Family Caregiving for People with Cancer and Other Serious Illnesses: Proceedings of a Workshop (2023)
Chapter: Proceedings of a Workshop
Proceedings of a Workshop
INTRODUCTION1
The difficult and challenging journeys that people with cancer and other serious illnesses face are often made more manageable by the critical care and support of family caregivers. While they derive great joy and satisfaction from caring for their loved ones, the physical, psychological, emotional, and financial toll that a family caregiver experiences can be significant.
To examine the opportunities to better support family caregivers for people with cancer and other serious illnesses, the Roundtable on Quality Care for People with Serious Illness, the National Cancer Policy Forum, and the Forum on Aging, Disability, and Independence hosted a public workshop, Family Caregiving for People with Cancer and Other Serious Illnesses, on May 16–17, 2022. This workshop built upon previous work, including the 2016 National Academies of Sciences, Engineering, and Medicine (the National Academies) consensus report Families Caring for an Aging America
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop has been prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants, and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
(NASEM, 2016), which called for developing a national family caregiver strategy that recognizes the essential role of caregivers to the well-being of their loved ones. The report noted that family caregivers are not a heterogeneous group and include diverse people of all ages and backgrounds, some of whom do not have a family connection or legally defined relationship with the care recipient but are friends, partners or neighbors. Moreover, the report points out that the circumstances of individual caregivers and the caregiver context are extremely variable. Family caregivers may live with, nearby, or far away from the person receiving care. Regardless, the family caregiver’s involvement is determined primarily by a personal relationship rather than by financial remuneration. The care they provide may be episodic, daily, occasional, or of short or long duration. The caregiver may help with simple household tasks; self-care activities such as getting in and out of bed, bathing, dressing, eating, or toileting; or provide complex medical care tasks, such as managing medications and giving injections.2
This workshop unfolded over six sessions. Greg Link of the Administration for Community Living (ACL) opened the workshop with a Keynote Address that provided an overview of the Recognize, Assist, Include, Support and Engage (RAISE) Family Caregivers Act, and set the stage for subsequent sessions that explored the diverse needs of family caregivers; the resources, support, and training required by family caregivers; several exemplars of effective programs that meet these needs; and the importance of integrating caregivers into the health care team. Presentations also examined key research gaps and opportunities and discussed ways to include caregivers in research activities. The workshop’s final session explored the relevant policy landscape, and initiatives on the national and state levels to support family caregivers, such as the RAISE and the Caregiver Advocacy, Research, and Education (CARE) Acts as well as potential employment policies and insurance benefit designs to support family caregivers. To highlight the critical role of the family caregiver, insights and perspectives of the family caregiving experience—the caregiver voice—were incorporated throughout all of the workshop sessions.
This Proceedings of a Workshop summarizes the presentations and discussions and highlights suggestions from individual participants to improve
___________________
2 The NASEM report uses the terms “family caregiver” and “caregiver” interchangeably and does not use the terms “informal” or “unpaid” although such terms are often used in the economics and medical literature to differentiate family caregivers from “formal” caregivers—paid direct care workers (such as home care aides) or health and social service professionals.
support for family caregivers. These suggestions are discussed throughout the proceedings and are summarized in Box 1. Appendices A and B contain the workshop statement of task and workshop agenda, respectively. The speakers’ presentations (as PDF and audio files) have been archived online.
OPENING REMARKS
Randall Oyer, clinical professor of medicine at the Perelman School of Medicine, medical director of the Ann B. Barshinger Cancer Institute, and medical director of oncology and of the Cancer Risk Evaluation Program at Penn Medicine Lancaster General Health, opened the workshop by noting that in his 40 years as a physician, he personally has seen the critical impact that caregivers make. He added, however, that in his view, the medical profession has misunderstood and undervalued this vital role. Grace Campbell, assistant professor at the Duquesne University School of Nursing, and director of quality and system integration at the Family CARE Center in the gynecologic oncology program at the Hillman Cancer Center at the University of Pittsburgh Medical Center, built on Oyer’s remarks by noting the universality of the caregiving experience. Almost everyone, she observed, is or will be a caregiver at some point in their lives. Nevertheless, with more than 50 million family caregivers in the United States, the health care system has yet to provide widespread, systematic implementation of meaningful programs and resources (AARP and National Alliance for Caregiving, 2020). Campbell’s clinic, for example, offers a listening and supportive ear, assistance with navigating the complex health care system, and referrals to the few resources that are available, but these services barely scratch the surface of what many caregivers need. “Clearly, real change is needed,” said Campbell.
ACL’S ROAD MAP FOR CHANGE
To set the stage for the first session, a short video, entitled “Faces of Caregiving,”3 produced by the ACL was shown. Following the video, Greg Link, director of the Office of Supportive and Caregiver Services at ACL, began by remarking that Campbell’s call for health system recognition of caregivers requires a focused and comprehensive approach at both the federal and state levels to examine the needs and concerns of family caregivers
___________________
3 The short video can be seen at https://acl.gov/RAISE/report (accessed July 20, 2022).
and address them proactively in person- and family-centered ways. “For an experience as common as caregiving, one as old as humanity itself, we do not have a cohesive national approach for addressing an issue that will eventually impact nearly every one of us in some way, and not necessarily in a positive way,” said Link.4
Link shared that he has seen the need to address the challenges of caregiving both professionally, over the course of his 35 years in the aging field, and personally, when he cared for his aging parents. Even as someone who considers himself well versed on the issues, he was surprised at how little he knew about what to do, where to go, and whom to call when faced with the myriad challenges of caring for his parents. Certainly, programs and services were available, but they were fragmented and often hard to locate and access. Despite many positives to caring for a family member, Link observed that, if intense, long, and difficult enough, it will likely result in serious physical and emotional conditions and serious impacts on careers and family finances.
Link explained that the ACL is responsible for implementing the requirements of the RAISE Family Caregivers Act of 20175 and the Supporting Grandparents Raising Grandchildren Act.6 Between those two
___________________
4 For more information on the diversity of the caregiving experience, see https://www.youtube.com/watch?v=PGvTOIwnoys (accessed June 9, 2022).
5 Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act of 2017, Public Law 119, 115th Congress (January 22, 2018).
6 Supporting Grandparents Raising Grandchildren Act, Public Law 196, 115th Congress (July 7, 2018).
acts, Link noted that he and his team are trying to address the breadth of the family caregiving experience. The RAISE Act has three key components: a Family Caregiving Advisory Council, which ACL established in 2019; an initial report to Congress, which the advisory council delivered in September 2021 (RAISE Family Caregiving Advisory Council, 2021); and a national family caregiving strategy, which the advisory council and Supporting Grandparents Raising Grandchildren Advisory Council are developing and will be implementing together. Link explained that the advisory councils’ efforts were combined to take a cohesive approach to developing an inclusive and respectful national response to the needs of family caregivers.
ACL’s report to Congress7 includes 26 recommendations, each accompanied by a story from caregivers and links to videos to bring the recommendations to life, under five broad goals:
- Awareness and outreach
- Engagement of family caregivers as partners in health care and long-term services and supports
- Services and supports for family caregivers
- Financial and workplace security
- Research, data, and evidence-informed practices
Shortly after ACL began implementing the requirements of the RAISE Act, The John A. Hartford Foundation asked how it could help. The collaboration led to the RAISE Family Caregiver Resource and Dissemination Center,8 which the National Academy for State Health Policy (NASHP) developed with funding from the foundation.9 With assistance from Community Catalyst, the University of Massachusetts Boston, and the National Alliance for Caregiving, NASHP helped ACL collect what Link described as “an incredible amount of public input at every step along the way,” including input from caregiver focus groups and information gathered during stakeholder listening sessions with aging and disability organizations.
___________________
7 https://acl.gov/programs/support-caregivers/raise-family-caregiving-advisory-council#:~:text=On%20September%2022%2C%202021%2C%20the,for%20better%20supporting%20family%20caregivers (accessed July 20, 2022).
8 Additional information is available at https://www.nashp.org/the-raise-family-caregiver-resource-and-dissemination-center/ (accessed June 9, 2022).
9 See https://www.johnahartford.org/grants-strategy/the-raise-act-family-caregiver-resource-and-dissemination-center (accessed August 11, 2022).
The advisory councils are using the information gathered through these activities and the 26 recommendations to develop the national strategy, which will identify actions that the federal government, along with states, local communities, providers of health and long-term services and supports, and others can take to recognize and support family caregivers (ACL, 2021). Link noted that the councils have solicited input from 15 federal agencies regarding actions that they would commit to. Link explained that the strategy will seek to eliminate redundancies across agencies and promote greater adoption of the following:
- Person- and family-centered care across settings;
- Assessment and service planning;
- Information, education and training supports, referral and care coordination;
- Respite options;
- Financial security and workplace issues; and
- Service delivery based on the performance, mission, and purpose of a program.
The national caregiving strategy, observed Link, will speak directly to the diverse needs of family caregivers and diversity and inclusion issues. It will be four separate but interlocked documents, starting with a narrative and framing of issues and the 26 recommendations, plus three from the grandparents council, reframed as outcomes that the two advisory councils believe the country needs to achieve. The second document details the more than 350 actions that the federal agencies committed to, within the scope of their current programs.
A third document will discuss actions that states, communities, clinicians, long-term care providers, employers, researchers, faith-based organizations, schools, and other entities can take, based largely on input gathered from the focus groups and listening sessions. It will also include an intensive review of existing reports and recommendations that other organizations have issued and tools, resources, links to other strategies, and examples of successful strategies. The goal is for this to be useful and serve as a road map for any sector that wants to better support and recognize family caregivers, noted Link.
The final document contains the key crosscutting considerations identified by the councils as critical to every action, including the following four broad themes:
- Need for person- and family-centered approaches: As the U.S. works to create a system of interrelated responses to the needs of family caregivers, it is important that the family caregivers themselves—not health care systems or providers—remain the focal point.
- Recognize and address trauma and its impact: Provide support to family caregivers in a trauma informed way.
- Focus on diversity, equity and inclusion: Advance equity by recognizing that family caregivers from unserved, underserved, and/or marginalized communities experience unique needs that often go unaddressed. They are more likely to experience significant disparities in the intensity of caregiving and greater negative physical, emotional, and financial impacts.
- Recognize the importance of direct care workers: The development of a robust, well-trained, and well-paid direct care workforce is critical to ensuring family caregivers and the people they support have access to reliable, trusted supports and assistance when and where they need it.10
Link pointed out that the strategy will not be mandatory, and the RAISE Act does not give ACL any enforcement authority. He expressed confidence, however, that the strategy will become a tool for educators, researchers, advocates, families, and program leaders to examine what they can do, take what they have and see what might be missing, and make it work better and more efficiently with less duplication. Link observed that caregiving can be anxiety producing, empowering, overwhelming, exhausting, hopeful, and lonely, but a national strategy can elevate the conversation, reframe the narrative, drive change and innovation, promote greater recognition and inclusion of family caregivers, be a tool for advocacy, guide program planning and policy development, and shape research. ACL, he added, believes in the power of the consumer voice, which has informed everything it has done to implement the RAISE Act and Grandparents Act.
Link quoted Abena Apau Buckley, a family caregiver featured in the ACL video: “I’m glad that I had the means to be able to do it the way that I did, and still there’s so much that we lost because of how little real support is at a societal level that I had… You’re [going to] get sick, your family members are [going to] get sick, your kids might get sick, that is a given, so
___________________
10 For more information see: https://acl.gov/sites/default/files/RAISE_SGRG/NatlStrategyToSupportFamilyCaregivers.pdf (accessed June 9, 2022).
given that that’s going to happen, why do we not have a solution for how to help people?” Link said he believes that the time is now to provide a path to answering Abena’s question.
Reactor Panel
Sheria Robinson-Lane, assistant professor in the Department of Systems, Populations, and Leadership at the University of Michigan School of Nursing, shared her perspective that it is imperative that the national strategy be inclusive in its approach to what a modern family looks like and the different types of caregivers who need information in ways that allow them to live an optimal life. She pointed out that this is not just about improving access to care and services for people who are dealing with disability, chronic illness, dementia, and other health conditions in a way that relieves some of the caregiver’s burden. It also means giving caregivers access to support for their mental health so they can meet their own daily needs and supporting the most vulnerable caregivers including older adults, people with disabilities, communities of color, as well as the LGBTQ+ community. Robinson-Lane called for an intersectional11 approach in thinking about how to make sure that the person who is most in need is both getting help and being heard. She asked, “How are we ensuring that their voices are still heard when we are in a position of power and leadership? That is truly the way to make sure that a national agenda is inclusive and that we do not leave anybody behind in our approach, so as to make sure that the needs of families and communities are met.”
Loretta Christensen, a member of the Navajo Nation and chief medical officer of the Indian Health Service (IHS), said she appreciated that ACL’s information-gathering process solicited input from tribal communities, which have challenges that other communities do not. In Indian Country, she noted, 9 of every 10 caregivers are family members. During the COVID-19 pandemic, with so much of the medical community focused on testing, vaccinating, and treating COVID patients, what limited services
___________________
11 Intersectionality is defined as “the complex, cumulative way in which the effects of multiple forms of discrimination (such as racism, sexism, and classism) combine, overlap, or intersect especially in the experiences of marginalized individuals or groups.” Merriam-Webster. (n.d.). Intersectionality. In Merriam-Webster’s collegiate dictionary. https://unabridged.merriam-webster.com/collegiate/intersectionality/ (accessed September 28, 2022).
existed became even more scarce. This increased family caregiving responsibilities, even for those who had family members that were seriously ill from COVID, further underscoring the importance of reliable and sustainable support for caregivers.
Christensen explained that Indian Country deals with many social determinants of health that make caregiving challenging. For example, one third of the Navajo Nation homes on tribal land do not have electricity or running water,12 making it imperative to adjust a care plan that typically includes a mechanical device. In addition, broadband does not reach 50 percent of the homes in rural areas in Indian Country,13 making it difficult for those families to access telehealth. She explained that an approach to training, educating, and providing resources is needed for what is essentially a new health care workforce composed of family members.
One imperative, said Christensen, is to provide enhanced access to effective mental health care for caregivers and develop culturally sensitive and appropriate materials. There are 574 recognized tribes, she noted, each with its own customs and understanding of cancer, dementia, and other chronic diseases. Christensen added that the IHS is including trauma-informed care in all of its staff trainings to empower staff to show respect to everyone they encounter. She emphasized that innovation and partnerships are crucial to addressing the challenges of family caregiving in Indian Country.
Discussion
Julie Bynum, professor of medicine in the Division of Geriatric Medicine at the University of Michigan, opened the discussion session with the observation that she was struck that Black and Native American communities, for example, have long been involved in family caregiving in the absence of national and large-program support. She wondered about a way to learn from communities and use that information in creating the national strategy rather than the national strategy telling the communities what to do. Link explained that in the initial RAISE report to Congress and forthcoming National Family Caregiving Strategy, the needs and perspectives of
___________________
12 See https://www.energy.gov/sites/prod/files/2016/01/f29/38_nuta_denetclaw_ahasteen.pdf (accessed July 29, 2022).
13 See https://www.npr.org/2018/12/06/673364305/native-Americans-on-tribal-land-are-the-least-connected-to-high-speed-internet (accessed July 29, 2022).
diverse communities, including tribal communities, are addressed and considered. He specified that racial, cultural, ethnic, and linguistic differences were treated as crosscutting themes that speak to all the recommendations and actions contained in the strategy.
Robinson-Lane commented that too often, the approach is to address problem solving with the majority in mind, which leaves out a minoritized population. In her view, the programs should be designed specifically targeted for minoritized populations that incorporates sensitivity to cultural differences. Another challenge is to include the voice of health care workers who are also caregivers. She noted that often, particularly in the COVID-19 era, health care workers are already feeling considerable stress, and adding the burden of caring for young children at home or an aging parent adds to their stress. To keep the workforce healthy, it is important to support its members, specifically the low-wage workers who are most likely to come from minoritized backgrounds.
Christensen remarked that including people from rural and extremely rural areas at the table and providing services to the people who live there is extremely challenging and not well appreciated by those in more urban areas. Christensen described the area in which she grew up, the Navajo Nation, which encompasses 27,000 square miles,14 where resources can be far from the people who need them. Tanker trucks deliver water to many homes because they do not have running water, and that large geographic area has only 14 grocery stores, creating significant challenges for getting food to families in need. Serving this community and other extremely rural areas is not impossible. However, it requires a different approach, one that accounts for the lack of home care and other services that are more common in less isolated areas and the increased cost of transportation to get to an appointment. Christensen emphasized that partnerships and funding are the key, with the latter being in short supply. On the positive side, she noted, the community cherishes the relationships between the reservation’s families and its elders. Increased education and training for families and optimizing public health nursing and the reservation’s “community health representatives” are needed to support family caregiving.
Bynum noted the importance of reverse translation, which involves applying innovations and lessons learned from communities to inform a more robust national strategy. She asked about signs of increased cohesion
___________________
14 See https://www.nytimes.com/2021/05/21/us/navajo-cherokee-population.html (accessed August 4, 2022).
among community, hospital, family, and clinical services and all the different disciplines involved in delivering care. Link noted that at the federal level, the initial report to Congress included an inventory of the federal programs and initiatives that support family caregivers and that the relevant agencies’ responses overwhelmingly recognized the role they need to play and the interconnectedness of their programs. The key, he said, will be how the agencies come together once the national strategy is released to reduce duplication and identify areas where they can improve collaboration. It will also be important to see how the states, communities, health and long-term services providers, faith communities, school systems, and others will view the strategy and look for ways they can participate. “Once we know what is possible and what supports are needed in the way of technical assistance, we can then begin to take that next step to support that kind of development,” said Link. “I believe that the framework we are creating for a national approach will serve as a real conversation starter.”
