2023). Academy of breastfeeding medicine clinical protocol #21: Breastfeeding in the setting of substance use and substance use disorder (Revised 2023). Breastfeeding Medicine, 18(10), 715–733. https://doi.org/10.1089/bfm.2023.29256.abm
Hartman, S., Barnett, J., & Bonuck, K. A. (2012). Implementing international board-certified lactation consultants intervention into routine care: Barriers and recommendations. Clinical Lactation, 3(4), 131–137. https://doi.org/10.1891/215805312807003799
Health Resources and Services Administration. (2025). Women’s preventive services guidelines. https://www.hrsa.gov/womens-guidelines
Heck, J. L. (2021). Postpartum depression in American Indian/Alaska Native women. The American Journal of Maternal/Child Nursing, 46(1), 6–13. https://doi.org/10.1097/NMC.0000000000000671
Hill, P. D., Aldag, J. C., Chatterton, R. T., & Zinaman, M. (2005). Comparison of milk output between mothers of preterm and term infants: The first 6 weeks after birth. Journal of Human Lactation, 21, 22–30. https://doi.org/10.1177/0890334404272407
Hinton, L., Locock, L., & Knight, M. (2015). Maternal critical care: What can we learn from patient experience? A qualitative study. BMJ Open, 5(4), e006676. https://doi.org/10.1136/bmjopen-2014-006676
Hoban, R., Patel, A. L., Medina Poeliniz, C., Lai, C. T., Janes, J., Geddes, D., & Meier, P. P. (2018). Human milk biomarkers of secretory activation in breast pump-dependent mothers of premature infants. Breastfeeding Medicine, 13(5), 352–360. https://doi.org/10.1089/bfm.2017.0183
Hobbs, A. J., Mannion, C. A., McDonald, S. W., Brockway, M., & Tough, S. C. (2016). The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy and Childbirth, 16(1), 90. https://doi.org/10.1186/s12884-016-0876-1
Hodnett, E. D., Gates, S., Hofmeyr, G. J., & Sakala, C. (2013). Continuous support for women during childbirth. Cochrane Database of Systematic Reviews, (5), Article CD003766. https://doi.org/10.1002/14651858.CD003766.pub5
Holmes, A. V., McLeod, A. Y., & Bunik, M. (2013). ABM Clinical Protocol #5: Peripartum breastfeeding management for the healthy mother and infant at term, revision 2013. Breastfeeding Medicine, 8(6), 469–473. https://doi.org/10.1089/bfm.2013.9979
Hookway, L., Lewis, J., & Brown, A. (2021). The challenges of medically complex breastfed children and their families: A systematic review. Maternal & Child Nutrition, 17(4), e13182. https://doi.org/10.1111/mcn.13182
Horta, B. L., Loret de Mola, C., & Victora, C. G. (2015). Breastfeeding and intelligence: A systematic review and meta-analysis. Acta Paediatrica, 104(467), 14–19. https://doi.org/10.1111/apa.13139
Horta, B. L., Rollins, N., Dias, M. S., Garcez, V., & Pérez-Escamilla, R. (2023). Systematic review and meta-analysis of breastfeeding and later overweight or obesity expands on previous study for World Health Organization. Acta Paediatrica, 112(1), 34–41. https://doi.org/10.1111/apa.16460
Howell, E. A. (2018). Reducing disparities in severe maternal morbidity and mortality. Clinical Obstetrics & Gynecology, 61(2), 387–399. https://doi.org/10.1097/GRF.0000000000000349
Hoyt-Austin, A. E., Kair, L. R., Larson, I. A., Stehel, E. K., & Academy of Breastfeeding Medicine. (2022). Academy of Breastfeeding Medicine Clinical Protocol #2: Guidelines for birth hospitalization discharge of breastfeeding dyads, revised 2022. Breastfeeding Medicine, 17(3), 197–206. https://doi.org/10.1089/bfm.2022.29203.aeh
Huang, L., Xu, S., Chen, X., Li, Q., Lin, L., Zhang, Y., Gao, D., Wang, H., Hong, M., Yang, X., Hao, L., & Yang, N. (2020). Delayed lactogenesis is associated with suboptimal breastfeeding practices: A prospective cohort study. The Journal of Nutrition, 150(4), 894–900. https://doi.org/10.1093/jn/nxz311
Human Milk Banking Association of North America. (2025, February 6). Milk banking news. https://www.hmbana.org/news/blog.html/article/2025/02/06/nonprofit-milk-banks-dispense-record-11-million-ounces-of-donor-milk-in-2024-a-10-increase-reflects-growing-demand-for-life-saving-nutrition-for-medically-fragile-infants
Hung, K. J., & Berg, O. (2011). Early skin-to-skin after cesarean to improve breastfeeding. The American Journal of Maternal Child Nursing, 36(5), 318–326. https://doi.org/10.1097/NMC.0b013e3182266314
Institute of Medicine. (1991). Nutrition during lactation. National Academies Press. https://doi.org/10.17226/1577
Ip, S., Chung, M., Raman, G., Chew, P., Magula, N., DeVine, D., Trikalinos, T., & Lau, J. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evidence Report/Technology Assessment, 153, 1–186.
