Summary
The consistent and compelling evidence concerning how social determinants shape health has led to a growing recognition throughout the health care sector that improvements in overall health metrics are likely to depend—at least in part—on attention being paid to these social determinants. The shift in the health care sector toward value-based payments that incentivize prevention and improved health and health care outcomes for persons and populations rather than service delivery alone has made possible expanded approaches to addressing health-related factors that may be upstream from the clinical encounter. And there is increasing interest in the role of the health care sector in mitigating adverse social determinants (termed “social risk factors” and including a lack of access to stable housing, nutritious food, or reliable transportation) in order to achieve more equitable health outcomes. The combined result of these trends has been a growing emphasis on health care systems paying attention to upstream factors and addressing the social determinants of health (SDOH).1 Taking social risk factors into account is critical to improving both primary prevention and the treatment of acute and chronic illness because social contexts influence the delivery and outcomes of health care.
In considering how health care systems should address these social determinants, a number of important questions arise, including how to integrate social care (that is, services that address health-related social risk factors and social needs) into clinical practice and what kinds of
___________________
1 A list of social determinants of health is included in Table 1-1 of this report.
infrastructure will be required to facilitate such activities. To begin addressing these questions, a broad coalition of foundations, social work associations, educational institutions, and other organizations came together to support this National Academies of Sciences, Engineering, and Medicine (the National Academies) study. The study was intended to examine the potential for integrating services addressing social needs and the SDOH into the delivery of health care with the ultimate goal of achieving better health outcomes.2 The National Academies appointed a committee of 18 subject-matter experts to address this task. Specifically, the committee was asked to assess several factors: the approaches to social care integration that are currently being taken by health care providers and systems as well as any new or emerging approaches and opportunities; the current roles in such integration that are being taken on by different disciplines and organizations as well as new or emerging roles and types of providers; and the current and emerging efforts to design health care systems in such a way as to improve the nation’s health and reduces health inequities. The committee also was asked to recommend how to expand social care services, to better coordinate roles for social care providers in interprofessional care teams in diverse health settings, and to optimize the effectiveness of social care services to improve health and health care.
Over the course of the 18-month study, the committee held four in-person meetings and two Web-based meetings to gather evidence, review and deliberate on the evidence, and develop conclusions and recommendations. Several types of evidence were considered, including peer-reviewed literature, reports from governmental agencies and private organizations, books, websites, and invited presentations to the committee during public sessions. Although the committee cast a wide net in its efforts to identify relevant sources of information, it did not conduct a systematic literature review. As part of the National Academies consensus study process, the committee’s draft report underwent a rigorous, independent external review by another group of experts to ensure that the report addressed its charge, that its findings are supported by the scientific evidence, that its exposition and organization are effective, and that it is impartial and objective.
FIVE HEALTH CARE ACTIVITIES TO BETTER INTEGRATE SOCIAL CARE
The committee identified five complementary activities that can facilitate the integration of social care into health care. The activities are
___________________
2 The complete Statement of Task is presented in Chapter 1 of this report.
awareness, adjustment, assistance, alignment, and advocacy (see Figure S-1 and Table S-1). The specific types of activities that are undertaken will likely vary across health care settings and within settings and also by the social factors being addressed, and the context of a setting will influence which specific types of social and health care integration activities are adopted.
Some health care systems have had success using these five types of activities to strengthen social care services and to link social care with improved health outcomes. However, in most cases where social care activities occur, there have been few robust outcome evaluations carried out, which limited the committee’s ability to make recommendations about specific evidence-based practices. Rather, the committee focused on a framework that describes the scope of these practices.
FINDINGS
Each of the five activities described in the previous section—awareness, adjustment, assistance, alignment, and advocacy—involves systems-level changes. After a review of the evidence base on existing and emerging activities and opportunities for integrating social care into health care, the committee identified three key necessities for successful integration: an appropriately staffed and trained workforce, health information technology innovations, and new financing models.