Robinson-Lane noted that in her experience, communication is often lacking between federal and state agencies and communities regarding available services and how to access them. She asked, “How do we get information about cigarettes and alcohol into the communities effectively, but we cannot seem to get messaging about important health information?” She also called for health care organizations to be more thoughtful about reaching out into their communities and abandon the attitude of “build it and they will come,” which is not happening. There is also a need to identify the barriers that are preventing individuals from engaging with the health care system and develop approaches and resources to care for them. The key, in Robinson-Lane’s view, will be to be intentional about developing relationships with the community, which she believes will lead to more sustainable and inclusive programs.
Christensen stressed the importance of delivering services through a patient-centered medical home, which is an added challenge in Indian Country, particularly for people with cancer, because IHS facilities typically refer individuals to academic centers in bigger cities. Putting together a plan for accessing services at the local level is critical in those situations, as is providing the means for patients or family members to get answers immediately about available resources and how to access them.
Responding to a question about plans to disseminate the national strategy, Link explained that after ACL delivers that to Congress in the early fall, it will convene a joint meeting of the two advisory councils to release the strategy publicly, as it did for the initial reports. ACL will also look broadly
to partners in the aging and disability communities to help with dissemination efforts and with the advocacy community to examine what they can do to advocate for change at the local, state, and federal levels.
Link reiterated that the RAISE Act does not provide ACL with any enforcement authority, and Congress only appropriated $300,000 to implement it. In contrast, the National Alzheimer’s Project Act15 came with appropriations to fund research and programs. The RAISE Act, he said, is more about encouraging agencies and programs to collaborate effectively and eliminate duplication. The goal is also to provide a road map for change and a cohesive set of ideas and actions that states, communities, and other sectors can implement. “I truly believe that this will be the tool for mobilizing activity at multiple levels, as well as a tool for advocates to say this is what we need, and this is how we should be working more effectively,” noted Link.
Oyer commented on the complexity of the multi-caregiver approach, especially when caregivers in the same family have different needs and require different linkages to help. Robinson-Lane suggested that hospice and palliative care organizations may be a model for effectively engaging with families, as they are accustomed to mediating conflicts among family members who have different ideas about what the end of life should be. One approach to consider, she said, is to involve the family in decisions about goals of care and planning early in the process. Talking about goals of care in a family setting changes the dynamic, moving it from a strictly medically focused conversation to a more thoughtful one that helps create a plan that takes into account the needs of patients, caregivers, and family members.
Christensen agreed that it is best to approach caregiving as a family, set ground rules and goals, identify a spokesperson, and hold periodic conversations, since the caregiving approach is fluid as the needs of care change with advancing illness. She has found that involving palliative care specialists, clinicians, community health workers, or other local service providers in these regular, recurring conversations has been successful in creating a strong family plan and can be a crucial anchor throughout.
Link observed that it is important to handle family disagreements delicately and tap into the strengths that each individual can bring to the caregiving dynamic. One family member, for example, might be better
___________________
15 For more information see: https://www.nia.nih.gov/about/nia-and-national-plan-address-alzheimers-disease and https://aspe.hhs.gov/collaborations-committees-advisory-groups/napa (accessed October 12, 2022).
suited to handle financial matters, while another may better handle chores. A comprehensive, evidence-informed caregiver assessment involving the entire family, particularly when coupled with care navigation services or case management, can help eliminate potential discord and infighting. A multipronged approach is important because each member of the caregiving team approaches an identical situation with different ideas, fears, strengths, and biases, and it is critical to acknowledge that reality if care is to be truly family centered.
In closing, Bynum emphasized that ACL needs collaborators from the caregiving community to help implement its national strategy, which is only a starting point. She emphasized that reaching the finish line will require action from communities, health systems, health care payers, and others.
UNDERSTANDING THE NEEDS OF FAMILY CAREGIVERS
Jennifer Ballentine, executive director of the CSU Shiley Haynes Institute for Palliative Care, introduced the second session by noting that it would focus on the diverse needs of family caregivers through stories shared by speakers that identified a specific need and proposed a solution. Rebecca Kirch, executive vice president for healthcare quality and value at the National Patient Advocate Foundation (NPAF), explained that her caregiving experience started in the mid-2000s when her brother was diagnosed with lung cancer that had metastasized to the brain. This experience was difficult because the oncology team was eager to push “everything they had,” even though it was clear that he did not have much time to live and did not want to spend what little he had left undergoing debilitating chemotherapy and radiation. Kirch and her family were confronted with the challenge of honoring her brother’s desire to go to the beach one last time. “We got him there, but it was tricky, and we did not have the support we needed from the health system,” said Kirch, who noted that regimented clinical treatment schedules do not offer the flexibility that families or caregivers often need as they are caring for their loved ones.
Kirch explained that experience taught her to stand her ground, a lesson she applied when her mother was diagnosed several years later with amyotrophic lateral sclerosis (ALS). The family focused on palliative care to ensure that her mother’s life would be as enriching and engaged as possible. Currently, Kirch is the primary caregiver for her husband, who has a neurological condition of unknown origin. The combined stresses of caring for him and their two young children led to significant difficulty sleeping
and eating. Kirch shared that community, including the members of the Roundtable on Quality Care for People with Serious Illness, supported her when she had her first panic attack. “Community is the key that makes up for system gaps,” she said.
Cathy Bradley, professor and associate dean for research at the Colorado School of Public Health, University of Colorado at Denver, and deputy director of the University of Colorado Comprehensive Cancer Center, said that as a health economist, her research interest lies at the intersection between work and health and the tradeoffs that individuals and caregivers have to make when faced with serious illness. She related an experience of a participant in a study she was conducting. The individual was diagnosed with aggressive breast cancer within months of giving birth to her second child. She had been the family’s primary wage earner. Her husband had finally been promoted into a position that he had worked hard to attain. He wanted to maintain that job and its income and health insurance yet also care for his wife and their two young children. Bradley noted that this story underscores the need to develop a business case for employers to keep caregivers in their jobs. She pointed out that although that has become true for disabled individuals and is becoming more common for young parents after childbirth, workforce support for all types of caregivers is not a reality.
Wendy Lichtenthal, associate attending psychologist and director of the bereavement clinic in the Department of Psychiatry and Behavioral Sciences at Memorial Sloan Kettering Cancer Center, shared the story of a young couple with three children. While nursing their youngest, the woman found a lump in her breast; within a month, she was diagnosed with breast cancer with local metastases. The husband immediately became her physical and emotional support in the face of debilitating lymphedema and nerve pain, which made it impossible for her to even carry their infant.
When the COVID-19 pandemic closed the school where her husband taught, he had to teach remotely while also caring for his own children and his wife, who was undergoing chemotherapy. One evening, after a treatment, his wife said she was not feeling well. He could see that something was wrong but could not decide if he should take her to the emergency department, which would require finding a caretaker for the children and possibly expose her to the COVID-19 virus. He suggested that his wife lie down, and they would revisit the situation in the morning.
The woman never woke up. The grieving husband was full of regret about his decision. Riddled with guilt, he eventually contacted his local hospital to see what kind of support was available. He attended its bereavement
group, but it was only much older bereaved spouses, none with dependent children, and he left feeling more alone than ever. He turned to the list of therapists the hospital had given him, but due to the pandemic and resulting mental health crisis, only one of the 11 he called had time for him, and that therapist did not specialize in bereavement therapy.
This story provides important context for the need for continuity of care for caregivers into bereavement, Lichtenthal observed. She explained that the bereavement experience is often directly related to the caregiving experience because guilt and regret are the norm rather than the exception. Thus, she said, bereavement-conscious training is needed for medical staff, and health systems need to invest in personnel dedicated to screening and triaging evidence-based care for bereaved caregivers. “There is talk about family-centered care, and what family-centered care is doing is fostering an attachment and a dependence on the health care system, so it is the responsibility of the health care system to continue that care for caregivers and not abandon them,” stressed Lichtenthal. “It is really a moral imperative.”
Dannell Shu, a member of the Pediatric Palliative Care National Task Force and Minnesota Department of Health’s Palliative Care Advisory Council, explained that she was the caregiver for her son, who was born with severe brain damage and not expected to live for more than a few hours or days. While he was in the neonatal intensive care unit, she and her husband received a palliative care consult, which led to sustained palliative care services that allowed them to transition their son to their home. Shu shared that their goal was to bring him home, regardless of how long or short his life would be. Shu explained that their palliative care team taught them how to care for their son and make medical decisions for him based on their values. She added that palliative care freed her, as the mother and primary caregiver, to navigate the hundreds of clinic visits with more than 15 specialists and arrange for caregivers to help her at home.
Shu and her husband set up an intensive care unit (ICU) at their home, and Shu’s husband had to take on additional jobs to make ends meet. They quickly learned that running an ICU requires more than one person; fortunately, Shu’s mother was able to move to Minnesota to help. Importantly, they were able to obtain medical assistance through Minnesota’s Medicaid program, which allowed them to hire paid caregivers. Recruiting, hiring, and training them, most of whom had no experience with a medically complex child, became a new job for Shu. She explained that they were able to apply for a Medicaid waiver that provides additional supports for medically complex individuals, which enabled them to receive consumer-directed
community support to meet their son’s medical needs. More than 90 percent of that paid for caregivers. The waiver budget enables a family caregiver to be paid 40 hours a week. Though the $17/hour did not cover all their needs, it did allow Shu’s husband to only work one job (rather than multiple jobs) and to give more focused time and attention to caring for their son.
Against the backdrop of these personal caregiving stories, Alexandra Drane, cofounder and chief executive officer of ARCHANGELS, presented the Caregiver Intensity Index,16 a tool designed to assess a caregiver’s intensity level by asking a wide range of questions that relate to
- the unpredictable nature of caregiving
- disagreements with family members about sharing the caregiving burden
- feeling underprepared for most situations they encounter as a caregiver
- feeling overwhelmed by caregiving demands
- feeling depressed
- feeling manipulated by the person one is caring for
- having someone to turn to for support
- the financial impacts of caregiving
Drane explained that the tool not only helps to validate the stressful experience of caregiving but also provides caregivers with a common language with family, friends, coworkers, and neighbors.
Discussion
Ballentine opened the discussion session by asking the panelists about the business case for employers to provide caregiving supports, such as leave. In response, Bradley pointed out that it costs a company about three times an employee’s annual salary to replace them. Fifty percent of caregivers work 35 hours a week or more, forcing them to balance caregiving and work. In her view, the business case starts with getting employers to see that caregivers are not a burden and then enabling a conversation around flexibility. While the Americans with Disabilities Act requires employers to accommodate people who are sick, with cancer mentioned specifically, caregivers are not afforded the same accommodations. Bradley observed that
___________________
16 For more information see: https://www.archangels.me/ (accessed September 28, 2022).
her research on cancer patients has revealed work flexibility to be the single most important accommodation, and she imagines that caregivers would benefit in the same way.
Drane cited data from surveys conducted in late 2020 to early 2021, which found that 43 percent of the more than 10,000 adult respondents identified as parents of children, caregivers of adults, or both (Czeisler et al., 2021b). Drane noted that the survey data also revealed that in the early stages of the COVID pandemic, caregivers of adults reported a higher levels of mental distress than other adults did (Czeisler et al., 2021b). The data indicate that 70 percent of these caregivers are struggling with at least one significant mental health condition, such as anxiety, depression, COVID-related stress, trauma- and stress-related disorders, or suicidal ideation (Czeisler et al., 2021a). Drane added that nearly a quarter of U.S. adults are now the “sandwich generation”: they are caring for both children and parents, and approximately 85 percent of them are struggling with a significant mental health impact (Czeisler et al., 2021b).
Drane noted that prior to the pandemic, 8 percent of the individuals who used the Caregiver Intensity Index (CII) tool were “in the red”—experiencing the most stress with the least support; that tripled to 24 percent during the pandemic, where it held steady for 20 months (Czeisler et al., 2021b; The National Alliance for Caregiving, 2020). Drane reported that 29 percent of individuals who used the CII were currently in the red, due to the pressures of inflation, global unrest, and other factors (Czeisler et al, 2021b). Drane emphasized that this translates to a greater than 90 percent risk of at least one significant mental health impact, underscoring that caregiving is about mental health, which is part of the business case for providing caregiver support (Czeisler et al., 2021b).
Another economic argument for supporting caregivers, added Lichtenthal, is “presenteeism” (people returning to work who are not functioning at full capacity). Bradley emphasized that it is important to remember that despite a compelling business case for supporting workers who are caregivers, there is also a moral imperative to do the right thing.
Caregivers also develop unique skillsets that can save the health care system money. Kirch pointed out that Minnesota’s caregiver support policy likely has a significant return in the form of savings to the state and health care system. Bradley called for Minnesota’s waiver policy to be systematized nationally. She noted that during the pandemic, the state allowed family caregivers to be paid for more than 40 hours a week, a recognition of the scope of the caregiver shortage.
When asked to discuss the resources that helped Shu and her husband, Shu said that connecting with parents and others in a similar situation is important. While organizations such as the national Courageous Parents Network17 did not exist when her son was born, it is now a critical support system. Shu pointed out that it was other parents, not anyone in the health system, who alerted her to the waiver program,18 and that the state’s consumer-directed community support system provides trained and paid community connectors to help families write the plan required to secure a waiver. Another valuable connection, said Shu, was with a public health nurse who pointed her to resources and people in the community.
Kirch emphasized that palliative care is a critical resource, as is families learning from families. Navigators can also be a good resource to connect caregivers to services. NPAF provides support over the phone, but philanthropic provision of these services will not address all of the nation’s needs. Rather, strategies need to be developed to integrate social and financial needs navigation into the health system.
Drane commented that many caregivers are not aware that they are in that role, and this is particularly true of people who are most at risk, including those in rural, Black, Latinx, Hispanic, younger, and essential worker populations. Rather, they view themselves as being a good family member, a friend, or someone who cares. Drane also shared that a physician whom she met after giving a presentation did not realize he was a caregiver and could benefit from bereavement support, even though he and his wife were caring for two children under five and also his father and mother-in-law, both of whom died from COVID. Drane noted that because people do not see themselves in the caregiver role, they may not take advantage of available employee-assistance programs.
Ballentine, commenting about the need to start addressing grief among family members at the time of diagnosis and not just toward the end of life, asked the panelists for their ideas on how to make care more bereavement conscious. Lichtenthal replied that at the threat of loss, the grief process begins. However, anticipatory grief is different from the losses that happen along the way that also cause grief. Grief and the related separation distress response, she said, are about not wanting to lose someone, and that triggers
___________________
17 For more information, see https://courageousparentsnetwork.org/ (accessed July 18, 2022).
18 See https://mn.gov/dhs/people-we-serve/people-with-disabilities/services/home-community/programs-and-services/cadi-waiver.jsp (accessed February 15, 2023).
a desire to protest that loss, which affects decision making. “Bereavement consciousness for the health care system is a mindfulness of what is coming up that is actually grief,” she explained.
While many might recognize on an intellectual level that discontinuing curative treatment, for example, might be reasonable and reduce suffering in the long term, such awareness is overpowered by the separation distress response. It is important, said Lichtenthal, for providers to recognize the role grief and fear of loss play in decision making. Providers also need to be conscious of what a family is going to carry forward into bereavement; they are always going to wonder if they could have done more. Kirch, taking that idea one step further, said it is also important for clinicians to recognize anticipatory grief in themselves and the role it might play in their decision-making process regarding the desire to continue treating a patient when the family and patient are ready to move to palliative care and hospice.
Ballentine suggested that the clinician’s office is the place to lay the groundwork for patient- and family-centered care, which involves keeping caregivers informed about the care they will need to provide and emphasizing the need to care for themselves. Stressing the importance of viewing the patient and family as the unit of care, Lichtenthal commented that an investment in resources is needed to support caregivers from the time of diagnosis, including training clinical staff how to discuss such matters in a way that empowers people and engages in regret prevention. Shu added that it would help caregivers if they attended every appointment, if only to make sure they are hearing the same information as the patient in terms of care needs, which would also enable them to discuss the care plan directly with the provider.
Drane said her organization conducted a study that found that 80 percent of a large panel of health care providers believe that caregivers should be present during patient visits and be engaged in care plan discussions (Shah and Drane, 2021). However, when asked if they actually engage caregivers, only 20 percent of the health care providers said they do (Shah and Drane, 2021). Drane explained that she and her colleagues strategize about ways to ensure caregivers are at the table when care plans are developed and discussed.
One approach to elevating the role would be to include it on each caregiver’s resume, suggested Drane. This formal recognition of unpaid caregiving as work would underscore that the individual is building a new skillset that is of value to potential employers. Drane recommended that caregivers visit the ARCHANGELS website to be reminded of the job skills
they have developed. “You know how to problem solve. You are a product manager. You get things done under tight time constraints that everyone else has said is impossible,” said Drane. Bradley added that standing behind and supporting caregivers can generate a tremendous amount of loyalty to the company.
Insurance companies should also recognize the value of caregivers because they are the best in-network providers possible, said Kirch. “The cost-sharing we do is completely unquantified, but it is a big boon for the insurance plan business,” Kirch emphasized. She asked why the insurance industry could not develop a benefit, such as credit toward a deductible or the out-of-pocket limits. Kirch called for businesses to demand that insurance companies involve caregivers in benefit design to address some of these challenges. Ballentine suggested offering family caregiving insurance, similar to long-term care insurance.
Ballentine then asked the panelists for their ideas on how to support the needs and concerns of long-distance caregivers. Shu suggested identifying specific ways that extended family members can be involved even from afar. Kirch said she faces this problem with her father, who lives hours away, and she cannot leave home for long because she has to manage in-home dialysis for her husband 6 days a week. Her best friend, who lives in the same town as her father, checked on him. Then her friend connected her with community resources that conducted a geriatric assessment in his home, where he wanted to stay. Kirch was able to find what she called an “underground of caregivers,” which was critical given the lack of any established system. This gap exists across the nation and needs to be addressed, she emphasized.