Jack, A., Mullin, C., Brown, E., Burtner, M., Standish, K. R., Fields, A., Rosen-Carole, C., & Hartman, S. (2024). Academy of breastfeeding medicine clinical protocol #19: Breastfeeding promotion in the prenatal period (Revised 2024). Breastfeeding Medicine, 19(8), 575–587. https://doi.org/10.1089/bfm.2024.0203
Jegier, B. J., Smith, J. P., & Bartick, M. C. (2024). The economic cost consequences of suboptimal infant and young child feeding practices: A scoping review. Health Policy and Planning, 39(9), 916–945. https://doi.org/10.1093/heapol/czae069
Johnson, A., Kirk, R., Rosenblum, K. L., & Muzik, M. (2015). Enhancing breastfeeding rates among African American women: A systematic review of current psychosocial interventions. Breastfeeding Medicine, 10(1), 45–62. https://doi.org/10.1089/bfm.2014.0023
Jordan, S., Emery, S., Watkins, A., Evans, J. D., Storey, M., & Morgan, G. (2009). Associations of drugs routinely given in labour with breastfeeding at 48 hours: Analysis of the Cardiff Births Survey. BJOG: An International Journal of Obstetrics and Gynaecology, 116(12), 1622–1632. https://doi.org/10.1111/j.1471-0528.2009.02256.x
Juntereal, N. A. (2024). Measuring human milk biomarkers at point-of-care: An emerging opportunity for nurses. The American Journal of Maternal/Child Nursing, 49(2), 116–117. https://doi.org/10.1097/NMC.0000000000000993
Kehinde, J., O’Donnell, C., & Grealish, A. (2023). The effectiveness of prenatal breastfeeding education on breastfeeding uptake postpartum: A systematic review. Midwifery, 118, 103579. https://doi.org/10.1016/j.midw.2022.103579
Khatib, M. N., Gaidhane, A., Upadhyay, S., Telrandhe, S., Saxena, D., Simkhada, P. P., Sawleshwarkar, S., & Quazi, S. Z. (2023). Interventions for promoting and optimizing breastfeeding practices: An overview of systematic review. Frontiers in Public Health, 11, 984876. https://doi.org/10.3389/fpubh.2023.984876
Kioumourtzoglou, M.-A., Coull, B. A., O’Reilly, É. J., Ascherio, A., & Weisskopf, M. G. (2018). Association of exposure to diethylstilbestrol during pregnancy with multigenerational neurodevelopmental deficits. JAMA Pediatrics, 172(7), 670. https://doi.org/10.1001/jamapediatrics.2018.0727
Kitsantas, P., Gaffney, K. F., Nirmalraj, L., & Sari, M. (2019). The influence of maternal life stressors on breastfeeding outcomes: A US population-based study. The Journal of Maternal-Fetal & Neonatal Medicine, 32(11), 1869–1873. https://doi.org/10.1080/14767058.2017.1421929
Kozhimannil, K. B., Attanasio, L. B., Hardeman, R. R., & O’Brien, M. (2013). Doula care supports near-universal breastfeeding initiation among diverse, low-income women. Journal of Midwifery & Women’s Health, 58(4), 378–382. https://doi.org/10.1111/jmwh.12065
La Leche League. (2020). Thinking about nursing your toddler? https://lllusa.org/toddler-nursing/
Labarere, J., Gelbert-Baudino, N., Ayral, A. S., Duc, C., Berchotteau, M., Bouchon, N., Schelstraete, C., Vittoz, J. P., Francois, P., & Pons, J. C. (2005). Efficacy of breastfeeding support provided by trained clinicians during an early, routine, preventive visit: A prospective, randomized, open trial of 226 mother-infant pairs. Pediatrics, 115(2), e139–e146. https://doi.org/10.1542/peds.2004-1362
Ladge, J. J., & Little, L. M. (2019). When expectations become reality: Work–family image management and identity adaptation. Academy of Management Review, 44(1), 126–149. https://doi.org/10.5465/amr.2016.0438
Laughlin, L. (2013). Who’s minding the kids? Child care arrangements: Spring 2011 (Current Population Reports No. P70-135). U.S. Census Bureau. https://www.census.gov/prod/2013pubs/p70-135.pdf
Lawrence, R. A., & Lawrence, R. M. (2021). Breastfeeding: A guide for the medical profession (9th ed.). Elsevier Health Sciences.
Little, L. M., & Masterson, C. R. (2023). Mother’s reentry: A relative contribution perspective of dual-earner parents’ roles, resources, and outcomes. Academy of Management Journal, 66(6), 1741–1767. https://doi.org/10.5465/amj.2019.1344
Litwan, K., Tran, V., Nyhan, K., et al. (2021). How do breastfeeding workplace interventions work?: A realist review. International Journal for Equity in Health, 20, 148. https://doi.org/10.1186/s12939-021-01490-7
Lockyer, F., McCann, S., & Moore, S. E. (2021). Breast milk micronutrients and infant neurodevelopmental outcomes: A systematic review. Nutrients, 13(11), 3848. https://doi.org/10.3390/nu13113848
Louis-Jacques, A. F., & Stuebe, A. M. (2020). Enabling breastfeeding to support lifelong health for mother and child. Obstetrics and Gynecology Clinics of North America, 47(3), 363–381. https://doi.org/10.1016/j.ogc.2020.04.001
Lowenfels, A., Murphy, M., Archibald, A., Avellino, S., & Potestio, K. (2024). Implementing policy and practice changes to support breastfeeding duration in New York state communities. Preventing Chronic Disease, 21, 240003. https://doi.org/10.5888/pcd21.240003
Lynch, J., & Smith, G. D. (2005). A life course approach to chronic disease epidemiology. Annual Review of Public Health, 26, 1–35. https://doi.org/10.1146/annurev.publhealth.26.021304.144505
MacDorman, M. F., & Declercq, E. (2019). Trends and state variations in out-of-hospital births in the United States, 2004–2017. Birth, 46(2), 279–288. https://doi.org/10.1111/birt.12411
Mago-Shah, D. D., Athavale, K., Fisher, K., Heyward, E., Tanaka, D., & Cotten, C. M. (2023). Early pumping frequency and coming to volume for mother’s own milk feeding in hospitalized infants. Journal of Perinatology: Official Journal of the California Perinatal Association, 43(5), 629–634. https://doi.org/10.1038/s41372-023-01662-z
Mahmood, I., Jamal, M., & Khan, N. (2011). Effect of mother-infant early skin-to-skin contact on breastfeeding status: A randomized controlled trial. Journal of the College of Physicians and Surgeons—Pakistan, 21(10), 601–605. https://doi.org/10.2011/JCPSP.601605
Malik, R., Hamm, K., Schochet, L., Novoa, C., Workman, S., & Jessen-Howard, S. (2018). America’s child care deserts in 2018. Center for American Progress. https://www.americanprogress.org/article/americas-child-care-deserts-2018/