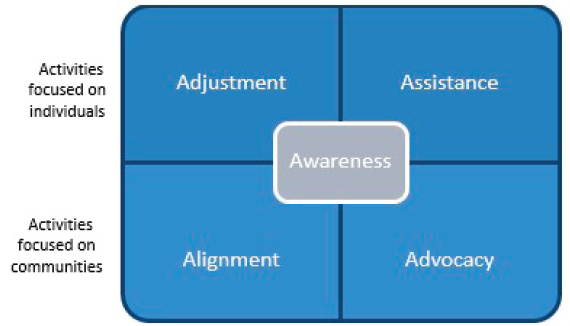
TABLE S-1
Definitions of Health Care System Activities That Strengthen Social Care Integration
| Activity | Definition | Transportation-Related Example |
|---|---|---|
| Awareness | Activities that identify the social risks and assets of defined patients and populations. | Ask people about their access to transportation. |
| Adjustment | Activities that focus on altering clinical care to accommodate identified social barriers. | Reduce the need for in-person health care appointments by using other options such as telehealth appointments. |
| Assistance | Activities that reduce social risk by providing assistance in connecting patients with relevant social care resources. | Provide transportation vouchers so that patients can travel to health care appointments. Vouchers can be used for ride-sharing services or public transit. |
| Alignment | Activities undertaken by health care systems to understand existing social care assets in the community, organize them to facilitate synergies, and invest in and deploy them to positively affect health outcomes. | Invest in community ride-sharing or time-bank programs. |
| Advocacy | Activities in which health care organizations work with partner social care organizations to promote policies that facilitate the creation and redeployment of assets or resources to address health and social needs. | Work to promote policies that fundamentally change the transportation infrastructure within the community. |
Workforce
All members of an interprofessional team working to address health-related social needs may have a role in carrying out awareness, adjustment, assistance, alignment, and advocacy activities. The social care workers on the team may include nurses; physicians; social workers; community health workers; social service navigators, aides, assistants, and trained volunteers; home health aides; personal care aides; family caregivers; case managers; gerontologists; lawyers; and others. The committee found that
- Effectively integrating social care into the delivery of health care requires effective interprofessional teams that include experts in social care.
- The social care workforce can include many types of workers. Social workers are specialists in providing social care who have a long history of working within health care delivery. Models
-
that include community health workers show promise. As models continue to evolve and develop, roles may expand for other workers, such as social service navigators, aides, and assistants; trained volunteers; home health aides and personal care aides; and family caregivers. Other fields are emerging to meet the social needs of older adults (e.g., gerontology) and other specific populations. Integrating other professions—such as lawyers through medical–legal partnerships—also holds promise.
- Understanding the role each member of an interprofessional team plays in the awareness, adjustment, assistance, alignment, and advocacy activities is important for ensuring effective collaboration among team members and for maximizing their ability to address patients’ social needs.
- In order to effectively address social care in the delivery of health care, interprofessional team members should operate at their full scope of practice. Federal, state, and institutional barriers limit the scope of practice and the full use of social workers and other social care workers in caring for patients, such as in providing care management as part of an interprofessional team.
- For interprofessional teams to effectively address social care in the context of health care financing structures need to be aligned. Federal, state, and institutional barriers exist that may limit the adequate payment of social workers, gerontologists, and other social care workers.
- Research is needed on workforce issues related to integrating social care and health care, including studying the effect on health and financial outcomes of various configurations of the health care workforce intended to better address the social needs of the populations served.
Data and Digital Tools
Advances in technology that allow for the application of data and digital tools have the potential to improve efforts by health care systems and their social care partners to address health-related social needs via awareness, adjustment, assistance, alignment, and advocacy activities. Many sources of data exist, including health care claims, electronic health records, census data, and community-level findings concerning the SDOH. The types of digital tools available include predictive analytics, natural language processing, geocoding and hotspotting (the strategic use of data to reallocate resources to a small subset of high-needs, high-cost patients), point-of-care decision support, augmented intelligence, the Internet of Things, telehealth and other virtual care, automated interactions
(e.g., chat bots and holograms), self-driving cars, and digital platforms for interoperability. The committee found that
- Data and technology have transformed the consumer experience in many sectors of life and are doing so in health care.