Bradley said she finds it ironic that large- and medium-sized employers are competing with each other on worker well-being programs but have no plan for when someone actually gets sick or becomes a caregiver. Small employers, she added, are not subject to the requirements of the Families with Medical Leave Act or the Americans with Disabilities Act, so no protections are in place for those employees. “There needs to be a cultural change as to how we treat people who are providing care for others, because it is such a vital part of our economy,” said Bradley. Drane added that retention and recruitment challenges are reasons why more human resources departments are starting to pay attention to the notion of supporting caregivers.
An audience member questioned whether expecting U.S. businesses and federal and state governments to support caregivers is the best approach. Bradley replied that no one action is going to solve this problem,
and making the business or social needs case is only part of the solution. Bradley reiterated that supporting caregivers should be valued from a cultural perspective. Lichtenthal added that the universality of caregiving is something to capitalize on when talking to people in power who will likely experience this on a personal level eventually. Ballentine noted the great deal of rhetoric around the importance of keeping families intact and families being the foundation of society, so an argument can be made that this is about supporting families and allowing them to stay together. A workshop participant suggested that a useful way to think about caregiving would be to recognize that it is an essential component of delivering health and medical care services and supports.
Drane noted that one issue not raised in the discussion is the presumption that people are able to, equipped for, and are ready and wanting to take on caregiving responsibilities. Drane used the example of “Hospital at Home,” suggesting that hospitals use a new “checklist” in determining whether a potential caregiver is a good fit for taking on the responsibilities. This would include someone taking that person into a separate room and explaining in detail what caregiving at home would entail. It is important that the person is enabled and empowered to make an informed choice about whether it is a role that they are willing and able to accept.
In closing, Ballentine commented that stories can persuade, and the stories shared during the session are so powerful and relatable that they can underpin future policy discussions and decisions.
PROVIDING EFFECTIVE SUPPORT FOR FAMILY CAREGIVERS
A Dementia-Friendly Program for African American Faith Communities and Families Living with Dementia
Fayron Epps, assistant professor at Emory University’s Nell Hodgson Woodruff School of Nursing, opened the third session, which focused on exemplars of caregiver support programs. Epps described Alter, a faith-based community program. Epps and her colleagues launched Alter in 2019 to encourage culture change, shift perceptions about dementia, and strengthen support services within and in partnership with African American churches (Epps et al., 2019, 2020a, 2021, 2022; Gore et al., 2022).19 Epps pointed out that Alzheimer’s disease and other dementias are the fourth leading
___________________
19 Additional information is available at https://alterdementia.com (accessed June 9, 2022).
cause of death among older African Americans.20 The idea for Alter arose after she and her colleagues identified a huge need to expand awareness about dementia and address the social isolation that it entails coupled with the importance of religion to the well-being of older African Americans living with dementia (Epps and Williams, 2020).
In meeting with the pastors, Epps found that many of them did not realize the extent of the problems dementia was causing in their congregations and communities. Alter staff also found that they needed to work with faith leaders to send the message that family members and their caregivers are welcome, supported, and accepted by the congregation, whatever their burdens might be. The ultimate goal for Alter, said Epps, is to preserve access to church—and the social support it provides—for families living with dementia.
Alter provides training sessions, materials, and videos for church leaders and in-person and virtual support for members with dementia and their families when they need additional help or have questions that the leaders cannot answer. Epps and her colleagues also hold education sessions for an entire congregation to help them become more aware of the needs of those with dementia and the people who care for them while providing tools and techniques for addressing the cultural taboos associated with dementia. Epps said that she always asks the churchgoers if they want to be part of a trailblazing dementia-friendly community; they may not see the need immediately, but she and her colleagues gently persist in introducing the program and talking about how important it is for the broader community.
Epps explained that Alter’s partnerships with churches come with a 2-year commitment and a memorandum of understanding that drives home what the churches are committing to do. Once a church joins the Alter community, it receives a welcome kit with brochures and materials for church members and a financial contribution to ensure that it can implement the program. Epps and her colleagues then ask the churches to carry out eight core activities (Box 2) and eight additional activities around education, support, and worship that the churches can customize. An education activity, for example, might be holding Memory Sunday, a yearlong collaboration between faith communities and health and community organizations focused on raising awareness about memory loss, aging, and Alzheimer’s disease in the African American community that culminates
___________________
20 See https://www.usagainstalzheimers.org/health-disparities-race-and-alzheimers (accessed August 16, 2022).
in an event on the second Sunday in June.21 A support activity might be organizing a Memory Café, forming a dementia support group or respite program, or establishing a resource library. Creating visual aids and adjusting the length of the service are examples of worship activities (Epps et al., 2020b). Epps noted that after 2 years, Alter revisits whether a church wants to remain part of the initiative; if so, it becomes a legacy partner.
Epps noted that Alter has formed partnerships with 21 churches in Georgia, two in Illinois, and one in Florida over a 2-year period. Alter’s website has a function that allows families to locate an Alter church close to their home.
The next step, Epps explained, is to find partners with other faith communities. Epps noted that Alter is part of the Health Resources and Services Administration’s Geriatrics Workforce Enhancement Program,22 and she is
___________________
21 Additional information is available at https://www.nia.nih.gov/research/alzheimers-dementia-outreach-recruitment-engagement-resources/memory-sunday-toolkit (accessed September 28, 2022).
22 For more information on the Geriatric Workforce Enhancement Program, see https://www.hrsa.gov/grants/find-funding/hrsa-19-008 (accessed August 4, 2022).
looking to work with more churches around the country. So far, she has partnered with ones in Minnesota and Virginia and is in discussions with one in Arkansas. “We are trying to expand and create an infrastructure to be able to support Black churches as we address family caregivers that are supporting those living with dementia,” said Epps.
Malcoma Brown-Ekeogu, a member of Alter’s advisory committee, is a caregiver for her husband who has the behavioral variant of frontal temporal degeneration. This condition causes him to yell out inappropriate things or touch people inappropriately. Before joining Alter, Brown-Ekeogu and her husband had stopped attending church because of those behaviors, and she felt lost in terms of how to continue to maintain connections with the community. Once Brown-Ekeogu became involved with Alter and started taking part in different focus groups, she began sharing her experiences—peeling the Band-Aid off the sores in her life and sharing them, as she put it—so that she might make things better for other care partners23 experiencing the same problem. Doing that, she said, helped her grow and become a better care partner herself.
Brown-Ekeogu noted that someone from Alter attended the first session with her to see how things went. The sermons are only 10–15 minutes long, which is just long enough to keep her husband engaged. Initially, she said, he did not participate, but the second time, he clapped his hands to one of the songs and said “Amen” at the end of prayers. Brown-Ekeogu said that on days when she feels blue, she rewatches the program videos on YouTube to refresh herself. She said that her view on the benefits of the Alter program is that with unity comes strength.
A Clinical Service Dedicated to Supporting Cancer Caregivers
Allison Applebaum, associate attending psychologist and director of the Caregivers Clinic at Memorial Sloan Kettering (MSK) Cancer Center, opened her remarks noting that when she arrived in 2010 as a postdoctoral fellow, she recognized a vast unmet need for psychosocial support for cancer caregivers. MSK offered, for example, a once-a-month drop-in group, which was the norm for comprehensive cancer centers nationwide. However, a large body of research indicated that caregivers desired support focused on their own unique psychosocial needs—support they were not receiving—in addition to the supportive services offered regarding care for their loved ones.
___________________
23 The speaker used the term care partner rather than caregiver throughout her remarks.
In response to these needs, Applebaum established the Caregivers Clinic, alongside the cancer center’s Family Therapy Clinic and Bereavement Clinic, as part of the MSK Family Care Program (Figure 1). The Caregivers Clinic strives to assure that no caregiver or family experiencing significant distress as a result of their role goes unidentified and deprived of necessary psychosocial services. It provides care that encompasses the entire journey from diagnosis through bereavement. Applebaum noted that many caregivers come in because they have significant symptoms of anxiety, depression, and, increasingly, post-traumatic distress disorder (PTSD). Many also find it difficult to speak with their loved ones and the health care team about advance care planning, what to expect, and how to plan, so in addition to education and support through various psychotherapeutic approaches, the clinic offers communication skills training. Inevitably, many caregivers also have concerns related to existential distress, which Applebaum pointed out, we all experience when we connect to our—and our loved ones’—mortality.
The Caregivers Clinic began in November 2011 and, by November 2021, had 222 referrals from the MSK Department of Psychiatry and Behavioral Sciences and another 515 referrals from other MSK departments, according to Applebaum. Those referrals led to 408 psycho-diagnostic visits that turned into over 4,000 follow-up psychotherapy sessions and 144 caregivers requesting or requiring medication management. The clinic has con-
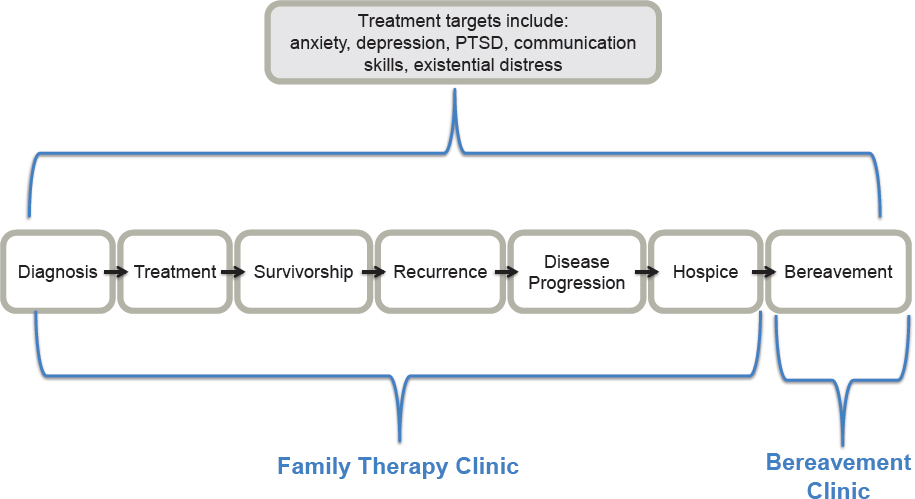
SOURCE: Adapted from Applebaum presentation, May 16, 2022.
ducted three ad hoc group sessions for 98 couples and families focusing on a specific concern, such as how to talk about the future with a family member.
Applebaum and her colleagues advocated that caregivers should register as patients at MSK so that they would have their own medical record. For Applebaum, documenting caregiver data in a medical record should be part of the standard of care (Applebaum et al., 2021). At the diagnostic visit, caregivers receive an ICD-10 diagnostic code that is entered into the medical record and used to bill for services. The clinic bills all of its services to insurance carriers except when caregivers come in for follow-up care with the program’s fellows, which is free. Since March 2020, the clinic has held its sessions via telepsychiatry, and they are paced to meet caregiver needs. “The reality is some caregivers come to us with intense distress and in need of ongoing care, and others come to us purely to learn how to communicate with their loves ones,” said Applebaum. This is something they can achieve with a small number of sessions, she added. Sessions rely heavily on empirically supported interventions, such as cognitive behavioral therapy.
Applebaum pointed out that the clinic is dealing with extraordinary demand amplified by the COVID-19 pandemic. Challenges have arisen because of long wait times for care and infrequent sessions. The clinic supplements care from its attending physicians by involving externs, interns, and fellows. It also refers caregivers on the wait list to clinical trials designed to test psychotherapy interventions tailored specifically to caregivers’ needs. The clinic also developed a Caregiver-to-Caregiver mentoring program that pairs caregiving experts—individuals who are no longer in the role or bereaved at least 1 year—with current caregivers to provide ad hoc support that is both free and offered with greater flexibility in scheduling.
The cost of care is an important concern, particularly when someone has insurance that does not include mental health coverage. Applebaum and her colleagues refer those caregivers to program fellows, who provide free care. Another challenge arises when patients come from places outside of New York and New Jersey, where she and her colleagues are licensed to practice. “I, as a licensed psychologist in New Jersey and New York, cannot provide care to a patient of mine if they go home to Ohio or Pennsylvania,” she said. During the pandemic, they received temporary licenses to treat patients from out of the area, but that flexibility is ending. Now, she said, she and her colleagues refer those patients to social workers and community-based organizations.
Applebaum identified the switch to telemedicine as a silver lining to the COVID-19 pandemic. It addressed many historic barriers to psycho-
social service use among caregivers; the number of no-shows dropped precipitously. However, it has created a new challenge in meeting the soaring demand.
Applebaum says the clinic can improve distress screening to identify caregivers who truly need its supportive services in contrast to those who are distressed due to other reasons, such as financial concerns, and would benefit more from speaking with patient financial services. The clinic is also piloting the CancerSupportSource-Caregivers tool (Zaleta et al., 2021), an automated, online screening tool that Applebaum believes will be effective in helping triage caregivers to the appropriate level of care. She would also like to see the hospital do a better job of identifying caregivers when patients first come for care, creating a medical record immediately, and conducting early and repeated distress screening assessments, especially at transition points in patients’ care. Applebaum concluded her remarks by noting that expanding peer support through the Caregiver-to-Caregiver mentoring program is also on her wish list.
Peter Gee, a nursing student at New York University School of Nursing and caregiver for his husband, who was diagnosed with glioblastoma in November 2018 and passed away in June 2020, credits MSK with providing the best, most comprehensive, and holistic support for him and his husband. Gee explained that when his husband was first diagnosed, he wanted to put every effort into what he thought was “the right thing to do” for someone with terminal cancer. He began weekly therapy sessions and convinced his husband to try it, too. After several sessions, Gee’s husband declared that it was not helpful and stopped. Gee also stopped going, because it was taking up too much of his time, which included working and supporting his husband in his treatment plan. “I remember thinking back at the time how exhausting it was to have to explain the logistics of brain cancer to my very well-intentioned therapist,” said Gee. “The sessions also felt so open ended, which at the time was not what I needed.”
Gee shared that during their cancer journey, he learned that the patient and caregiver can respond differently to the diagnosis. His husband, for example, remained optimistic that he would be among the 5 percent of glioblastoma patients who survive to year 5. Gee, on the other hand, experienced anticipatory grief every moment of his day. Six months in, his husband’s oncologist informed them that the original tumor had become two. Nonetheless, his husband remained optimistic while Gee, in his words, “started losing it.” Fortunately, the neuro-oncologist and nurse noticed his visual cues and pulled Gee into a separate room where he could
break down in private and not affect his husband’s optimistic outlook. It was then that he learned about the caregivers clinic, which connected him quickly to a psychotherapy trial for caregivers that tested a process called meaning-centered psychotherapy (MCP). MCP focuses on helping patients and caregivers connect to sense, meaning, and purpose despite the unique and complementary challenges they face (Breitbart et al., 2018).
Gee found the eight MCP sessions transformative, and he asked if his husband could join in. Gee recalled how important it was for both of them to explore their identities before, during, and after cancer. MCP also gave them a shared language they used to communicate better with each other. “Debriefing with one another about each session was not only healing but was a starting point for our own conversations as a couple,” said Gee. For example, the sessions made Gee think about what he would do after his husband died; in one session, he thought about shifting careers from human resources into nursing. Gee shared this idea with his husband, who asked why he did not start nursing school immediately. Nearly 2 years after his husband’s death, Gee is halfway through an accelerated undergraduate nursing program.
Gee shared that a key lesson he learned is that seamless integration between primary and behavioral health providers, nurses, and social workers is the exception, not the norm, even though it leads to better patient outcomes. “If the medical team had ignored me and did not connect me to the caregivers clinic and the MCP trial, I would be experiencing grief and widowhood very differently,” he said. Gee now volunteers to be a mentor in the caregiver-to-caregiver program, which has reminded him that there is no right or wrong way to be a caregiver. Caregivers continue to experience extraordinary distress and need caregiver-specific supports.
Another observation that Gee shared was that the home hospice system is broken. “We did 8 weeks of home hospice, and because it was during the first wave of COVID-19, we lost all of our community support,” said Gee. “It really is unacceptable that we leave it up to families and loved ones to do this on their own.” In Gee’s view, ways of providing financial support to family caregivers need to be developed along with ways to expand access to home health aides. Gee also proposed that a death doula should be part of the standard of care.
Gee’s final observation was even though he and his husband had supportive employers and excellent health care insurance, knew how to advocate, and were legally married, the logistics of living and dying with brain cancer were “beyond overwhelming.” Gee said that a quote from
Vaclav Havel, former president of the Czech Republic, helped sustain them during their cancer journey. “He said that hope is definitely not the same thing as optimism. Hope is not the conviction that something will turn out, but the certainty that something makes sense regardless of how it turns out. I had mistakenly misunderstood the hope that Jeff expressed at the beginning of our cancer journey,” said Gee. He and his husband felt as if they were passengers along for a ride on a turbulent roller coaster, but the programs they participated in put them back in control and allowed them to focus on the decisions they could control. “We were able to get clarity on where we stood individually and as a couple, and this allowed us to have better connections with our primary care team, our family, and our friends,” said Gee.
Family Caregiving in Indigenous Communities
Loretta Christensen, the IHS chief medical officer and enrolled member of the Navajo tribe, explained that the mission of IHS is to raise the physical, mental, social, and spiritual health of American Indians and Alaska Natives to the highest level, and its vision is one of healthy communities and quality health care systems through strong partnerships and culturally responsive practices (see Box 3 for an overview of the IHS).
IHS relies on programs such as the Public Health Nursing Program24 for home visits, assessments, and patient evaluations. Some of the nurses speak the Navajo language, for example, and will do home visits; if they do not, they travel with a driver who is fluent in the language of the particular tribe to allow for adequate and accurate communication. Community Health Representative Programs,25 which the tribes typically run, send people into rural areas to conduct assessments, educate and care for families, and arrange for support services for families. For example, the program arranged for deliveries of food and disinfectants during the pandemic.