Marino, J. A., Meraz, K., Dhaliwal, M., Payán, D. D., Wright, T., & Hahn-Holbrook, J. (2023). Impact of the COVID-19 pandemic on infant feeding practices in the United States: Food insecurity, supply shortages, and deleterious formula-feeding practices. Maternal & Child Nutrition. https://doi.org/10.1111/mcn.13498
Marks, K. J., Nakayama, J. Y., Chiang, K. V., Grap, M. E., Anstey, E. H., Boundy, E. O., Hamner, H. C., & Li, R. (2023). Disaggregation of Breastfeeding Initiation Rates by Race and Ethnicity—United States, 2020–2021. Preventing Chronic Disease, 20, 230199. https://doi.org/10.5888/pcd20.230199
Martin, J. A., & Osterman, M. J. K. (2025). Increases in neonatal intensive care admissions in the United States, 2016–2023 (NCHS Data Brief No. 525). National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db525.htm
Martin-de-las-Heras, S., Velasco, C., Luna-del-Castillo, J., & Khan, K. (2019). Breastfeeding avoidance following psychological intimate partner violence during pregnancy: A cohort study and multivariate analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 126(6), 778–783. https://doi.org/10.1111/1471-0528.15592
Martino, J., & Spatz, D. (2014). Human milk banking in North America: A paradigm shift. Journal of Human Lactation, 30(3), 315–319. https://doi.org/10.1177/0890334414525994
McCoy, M. B., & Heggie, P. (2020). In-hospital formula feeding and breastfeeding duration. Pediatrics, 146(1), e20192946. https://doi.org/10.1542/peds.2019-2946
McNally, D., & Spatz, D. L. (2020). Mothers who engage in long-term informal milk sharing. The American Journal of Maternal/Child Nursing, 45(6), 338–343. https://doi.org/10.1097/NMC.0000000000000660
Meek, J. Y., Feldman-Winter, L., & Noble, L. (2020). Optimal duration of breastfeeding. Pediatrics, 146(5), e2020021063. https://doi.org/10.1542/peds.2020-021063
Meek, J. Y., Noble, L., & Section on Breastfeeding. (2022). Policy statement: Breastfeeding and the use of human milk. Pediatrics, 150(1), e2022057988. https://doi.org/10.1542/peds.2022-057988
Meier, P. P., Johnson, T. J., Patel, A. L., & Rossman, B. (2017). Evidence-based methods that promote human milk feeding of preterm infants. Clinics in Perinatology, 44(1), 1–22. https://doi.org/10.1016/j.clp.2016.11.005
Metallinos-Katsaras, E., Brown, L., & Colchamiro, R. (2015). Maternal WIC participation improves breastfeeding rates: A statewide analysis of WIC participants. Maternal and child health journal, 19(1), 136–143. https://doi.org/10.1007/s10995-014-1504-1
Mikiel-Kostyra, K., Mazur, J., & Bołtruszko, I. (2002). Effect of early skin-to-skin contact after delivery on duration of breastfeeding: A prospective cohort study. Acta Paediatrica, 91(12), 1301–1306. https://doi.org/10.1080/08035250216102
Miller, J., Tonkin, E., Damarell, R. A., McPhee, A. J., Suganuma, M., Suganuma, H., Middleton, P. F., Makrides, M., & Collins, C. T. (2018). A systematic review and meta-analysis of human milk feeding and morbidity in very low birth weight infants. Nutrients, 10(6), 707. https://doi.org/10.3390/nu10060707
Miller-Graff, L. E., Ahmed, A. H., & Paulson, J. L. (2018). Intimate partner violence and breastfeeding outcomes in a sample of low-income women. Journal of Human Lactation, 34(3), 494–502. https://doi.org/10.1177/0890334418776217
Mitanchez, D., Yzydorczyk, C., Siddeek, B., Boubred, F., Benahmed, M., & Simeoni, U. (2015). The offspring of the diabetic mother—Short- and long-term implications. Best Practice & Research. Clinical Obstetrics & Gynaecology, 29(2), 256–269. https://doi.org/10.1016/j.bpobgyn.2014.08.004
Mizrak, B., Ozerdogan, N., & Colak, E. (2017). The effect of antenatal education on breastfeeding self-efficacy: Primiparous women in Turkey. International Journal of Caring Sciences, 10, 503–510.
Modi, D., Dholakia, N., Gopalan, R., Venkatraman, S., Dave, K., Shah, S., Desai, G., Qazi, S. A., Sinha, A., Pandey, R. M., Anand, A., Desai, S., & Shah, P. (2019). mHealth
intervention “ImTeCHO” to improve delivery of maternal, neonatal, and child care services—A cluster-randomized trial in tribal areas of Gujarat, India. PLoS Medicine, 16(10), e1002939. https://doi.org/10.1371/journal.pmed.1002939
Montgomery, A., Hale, T. W., Marinelli, K. A., Bunik, M., Noble, L., Brent, N., Grawey, A. E., Holmes, A. V., Lawrence, R. A., Powers, N. G., Seo, T., & Taylor, J. S. (2012). ABM clinical protocol #15: Analgesia and anesthesia for the breastfeeding mother, revised 2012. Breastfeeding Medicine, 7(6), 547–553. https://doi.org/10.1089/bfm.2012.9977
Moore, E. R., Bergman, N., Anderson, G. C., & Medley, N. (2016). Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews, 11. https://doi.org/10.1002/14651858.CD003519.pub4
Mottl-Santiago, J., Walker, C., Ewan, J., Vragovic, O., Winder, S., & Stubblefield, P. (2008). A hospital-based doula program and childbirth outcomes in an urban, multicultural setting. Maternal and Child Health Journal, 12(3), 372–377. https://doi.org/10.1007/s10995-007-0245-9
Murray, E. K., Ricketts, S., & Dellaport, J. (2007). Hospital practices that increase breastfeeding duration: Results from a population-based study. Birth, 34(3), 202–211. https://doi.org/10.1111/j.1523-536X.2007.00172.x
National Academies of Sciences, Engineering, and Medicine (National Academies). (2019). Vibrant and healthy kids: Aligning science, practice, and policy to advance health equity. National Academies Press. https://doi.org/10.17226/25466
———. (2020). Birth settings in America: Outcomes, quality, access, and choice. National Academies Press. https://doi.org/10.17226/25636
———. (2024). Launching lifelong health by improving health care for children, youth, and families. National Academies Press. https://doi.org/10.17226/27835
National Center for Health Statistics. (2025). Births—Method of delivery. https://www.cdc.gov/nchs/fastats/delivery.htm
Neifert, M. R., Seacat, J. M., & Jobe, W. E. (1985). Lactation failure due to insufficient glandular development of the breast. Pediatrics, 76(5), 823–828.