- Billions of dollars in federal resources spurred the digitization of health care through the widespread adoption of electronic health records and interoperability. Social care has not benefited from the same resources and policy attention as has the health care sector, and it lags far behind in digitization.
- Private equity has supported the health technology economy. Venture capitalists are increasingly investing in health technology startup companies that are working to address the SDOH.
- Local efforts to share health care and social care data exist, including emerging private-sector solutions. These are not supported by a strategic national vision or coupled with resources or defined technology standards.
- Interoperability and data sharing between health care and social care are hampered by the lack of infrastructure, data standards, and modern technology architecture shared between and among organizations.
- With an increasing number of stakeholders sharing protected health information in order to coordinate care, data privacy and security remain challenging elements to manage.
- Digital approaches to integrating social care into health care may increase existing health disparities by exacerbating the digital divide and by codifying bias within health systems.
- There is a paucity of rigorous research that can inform a collective understanding of best practices and outcomes of efforts to integrate social care with health care.
Financing
The financing of health care offers an opportunity to better integrate social care into health care, but substantial barriers exist to doing so. The key challenges identified by the committee are how the legal definition of health care affects the inclusion of social care, how methods for paying providers incentivize or disincentivize the integration of social care into health care delivery, how quality and accountability for the integration of social care are defined and measured, how care for populations with complex social and health needs is financed, and the limited administrative capacity of many social care providers. The committee grouped its findings into the following categories:
-
Definition of health care and how it affects the inclusion of social care as part of health care
- Statute and contract definitions of what constitutes health care have been largely driven by the cultural history of medicine and have made it less likely that social care activities would be included in the health care setting.
- Within existing definitions of health care, state Medicaid programs and their contracted managed care plans and accountable providers are innovating with awareness, adjustment, assistance, and alignment activities to pay for social care in health care settings using state plan amendment authority and the waiver process.
- There remains great variation among states in the level of social care activity; the Centers for Medicare & Medicaid Services (CMS) provides only limited guidance about permissible social care activities and benefits.
- Rate-setting processes for health plans and providers can be influential in obtaining financing for the integration of social care in the health care setting; the key factors are the rates calculated, risk adjustment elements to those rates, performance incentives, and the definition of medical services and quality improvement activities in the calculation of medical loss ratios.
- Among the states with approved waivers there is much experimentation, with informal mechanisms for learning the results of the experimentation. Formal evaluations of these waiver activities typically are not timely and do not influence policy and practice.
- The Medicare Advantage plan bidding process insufficiently promotes competition on the basis of care coordination and high-quality care.
- Medicare’s new supplemental benefits guidance to Medicare Advantage plans, made possible by the Creating High-Quality Results and Outcomes Necessary to Improve Chronic Care Act of 2018 (CHRONIC Care Act),3 has created new opportunities to integrate social care into the health care of Medicare beneficiaries.
-
Incentives to integrate health care and social care
- The prevailing model of health care provider payment—fee-for-service—does not encourage the integration of social care. The current shift to alternate payment models led by the
___________________
3 Section III of Public Law 115-123, February 9, 2018.
-
-
Center for Medicare & Medicaid Innovation (a center within CMS) activities—particularly the shift to accountable care organizations—aligns incentives for the provision of social care.
- Just as state Medicaid programs are experimenting with different covered services definitions, they are innovating with new methods to pay providers, such as through accountable care organizations, in part to encourage more social care integration work. There is less such work taking place for commercial and Medicare populations. Furthermore, great variation among states exists in the types of population-based payment models (i.e., models in which a provider agrees to accept responsibility for the health of a group of patients in exchange for a set amount of money) that are being deployed, and, as with covered service definitions, states and, in some cases, their contracted health plans are not performing formal evaluation of these activities.