Given the shortage of food stores, caregivers have to decide whether they are going to spend their time caring for their family or making the long journey to and from the nearest grocery store. They also face the challenge of getting around the reservation, given the high cost of gas and large number of unpaved roads. Christensen noted that when the weather makes the roads impassable, IHS employees will park their car near a
___________________
24 See https://www.usphs.gov/professions/nurse (accessed August 29, 2022).
25 See https://www.ihs.gov/chr/ (accessed August 4, 2022).
major road and walk miles to their client. Because money is often limited, families only buy small amounts of care supplies, which requires even more long-distance trips.
Another key challenge is the lack of access to cancer care (Guadagnolo et al., 2017). Typically, patients must travel to urban or suburban areas, and often family members cannot afford to accompany them. This not only deprives the patient of the support they need but prevents family members from hearing instructions from and asking questions of the health care team. This latter problem is compounded because these distant facilities often do not have a level of cultural sensitivity and appropriateness to discuss cancer and care in a way that a tribal member can understand. Christensen added that members of different tribes can have a different understanding about cancer in general, making it important to customize information delivery. “Sometimes, it is not just one size fits all in Indian Country,” said Christensen.
IHS works with partners from some tribal organizations to define the needs in Indian Country. Given that the majority of caregivers are family members, it is important to get feedback from the caregivers as to what they need, what frightens them, and how IHS can support them. One goal is to provide education and resources and to include the caregivers in each step of the care planning process by having as many family members at clinic or home visits as possible. Another goal is to enhance the scope of work for public health nursing, community health representatives, lifestyle coaches, and navigators to address workforce issues in the coming years, given the shortage of nurses. The idea is to get as much work done in the communities so that every patient does not need to travel to a facility. This effort includes bringing cancer resources near tribal communities, getting doctors to spend time in Indian Country, or enhancing telehealth capabilities.
At the heart of the IHS family caregiving strategy is ensuring that the diverse needs of Indigenous communities are included. IHS wants to develop reliable, sustainable support systems for family caregivers and increase its work with partners to provide information and educate tribal communities about family caregiving. Christensen’s team is also holding discussions regarding data collection and analysis, to get a better understanding of the challenges, and looking at caregiving and multidisciplinary teams, to see how they can fit into the patient-centered medical home. Christensen noted that IHS is rolling out a new system of primary care that will include more support for this work, and it will combine behavioral health, substance misuse screening, and social work into one visit.
Elton Becenti, Jr., a member of the Navajo Nation and field engineer for IHS who lives in Crownpoint, NM, a larger town on the Navajo reservation, described his family’s experience with cancer and caregiving. Becenti explained that while Crownpoint has a full-service IHS facility, patients have to travel 60 miles to the New Mexico Cancer Center in Albuquerque.
Becenti’s journey with caregiving began in 1999 when he was 16 and his mother, who was going through a divorce, was diagnosed with colon cancer. IHS did not provide support services at the small Crownpoint facility. He took on as many responsibilities as he could, including cooking, cleaning, and taking care of his younger brother. Becenti identified the lack of empathy from his mother’s main oncologist as a key challenge, noting it was difficult to process all the medical information.
Eight years after his mother died, Becenti’s father was also diagnosed with colon cancer. By then, the cancer center had opened in Gallup. It was an hour away but half the distance that his mother had to travel for treatment. IHS caregiver support services were limited, and once again, he lacked resources for how to cope with and relieve the stress of being the primary caregiver. The cancer center offered some counseling; the staff, including the oncologist, were helpful, caring, and understanding, unlike his earlier experience. In addition, the primary care physician at the Crownpoint facility was kind and compassionate, which made a world of difference. Nonetheless, he had days when he felt he was battling cancer more than his father was and had many months of little to no sleep. Becenti’s father also ultimately passed away.
Based on these two experiences, Becenti recommended improving care in rural areas by having respite care, a team to relieve the caregiver for a day so they can take a break, and someone who could deliver meals a few times a week. He also suggested that virtual technologies, such as Zoom, and telehealth services could provide the caregiver with a virtual team that could check in on them and the patient and provide more support. He added that teams could help educate both patients and caregivers about their treatment regimens, the side effects they experience, and medicines that could relieve those side effects. Lacking such support, Becenti shared that he had to educate himself by finding information online, such as on the M.D. Anderson Cancer Center and Colon Cancer Care Alliance websites.
ACCA’s Advanced Illness Care Program
Janice Bell, associate dean for research and professor at the University of California at Davis Betty Irene Moore School of Nursing, explained that
the Alameda County Care Alliance (ACCA)26 is unique in that, unlike other programs for people with serious illness, which often start within academia or within a health system and then reach out to the community, ACCA started within the African American faith community and built partnerships on that base. She pointed out that because about 87 percent of African Americans are actively involved in organized religion,27 the church has excellent potential to educate and empower and has been doing so for hundreds of years. It also has the advantage of being a trusted source in the community (Harmon et al., 2014).
From its beginning in five churches in 2013, ACCA brought together members of the health, public health, philanthropic, and academic communities with the goal of advancing equity for people with serious illness and their family caregivers. Kaiser Permanente, through its community benefits program, was the original funder and continues to support the program, while Bell’s institution provides technical assistance, and intervention development, training, and evaluation support. The Public Health Institute provides project management and acts as the fiscal sponsor. ACCA launched its pilot program in 2014 and has grown to include 42 churches. Bell noted that the California Health Care Foundation is currently funding a feasibility pilot project to understand the needs for establishing an ACCA hub in the Los Angeles area.
The Advanced Illness Care Program (AICP),28 a lay care navigator intervention designed to support people with serious illness and their family caregivers in Alameda County, Contra Costa County, and San Francisco, is the centerpiece of ACCA’s work.29 The church-based AICP systematically addresses five program cornerstones. The first is to address spiritual needs by focusing on spiritual support, meditation and prayer, and support from the faith community. Bell explained that faith is not a requirement; AICP has started receiving referrals from care partners in the community for indi-
___________________
26 For more information on Alameda County Care Alliance, see https://www.care-alliance.org/ (accessed August 4, 2022).
27 See https://www.pewresearch.org/religion/2021/02/16/faith-among-black-Americans/ (accessed August 4, 2022).
28 For more information on the Advanced Illness Care Program, see https://www.care-alliance.org/advanced-illness-care-program-aicp (accessed August 4, 2022).
29 Through a series of 5 to 12 in person meetings and telephone conversations over a period of about 6 months, the Care Navigator helps program participants meet their caregiver needs and links them to resources. https://www.care-alliance.org/advanced-illness-care-program-aicp (accessed August 4, 2022).
viduals who do not identify as having a spiritual or religious inclination. The program does not emphasize this cornerstone for them, though program evaluation data suggest that approximately 85 percent of visits involve prayer.
The second cornerstone, meeting health needs, provides physical and emotional support and tools that help participants prepare for provider visits and communicate their needs. The advance care planning cornerstone helps participants understand, choose, document, and receive the care they prefer. The fourth cornerstone, meeting social needs, involves referrals to resources, such as transportation, meals, housing, and financial or legal support. The final cornerstone, meeting caregiver needs, recognizes and celebrates caregivers, provides them with support, and then works with patients to address their caregiving needs. Bell said that people can join the program as caregivers, as someone with serious illness, or in dyads.
The caregivers in the program are 21–88 years old, with a mean age of 85, Bell noted. More than 80 percent are African American, and 61 percent have an annual household income of less than $50,000. Caregivers themselves average more than one chronic condition, and many of them in time switch roles, becoming participants with serious illness. By the end of the program, 55 percent of the participants have completed advance directives, which Bell noted is astonishing given the much lower completion rate in the African American community nationwide.
Bell explained that the caregiving cornerstone draws on resources such as referrals to in-home support services, respite care, and financial assistance applications, as well as tools specific to the programs. Tools include a goal-setting tool, a worksheet called “Eight Ways to Feel Better,” and a workbook for caregivers that focuses on helping them improve their own self-care, identify the needs of their care recipients, and identify others in their network who can help them. To illustrate how the cornerstones come together, Bell quoted a caregiver who said, “Prior to my mother’s death she [the care navigator] provided comfort. She gave me phone calls. She followed up. She plugged me in with resources…prepared me emotionally by [describing] the process that my mother may have to go through and the decisions I may have to make.”
Bell presented a diagram to highlight the different ways in which ACCA touches people (Figure 2). People enrolled in the program and who typically receive 5–12 visits are in the center, followed by those who may have personal contact with the navigator but do not enroll or enroll and may not finish. Beyond that, ACCA influences church culture and it changes community expectations. Since 2016, ACCA has served over
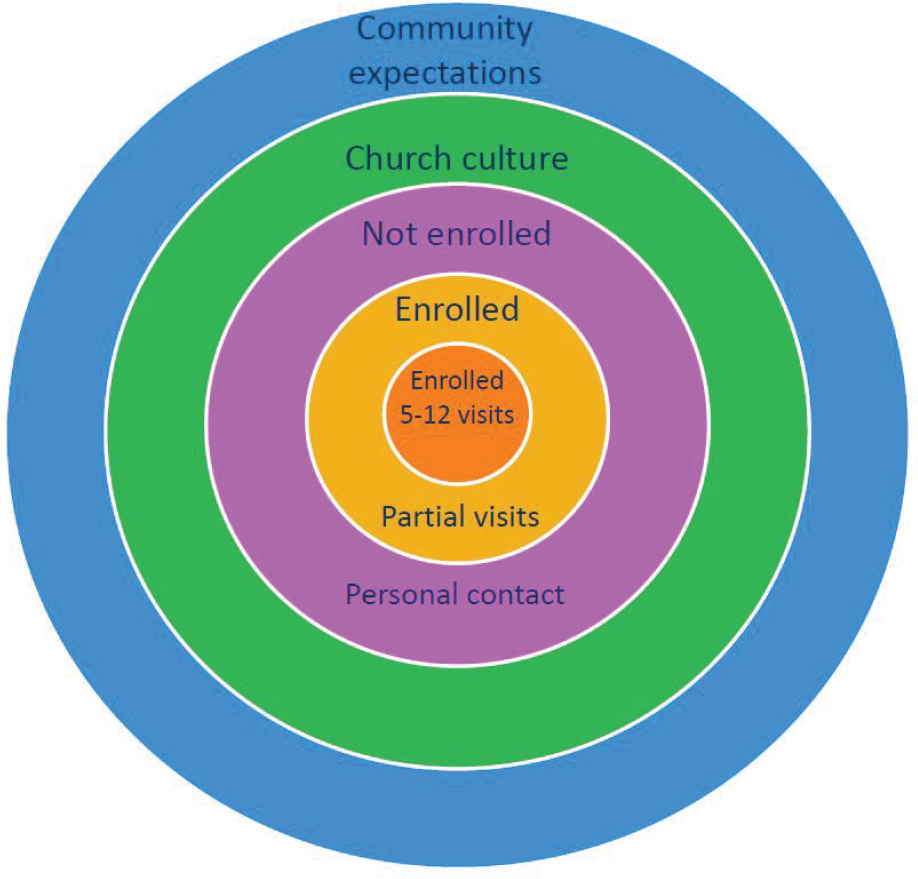
SOURCE: Bell presentation, May 16, 2022.
1,500 participants—those in the center of the diagram—and touched over 16,500 individuals. In 2021–2022, the program served 314 participants and touched 2,052 individuals.30
Since its launch, ACCA has conducted an annual congregation assessment survey, usually around the time of National Health Care Decisions Day in April. The survey was sent to a random sample of people in church on that Sunday in 201931 and shows that about 15 percent of congregants are caring for someone with an advanced illness, with 43 percent of them providing care
___________________
30 See https://www.care-alliance.org/impact (accessed September 7, 2022).
31 See https://static1.squarespace.com/static/60a2e229a24b351d37e9d0d6/t/60dc07af9dac936539fb27e1/1625032623445/CAS-2019-Results-ALL.jpg (accessed September 7, 2022).
7 days a week and 13 percent providing care without a break. The most recent survey revealed that 47 percent of congregants have completed an advance directive—up from 40 percent when the program started—and 24 percent have completed a Physician Orders for Life-Sustaining Treatment form.32
Bell described a number of community-based activities that ACCA is involved in, including an annual caregiver recognition celebration that draws approximately 1,000 people. It includes an awards ceremony and a dinner served by participating pastors. “It is a real opportunity for community to come together including health system partners and philanthropy partners to really celebrate the caregivers,” said Bell. ACCA also sends recognition letters to all known caregivers and hosts the I Choose to Prepare event that focuses on youth in the community and allows them to discuss their thoughts about end-of-life issues.
ACCA’s Choosing to Prepare Pastor Training centers on the documentary short film Extremis, an ICU-based film about decisions required at the end of life. ACCA has developed discussion guides to accompany the film, and it trains pastors and faith leaders to host screenings and community discussions about the topic. ACCA also hosts dinners that invites palliative care physicians to join with pastors to break bread, share a meal, talk about common experiences, and discuss ways of supporting people with serious illness and their family caregivers.
Lyn-Tise Jones, one of ACCA’s lay care navigators and caregiver for her mother, witnessed her tall, committed, and strong mother care for everyone but herself until a cold November night in 2019. “I watched her life exit through her eyes when she was delivered the news of having Stage 4 endometrial cancer,” said Jones. “In that moment, the rug was suddenly pulled from underneath our family, and my mother was in need of being taken care of. Even as I tell the story, it is painfully difficult to recount those difficult moments of her diagnosis.”
Jones left her job as director of a local family resource center to become her mother’s full-time caregiver. She had no idea what to do and felt confused, defeated, and isolated. “She found ACCA to be a sophisticated, loving, and praying group of people. I can truly say that without them I would not have been able to take care of my mother for those 27 months, and even now gaining the support that I get from all of them,” she said.
___________________
32 See Congregational Assessment Survey results at https://static1.squarespace.com/static/60a2e229a24b351d37e9d0d6/t/60dc07af9dac936539fb27e1/1625032623445/CAS-2019-Results-ALL.jpg (accessed September 7, 2022).
The caregiving experience led to her new purpose in life, which is to help as many caregivers as possible. She noted that despite years of formal education and many awards, degrees, and accolades, she was unprepared for becoming a full-time caregiver for her mother and “felt like an ant going against an elephant.” As a care navigator, she began to meet with individuals, which helped her not focus so much on her own circumstances. Yes, it was painful and distressing, she said, but she found she was able to work with individuals, connect with similar stories, and share what she has experienced with her mother as a way of helping other caregivers.
By sharing others’ caregiving stories, Jones explained, she is able to identify participants’ needs and goals and provide trusted referrals and resources. She recalled that few things were more disturbing when she was caring for her mother than walking into a hospital and getting a laundry list of services and phone numbers, the majority of which did not work. Through relationship building and her own research on referrals, she has been able to provide meaningful support to those in need and empower herself and others with the tools and training that ACCA provides. Jones noted that care navigator surveys have shown that the navigators are always able to establish trusting relationships with participants. “It is not so much what you can tell me, but what do you know, what have you been through, what have you experienced,” she said.
Jones shared that a key challenge she experienced as she became more anchored in the program and it was getting more referrals from larger health care systems was how difficult it was to form a relationship with people who were already feeling isolated by the medical institutions where they were receiving care. She explained that when she shares her story about the challenges she faced providing care for her mother when she was hospitalized during the COVID-19 pandemic, some of those reluctant caregivers start bonding with her and suddenly feel that they have someone who understands what they were going through.
Jones noted that empowerment is fundamental to the program because it allows people to understand that they have a choice in their care. She emphasized that building trust for effective community relationships is paramount because trust is essential for people to be fully present and open. Trust has to extend through all the service providers, so it is important to make sure the long-term community partners include champions.
An Academic–Clinical Partnership to Support Family Caregivers
Roger Kirwin shared his experience as the caregiver for his wife, who died of cancer in 2021. Kirwin explained that throughout the nearly 30 years they were married, he and his wife led a somewhat unconventional lifestyle due to his work in the U.S. and U.K. motorcycle industries. They met in 1985 when he was attending a meeting at the Harley-Davidson factory in York, PA; after a 6-year transatlantic romance, they settled in an old village in northwest England and had a second home in Bedford, PA.
When diagnosed with ovarian cancer, his wife elected to receive life-sustaining treatment at Magee-Womens Hospital at UPMC, and they moved in with her brother, who had a home nearby. Kirwin shared that he hoped that her extended family would provide moral support that only relatives can. “Little did I ever think that, as her hair fell out and the weight loss became apparent, these devoted people who flocked to wish her well at the onset of treatment would actually stop coming around to visit, unable to face what was happening to her and no doubt confronting their own mortality by proxy,” said Kirwin.
Over the next 2 years, Kirwin settled into a routine of spending 4 days a week in Pittsburgh taking his wife to various medical appointments and 3 days a week trying to keep his motorcycle suspension business afloat and provide for his family. It was physically exhausting and emotionally draining. He does not remember going to the UPMC GynOnc Family Caregiver Advocacy, Research, and Education (CARE) Center and says someone must have invited him because he would have never sought emotional help on his own. Nonetheless, the center became a regular place for him to visit when his wife was receiving chemotherapy.
Kirwin remarked that he was so accustomed to focusing on his wife’s cancer that he felt the caregiver role was somewhat insignificant compared to that of the physicians treating his wife. Complicating the matter, he added, was the overbearing sense of helplessness that he could not share with his wife or close family. “I thought my pain was only of consequence to me,” he said. Eventually, he began to trust the nurse interventionist at the CARE Center who called him regularly, and her “skillful wordplay” started to make a huge difference in his well-being.
His wife moved into hospice and died 10 days later. He was only able to share his feelings with that CARE Center nurse, who had become his confidant by then. “I do not know if she was aware of the significant support
that she afforded me, but she gave me a valuable sense of perspective on the malediction of cancer and its impact, and she also gave me suggestions of how I could deal with it,” said Kirwin. For that gift, he said, he values the skill and support of the center staff as much, if not more, than that of the hospital’s capable medical staff.