Noble, L. M., Okogbule-Wonodi, A. C., & Young, M. A. (2018). ABM Clinical Protocol #12: Transitioning the breastfeeding preterm infant from the neonatal intensive care unit to home, revised 2018. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 13(4), 230–236. https://doi.org/10.1089/bfm.2018.29090.ljn
Nommsen-Rivers, L. A., Mastergeorge, A. M., Hansen, R. L., Cullum, A. S., & Dewey, K. G. (2009). Doula care, early breastfeeding outcomes, and breastfeeding status at 6 weeks postpartum among low-income primiparae. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 38(2), 157–173. https://doi.org/10.1111/j.1552-6909.2009.01005.x
Nommsen-Rivers, L. A., Wagner, E. A., Roznowski, D. M., Riddle, S. W., Ward, L. P., & Thompson, A. (2022). Measures of maternal metabolic health as predictors of severely low milk production. Breastfeeding Medicine, 17(7), 566–576. https://doi.org/10.1089/bfm.2021.0292
Obbagy, J. E., Spahn, J. M., Wong, Y. P., Psota, T. L., Spill, M. K., Dreibelbis, C., Gungor, D. E., Nadaud, P., Raghavan, R., Callahan, E. H., English, L. K., Kingshipp, B. L., LaPergola, C. C., Shapiro, M. J., & Stoody, E. E. (2019). Systematic review methods for the Pregnancy and Birth to 24 Months Project. The American Journal of Clinical Nutrition, 109, 698S–704S. https://doi.org/10.1093/ajcn/nqy226
Odom, E. C., Li, R., Scanlon, K. S., Perrine, C. G., & Grummer-Strawn, L. (2013). Reasons for earlier than desired cessation of breastfeeding. Pediatrics, 131(3), e726-732. https://doi.org/10.1542/peds.2012-1295
Office of the Surgeon General, Centers for Disease Control and Prevention, & Office on Women’s Health. (2011). The Surgeon General’s call to action to support breastfeeding. Office of the Surgeon General. https://www.ncbi.nlm.nih.gov/books/NBK52691/
Olff, M., Frijling, J. L., Kubzansky, L. D., Bradley, B., Ellenbogen, M. A., Cardoso, C., Bartz, J. A., Yee, J. R., & van Zuiden, M. (2013). The role of oxytocin in social bonding, stress regulation and mental health: An update on the moderating effects of context and interindividual differences. Psychoneuroendocrinology, 38(9), 1883–1894. https://doi.org/10.1016/j.psyneuen.2013.06.019
Olufunlayo, T. F., Roberts, A. A., MacArthur, C., Thomas, N., Odeyemi, K. A., Price, M., & Jolly, K. (2019). Improving exclusive breastfeeding in low and middle-income countries: A systematic review. Maternal & Child Nutrition, 15(3), e12788. https://doi.org/10.1111/mcn.12788
Öztürk, R., Ergün, S., & Özyazıcıoğlu, N. (2022). Effect of antenatal educational intervention on maternal breastfeeding self-efficacy and breastfeeding success: A quasi-experimental study. Revista Da Escola de Enfermagem Da USP, 56, e20210428. https://doi.org/10.1590/1980-220x-reeusp-2021-0428
Pathirana, M. M., Ali, A., Lassi, Z. S., Arstall, M. A., Roberts, C. T., & Andraweera, P. H. (2022). Protective influence of breastfeeding on cardiovascular risk factors in women with previous gestational diabetes mellitus and their children: A systematic review and meta-analysis. Journal of Human Lactation, 38(3), 501–512. https://doi.org/10.1177/08903344211034779
Parasuraman, S., Lebrun-Harris, L., & Jones, J. (2020). Breastfeeding initiation, duration, and exclusivity among WIC-eligible populations. Health Services Research, 55(Suppl 1), 30–31. https://doi.org/10.1111/1475-6773.13366
Paraszczuk, A. M., Candelaria, L. M., Hylton-McGuire, K., & Spatz, D. L. (2022). The voice of mothers who continue to express milk after their infant’s death for donation to a milk bank. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 17(8), 660–665. https://doi.org/10.1089/bfm.2021.0326
Parker, M. G., Stellwagen, L. M., Noble, L., Kim, J. H., Poindexter, B. B., Puopolo, K. M., & Section on Breastfeeding, Committee on Nutrition, Committee on Fetus and Newborn. (2021). Promoting human milk and breastfeeding for the very low birth weight infant. Pediatrics, 148(5), e2021054272. https://doi.org/10.1542/peds.2021-054272
Patnode, C. D., Henninger, M. L., Senger, C. A., Perdue, L. A., & Whitlock, E. P. (2016). Primary care interventions to support breastfeeding: Updated evidence report and systematic review for the US preventive services task force. JAMA, 316(16), 1694–1705. https://doi.org/10.1001/jama.2016.8882
Patnode, C. D., Henrikson, N. B., Webber, E. M., Blasi, P. R., Senger, C. A., & Guirguis-Blake, J. M. (2025). Breastfeeding and health outcomes for infants and children: A systematic review. Pediatrics, 156(1). https://doi.org/10.1542/peds.2025-071516