-
-
Quality and accountability
- Definitions of health care services and conditions have historically provided insufficient clarity and guidance for integrating and addressing social care.
- Population outcome measures for accountable entities, or accountable care organizations, are numerous and highly variable among the states.
- The conclusions included in a previous National Academies report on adjusting Medicare payments for social risk factors4 have not been applied in Medicaid settings to payments or outcome measures.
- Even with good accountability measures, health plans and providers struggle to justify investments when returns are delayed and accrue to collaborators. The lack of continuous eligibility for Medicaid benefits exacerbates this problem, as does the long-term nature of the returns on investments in social care integration and on upstream investment in pediatric populations. Geographic exclusivity, which limits the number of providers operating within a region, makes it possible for partners to make longer-term investments, but this is not possible in populous settings.
___________________
4 National Academies of Sciences, Engineering, and Medicine. 2017. Accounting for social risk factors in Medicare payment. Washington, DC: The National Academies Press. https://doi.org/10.17226/23635.
-
- The Internal Revenue Service (IRS) community benefit standard is another opportunity to finance the integration of social care in health care settings. Experience has shown varying levels of engagement by health systems, little enforcement by the IRS, and varying levels of aligned attention from states and communities.
-
Financing care for patients with complex health and social needs
- Patients enrolled in both Medicaid and Medicare have the highest social needs, but the division of their health care financing between state and federal agencies creates barriers to addressing those needs in a way that integrates social care.
- The Programs of All-Inclusive Care for the Elderly program enrolls a fraction of dual eligibles and has demonstrated mixed results.
- No systematic evaluations exist for dual-eligible special needs programs in part because each state’s program is unique. The CHRONIC Care Act mandated the evaluation of dual-eligible special needs programs, which may assist with standardization.
- The financial alignment demonstration for dual eligibles shows that while care innovation increases with alignment, administrative and financial challenges remain.
- Evaluations of the financial alignment demonstration have found savings in two states and improved health care use outcomes in additional states. The demonstration has been extended and expanded to accrue more of the data needed to evaluate its effectiveness.
-
Capacity building for social care providers
- Social service agencies and health care organizations have historically not worked together, and they are funded by different systems.
- Health systems may “medicalize” the integration of social care into health care. Health systems often use models of care requiring research, diagnostic codes, and technical specialization, which adds cost and complexity, with the ultimate result being effects on population health that are neutral or negative.
- The administrative costs of social care providers could increase as a result of efforts to integrate social care into a health care setting based on a medical model for consultation and referral.
RECOMMENDATIONS
Enabling the health care sector to engage in activities that strengthen social care and community resources will require new approaches to system design, staffing, information and technology systems, financing, and research. The committee identified five goals whose accomplishment will result in better integration of social care into health care, which may in turn result in improved health and reduced health disparities. Those goals are to
- Design health care delivery to integrate social care into health care, guided by the five health care system activities—awareness, adjustment, assistance, alignment, and advocacy.
- Build a workforce to integrate social care into health care delivery.
- Develop a digital infrastructure that is interoperable between health care and social care organizations.
- Finance the integration of health care and social care.
- Fund, conduct, and translate research and evaluation on the effectiveness and implementation of social care practices in health care settings.
Goal 1. Design health care delivery to integrate social care into health care.
Recommendation 1. Health care organizations should take steps to integrate social care into health care. Specific steps include
- Make and communicate an organizational commitment to addressing health-related social needs and health disparities at the community and individual levels.
- Recognize that comprehensive health care should include understanding an individual’s social context. Evidence is rapidly accumulating concerning the most effective strategies for screening and assessing for social risk factors and social needs. Such strategies should include standardized and validated questions, as available, and should use interoperable data systems to document results.