Heidi Donovan, director of the UPMC GynOnc Family CARE Center at the Magee-Womens Hospital and professor of nursing and medicine and co-director of the National Rehabilitation Research and Training Center on Family Support at the University of Pittsburgh, commented that while the nurse interventionist who counseled Kirwin is an amazing person, she works in a system that allows someone like her to provide the type of support that family caregivers deserve. That system, the Family CARE Center, started as a trial in 2018 funded jointly by UPMC and the University of Pittsburgh School of Nursing. After participating in an American Society of Clinical Oncology quality training program, Donovan and her colleagues launched the center in 2019. It now has one staff member who devotes 60 percent of their time to the center, three nursing faculty members, and a retired nurse volunteer, who counseled Kirwin.
The center’s guiding principle is that caregivers need, but rarely receive, training as valuable members of the health care team and education and support to recognize and manage the emotional and physical stress of care. Donovan and her colleagues believe that these dual needs are best served by providing self-management support, by which she meant support for illness-related tasks. Donovan defined self-management as “awareness and active participation in the recovery, recuperation and rehabilitation and even death to minimize the consequences of treatment and promote health and well-being for the entire family” (Barlow et al., 2002). Self-management support is essential to quality care, said Donovan, and when done well, it can prepare a proactive practice team and create informed, activated patient teams that can have productive interactions to improve functional and clinical outcomes (Epping-Jordan et al., 2004).
Donovan noted that she and her colleagues built the CARE Center on a strong theoretical foundation and descriptive and correlational pilot study data with family caregivers (Donovan and Ward, 2001; Donovan et al., 2007, 2008; Ward et al., 2009). Those led to two large randomized clinical trials that demonstrated the efficacy of this approach (Boele et al., 2022a, 2022b; Campbell et al., 2020; Choi et al., 2012; Donovan et al., 2014, 2022; Ward et al., 2009). They are now working to implement a scale-up intervention trial.
TABLE 1 Representational Approach to Patient/Family Education
| Intervention Elements | Description | Goal |
|---|---|---|
|
In-depth assessment of how caregiver views the problem/issue and its impact on patient and family. |
Shared understanding between caregiver and clinician. Motivate caregiver to make change. |
|
Discover issues and misunderstandings that interfere with self-management. | Reduce barriers to successful self-management. |
|
Evidence-based caregiver guides:
|
Promote confidence in ability to effect change. |
|
Assist caregiver to identify realistic goals and strategies to meet goals. | Provide clear road map for action. |
|
Follow up to evaluate progress toward goal, and modify plan if needed. | Model ongoing iterative process; build relationship. |
SOURCE: Donovan presentation, May 16, 2022.
This theoretical foundation derives from the representational approach to patient education (see Table 1). The first encounter, which begins with an in-depth, individualized, representational assessment of the family’s concerns, facilitates reaching a shared understanding of those concerns and motivates the caregiver to seek out more information to feel valued and understood and to make changes. During those initial conversations, program staff look for gaps or misunderstandings they need to fill to help reduce some of the barriers to successful self-management of the caregiver and their loved one’s health.
Staff then provide evidence-based information about caring for the patient, caring for themselves, and communication and support resources. Staff help the caregiver with problem solving, identifying realistic goals and strategies to reach those goals, and creating a clear action plan. Donovan emphasized the importance of review and follow-up to building a trusting
relationship and demonstrating that this is not a one-time process but an iterative one. She acknowledged that while the research studies she and her colleagues conducted highly protocolized these elements, fidelity to a theory-guided intervention met head on with the realities of implementation in a busy outpatient clinical practice.
Donovan worked with stakeholders to identify key elements of the program, which led to four aims:
- Identify and document a primary family caregiver, as defined and designated by the patient, for every patient seen in the clinic;
- Assess and document the level and sources of caregiver distress for caregivers of patients diagnosed with cancer;
- Provide information, self-management, and problem-solving support; and
- Facilitate referrals to specialty services, given that the program is meant to provide supplemental care.
Every new patient packet includes a form asking the patient to identify their closest support person. This information goes into the patient’s electronic health record and the CARE Center tracking system. The center has identified and documented over 1,600 caregivers over the past 3 years. Staff contacts that caregiver, through proactive outreach, staff and student rounds on the inpatient clinic, or clinician referral, and conducts a brief assessment using the distress thermometer and an adapted problem list for family caregivers (Figure 3).
From 515 caregiver assessments, the CARE team learned that they serve an almost equal number of men and women, who are largely middle-aged and supporting a spouse, partner, or mother. Caregivers have a mean distress level of 4, and their distress arises from needs related to providing care or needs related to self-care (see Box 4).
Center staff work to provide tiered support, starting with assessment and offering information, which includes materials on caring for the caregiver; helping the patient manage symptoms, side effects, nutrition, and the stress of having cancer; and finding support with communication, employment, and legal issues. Tier two adds self-management support, and tier three refers the caregiver to specialty services. The approach, said Donovan, is to teach and support the caregiver to maintain their own emotional help using vetted online resources, referrals to behavioral oncology and palliative care navigation, and connection and warm handoffs to community organization

SOURCE: Donovan presentation, May 16, 2022. Reproduced with permission from National Comprehensive Cancer Network’s (NCCN) Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for NCCN Distress Management v2.2023 © 2022 National Comprehensive Caner Network, Inc. all rights reserved. Guidelines® and illustrations herein may not be reproduced in any form for any purpose without the express written permission of NCCN. To view the most recent and complete version of the NCCN Guidelines, go online to NCCN.org. The NCCN Guidelines are a work in progress that may be refined as often as new significant data becomes available. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
resources. She noted that the gynecological oncology program has integrated its teaching and training mission with the center using undergraduate students, graduate students, and gynecologic oncology fellows.
Donovan noted key challenges, including difficulty with electronic health record integration, data collection, management, balancing clinical care with research assessment, and demonstrating outcomes to ensure that UPMC continues to appreciate the value of the center and support it. She said that she and her colleagues are working to implement a mobile health app, develop an implementation strategy by training UMPC students and fellows to advance the work, and move toward further integration with the electronic health record.
Discussion
Randy Jones, professor and assistant director of community outreach and engagement at the University of Virginia School of Nursing and session co-moderator, with Clyde W. Oden, ACCA’s assistant director, opened the discussion by asking the panelists for ideas on how individuals would start caregiver support programs in their own communities similar to the ones featured in the presentations. Epps responded that a key first step is to hear from the community to identify what it wants. Applebaum agreed and added that getting buy-in from medical staff is important as well, particularly when the program is going to be in a cancer center or other medical institution where mental health care might not be a top priority. Donovan added that she had to engage with the administration and clinicians at her institutions and convince them that as researchers, she and her collaborators would focus on providing care and put their research agenda on hold until after they established that they could provide high-quality care. Donovan
discussed the challenges of demonstrating the impact of their programs, noting: “It’s a longer-term process. We are dealing with [caregivers] in periods of intense stress, but the kinds of mental and physical consequences that come from that unrelieved stress often take a while to manifest, so it’s hard to really demonstrate those strong outcomes,” she explained.
A workshop participant asked about efforts to address logistical demands that typically are overwhelming for caregivers. Applebaum replied that attention certainly needs to be paid, given that a large part of the distress results from efforts to navigate a fragmented health care system. Applebaum suggested that having lay caregiver navigators in an institution is one way to address that need. She added that an important benefit of having mental health care services available at the same place where a loved one receives care is the continuity and ease of access.
Amy Melnick, executive director of the National Coalition for Hospice and Palliative Care, asked the panelists if a disease-specific caregiver group was a best practice. Applebaum said caregivers experience certain common needs and emotions regardless of the health issue, but some conditions, such as brain cancer or dementia, do come with unique demands for which a disease-specific caregivers can offer the precise support that is often difficult to find. Epps said that as she works with faith communities, she wants to make sure she can refer families to various support groups, both disease specific and others, such as those that support spouses or men. She informs families that they can attend multiple support groups and try different groups to find one that best suits their needs.
Donovan said her team has been trying to identify a core set of risk factors for family caregivers to use across settings. These could serve as themes for structured group support that would cut across different caregiving situations. A support group of caregivers whose loved ones have different illnesses can provide advice on how people handle those common problems. At the same time, Donovan noted, disease-specific stressors might be best addressed with additional care, such as in a breakout session or with specific supplements.
Bell said it would be helpful to have more funding sources for community-based work in addition to well-controlled research studies. She also said that measuring outcomes, such as preventing hospital readmissions or saving money, may not be the best way to judge whether an institution should support caregiver support programs. “It is doing the right thing by caregivers and supporting their journey,” she said.
Responding to a question about any particular barriers or challenges he and his husband faced as a gay couple, Gee said he had not truly understood
how important it was to be legally married until his husband developed cancer. In terms of cultural competency, he felt fortunate to have had the benefit of interacting with clinical staff at MSK who were well-trained to work with LGBTQ+ individuals. He added that as a nursing student, he is learning that many of the norms he experienced at MSK are not necessarily the norms at other health care systems.
INTEGRATING FAMILY CAREGIVERS INTO THE HEALTH CARE TEAM
Caregiving for a Loved One with Alzheimer’s Disease
Jason Karlawish, professor of medicine in the Perelman School of Medicine, co-director of the Penn Memory Center at the University of Pennsylvania, and caregiver for his father with mild cognitive impairment from Alzheimer’s disease, led off the fourth session on integrating family caregivers into the health care team. Karlawish explained that caregiving is the oldest profession, and the concept appears in the Old Testament. In the Book of Ruth, he noted, Naomi tells her widowed daughters-in-law that they should return to their villages to find new husbands and that she would be fine on her own. Ruth, however, refuses to leave Naomi. While the word “caregiver” does not appear in the Bible, Karlawish noted that is exactly the role that Ruth assumes. Karlawish added that increased usage of the term “caregiver” aligns with the rising number of individuals diagnosed with Alzheimer’s disease. Karlawish also noted that use of the word “autonomy” rises exponentially in the twentieth century, indicating, in Karlawish’s view, the recognition of Alzheimer’s as a disease because it causes significant loss of autonomy.
Karlawish pointed out that robots are now able to comfort people with cognitive impairment by interacting emotionally with them and may be able to carry out discrete caregiving tasks. ElliQ,33 for example, is a robot that engages a person in conversations, motivates them to adopt healthier habits, and even surprises them with jokes and suggestions. ElliQ uses artificial intelligence to learn who its owner is and tailor conversation to them.
Caregivers, said Karlawish, take on at least one of four roles, some of which only humans can currently fulfill: extended body, extended cognition, extended mind, and extended self. An example of a task of extended
___________________
33 For more information, see https://elliq.com/ (accessed August 9, 2022).
body is assisting a loved one to cross the room. Leaving sticky notes to remind the patient of things they have to do is an example of extended cognition; as many caregivers say, they are their spouse’s working memory. Karlawish explained that making a spouse’s annual donation to a local arts fund, something that was an important part of who that person is, is an example of serving as the extended self. That requires truly knowing who that person is and so cannot be entirely managed by technology, noted Karlawish, and these extended roles separate caregiving from the services that other members of the care team can provide.
Karlawish objected to the use of terms such as “informal” versus “formal” care or “skilled” versus “nonskilled” to describe what caregivers do. “This is all quite skilled,” he said. “To call it unskilled is an insult.” Karlawish also noted that many caregivers take on the disease attributes of their loved ones because while they do not have the pathology, they do have the disease experience. He called out the importance of training, supporting, and accommodating caregivers as extensions of the patient’s body, cognition, mind, and self. Ethics, he said, has a theory that someone is either competent to make decisions or not. “But in between is this vast need for support and supported decision making,” said Karlawish, and caregivers need training to help their loved ones make decisions. For individuals with dementia, caregivers become two minds in one body, their own mind and the mind of the person they are supporting.
Karlawish shared that he believes it is insulting to call a caregiver a visitor and not a member of the care team. “We saw over the last years precisely what happens when you take away visitors, and I will not embellish that except to say that we should revisit what it even means to have a visitor policy,” said Karlawish. He noted that even in his memory center, he struggled to have a sufficient number of chairs and space to accommodate all family members.
Karlawish concluded his remarks noting that it is a moral imperative to give caregivers access to the patient’s medical record, given their role. Karlawish also highlighted the need to compensate caregivers.
Including Family Caregivers in Patient Health Care Teams
Courtney Harold Van Houtven, research career scientist at the Center of Innovation to Accelerate Discovery and Practice Transformation, part of the Durham Veterans Affairs (VA) Health Care System, and professor in the Department of Population Health Science at Duke University School
of Medicine and the Duke-Margolis Center for Health Policy, discussed some innovations at the VA regarding the role of family caregivers. She began by emphasizing that health care systems are complicated and chaotic and sometimes work better when teams include perspectives from different professionals, including caregivers, when they are self-organized and non-hierarchical (Cilliers, 1998; Stacey, 2001; Van Houtven et al., 2019a). Self-organization,34 explained Van Houtven, increases information flow, which should increase the quality of care for patients.
Van Houtven noted that there are more than 5.5 million caregivers of veterans, according to a 2014 RAND Corporation report (Ramchand et al., 2014). They act as case managers, undertaking a variety of the responsibilities that a formal health care provider would deliver (Ramchand et al., 2014). Van Houtven noted that in addition to knowing a patient’s status, they offer critical information to providers about their own capacity to provide care safely in the home. The RAND report recommended that health care settings serving veterans should acknowledge caregivers as part of the health care team, and yet as the National Academies report Families Caring for an Aging America detailed, practical approaches for including and engaging caregivers remain poorly defined (NASEM, 2016).
In 2014, Van Houtven began directing the Partnered Evaluation Center, which evaluated the VA’s Caregiver Support Program, 35 the largest such program in the nation. The program provides training and even stipends to qualifying caregivers, and Van Houtven was charged with assessing the impact of such support on patients and whether engaging caregivers increases high-value care. Van Houtven emphasized that it does enhance the care quality, noting that “it increases primary care engagement without increasing things like emergency department or inpatient visits” (Bruening et al., 2020; Van Houtven et al., 2019a, 2019c).
Van Houtven and her team conducted in-depth interviews with approximately 100 caregivers involved in the program (Bruening et al.,
___________________
34 “Self-organization” generally refers to situations wherein individual team members adjust their behavior to one another’s actions and the changing environment. According to complexity science research, effective self-organization depends upon three critical system parameters: the nature of connections among people, the rate of information flow throughout the system, and the cognitive diversity (that is, the different perspectives, training, and experience) of the team. For more, see https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.05486 (accessed September 28, 2022).
35 For more information see https://www.caregiver.va.gov/support/New_CSC_Page.asp (accessed October 18, 2022).
2020). She learned that they appreciated the tailored and individualized support from caregiver support coordinators throughout the VA system who help them navigate the complex care system. However, they expressed frustrations with the system, a point Van Houtven illustrated with a quote from one caregiver: “I do not have a sense that there is a team, somebody coordinating his condition saying, ‘Okay, that’s your primary care doctor, that’s the neurologist… I’m the person coordinating all this and you’re the caregiver and we’re all part of this team.’ I don’t have that sense at all.”
Van Houtven and her colleagues developed the Caregiver Perceptions about Communication with Clinical Team Members (CAPACITY) measure, which examines two domains about how well the team performs at communicating with them and considering their preferences, needs, and capacity to care. They have fielded the measure with multiple types of caregiver populations enrolled in Medicare or among veterans. They found that scores were consistent across illnesses and populations, which indicates the long way to go in terms of supporting caregivers as a member of the team (Van Houtven et al., 2019b, 2020).
Van Houtven shared that a survey of caregivers’ experiences on the veteran care team for post-9/11 veterans found that 56 percent of the caregivers said the patient’s health care team never asked for their ideas about managing their veteran’s health; 69 percent said the patient’s health care team never asked whether they have the skills or training they need to help their veterans; and 72 percent said the patient’s health care team never asked if they needed help at home in managing their veteran’s health condition (Van Houtven et al., 2019b). “This is in a system of care that actually covers long-term care comprehensively and also has a very extensive caregiver support program,” said Van Houtven.
A new initiative launched by the VA and the Elizabeth Dole Foundation, the Campaign for Inclusive Care,36 has the goal of empowering health care providers and professionals to engage caregivers as part of the veteran care team through policy, practice, and culture change. This program convened a strategy meeting with scores of different types of providers and collected data from caregivers and providers to define the key components of care, which includes caregivers as part of the care team. Based on multiple perspectives garnered through caregiver interviews and surveys and from
___________________
36 See https://campaignforinclusivecare.elizabethdolefoundation.org/ (accessed August 5, 2022).
providers, inclusive care requires five key components (Boucher et al., 2021; Sperber et al., 2019):
- system-level policies of inclusion,
- a clear role definition of caregiver,
- a caregiver capacity assessment,
- explicit caregiver involvement, and
- guidelines for caregiver-professional communication.
Van Houtven commented that the definition of inclusive care is inviting the caregiver to participate in shared decision making and treatment planning (Shepherd-Banigan et al., 2021). According to caregivers, the key barriers to inclusion are a lack of time by the medical staff to “deal” with the caregiver; the attitude that caregivers are not providers, so they do not need to know any details; legal or privacy concerns; and frequent changes in the composition of the health care team. This last barrier not only leads to fragmentation but also prevents meaningfully engaging the caregiver in the care. Van Houtven noted that legal and privacy concerns are common and easy to surmount with training and being clear with providers about the rights of patients and caregivers.