Peñacoba, C., & Catala, P. (2019). Associations between breastfeeding and mother-infant relationships: A systematic review. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 14(9), 616–629. https://doi.org/10.1089/bfm.2019.0106
Pérez-Escamilla, R., Buccini, G. S., Segura-Pérez, S., & Piwoz, E. (2019). Perspective: Should exclusive breastfeeding still be recommended for 6 Months? Advances in Nutrition, 10(6), 931–943. https://doi.org/10.1093/advances/nmz039
Pérez-Escamilla, R., & Chapman, D. J. (2001). Validity and public health implications of maternal perception of the onset of lactation: An international analytical overview. The Journal of Nutrition, 131(11), 3021S–3024S. https://doi.org/10.1093/jn/131.11.3021S
Pérez-Escamilla, R., Tomori, C., Hernández-Cordero, S., Baker, P., Barros, A. J. D., Bégin, F., Chapman, D. J., Grummer-Strawn, L. M., McCoy, D., Menon, P., Ribeiro Neves, P. A., Piwoz, E., Rollins, N., Victora, C. G., & Richter, L. (2023). Breastfeeding: Crucially important, but increasingly challenged in a market-driven world. The Lancet, 401(10375), 472–485. https://doi.org/10.1016/S0140-6736(22)01932-8
Petit, M., Smart, D. A., Sattler, V., & Wood, N. K. (2021). Examination of factors that contribute to breastfeeding disparities and inequities for Black women in the US. Journal of Nutrition Education and Behavior, 53(11), 977–986. https://doi.org/10.1016/j.jneb.2021.08.013
Pineda, R., Knudsen, K., Breault, C. C., Rogers, E. E., Mack, W. J., & Fernandez-Fernandez, A. (2023). NICUs in the US: Levels of acuity, number of beds, and relationships to population factors. Journal of Perinatology, 43(6), 796–805. https://doi.org/10.1038/s41372-023-01693-6
Quinn, E. A., Palmquist, A. E. L., & Tomori, C. (2023). Biocultural lactation: Integrated approaches to studying lactation within and beyond anthropology. Annual Review of Anthropology, 52(1), 473–490. https://doi.org/10.1146/annurev-anthro-101819-110135
Raju, T. N. K. (2022). Achieving Healthy People 2030 breastfeeding targets in the United States: Challenges and opportunities. Journal of Perinatology, 43, 74–80. https://doi.org/10.1038/s41372-022-01535-x
Redshaw, M., Rowe, R., & Henderson, J. (2014). Listening to parents after stillbirth or the death of their baby after birth. Oxford: National Perinatal Epidemiology Unit, University of Oxford.
Reid, L. D. (2024). Trends in severe maternal morbidity complications by patient characteristics, 2016–2021 (HCUP Statistical Brief #312). Agency for Healthcare Research and Quality. https://hcup-us.ahrq.gov/reports/statbriefs/sb312-severe-maternal-morbidity-2016-2021.pdf
Renfrew, M. J., McCormick, F. M., Wade, A., Quinn, B., & Dowswell, T. (2012). Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews, (5), Article CD001141. https://doi.org/10.1002/14651858.CD001141.pub4
Reno, R. (2018). Using group model building to develop a culturally grounded model of breastfeeding for low-income African American women in the USA. Journal of Clinical Nursing, 27(17–18), 3363–3376. https://doi.org/10.1111/jocn.13791
Rhodes, E. C., Zahid, M., Abuwala, N., Damio, G., LaPlant, H. W., Crummett, C., Surprenant, R., & Pérez-Escamilla, R. (2024). Experiences of breastfeeding peer counseling among women with low incomes in the US: a qualitative evaluation. BMC Pregnancy and Childbirth, 24(1), 120. https://doi.org/10.1186/s12884-023-06213-0
Roberts, A., Bitar, G., Moustafa, A., Shahbazian, C., Drone, K., Folh, K., & Blackwell, S. (2025). “Keep transfusing until the bleeding stops”—Massive transfusion and circulatory overload in obstetric hemorrhage. Pregnancy, 1(S1), e12026. https://doi.org/10.1002/pmf2.12026
Robinson, K., Fial, A., & Hanson, L. (2019). Racism, bias, and discrimination as modifiable barriers to breastfeeding for African American women: A scoping review of the literature. Journal of Midwifery & Women’s Health, 64(6), 734–742. https://doi.org/10.1111/jmwh.13058
Roig, J., Rekawek, P., Doctor, T., Naert, M. N., Cadet, J., Monro, J., Stone, J. L., & Liu, L. Y. (2024). Postpartum hemorrhage after vaginal delivery is associated with a decrease in immediate breastfeeding success. American Journal of Perinatology, 41(16), 2252–2257. https://doi.org/10.1055/s-0044-1786750
Rollins, N. C., Bhandari, N., Hajeebhoy, N., Horton, S., Lutter, C. K., Martines, J. C., Piwoz, E. G., Richter, L. M., & Victora, C. G. (2016). Why invest, and what it will take to improve breastfeeding practices? The Lancet, 387(10017), 491–504. https://doi.org/10.1016/S0140-6736(15)01044-2
Rosenberg, K. R. (2021). The evolution of human infancy: Why it helps to be helpless. Annual Review of Anthropology, 50, 423–440. https://doi.org/10.1146/annurev-anthro-111819-105454