- Use patient-centered care5 models to more routinely incorporate social risk data into care decisions.
___________________
5 Patient-centered care is defined as providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions (Institute of Medicine. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press. https://doi.org/10.17226/10027).
- Design and implement integrated care systems using approaches that engage patients, community partners, frontline staff, social care workers, and clinicians in planning and evaluation and that incorporate the preferences of patients and communities.
- Include social care workers as being integral to a team-based approach to designing and delivering health care.
- Establish linkages and communication pathways between health care and social service providers. This is important for personal care aides, home care aides, and others who provide care and support for seriously ill and disabled patients and who have extensive knowledge of patients’ social needs.
- Develop and finance referral relationships with selected social care providers when feasible, supported by operational integration such as co-location or patient information systems. Social care providers and health care providers should establish a formal understanding and accountability within their contracting and referral relationships.
- Support the development of those infrastructure components needed to meet the goal of care integration, including the redesign and refinement of workflows, technical assistance and support, staff with the ability to support the redesign, champions of the redesign, information on best practices, health information technology to enhance integration, and support for community partners and their infrastructure needs.
Goal 2. Build a workforce to integrate social care into health care delivery.
Recommendation 2a. State legislatures, licensing boards, professional associations, and federal agencies should develop, expand, and standardize the scopes of practice of social workers, community health workers, gerontologists, and other social care workers.
Recommendation 2b. Social workers and other social care workers should be considered to be providers who are eligible for reimbursement by payers. Public and private payers should create standards for the reimbursement of social care, including assessment and such treatment as chronic care management, behavioral health integration, and transitional care management. Medicare/Medicaid payment advisory commissions should evaluate models in which social workers and other social care workers are reimbursement-eligible providers of social care services.
Recommendation 2c. Funders of health care workforce training (e.g., the U.S. Department of Health and Human Services, the U.S. Department of Veterans Affairs, and foundations) should include the social care workforce in their education, training, and practice initiatives.
Recommendation 2d. Schools for health professions (including schools of medicine and nursing) as well as continuing education programs should incorporate competency-based curricula on social care. Curricula should include evidence on the social determinants of health, protocols for working in interprofessional teams to address social needs in health care settings, interpersonal and organizational approaches to advancing health equity and decreasing health disparities, and competencies relating to collecting, securing, and using data and technology to facilitate social and health care integration. Schools of health professions should also engage social workers in instructional roles in order to model their participation in interprofessional teams and to provide information on social risk screening and social care resources and referrals.
Recommendation 2e. Credentialing organizations for medicine, nursing, and other health professions should incorporate knowledge about the social determinants of health and the importance of addressing social needs in licensing examinations and continuing education requirements.
Recommendation 2f. Schools of social work as well as continuing education programs should use competency-based curricula on social care. In addition to educating students about the social determinants of health and health disparities, the curricula should include information about effective models that integrate social care and health care delivery, the interprofessional workforce, technology, and payment models that facilitate implementation and competencies relating to collecting, securing, and using data and technology to facilitate social and health care integration.
Recommendation 2g. State agencies and academic institutions, including community colleges, should develop standards for training and advancement (e.g., career ladder programs) for community health workers and other emerging social care workers.
Recommendation 2h. Foundations and other funders should commission a follow-up comprehensive report on the role of social work in health care as social care and health care integration continues to evolve.
Recommendation 2i. Foundations and other funders should fund a campaign to raise awareness among the health care professions and others
about the value and contributions of social workers and other social care workers in health care.
Goal 3. Develop a digital infrastructure that is interoperable between health care and social care organizations.
Recommendation 3a. The federal government should establish a 21st-century social care digital infrastructure on a scale similar to that described in the Health Information and Technology for Economic and Clinical Health Act of 2009,6 and it should identify and deploy policies and resources to build the internal capacity necessary for social care organizations and consumers to interoperate and interact with each other and the health care system.