Based on what they learned about the barriers to inclusion, the VA Caregiver Support Program and strategy team decided to develop an education and awareness campaign, which they piloted in the VA and then rolled out nationally. The resulting Academy of Inclusive Care comprises a short, four-unit course, with each unit lasting 15 minutes.37 The units provide an introduction to the practice of inclusive care, discuss who military and veteran caregivers are, address communicating with the caregiver, and provide an understanding of the caregiver journey and a map for it to drive home the message that this is a longitudinal process in which needs change over time based on the trajectory of the disease or condition. The program uses the acronym CARE, which stands for Consider who else needs to be present, Acknowledge that the caregiver has taken on extra work that will impact their wellness, Review the role and responsibilities that the caregiver is comfortable with, and Encourage the caregiver by identifying barriers and offering to help develop solutions to help make their role easier. This acronym, said Van Houtven, provides a standardized language and under-
___________________
37 Additional information is available at https://campaignforinclusivecare.elizabethdolefoundation.org/academy-for-inclusive-care/ (accessed August 5, 2022).
standing for the providers. She noted that the program has been delivered to 5,000 VA providers. Champions have been identified at each site who are spreading awareness, recruiting providers, and trying to change the culture to make caregiver inclusion a standard of care.
Van Houtven explained that the VA has rolled out its own caregiver-linked electronic health record for those who are engaged in caregiver support services. It is now working on developing a toolkit to give caregivers the skills they need to communicate effectively with providers and engaging leadership across the VA to make this the standard, which requires getting the entire primary care service involved because that is where most care is delivered.
In terms of learning from the VA experience, Van Houtven identified a need to test and evaluate models of caregiver inclusion in both outpatient and inpatient settings within private health systems. This evaluation should examine if inclusion affects emergency department visits, hospitalizations, costs, and discharge to home as a means of establishing a return on investment. Policy changes are needed to ensure reimbursement for health care team visits with caregivers (Riffin et al., 2022), performance rewards for teams that include caregivers (Van Houtven et al., 2019a), pay for caregivers (Werner and Van Houtven, 2020), expansion of caregiver supports along the lines of the RAISE Act, and incorporation of caregiving and inclusive care into health professionals’ educational curricula (Leykum et al., 2022). Finally, in terms of health systems, Van Houtven emphasized the need for health-system-level changes to formally recognize and identify caregivers and document this information in health records in a standardized way (Ma et al., 2022; Van Houtven et al., 2022). In closing, she pointed out the importance of expanding support to groups that face racial, ethnic, and economic inequities and groups that face greater care responsibilities, cost, and poorer outcomes (Choi et al., 2021).
Caregivers as Surrogate Decision Makers for Patients with Serious Illness
Terri Fried, professor of medicine and section chief for geriatric medicine at Yale University School of Medicine, began with an important observation about the power of family caregiving. In a study published in 2020, researchers showed that a multidisciplinary intervention—the Hospital Elder-Life Program developed by researchers at Yale University School of Medicine (Inouye et al., 1999, 2000, 2006)—can prevent delirium in at-
risk hospitalized patients. Fried explained that it was designed specifically to include family members as part of the treatment team in a randomized controlled trial conducted in China, where it is common to have family members provide care in the hospital (Wang et al., 2020); it achieved a 40 percent reduction in the incidence of delirium, better than anywhere it has been tried in the United States (Inouye et al., 1999).
Moving from this example of the importance of including family members in care, Fried argued that it is the responsibility of the health care team to prepare caregivers to serve as surrogate decision makers and also to recognize the huge stress and burden that caregivers bear in the role of decision makers. “Our job is to facilitate communication between patients and caregivers and prepare caregivers for in-the-moment decision making,” she said.
Fried referenced a study of ICU patients that found that 33 percent of their family members were assessed as having post-traumatic stress disorder (PTSD) at 90 days after the loved one’s death or discharge, and 60 percent of family members who were involved in end-of-life decisions had PTSD (Azoulay et al., 2005). Fried identified a number of reasons for this, starting with a lack of communication with caregivers. In a study conducted by Fried and her colleagues, caregivers of patients with serious illness reported that communication was important, but 40 and 37 percent said they wanted to talk more or that it was difficult to talk to their loved ones, respectively (Fried et al., 2005). These numbers were higher than the patients’ reports. The problem, according to Fried, is that caregivers whose need for communication was unmet had higher caregiver burden scores.
Fried noted significant missed opportunities for communication, which she identified by interviewing bereaved caregivers (Fried and O’Leary, 2008). One caregiver shared that “what I didn’t know until after he had died [is that] 2 weeks before he died, he called my sister and told her he wasn’t going to be around much longer. He knew he was going but he didn’t want to tell me because I’d get mad at him.... I just wanted him to fight, and he just wanted to tell her what he felt for me,” and another said, “the social worker from hospice came to talk to me, and I found out after he died that he already knew he was dying, but he did not want to tell me, and I did not want him to know that I knew he was dying, so I told them not to say anything. So, between the two of us, we were trying to keep each other from knowing that he was dying” (Fried and O’Leary, 2008).
Fried pointed out that caregivers overestimate their ability to make surrogate decisions. In a study of older persons and their surrogate decision makers, Fried and her colleagues found that over 75 percent of caregivers
were extremely confident in their ability to make the decisions (Fried et al., 2019). However, when asked about what their loved ones value in terms of their goals of care, only 20 percent of the caregivers were actually knowledgeable. Moreover, only 22 percent of the dyads agreed that they had communicated with each other; 42 percent agreed that communication did not occur. The remaining 36 percent disagreed about it (Fried et al., 2017).
To explain these findings, Fried relied on lessons learned from people with lived experience. One caregiver, Fried explained, realized that she and her husband had never talked about issues related to the use of life support. The caregiver shared that “he knows that he does not want life support but he doesn’t understand the fact that there can be illness that you can still live [with] but [it] will affect the way you live” (Fried et al., 2016). Fried added that another caregiver observed that “the whole issue of life support, to me anyway, is at what point does the person not want continued life support, or even [do they want] life support to be initiated? How compromised do you have to be? What chances are there for any level of recovery? All of those things play into it and that we have never discussed” (Fried et al., 2016).
Fried pointed out the problems with trying to make specific treatment decisions in advance of an actual, rather than hypothetical, clinical scenario. Fried explained that the human ability to adapt to disability and illness is almost endless and the patient’s preferences and willingness to endure a diminished quality of life to extend the quantity of life can change over the course of an illness. “The problem is if people have a single discussion where the patient documents his or her preference, the thought is we are done,” said Fried. “If we do not encourage continued communication, we do not know how those preferences might be changing over time.” In addition, it is impossible to understand what the patient’s best interests will be in a specific clinical situation, and most patients also want caregivers to take their own needs into account.
Instead, providers need to encourage patients and caregivers to talk more generally about what matters most at the end of life. As Fried explained, they need to ask questions about what the final illness trajectory will look like, discuss when life is no longer worth living, question if that perspective changes over time, and discuss how much leeway caregivers have to make decisions. Fried added that clinicians need to recognize the burden they place on caregivers, and that will require training. “This is the one area where we really need to do shared decision making. We are not just sharing in the decision, we are sharing in the burden,” she said. “How many caregivers think that we are asking them to make a decision that is going to
result in the death of a loved one? How can anybody be asked to do that?” In closing, Fried noted that clinicians should take on the technical burden of describing the choices so that the caregiver can see how those choices are or are not going to accomplish the story they want to write.
Supporting Care Partners with Health Information Technology
In the final presentation of the day, Catherine DesRoches, executive director of OpenNotes and associate professor of medicine at Harvard Medical School, explained that OpenNotes38 is a philanthropically supported initiative designed to improve health care through increased information transparency. Specifically, that means ensuring patients and care partners39 have the information they need about their loved ones to make informed care decisions. DesRoches and her colleagues found that patients share their information with their partners, their friends, and the lady down the street who happened to be a nurse who might help them. Caregivers surveyed about getting this information reported that they find it extremely helpful. In fact, getting this information makes it more likely that caregivers will remember the care plan, understand what they are supposed to do, and know which medications their loved one is taking and how to take them (Chimowitz et al., 2018; Jackson et al., 2014; Wolff et al., 2016).
DesRoches is also the primary caregiver for her aunt, who was diagnosed with dementia in 2016. Inspired by others’ honest accounts of their caregiving experiences, DesRoches shared that her aunt can be difficult, prickly, snappish, and cold. “Her diagnosis of dementia did not turn her into a malleable human being,” she said. DesRoches noted that a win she had early on was getting her aunt to give her proxy access to her patient portal, which enabled her to see clinical notes, medications, and test results and communicate directly with the health care team about issues that would anger her aunt if they were raised at a clinical visit. DesRoches added that such access also enabled her to prevent a serious medication error in an emergency department, where staff was about to use a 2-year-old medication list and inappropriately discharge her aunt.
___________________
38 See https://www.opennotes.org/news/new-onc-rule-interoperability-2020/ (accessed August 5, 2022).
39 The individuals selected to share access to patients’ portals are referred to as “care partners.” For more information, see https://academic.oup.com/jamia/article/23/6/1150/2399296/ (accessed August 5, 2022).
DesRoches explained that she and her colleagues are working on projects focused on the continuum of complexity around information technology, from using the portal as a proxy to using it and electronic health record to create feedback loops for clinical care (Figure 4). DesRoches noted that most health organizations now offer a patient portal and many also offer proxy access. In one ongoing project, she and her colleagues are trying to increase the use of proxy access at three clinical sites by designing a process that would remind patients, care partners, clinicians, and other staff about the portal as the patient and care partner moved through a clinical visit. They designed this process working with care partners, patients, clinicians, and staff, she explained, and it includes hanging posters in waiting and exam rooms and passing out informative brochures to patients that explain why they might want to sign up for proxy access and how to go about doing that.
Another project DesRoches is working on explores using existing functions in the patient portal to identify care partners: patients receive a questionnaire in advance of their visit that inquires if they are the patient or someone filling out the form for them. If the latter, the person is asked to provide their name and relationship to the patient. This information is stored in a structured field in the electronic health record and easily accessible to the clinician.
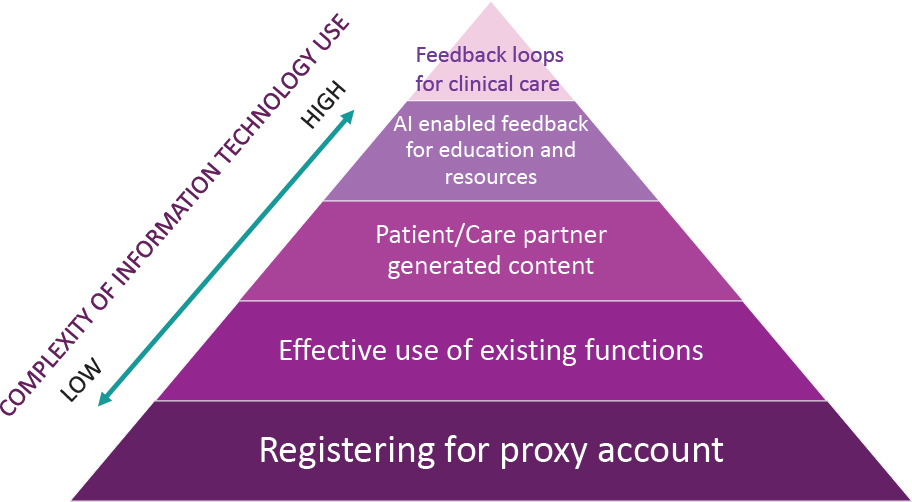
SOURCE: DesRoches presentation, May 16, 2022.
DesRoches described a third project, ongoing at three clinical sites, that is trying to identify care partners of patients coming to the clinic and patients who are care partners themselves, understanding that care partner responsibilities can have a profound impact on a caregiver’s health. Patients receive a previsit questionnaire that asks who they are, if they are the patient or someone else, how long it has been since their last visit, how they are doing, and if they have any new symptoms, with some prompts to tell them what kinds of information to enter. “This is essentially drafting the subjective part of a clinical note,” said DesRoches. The questionnaire also asks the person to list the three most important things they want to discuss, setting an agenda for the visit. At the end, the questionnaire asks if the person is caring for a relative or friend. A yes answer links to the CII, discussed in an earlier session of the workshop, and the person can come back to the questionnaire to enter their CII score. This information is then available to the clinician before the visit and pulled into the clinical note; when the clinicians open the note to do their own documentation, the information is already there.
In closing, DesRoches shared that she and her colleagues have been working on the possibility of using artificial-intelligence-enabled feedback for education and to provide resources through the portal. The idea is that a patient or caregiver would complete the questionnaire, and the software would identify key phrases that might suggest resources to address a particular problem, such as the patient having difficulty sleeping. They are also working on developing feedback loops for clinical care that would ask patients and caregivers in between visits if they are following through on a particular task.
Discussion
Sara Damiano, national director of palliative care at Ascension40 and session co-moderator with Allison Applebaum, opened the discussion session by commenting on a key theme reinforced throughout the speakers’ presentations: the importance of communication, shared decision making, and conversations about goals of care. She asked Fried if she could talk more about the barriers that impede conversations between family caregivers and patients and ways of overcoming them. Fried replied that a number
___________________
40 As of August 2022, Ms. Damiano is the Director of Strategy, Integrated Kidney Care at DaVita Kidney Care.
of tools were developed to address these barriers, such as the conversation project’s starter kit and the PREPARE for Your Care website.41 Fried noted the belief that this work needs to happen outside of the clinical setting. The question, she said, is how much can a clinical intervention or clinical touch jumpstart the conversation to ensure that it can continue at home. Fried and her colleagues have completed a trial recently in which they found that brief interactions with individuals trained in motivational interviewing, from psychology interns to hospital social workers, helped overcome some of the barriers that impede meaningful conversations.
Responding to a question about his remarks related to caregivers being an extension of a patient’s self, Karlawish explained that that perspective recasts the role from doing chores to engaging in a morally intense activity. Fried commented that Karlawish’s concept is important for the role of caregivers as surrogate decision makers, the conundrum of respecting an individual’s advance care plan, and the reality that patients are part of familial and caring units. For Fried, it is important to ask patients and their loves ones to think about how much of the story they want to write ahead of time and how much they will leave to be written, with the express recognition that things will get increasingly difficult for the caregiver in terms of decision making as the illness progresses. Applebaum added that it is clear that these conversations cannot happen only once but need to be repeated as goals of care change.
James Tulsky, chair of the Department of Psychosocial Oncology and Palliative Care at the Dana-Farber Cancer Institute, remarked that Karlawish’s notion of the extended mind and extended self rings true for him and is a great moral argument in defense of providing support for caregiving. He shared that based on what he sees in the hospital, how caregivers are viewed by health care teams does not have a great deal of nuance: they see them as valued allies and heroes or as the enemy or an obstruction. Tulsky wondered if the caregiver’s extended mind and self can cause conflict with the patient or clinician. Karlawish responded that families can be difficult, but it is important to consider the role the health system has played in making them difficult. For him, it is important to remember that caregivers are not angels or heroes but humans doing the best they possibly can with uncertain information. That allows for having a normal human conversation between two people who are trying to do the best they can.
___________________
41 For more information, see https://theconversationproject.org/ (accessed August 5, 2022) and https://prepareforyourcare.org/en/welcome (accessed August 5, 2022).
In response to Damiano’s question about barriers to using OpenNotes in terms of disparities in health literacy and health equity, DesRoches responded that one surprising finding from her work is that people who reported lower levels of formal education or speak a language other than English at home were more likely to report benefiting from reading their notes. She shared the example of a woman who spoke a language other than English at home, who said that reading her clinical notes helped her recall what her doctor told her in English which she had to translate, making it difficult to remember what she had heard. DesRoches noted that people only remember about half of what they hear in a clinical visit, even less when it is stressful, a difficult diagnosis is delivered, or the patient and caregiver disagree. Having access to clinical notes allows people to revisit what was said. She cautioned against underestimating what any patient will do or the resourcefulness of a patient who wants information.
DesRoches pointed out that issues of health equity are important because people who have lower levels of formal education, speak a language other than English, or are Black or Latinx are less likely to be offered access to this technology and then less likely to use it for a variety of reasons. Van Houtven added that not having a caregiver field in the patient’s electronic health record is an equity issue because caregivers who self-nominate are often the least disadvantaged. Having a system where everyone is equitably asked about their caregiver or has their own caregiver-linked record is a way to make sure that everyone has the opportunity to identify one. Karlawish agreed and wondered if the EHR could include a prompt at the time of scheduling an appointment for people with certain diagnoses that would likely necessitate caregiving. In this way, the patient would be prompted to provide information about the person who would be assuming the role of caregiver.
Applebaum, noting that the VA has led the way with regard to integrating caregivers into the health care system, asked Van Houtven to talk about some of the lessons the VA has learned that could be used to motivate other health care systems. Van Houtven replied that the VA has the advantage of having an integrated system that can follow its patients over time. The VA can require that providers are trained, which makes it easier to implement programs such as the Campaign for Inclusive Care. Outside of the VA, the challenge is to demonstrate a return on investment for this type of intervention, perhaps in terms of improving communication with caregivers. Rewarding teams for including caregivers could earn providers’ buy-in, as would having reimbursements for health care visits that include the care-
giver, an idea that Karlawish supports. She also recommended introducing these concepts in medical and nursing schools and normalizing that caregivers are part of the health care team who can provide useful information.
Damiano then asked the panelists for their ideas on how to restructure health care delivery to provide time for clinicians to interact meaningfully with caregivers. Van Houtven responded that holding virtual rounds that include the caregiver would be a great solution. While this might require additional time up front, it could save time in the end and will improve outcomes because caregivers will know the symptoms to expect and be aware of any changes. Another idea would be to have the caregiver provide input before rounds for the clinicians to consider and include in treatment planning and decision making. Fried said this idea reminds her of a nursing home program that involved getting input from the certified nursing assistants who spend time with the residents and can pick up changes earlier than anyone else. She thought this could be viewed as a relatively easy change and would result in better outcomes and lower costs. Shifting away from fee-for-service health care payment would create time in the visit to interact with caregivers, added DesRoches.
Bynum asked the panelists if they had any insights about engaging family and surrogate decision makers in the primary care setting rather than in specialty care or more rural versus urban settings. Fried, speaking as a geriatrician, said that restricting engagement to specialty care will miss a huge group of people who do not have a predominant, single illness. Damiano suggested that the annual Medicare wellness visit, which typically includes more time, might be a good way for the patient and family caregiver to meet with a clinician with whom they already have a strong relationship.