Rosenberg, K. R., & Trevathan, W. R. (2016). Costly and cute: Helpless infants and human evolution. University of New Mexico Press. https://muse.jhu.edu/pub/169/edited_volume/book/48244
Royal College of Anaesthetists, Faculty of Intensive Care Medicine, Obstetric Anaesthetists’ Association, & Intensive Care Society. (2018). Care of the critically ill woman in childbirth: Enhanced maternal care. https://www.rcoa.ac.uk/sites/default/files/documents/2020-06/EMC-Guidelines2018.pdf
Ryan, A. S., & Zhou, W. (2006). Lower breastfeeding rates persist among the Special Supplemental Nutrition Program for Women, Infants, and Children participants, 1978–2003. Pediatrics, 117(4), 1136–1146. https://doi.org/10.1542/peds.2005-1555
Sabancı Baransel, E., Uçar, T., & Güney, E. (2023). Effects of prenatal breast-feeding education on postnatal breast-feeding fear in pregnant women in the COVID-19 pandemic: A randomized clinical trial. International Journal of Nursing Practice, 29(2), e13105. https://doi.org/10.1111/ijn.13105
Salariya, E. M., Easton, P. M., & Cater, J. I. (1978). Duration of breast-feeding after early initiation and frequent feeding. The Lancet, 312(8100), 1141–1143. https://doi.org/10.1016/S0140-6736(78)92289-4
Schanler, R. J. (2011). Outcomes of human milk-fed premature infants. Seminars in Perinatology, 35(1), 29–33. https://doi.org/10.1053/j.semperi.2010.10.004
Scheeren, M. F. D. C., Fiori, H. H., Machado, L. U., Volkmer, D. D. F. V., & Oliveira, M. G. D. (2022). Exact gestational age, term versus early term, is associated with different breastfeeding success rates in mothers delivered by elective cesarean section. Breastfeeding Medicine, 17(10). https://doi.org/10.1089/bfm.2022.0068
Schneider, A., & Gibbs, H. M. (2023). Data dashboard: An overview of child care and early learning in the United States. Center for American Progress. https://researchconnections.org/childcare/resources/173461
Schrott, R., Song, A., & Ladd-Acosta, C. (2022). Epigenetics as a biomarker for early-life environmental exposure. Current Environmental Health Reports, 9(4), 604–624. https://doi.org/10.1007/s40572-022-00373-5
Scorza, P., Duarte, C. S., Hipwell, A. E., Posner, J., Ortin, A., Canino, G., Monk, C., & Program Collaborators for Environmental influences on Child Health Outcomes. (2019). Research review: Intergenerational transmission of disadvantage: Epigenetics and parents’ childhoods as the first exposure. Journal of Child Psychology and Psychiatry, 60(2), 119–132. https://doi.org/10.1111/jcpp.12877
Section on Breastfeeding. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. https://doi.org/10.1542/peds.2011-3552
Segura-Pérez, S., Hromi-Fiedler, A., Adnew, M., Nyhan, K., & Pérez-Escamilla, R. (2021). Impact of breastfeeding interventions among United States minority women on breastfeeding outcomes: A systematic review. International Journal for Equity in Health, 20(1), 72. https://doi.org/10.1186/s12939-021-01388-4
Segura-Pérez, S., Richter, L., Rhodes, E. C., Hromi-Fiedler, A., Vilar-Compte, M., Adnew, M., Nyhan, K., & Pérez-Escamilla, R. (2022). Risk factors for self-reported insufficient milk during the first 6 months of life: A systematic review. Maternal & child nutrition, 18(Suppl 3), e13353. https://doi.org/10.1111/mcn.13353
Seoane Estruel, J., & Andreyeva, T. (2025). Breastfeeding trends following the US infant formula shortage. Pediatrics, 155(1), e2024067139. https://doi.org/10.1542/peds.2024-067139
Shetler, A., Guthrie, J., Thoma, M., & Hodges, L. (2023). Rates of breastfeeding initiation increased among low-income women, 2009–17; racial and ethnic disparities persist. USDA Economic Research Service. https://www.ers.usda.gov/amber-waves/2023/october/rates-of-breastfeeding-initiation-increased-among-low-income-women-2009-17-racial-and-ethnic-disparities-persist/
Simpson, K. R. (2022). Trends in labor induction in the United States, 1989 to 2020. MCN: The American Journal of Maternal/Child Nursing, 47(4), 235. https://doi.org/10.1097/NMC.0000000000000824
Sobczak, A., Taylor, L., Solomon, S., Ho, J., Kemper, S., Phillips, B., Jacobson, K., Castellano, C., Ring, A., Castellano, B., & Jacobs, R. J. (2023). The effect of doulas on maternal and birth outcomes: A scoping review. Cureus, 15(5), e39451. https://doi.org/10.7759/cureus.39451
Spatz, D. L. (2004). Ten steps for promoting and protecting breastfeeding for vulnerable infants. The Journal of Perinatal & Neonatal Nursing, 18(4), 385–396. https://doi.org/10.1097/00005237-200410000-00009
———. (2016). Informal Milk Sharing. MCN: The American Journal of Maternal/Child Nursing, 41(2), 125. https://doi.org/10.1097/NMC.0000000000000225