Recommendation 3b. The Office of the National Coordinator should be resourced to act on the Patient Protection and Affordable Care Act of 20107 Section 1561 recommendations, including the adoption of modern, secure, interoperable digital systems and processes that will allow all partners to share the administrative and other data necessary to enable consumers to seamlessly obtain and maintain the full range of available health care and social care services.
Recommendation 3c. The Office of the National Coordinator should support states and regions as they identify the appropriate interoperable platforms for their communities, based on open standards and a modern technical architecture that supports flexible interfaces to allow the health and social care systems and consumers to share the structured data necessary for care coordination, avoidance of error, and a reduced burden on organizations and people being served.
Recommendation 3d. The Federal Health Information Technology Coordinating Committee should facilitate data sharing at the community level across diverse domains such as health care, housing, and education so as to support social care and health care integration.
Recommendation 3e. Integrating social care and health care requires the sharing of new types of data between new partners, some of whom are covered by the privacy rule promulgated by the Health Insurance Portability and Accountability Act of 19968 and some of whom are not; there-
___________________
6 Public Law 111-5, February 17, 2009.
7 Public Law 111-148, March 23, 2010.
8 Public Law 104-191, August 21, 1996.
fore, the U.S. Department of Health and Human Services should work with the private sector to disseminate educational tools and guidance on the data security and privacy issues that arise when collecting and sharing personally identifiable information.
Recommendation 3f. The parts of the public and private sectors involved in developing and implementing analytic and technology resources, including cell and Internet access, should do so with an explicit focus on equity; the goal should be to avoid unintended consequences such as perpetuation or aggravation of discrimination and bias and the further marginalization of populations and to proceed with an appreciation of the impact on the existing social care system.
Goal 4. Finance the integration of health care and social care.
Recommendation 4a. The Centers for Medicare & Medicaid Services should clearly define which aspects of social care that Medicaid can pay for as covered services (e.g., in the context of providing care management, targeted case management, and home- and community-based long-term care services and supports as well as within the context of managed care).
Recommendation 4b. State Medicaid agencies should use the flexibility described by the Centers for Medicare & Medicaid Services in the social care that Medicaid pays for as a covered service and make the opportunities and limitations associated with that flexibility clear to health plans and health care and social care service providers.
Recommendation 4c. The Centers for Medicare & Medicaid Services (CMS) should accelerate learning about how the integration of health and social care can improve health and reduce health care costs by encouraging and approving waivers that support social care. Sustainable financing for effective interventions piloted in the waiver should be identified by the state and CMS as an outcome of the waiver.
Recommendation 4d. States should pursue policies of continuous program eligibility to, among other benefits, create stable pools of populations for which entities can be held accountable.
Recommendation 4e. The Centers for Medicare & Medicaid Services should consider additional Medicare reforms that can broaden Medicare coverage rules in a way that is consistent with lessons from Medicaid populations and the Creating High-Quality Results and Outcomes Necessary
to Improve Chronic Care Act of 2018 (CHRONIC Care Act).9 Health plans should take full advantage of the flexibility provided under the CHRONIC Care Act for supplemental benefits under Medicare.
Recommendation 4f. The Centers for Medicare & Medicaid Services and the states should coordinate the coverage and benefits administration of their Medicare and Medicaid dually eligible populations consistent with the emerging lessons of the financial alignment demonstrations. Efforts to improve alignment should be aggressively pursued over the short and long term, with an intentional focus on social care integration.
Recommendation 4g. The Centers for Medicare & Medicaid Services should develop incentives for health care organizations and the managed care programs that contract with Medicaid and Medicare to collaborate with community-based social services, such as area agencies on aging and centers for independent living.