Peggy Maguire, president and board chair of Cambia Health Foundation, asked Van Houtven to clarify whether research is available that indicates that including the caregiver improves medical outcomes for VA patients. Van Houtven replied that a study is now ongoing to assess whether meaningful inclusion does change outcomes and improve quality of life and quality of care. Maguire suggested a similar study exploring the impact on caregiver mental health and well-being. Such research, Maguire noted, could impact reimbursement rates and even Medicare star ratings. Van Houtven agreed and said the investigators have done qualitative interviews with caregivers who have had health care providers who have taken this training and they report feeling more included and have a more positive view of their engagement with the care team. Providers, for their part, report
feeling empowered by and excited about their new skills, which could be a bonus in terms of increasing provider satisfaction and reducing burnout. Applebaum added that in oncology, she and some of her colleagues have data showing that when the caregiver’s mental health improves, patients self-report that their quality of life improves.
Drane asked the panelists to comment on how to consider the needs of the caregiver while also protecting the quality of life as defined by the person for whom they are caring. Van Houtven said the challenge is that the United States has a system where most people do not have the resources to provide the kind of care that their loved ones want. For example, a parent might not want their adult child to be their caregiver and prefer to hire someone, but if neither has the financial resources to do so, that is not a real option. Karlawish said that a theme he heard throughout the day was that fundamental needs should be met, but that is not happening. In his opinion, without that, having intimate, deep conversations about larger moral issues is challenging and may lead to unwanted outcomes and conclusions.
Fried responded that Drane’s question raises another important issue specific to caregivers of patients with dementia that the discussions of the day had not covered, which is the tension between safety and freedom. The patient may want to live at home, for example, while the caregiver worries about the patient with dementia falling or forgetting to turn off the stove. She recalled how she had a patient in her geriatric clinic who wanted to eat sweets, while his wife was worried about his blood sugar levels. Questioning whose rights prevail, she observed: “I do not know that we have a systematic way to empower either the clinician or the patient and caregiver to feel good about those kinds of decisions,” said Fried. DesRoches added that for most families, particularly when dealing with dementia, choice is an illusion.
Karlawish pointed out that America’s financial services industry is in a position to be an institutional caregiver, in a sense. Banks and financial services industries see the initial stages of cognitive impairment in their clients, and some are taking this issue seriously. Some make ineffective gestures, however, and others still treat this as a risk mitigation issue. “I think a conversation about caregiving in America ultimately needs to think about how to include the banking and financial services industry in caregiving,” said Karlawish. One solution is to provide caregivers with view-only rather than joint accounts, which could help prevent family members or others from taking advantage of a cognitively impaired person. Karlawish pointed out that some financial institutions have systems that only allow certain types of expenses to be charged to an account.
Erin Kent, associate professor of health policy and management at the University of North Carolina Gillings School of Public Health, commented that health systems might want to consider using the Consumer Assessment of Healthcare Providers and Systems,42 given that it includes family-centered care as part of its metrics. She asked if any of the electronic health record systems that include caregiver documentation are accompanied by caregiver registries for research purposes, and if so, how those were developed. DesRoches said that in her experience, a physician or nurse champion in an organization sees the need and creates the registry, and it develops over time. Van Houtven said that the VA’s caregiver registry grew out of the Caregiver Support Program, but a primary care provider who identifies a caregiver cannot automatically create the record on their own. Instead, that information has to go to the caregiver support program, which approaches the caregiver and asks if they want to enroll.
Day One Wrap-Up
In wrapping up the first day of the workshop, Oyer summarized the important points from the day’s presentations and discussions. He began with what is being done well, noting the RAISE Act, which makes it possible to have a national strategy that codifies the concept of person and family-centered care. He noted that it is critically important that caregiver voices are at the center of both the design and implementation of any program or initiative and that public–private partnerships have great value. The exemplars and caregiver stories are important, as is the message that community programs work when they emphasize partnership, customized activities, community health representatives, and self-management support.
In terms of gaps, the challenge of advancing health equity was emphasized. It is also important to realize that caregivers need a variety of ways to receive information, medical pathways do not always fit with patient and family needs, employers must be more flexible to accommodate the time challenges caregivers face, and education, while important, is not sufficient.
Oyer’s last point was that implementation of a national strategy that makes it possible for caregivers to be equal members of the health care team should be a priority. Some approaches that the speakers highlighted include making time and space for caregivers as an extension of the patient and training teams on caregiver communication. Other approaches include
___________________
42 See https://www.ahrq.gov/cahps/index.html (accessed August 5, 2022).
making the medical team responsible for preparing caregivers to be surrogate decision makers and sharing health information electronically to enable caregivers to help with patient care and improve outcomes.
DAY TWO OF THE WORKSHOP
In her remarks to open the second day, Grace Campbell referred to a few key points from earlier speakers, such as the universality of the caregiving experience, observing that “We are all going to be, if we are not now, caregivers in our lives, sometimes multiple times.” She observed that the RAISE Act “is a great start and the strategies that are soon to come out from that are going to be an amazing road map for us.” She also called out the many programs and initiatives featured in earlier presentations that are “meeting the needs of caregivers right where they are.” Campbell reminded attendees that despite the progress in some areas, many gaps remain, particularly in health equity and ways to better design programs and initiatives to more closely meet caregivers’ specific needs. She added that more work also needs to be done to incorporate family members more fully into the health care team. She explained that the upcoming presentations would explore the challenges and opportunities in the research and policy realms.
RESEARCH CHALLENGES AND OPPORTUNITIES
Pamela Hinds, executive director of the Department of Nursing Science and professional practice and quality research integrity officer at Children’s National Hospital, professor of pediatrics in the School of Medicine and Health Sciences at George Washington University, and co-moderator of the fifth session, with Cathy Bradley, began by asking a series of questions:
- How can the nation address needed research on family caregivers?
- How can the nation focus—and remain focused—on what family caregivers find important while also addressing what health care systems find important about family caregiving?
- How can investigators minimize the burdens and maximize the benefits of their research, and how can they include health equity in all of their research?
- How can investigators gain access to caregivers when at times the only access is through the seriously ill patient?
- Are there strategies learned during the COVID-19 pandemic that might be relevant and applicable to studies regarding family caregivers as the backbone of caring for the seriously ill in the United States?
Translating the Caregiver Experience into Research
Rebekah Angove, vice president for patient experience and program evaluation and director of the Patient Advocate Foundation’s Patient Insight Institute, noted that the foundation serves approximately 153,000 patients a year, helping them address access and affordability challenges (Patient Advocate Foundation, 2021). Through that work, the foundation has learned a great deal about the patient and caregiver experience for those with chronic and complex illnesses. She added that the foundation created the Patient Insight Institute to amplify the voice of underserved patients with chronic and complex illnesses and expand their engagement in policy, care, and research while also collecting insights that the foundation can use in its initiatives. In her view, research is not an add-on to this work. “It is foundational to supporting and expanding the care that we are giving, the services we are providing, and the approach that we are taking to patient services, as well as caregiver support and services,” said Angove. She encouraged those who work in direct service, policy, and support spaces to think of research as a complementary and supportive means of expanding their work and maximizing its impact.
Angove pointed out that caregivers grew from 43.5 million to 53 million between 2015 and 2020, with nearly one in five adults providing care to an adult with health or functional needs (AARP and the National Alliance for Caregiving, 2020). This figure is probably low, she added, because most caregivers do not identify with that term, as discussed in previous sessions. When a caregiver or their support person calls the Patient Advocate Foundation, staff asks them who is supporting them or whom they are supporting, and only 5 percent use the word “caregiver.” “I imagine that if we asked that question differently and really explored the roles people are taking in others’ lives, that number would be higher,” said Angove.
Though health care overall and research are moving toward a patient-centric approach, it is important not to leave caregivers out of the equation, said Angove. The challenge from a research perspective is that while the caregiver does not exist without a patient counterpart, they have their own independent concerns and needs. She has found when talking to
patients and caregivers that the relationship is quite complex. For example, researchers often think of the caregiver as the gatekeeper, but she and her colleagues found that patients are hesitant to allow researchers access to their caregiver. Another challenge researchers face is that caregivers, particularly those who are from historically underrepresented and underserved groups and struggling with needs related to income security, health care, food, housing, and employment, are already under intense time and resource burdens and juggling their own needs with those of their loved ones. As a result, they may not have the energy or time to participate in research.
Angove and her team conducted a survey in which they asked members of their patient insight network if they had ever been contacted or approached about serving as a partner in a research team, and 15.35 percent said yes. When asked to what extent they feel they have valuable experiences to share with researchers, 27.68 percent said they had a great deal to share, 42.86 percent said they had a moderate amount to share, and 25.45 percent said not much; only 4.02 percent said they had nothing (Patient Advocate Foundation, 2021). In Angove’s view, this means untapped resources are available in the form of caregivers who are excited and interested in partnering and working on research projects and initiatives.
When her team asked about the challenges to participating in research, the caregivers reported a variety of challenges, including transportation, difficulties taking time off from work, and not being paid to participate. They also cited being unable to get away because they are caring for someone or taking care of their children, or because they have a disability or physical limitation that would make participation difficult. Nearly everyone, however, said they would be willing to participate if these burdens were addressed. In Angove’s opinion, it is the researchers’ responsibility to understand those barriers and find way to address them in order to effectively and meaningfully integrate caregivers into research projects.
Angove noted that despite the challenges, unique opportunities exist, too. The key is to expand patient engagement initiatives to include caregivers both as part of the patient–caregiver dyad and as a stand-alone community. She advised making sure that providers, caregivers, and their patients are in the room as a means of understanding the complex communication dynamics that several workshop speakers noted. It is also important to make sure that the caregivers who are engaged in research represent the full range of patient experiences. Accomplishing that requires understanding the diverse experiences of different treatment options and outcomes, representing different and diverse health conditions, and involving rural
patients, patients of different races, ethnicities, and sexual orientations, and nontraditional families. “That is the only way we are going to understand the full constellation of experiences that caregivers have,” said Angove.
Achieving that type of diversity will require changing outreach, communication, and recruitment tactics, which Angove and her colleagues are doing. For example, rather than merely asking if they are caregivers, they now allow caregivers to include other identifying characteristics such as spouse, partner, sibling, and so on. They have also started experimenting with asking what roles caregivers play as a means of socializing and normalizing the term “caregiver.” However, researchers need to be free to move away from that term because it does not resonate with all communities, cultures, or individuals.
The Science of Family Caregiving and Its Impact
Jennifer Wolff, the Eugene and Mildred Lipitz Professor and director of the Roger C. Lipitz Center for Integrated Health Care in the Department of Health Policy and Management at Johns Hopkins Bloomberg School of Public Health, began by emphasizing that the science of family caregiving is strong but its impact is comparatively weak. Wolff pointed out that while it is possible to define research impact in any number of ways, a foundational definition is that the benefit extends beyond the academic knowledge base (Greenhalgh et al., 2016). To the extent that health-oriented research is intended to benefit the well-being of individuals, families, and society, it is critical that investments in research minimize waste and yield high value, she added.
Noting the important gaps in the impact of research on family caregiving, Wolff said that a foundational challenge with descriptive research relates to measurement. “There is notable ambiguity in the terminology that we use to communicate with ourselves and with the public about what we mean, variable definitions that are used in our research studies to identify caregivers, and a recognition that caregiving exerts both positive and negative effects on wide-ranging outcomes from physical and emotional health to quality of life to economic well-being,” said Wolff. The net result is that despite a robust research enterprise, the evidence is diffuse and difficult to synthesize, which has been an impediment to making progress in the policy realm.
Wolff acknowledged the importance of the U.S. national survey infrastructure and caregiver-reported instruments. These, she said, have been foundational to understanding experiences across and within vulnerable
subgroups. However, she added, consensus is lacking on relatively basic information. For example, population surveys estimates about working-age adult caregivers vary by almost twofold (22–40 million) (Freedman and Wolff, 2020).
The research evidence about the consequences of caregiving is also notably variable, said Wolff. For example, the media has emphasized findings on the mortality impact of caregiving based in large part on a single 1999 study in which the effects were higher in a convenience sample of 76 spousal caregivers (Schulz and Beach, 1999). However, subsequent population-based studies and a meta-analysis have not replicated this finding and even suggest lower mortality among caregivers (Roth et al., 2015). The media also highlight a caregiving cliff, with fewer caregivers assisting a more impaired population and being at risk for more significant effects. However, a study she and her colleagues conducted, and other population-based studies, failed to bear that out (Wolff et al., 2018). She emphasized that her study, which looked at comparable estimates of older adults and caregivers over 16 years, found that caregivers were less likely to experience emotional, physical, and financial difficulty and more likely to be using respite care.
A recent synthesis of the evidence estimated the economic value of caregiving to vary as much as 10-fold, from $63 billion to $642 billion a year—or $1,575–$16,050 of value per caregiver, assuming 40 million caregivers—with the variability driven by variation in the numbers of caregivers and how researchers value their time (Mudrazija and Johnson, 2020). In comparison, the National Family Caregivers Support Program—the flagship federal program—has received approximately $150 million annually with no increase since its inception in 2001. That translates into approximately $4 of support per caregiver (assuming 40 million caregivers). Identifying pockets of excellence, such as the VA, Wolff pointed out “if the National Family Caregiver Support Program is an indicator of research impact, then it is clear we can do far better with respect to our research.”
Wolff noted the gaps regarding interventional studies. As the 2016 National Academies report Families Caring for an Aging America stated, studies involving small samples of family caregivers of people with dementia who are at-risk for negative psychological effects have generated the primary evidence base for interventional research (NASEM, 2016). It also pointed out that interventional research has largely focused on a single primary caregiver and been conducted outside of care delivery and without regard to scaling. In addition, relatively few studies focused on the outcomes and stakeholders that would drive adoption of particular interventions. The
result, said Wolff, is that relatively few caregivers now benefit from the collective wisdom of a robust research base. She also said that the overwhelming majority of interventional research has been focused at the individual and family levels rather than the community, policy, or societal levels (Figure 5) (NASEM, 2021). That type of research would facilitate scaling through employers, health care, or long-term services and supports.
For Wolff, this is the most opportune time for the research, policy, and practice communities to coalesce to increase impact by strengthening the science of family caregiving as a field. In terms of designing studies for impact, she pointed to the need for reporting standards to drive greater transparency and rigor in the published literature and in public discourse. Wolff observed that it is also important that individual studies provide clear and consistent nomenclature, definitions, and internally consistent estimates. Wolff also called for a critical review of the field to assess strengths and weaknesses and identify where to direct future research investments, such as establishing the infrastructure that facilitates surveillance to assess the impacts of policy and practice activities and generating progress related to expanding caregiver supports and services over geographies and providers. She noted that the
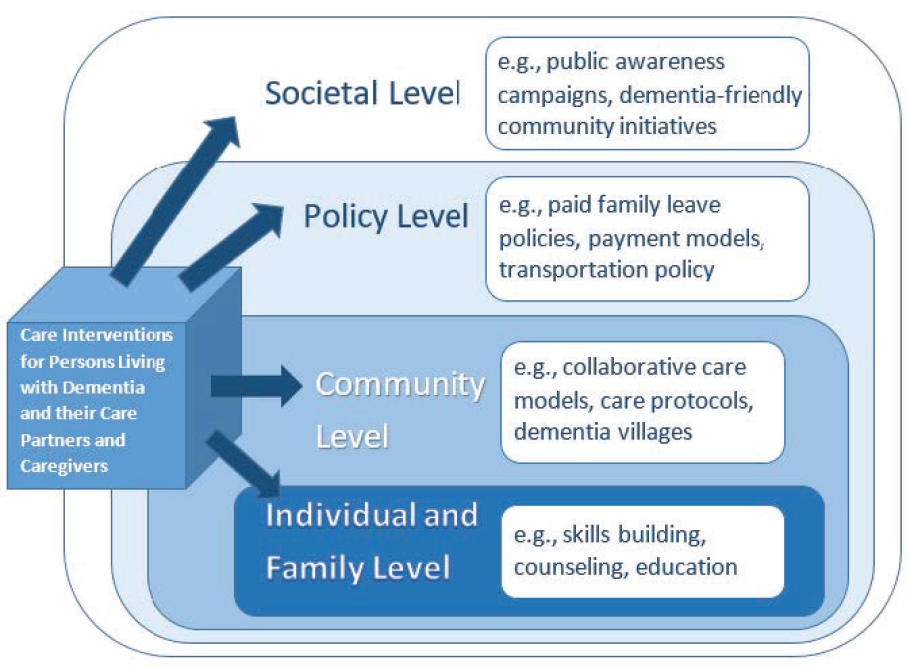
SOURCES: Wolff presentation, May 17, 2022; NASEM, 2021.
RAISE Caregiving Council has made several recommendations (RAISE Family Caregiving Advisory Council, 2021, p. 10).
Wolff highlighted the invisibility of caregivers in the context of care delivery, which creates a significant methodologic challenge. Without understanding how often caregivers are involved, whom they help, what they do, and their capacity and need for supports in real time at the point of care, she said, it is difficult to design and conduct embedded interventions that extend beyond the patient to identify, assess, and support caregivers. To enact transformational change in care delivery, Wolff said, it is imperative to rethink how to go about conducting this research. This requires doing interventional research differently; building new models that involve working directly with care delivery organizations, systems, and communities; and incorporating end users’ perspectives much earlier when designing and testing innovations.
Wolff acknowledged the opportunity to take advantage of existing initiatives and interventional studies. “The cup is half-full with respect to the impact of the [National Institute on Aging]-funded Impact Collaboratory43 and the John A. Hartford Age-Friendly Health Systems44 [Initiative] in developing interventions that are really targeted to subsequent scaling,” she said.