Spatz, D. L., Álvarez Rodríguez, S., Benjilany, S., Finderle, B., von Gartzen, A., Yates, A., & Brumley, J. (2024). Having enough milk to sustain a lactation journey: A call to action. Nursing for Women’s Health, 28(4). https://doi.org/10.1016/j.nwh.2024.02.007
Spiteri, G., & Xuereb, R. B. (2012). Going back to work after childbirth: Women’s lived experiences. Journal of Reproductive and Infant Psychology, 30(1), 1–16. https://doi.org/10.1080/02646838.2012.693153
Sriraman, N. K. (2017). The nuts and bolts of breastfeeding: Anatomy and physiology of lactation. Current Problems in Pediatric and Adolescent Health Care, 47(12), 305–310. https://doi.org/10.1016/j.cppeds.2017.10.001
Sriraman, N. K., Evans, A. E., Lawrence, R., Noble, L., & Board of Directors of the Academy of Breastfeeding Medicine. (2018). Academy of Breastfeeding Medicine’s 2017 position statement on informal breast milk sharing for the term healthy infant. Breastfeeding Medicine, 13(1), 2–4. https://doi.org/10.1089/bfm.2017.29064.nks
Stoody, E. E., Spahn, J. M., & Casavale, K. O. (2019). The pregnancy and birth to 24 months project: A series of systematic reviews on diet and health. The American Journal of Clinical Nutrition, 109(Suppl 7), 685S–697S. https://doi.org/10.1093/ajcn/nqy372
Stuebe, A. (2022). Medical complications of mothers. In R. A. Lawrence & R. M. Lawrence (Eds.), Breastfeeding: A guide for the medical profession (9th ed.). Elsevier. https://doi.org/10.1016/B978-0-323-68013-4.00015-8
Stuebe, A. M., Horton, B. J., Chetwynd, E., Watkins, S., Grewen, K., & Meltzer-Brody, S. (2014). Prevalence and risk factors for early, undesired weaning attributed to lactation dysfunction. Journal of Women’s Health, 23(5), 404–412. https://doi.org/10.1089/jwh.2013.4506
Stuebe, A. M., Jegier, B. J., Schwarz, E. B., Green, B. D., Reinhold, A. G., Colaizy, T. T., Bogen, D. L., Schaefer, A. J., Jegier, J. T., Green, N. S., & Bartick, M. C. (2017). An online calculator to estimate the impact of changes in breastfeeding rates on population health and costs. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 12(10), 645–658. https://doi.org/10.1089/bfm.2017.0083
Su, Q., Sun, X., Zhu, L., Yan, Q., Zheng, P., Mao, Y., & Ye, D. (2021). Breastfeeding and the risk of childhood cancer: A systematic review and dose-response meta-analysis. BMC Medicine, 19(1), 90. https://doi.org/10.1186/s12916-021-01950-5
Sudfeld, C. R., Fawzi, W. W., & Lahariya, C. (2012). Peer support and exclusive breastfeeding duration in low and middle-income countries: A systematic review and meta-analysis. PloS one, 7(9), e45143. https://doi.org/10.1371/journal.pone.0045143
Sullivan, S., Schanler, R. J., Kim, J. H., Patel, A. L., Trawöger, R., Kiechl-Kohlendorfer, U., Chan, G., Blanco, C. L., Abrams, S., Cotton, C. M., Laroia, N., Ehrenkranz, R. A., Dudell, G., Cristofalo, E. A., Meier, P., Lee, M. L., Rechtman, D. J., & Lucas, A. (2010). An exclusively human milk–based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk–based products. Journal of Pediatrics, 156(4), 562–567.e1. https://doi.org/10.1016/j.jpeds.2009.10.040
Tan, J., Zhang, Z., Yan, L. L., & Xu, X. (2024). The developmental origins of health and disease and intergenerational inheritance: A scoping review of multigenerational cohort studies. Journal of Developmental Origins of Health and Disease, 15, e1. https://doi.org/10.1017/S2040174424000035
Thompson, J. F., Heal, L. J., Roberts, C. L., & Ellwood, D. A. (2010). Women’s breastfeeding experiences following a significant primary postpartum haemorrhage: A multicentre cohort study. International Breastfeeding Journal, 5(1), 5. https://doi.org/10.1186/1746-4358-5-5
Thukral, A., Sankar, M. J., Agarwal, R., Gupta, N., Deorari, A. K., & Paul, V. K. (2012). Early skin-to-skin contact and breast-feeding behavior in term neonates: A randomized controlled trial. Neonatology, 102(2), 114–119. https://doi.org/10.1159/000337839
Tomori, C., Hernández-Cordero, S., Busath, N., Menon, P., & Pérez-Escamilla, R. (2022). What works to protect, promote and support breastfeeding on a large scale: A review of reviews. Maternal & Child Nutrition, 18(Suppl 3), e13344. https://doi.org/10.1111/mcn.13344
Tomori, C., & Palmquist, A. E. L. (2022). Racial capitalism and the US formula shortage: A policy analysis of the formula industry as a neocolonial system. Frontiers in Sociology, 7, 961200. https://doi.org/10.3389/fsoc.2022.961200
Tomori, C., Palmquist, A. E. L., & Quinn, E. A. (2018). Breastfeeding: New anthropological approaches. Routledge.