Recommendation 4h. The Centers for Medicare & Medicaid Services, state Medicaid agencies, employers, and health plans should accelerate the movement to alternative payment models. The measurements aimed at assessing value in these models should include activity-based measures for social care integration and outcome measures that reflect social risk and protective factors. These value-based payment and outcome measurement models should incorporate social risk adjustment and stratification in a way that is consistent with previous recommendations from the National Academies of Sciences, Engineering, and Medicine.10
Recommendation 4i. The U.S. Department of Health and Human Services, payers, and other private organizations, such as foundations and institutions with community-benefit obligations, should provide funding and technical assistance to support formal contractual relationships between community-based organizations and health care entities.
Recommendation 4j. Federal and state policy makers, health plans, health systems, and private-sector investors should consider collective financing mechanisms to spread risk and create shared returns on investments in social care so that returns do not accrue to a single investor.
___________________
9 Public Law 115-123, February 9, 2018.
10 National Academies of Sciences, Engineering, and Medicine. 2017. Accounting for social risk factors in Medicare payment. Washington, DC: The National Academies Press. https://doi.org/10.17226/23635.
Recommendation 4k. Health systems subject to community benefit regulations should comply with those regulations by considering partnering with community organizations to respond to identified community gaps in social care.
Recommendation 4l. States should pursue opportunities to align their hospital licensing requirements and public reporting with federal regulations regarding community benefits to ensure consistent obligations for health systems and to explicitly link their community benefits to the provision of social care.
Goal 5. Fund, conduct, and translate research and evaluation on the effectiveness and implementation of social care practices in health care settings.
Recommendation 5a. Federal and state agencies, payers, providers, delivery systems, and foundations should contribute to advancing research on and the evaluation of the effectiveness and implementation of social care practices.
- The National Institutes of Health (NIH), the Agency for Healthcare Research and Quality (AHRQ), the Centers for Medicare & Medicaid Services (CMS), the Patient-Centered Outcomes Research Institute, the Health Resources and Services Administration (HRSA), and other funders of research and program evaluation should encourage payers, providers, and delivery systems to incorporate a range of study designs and methods that include rapid learning cycles and experimental trials.
- NIH, AHRQ, CMS, foundations, and other funders of research and program evaluation should cultivate and support researchers who have expertise in health services, social sciences, and cross-disciplinary research.
- CMS should fully finance (without state contributions) independent state waiver evaluations to ensure robust evaluation of social care and health care integration pilot programs and to facilitate the dissemination of findings.
- The U.S. Department of Health and Human Services should establish and support a clearinghouse containing information on the best and most promising practices for social care integration in order to provide “lessons learned” to health systems, community-based organizations, researchers, and others.
Recommendation 5b. Funders of health care workforce research (e.g., the Agency for Healthcare Research and Quality and foundations) should include the social care workforce in studies of the effect of the social care workforce on the health and financial outcomes of health care delivery organizations.
Recommendation 5c. The Health Resources and Services Administration and other funders should support studies of the contribution of the social care workforce, including additional workers such as gerontologists and public interest lawyers, to addressing the social determinants of health in health and community care settings.
Recommendation 5d. The Centers for Medicare & Medicaid Services, the U.S. Department of Health and Human Services, state Medicaid agencies, the National Quality Forum, and the National Committee for Quality Assurance should establish mechanisms that ensure that research on effective demonstrations informs more permanent health care reforms, including the development of accountability measures and payment models.
Recommendation 5e. To enable comparative research and evaluation, researchers, evaluators, and agencies that develop measures and standards (e.g., the National Quality Forum, the National Committee for Quality Assurance, and the Centers for Medicare & Medicaid Services) should develop a consensus on and use a common core of measures reflecting social risk and protective factors as well as key health and social outcome measures. These measures should not be limited to clinical or economic metrics, but should include patient-reported outcomes and other outcomes relevant to a range of stakeholders, including patients, families, caregivers, communities, social care organizations, health care organizations, and payers. The Agency for Healthcare Research and Quality should curate these measures in a publicly available item bank.
This page intentionally left blank.

