Tschiderer, L., Seekircher, L., Kunutsor, S. K., Peters, S. A. E., O’Keeffe, L. M., & Willeit, P. (2022). Breastfeeding is associated with a reduced maternal cardiovascular risk: Systematic review and meta-analysis involving data from 8 studies and 1,192,700 parous women. Journal of the American Heart Association, 11(2), e022746. https://doi.org/10.1161/JAHA.121.022746
Tucker, Z., & O’Malley, C. (2022). Mental health benefits of breastfeeding: A literature review. Cureus, 14(9), e29199. https://doi.org/10.7759/cureus.29199
Ulfa, Y., Maruyama, N., Igarashi, Y., & Horiuchi, S. (2023). Early initiation of breastfeeding up to six months among mothers after cesarean section or vaginal birth: A scoping review. Heliyon, 9(6), e16235. https://doi.org/10.1016/j.heliyon.2023.e16235
Underwood, M. A. (2013). Human milk for the premature infant. Pediatric Clinics of North America, 60(1), 189–207. https://doi.org/10.1016/j.pcl.2012.09.008
U.S. Department of Agriculture. (2024). WIC breastfeeding data local agency report: Fiscal year 2023. Food and Nutrition Service. https://fns-prod.azureedge.us/sites/default/files/resource-files/wic-fy23-bfdla-report.pdf
U.S. Department of Labor. (2024). New data: Childcare costs remain an almost prohibitive expense. U.S. Department of Labor Blog. https://blog.dol.gov/2024/11/19/new-data-childcare-costs-remain-an-almost-prohibitive-expense
U.S. Food and Drug Administration. (2018). Use of donor human milk. U.S. Food and Drug Administration. https://www.fda.gov/science-research/pediatrics/use-donor-human-milk
Updegrove, K. (2004). Necrotizing enterocolitis: The evidence for use of human milk in prevention and treatment. Journal of Human Lactation, 20(3), 335–339. https://doi.org/10.1177/0890334404269800
van Veenendaal, N. R., Heideman, W. H., Limpens, J., Van Der Lee, J. H., Van Goudoever, J. B., Van Kempen, A. A. M. W., & Van Der Schoor, S. R. D. (2019). Hospitalising preterm infants in single family rooms versus open bay units: A systematic review and meta-analysis. The Lancet Child & Adolescent Health, 3(3), 147–157. https://doi.org/10.1016/S2352-4642(18)30375-4
van Veenendaal, N. R., van der Schoor, S. R. D., Heideman, W. H., Rijnhart, J. J. M., Heymans, M. W., Twisk, J. W. R., van Goudoever, J. B., & van Kempen, A. A. M. W. (2020). Family integrated care in single family rooms for preterm infants and late-onset sepsis: A retrospective study and mediation analysis. Pediatric Research, 88(4), 593–600. https://doi.org/10.1038/s41390-020-0875-9
Vedam, S., Stoll, K., MacDorman, M., Declercq, E., Cramer, R., Cheyney, M., Fisher, T., Butt, E., Yang, Y. T., & Powell Kennedy, H. (2018). Mapping integration of midwives across the United States: Impact on access, equity, and outcomes. PLoS one, 13(2), e0192523. https://doi.org/10.1371/journal.pone.0192523
Victora, C. G., Bahl, R., Barros, A. J. D., França, G. V. A., Horton, S., Krasevec, J., Murch, S., Sankar, M. J., Walker, N., Rollins, N. C., & Lancet Breastfeeding Series Group. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387(10017), 475–490. https://doi.org/10.1016/S0140-6736(15)01024-7
Wallenborn, J. T., Cha, S., & Masho, S. W. (2018). Association between intimate partner violence and breastfeeding duration: Results from the 2004—2014 pregnancy risk assessment monitoring system. Journal of Human Lactation, 34(2), 233–241. https://doi.org/10.1177/0890334418757447
Walters, D. D., Phan, L. T. H., & Mathisen, R. (2019). The cost of not breastfeeding: Global results from a new tool. Health Policy and Planning, 34(6), 407–417. https://doi.org/10.1093/heapol/czz050
Watkins, S., Meltzer-Brody, S., Zolnoun, D., & Stuebe, A. (2011). Early breastfeeding experiences and postpartum depression. Obstetrics and Gynecology, 118(2 Pt 1), 214–221. https://doi.org/10.1097/AOG.0b013e3182260a2d
Weiss, A., Liang, L., & Martin, K. (2022). Overview of hospital stays among children and adolescents, 2019. Agency for Healthcare Research and Quality. https://hcup-us.ahrq.gov/reports/statbriefs/sb299-Hospital-Stays-Children-2019.jsp
World Health Organization (WHO). (2021). Breastfeeding. World Health Organization. https://www.who.int/health-topics/breastfeeding
———. (2023a). Infant and young child feeding: Fact sheet. https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding
———. (2023b, October 16). WHO guideline for complementary feeding of infants and young children 6–23 months of age. https://www.who.int/publications/i/item/9789240081864
World Health Organization (WHO) & United Nations Children’s Fund (UNICEF). (2003). Global strategy for infant and young child feeding. World Health Organization. https://www.who.int/publications/i/item/9241562218
———. (2018). Implementation guidance: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: The revised Baby-Friendly Hospital Initiative.
———. (2021). Global Breastfeeding Scorecard 2021: Protecting breastfeeding through bold national actions during the COVID-19 pandemic and beyond.
Yang, S., Martin, R. M., Oken, E., Hameza, M., Doniger, G., Amit, S., Patel, R., Thompson, J., Rifas-Shiman, S. L., Vilchuck, K., Bogdanovich, N., & Kramer, M. S. (2018). Breastfeeding during infancy and neurocognitive function in adolescence: 16-year follow-up of the PROBIT cluster-randomized trial. PLoS Medicine, 15(4), e1002554. https://doi.org/10.1371/journal.pmed.1002554
You, H., Lei, A., Xiang, J., Wang, Y., Luo, B., & Hu, J. (2020). Effects of breastfeeding education based on the self-efficacy theory on women with gestational diabetes mellitus: A CONSORT-compliant randomized controlled trial. Medicine, 99(16), e19643. https://doi.org/10.1097/MD.0000000000019643
Zhang, Q., Chen, C., Xue, H., Park, K., & Wang, Y. (2021). Revisiting the relationship between WIC participation and breastfeeding among low-income children in the U.S. After the 2009 WIC food package revision. Food Policy, 101, 102089. https://doi.org/10.1016/j.foodpol.2021.102089
Zhao, Y., Lin, Q., Zhu, X., & Wang, J. (2021). Randomized clinical trial of a prenatal breastfeeding and mental health mixed management intervention. Journal of Human Lactation, 37(4), 761–774. https://doi.org/10.1177/0890334421991058
Zimmerman, D., Bartick, M., Feldman-Winter, L., Ball, H. L., & Academy of Breastfeeding Medicine. (2023). ABM clinical protocol #37: Physiological infant care-managing nighttime breastfeeding in young infants. Breastfeeding Medicine, 18(3), 159–168. https://doi.org/10.1089/bfm.2023.29236.abm

























