Moving from Silos to Bridges in Research
Erin Kent, associate professor and associate chair of the Department of Health Policy and Management at the Gillings School of Global Public Health, noted that most care recipients face multimorbidity. According to the Health Information and National Trends Survey,45 for example, caregivers who report that their loved ones only have cancer or only have dementia have been less than 6 percent in every survey since 2017. In contrast, 40–50 percent of caregivers report their loved ones have multiple chronic conditions.46 This is important, emphasized Kent, because the latter face increased demands and challenges with care coordination and often increased risk of strain. Yet despite this finding, research funding is siloed by health condition, she said.
___________________
43 See https://impactcollaboratory.org/ (accessed July 18, 2022).
44 See https://www.johnahartford.org/grants-strategy/current-strategies/age-friendly/age-friendly-health-systems-initiative (accessed July 18, 2022).
45 See https://hints.cancer.gov/ (accessed August 5, 2022).
46 See https://hints.cancer.gov/docs/Briefs/HINTS_Brief_40.pdf (accessed August 5, 2022).
Kent pointed out that among the 27 institutes and offices that constitute the National Institutes of Health (NIH) no office of caregiving research exists. Certain institutes, she said, have made significant contributions to research funding and intervention development and testing, and, to a lesser extent, adaptation and implementation of caregiving interventions. However, the lack of infrastructure to cross-pollinate ideas and share data often hinders collaboration and forces researchers to repeatedly develop new interventions and caregiving models. However, said Kent, an increasing number of reports are calling for adapting evidence-based interventions and implementing and sustaining them in practice. “We really need to stop continually reinventing the wheel,” she said.
No single discipline can address the challenges that families with serious illness face, and caregiving researchers know this. The problems are too many and too deep, said Kent. She called for funders to consider transdisciplinary and transinstitutional funding opportunities. Absent establishing an NIH office of caregiving research, Kent would like to see more cross-agency funding opportunities and more public–private partnerships, such as the VA and Elizabeth Dole Foundation collaboration. She called on foundations and professional societies to build deliberate bridges across these disciplinary divides as a means of sharing methods and practices. Kent also called for common data elements across the illness context, which she said will “greatly assist in providing more reproducible, rigorous and comparable caregiving research.”
Similarly, Kent identified an opportunity for gerontology, palliative care, nursing, and condition-specific interests to collaborate on research studies. She cited the second semiannual Building Bridges: Advancing Caregiving Research Across the Lifespan conference on caregiving research (fall 2022) as an opportunity to stimulate such cross-disciplinary research.47 She also noted that the North Carolina Caregiving Collaborative is bringing together researchers, advocates, clinicians, and caregivers to establish a statewide caregiving task force.
Another challenge, Kent noted, is that investigators often omit historically marginalized populations. As Angove pointed out, the barriers and burdens of participating in research are not trivial. Nonetheless, research representation matters, said Kent, if the goal is generalizable conclusions. A 2010 meta-analysis of 29 studies on cancer caregiving interventions,
___________________
47 Additional information is available at https://www.caregiving.pitt.edu/2nd-conference-caregiving-research (accessed January 18, 2022).
for example, found that 84 percent of the caregivers in them were White (Northouse et al., 2010). A 2017 systematic review of 50 cancer caregiving interventions found that 86 percent of caregivers in them were White (Ferrell and Wittenberg, 2017). “We are not really moving the needle on research representation,” said Kent.
Kent referenced a 2020 review of systematic reviews of caregiving for older adults (Young et al., 2020). It presented a model of heterogeneity in caregiving across multiple levels, including the caregiver, the person receiving care, caregiving characteristics, and caregiving context (Figure 6). The review found low to moderate quality for most interventions and a lack of specificity about social determinants of health.
Caregiving research also needs new blueprints. Inclusion, she said, should be the starting point, not the end point. The barriers to participating in research are about time, logistical needs, or cultural divides, said Kent, and investing in strategies to overcome those barriers is as critical as the content of those interventions. Furthermore, researchers need to study and address the social determinants of health and social needs at multiple levels. As an example, her institution has enCompass Carolina, a navigator-assisted program targeted to rural cancer caregivers and designed to identify social support needs and connect them to people and resources. It is an adaptation of the electronic social network assessment program (Reblin et al., 2018, 2022). In a project designed to iteratively adapt this intervention, Kent and

SOURCES: Kent presentation, May 17, 2022; Young et al., 2020.
her colleagues are partnering with rural caregivers and clinicians to make sure it is appropriate, acceptable, and feasible to deploy in a rural context.
Kent called out the lack of public and professional awareness about caregiving. Kent referred to Wolff’s remarks that caregivers often feel invisible. “If you think about it, they are often care-adjacent,” said Kent. “They can be in the same health care delivery system, they can be attending to their loved one as they go through treatment, but their own health needs, as we have heard from many caregivers, often go ignored.” She also noted that caregiving comes as a surprise to many, which is ironic since most everyone will either be or need a caregiver at some point. As the Caregiving in the U.S. 2020 study48 found, more than half of all caregivers did not have a choice in taking on this role.
Kent cited a need to foster more beacons in the caregiving space and recognize that caregivers often do not know where, how, and from whom to obtain resources. Public service announcements would help, such as the Portraits of Care49 and #CareCantWait50 campaigns, AARP billboards, and National Alliance of Caregiving’s caregiver spotlights. She acknowledged the increasing efforts to develop interprofessional family caregiving competencies, but more continuing education on caregiving for health professionals is needed, and emphasizing these competencies needs to start earlier in the educational pipeline. “The notion of caregiving and being a caregiver should not be something that is introduced to someone when they are in the throes of actually doing it,” Kent observed. In closing, she emphasized that the family caregiving field needs more data, more stories, and broader reach.
Research Challenges and Opportunities with Minoritized Populations
In the session’s final presentation, Robinson-Lane discussed research on minoritized populations. She noted that 42 million caregivers are aiding persons over the age of 50 (AARP and National Alliance for Caregiving, 2020), and 11 million are caring for individuals with Alzheimer’s disease and other dementias.51 Pointing out that much of the information about
___________________
48 Available at https://www.caregiving.org/wp-content/uploads/2021/01/full-report-caregiving-in-the-united-states-01-21.pdf (accessed September 28, 2022).
49 See https://www.carecantwait.org/portraits (accessed August 5, 2022).
50 See https://www.carecantwait.org/about (accessed August 5, 2022).
51 See https://www.alz.org/alzheimers-dementia/facts-figures#:~:text=More%20than%2011%20million%20Americans,valued%20at%20nearly%20%24272%20billion (accessed August 5, 2022).
caregivers comes from medical records, Robinson-Lane cautioned that these do not do a good job documenting whether a caregiver is present at a clinical appointment. Moreover, rarely is the patient’s racial, ethnic, or disability status recorded, not to mention the caregiver’s. Specifically, she recognized challenges with noting individuals who are biracial or multiracial, and research often groups all of them together as “other.” Robinson-Lane suggested changing “other” to “another” to humanize groups that cannot be categorized or whose numbers are too small. “We like to collapse groups and because we are concerned with the power or significance of the results, we miss opportunities to examine disparities among particular groups,” she explained.
Robinson-Lane detailed other challenges that arise from under-sampling populations such as Native Americans, Alaska Natives, and other Indigenous people and failing to account for the diversity of many Asian populations. She reiterated previous speakers’ messages that medical records do not capture caregivers’ health status or the multimorbidities of the person for whom they are caring. That information, said Robinson-Lane, would provide a better understanding of the complex needs that caregivers are coping with and how to support them more effectively.
Researchers tend to focus on activities of daily living (ADLs), which include everyday personal care needs, such as getting out of bed, getting dressed, and using the toilet, versus instrumental activities of daily living (IADLs), which include using the telephone, paying bills, and preparing meals. Caregivers from minoritized populations, specifically, Black and Latinx families, are most likely to provide high-intensity caregiving (defined as assistance with at least three ADLs or five IADLs), which results in more overall caregiving hours, said Robinson-Lane.
Robinson-Lane called on organizations that support the design of caregiver interventions to think about how they can be more culturally congruent. For example, the loved ones of Black family caregivers are often diagnosed late in the progression of dementia and more likely to receive a diagnosis of general or mixed dementia (a combination of vascular dementia and Alzheimer’s disease). As a result, studies recruiting caregivers of individuals with an Alzheimer’s-specific diagnostic criterion will automatically exclude a large number of Black individuals.
Racism, socioeconomic status, and other factors, such as geographical barriers, play a large role in driving health disparities, noted Robinson-Lane. One of the most preventable factors, she said, is organizational barriers, policies, and procedures, such as examining a single disease when
choosing populations to include in research. Overall, researchers should be thoughtful about the concept of institutional racism, which refers to policies, procedures, practices, and power structures that center a White frame of reference and assign value and structure opportunities based on race and ethnicity. Institutional racism leads to structuring organizations and considering policies and procedures with the White majority in mind, explained Robinson-Lane. She added that it also prevents researchers from being intentional and thoughtful about how to bring to the forefront some of the needs of minoritized populations, although they may be at the highest risk for disease conditions that research is looking to address.
Robinson-Lane also highlighted the importance of culturally responsive care, which involves organizations examining their communities, policies, and procedures with an appreciation for all the groups they might serve. She observed that a culturally responsive organization adjusts care and practices to meet a certain group’s needs or explains why it cannot. Some negotiation may need to occur when the goal is to maintain the standards of its research practices while also finding a way to be able to deliver more inclusive care.
Referencing the National Standards for Culturally and Linguistically Appropriate Services,52 which the Department of Health and Human Services Office of Minority Health issued almost 20 years ago, Robinson-Lane noted the persistent challenges to putting them into place. Of the 15 standards, two focus on management accountability for ensuring institutions are providing inclusive care and regularly assessing activities to ensure they are providing inclusive care and have internal organizational accountability.
Turning to the importance of culturally responsive research protocols, Robinson-Lane explained that this should involve engaging focus groups prior to launching a study to ensure that the research findings will be appropriate for the groups that the research will involve. “We want to be able to differentiate between the facts about the population that we may presume and evaluate for bias,” she said. For example, a large, national cancer trial looked at population dyads in order to improve cancer pain management, but the study designers presumed that the low-income population did not have access to cell phones. The investigators, including Robinson-Lane, fought hard to get cell phones to all participants, but it turned out everyone
___________________
52 Additional information is available at https://thinkculturalhealth.hhs.gov/clas (accessed September 28, 2022).
already had one. The research team could have avoided wasting time and money by first holding focus groups with the intended targets, she said.
On a final note, Robinson-Lane stressed the importance of targeted recruitment strategies. She pointed out that researchers often complain that they cannot reach the populations they want to study, but they do not invest any money in marketing or work with individuals who know how to reach those populations.
Discussion
Bradley, co-moderator for the session, opened the discussion session with a reference to Angove’s statement that the patient is the gatekeeper. Bradley shared that in her recruiting experience, patient–caregiver dyads have three types of gatekeepers. The first is very protective of the caregiver because they already feel guilty about how much their caregiver does for them, while the second is excited that someone is going to do something for their caregiver and encourages them to participate in the study. The third category is in denial that they even have a caregiver. Given those different views, Bradley asked Angove if she could talk about how to overcome the barriers to create the relationships needed to involve caregivers in research studies.
Angove replied that one way to address this challenge is to bring in community members to provide insights on language to use in the dyad recruitment process. She acknowledged that researchers, including herself, sometimes forget that the language they use internally and in their protocols is not what people in the real world use. “Caregiver” might be one example of a word that a researcher might reconsider, depending on the situation. Angove said her experience has been that if patients and caregivers understand the reasons for a study, the impact it could have, and the improvements that could come from it, they are more open to a conversation.
Wolff said she agreed completely with Angove’s comments about nomenclature and the importance of designing research studies that resonate with the end users. Wolff noted that she has often used different terms to communicate with the institutional review board (IRB) and the project’s funders than she does on the consent forms and enrollment scripts. Beyond that, she said, it is important to recognize that the diversity of different kinds of study designs are going to be crucial to deploy to be able to actually change care delivery. Different designs will also be necessary to recognize both the individuals who are living with serious illness or disability and the
broader set of individuals involved in their care. Some studies about caregivers, for example, might omit a consent form and instead try to collect information in the electronic health record.
Robinson-Lane agreed with Wolff’s comments on thinking about different research designs and added that it is also important to consider various research methods and approaches. Often, she said, researchers tend to minimize qualitative approaches that can provide deep insights into communities, their specific needs, and how they are engaging with systems. Such information is hard to get through large dataset analysis, for example. One approach to achieving inclusive research, she said, is community-based participatory research. The caveat is that this approach takes an incredible amount of time and skill to effectively build relationships with community partners that provide insights into the community’s needs and wants, but it improves research designs and implementation processes.
Wolff observed that the biggest challenge regarding partnerships with community organizations and developing alternative research designs arises from the lack of systematic approaches to understanding who relies on one or more caregivers and the lack of information about caregivers within routine data collection systems. Given that data drive delivery systems, Wolff would like to think about how to reformulate the information systems to better reflect patient preferences and caregiver involvement. This seems like a major challenge, but it presents an important opportunity to drive progress, Wolff emphasized. Kent added that efforts to standardize caregiver data collection efforts have increased, but standardizing what it means to be a caregiver is necessary. “I do not know that we will ever have one just universal definition because there are so many different typologies of caregiving,” said Kent. Bigger wins are possible, she said, when health systems are willing to adopt a standardized set of elements.
Robinson-Lane noted that it is standard practice in hospice and palliative care to collect information on multiple caregivers in the electronic health record. The infrastructure exists to do this, but health care systems need to prioritize enabling this capability the next time they make changes to the records. Angove noted that many caregivers are patients themselves, so one idea would be to capture a patient’s role as a caregiver at their own medical appointments.
In terms of partnering with organizations, Robinson-Lane remarked that it is important to engage community organizations from the beginning of a project, work with them to understand the framing of a particular issue and how they view that framing, and accept that they do not have the
time or budget to engage in projects in the same way that researchers do, so providing resources to them can make a big difference. For example, many community organizations cannot effectively analyze their data, so getting students involved to pull the data together can be a big help. All of this, said Robinson-Lane, comes down to inclusivity and changing power structures, recognizing that community organizations have important knowledge and can make key contributions to the research team. This approach elevates their status and can lead to effective and valuable collaborations.
Angove agreed with Robinson-Lane and noted that her organization engages in partnerships that extend its capacity to analyze research and disseminate its work. Providing funding to community organizations that researchers ask to take on substantial tasks, such as leading the recruitment effort, is important and something the investigators forget when writing their grant proposals. Kent noted the many conversations in implementation science about designing research studies with community partnerships and investment in mind from the start. In fact, she said, it is becoming less likely for implementation science studies to get funding unless they include both in the design from the outset. Kent pointed out that it does take more time for a community organization to start a project than many researchers and their institutions realize. She recommended that if academic institutions want to invest in community partnerships and early career investigators, they need to allow for those investigators to build enduring relationships with the community.
Bradley said she appreciated Kent’s comments because she has found that some of the barriers to community-based research and partnerships with the community stem from her own institution. She asked the panelists if any would be comfortable commenting on what researchers can do to educate IRBs and work with their institutions on ways to pay these community organizations. Wolff said that in her experience, one of the most effective ways of educating the IRB is to provide evidence from the peer-reviewed literature about what other investigators have done and how they have, for example, undertaken dyadic research or research that resembles implementation science more closely, or is more oriented toward quality improvement.
Wolff added that developing the infrastructure of investigators who are poised to lead more implementation science trials is one challenge. Another is that these trials require working within environments that have relatively high-capacity information systems or workflows so that they can actually deploy the intervention. Wolff shared her concern that this requirement
may exclude environments with less resources and create more disparities and inequities.
Robinson-Lane reiterated the importance of paying organizations for their research expenses, perhaps by getting funding for a research assistant to handle data collection. She has found that learning her institution’s rules allows her to work within them to either use an organization’s staff or pay for meeting space within it and then provide incentives in different ways. She also said it is the responsibility of researchers to engage with lower-resourced organizations and help them develop the capacity to participate. Kent pointed out that many comprehensive cancer centers have developed community outreach and engagement cores charged with designing mechanisms for working with and paying participating community organizations. Robinson-Lane added that studies should include funds to reimburse participants for transportation expenses.
Responding to a question about how her team has been able to recruit approximately 200 Black family caregivers of individuals with dementia during the pandemic, Robinson-Lane explained that one strategy was to use social media, which required being thoughtful about which platforms the intended study population uses and engaging experts outside of her domain—and obtaining the funding to pay them and for the campaigns—because the team did not know how to best use social media and marketing techniques. Robinson-Lane added that once the pandemic allowed for in-person activities, the approach was to go to community events to engage families where they are. Her team also reached out to the Michigan Alzheimer’s Disease Center and Michigan Urban African American Aging program to access their registries.
Robinson-Lane noted that while churches are a prime location to reach older Black adults, it is not appropriate to just show up at a church to recruit participants for a research study. Rather, it requires building a relationship first, perhaps giving a presentation for the church’s health ministry or bringing things such as blood pressure cuffs or scales as incentives for individuals to participate. “You have to give back when you are expecting to get something from the population, which is a different approach than I think we have taken traditionally in research,” said Robinson-Lane.
Bradley asked the panelists for their ideas on how to create a culture of research among caregivers. Angove said that when she served on Patient-Centered Outcomes Research Institute (PCORI) advisory groups, one suggestion was to involve caregivers in PCORI’s initiatives as a way to recognize the role of caregivers in patient care. For Bradley, that seems like a nice way to
start being inclusive—adding knowledge about their role in patient care and normalizing and acknowledging them in spaces where researchers are already engaging patients. Kent suggested engaging people early in a serious illness context, perhaps before they identify as caregivers, could be an on-ramp to participating in research. One thing her cancer center is doing is giving out stickers that have a logo and the word “caregiver” on it to bring visibility in the delivery context. This helps caregivers feel represented and visible to the care team, and it also helps them understand that they fill an incredibly important and positive role. “When people start understanding that this is a role that they are playing they may be more likely to want to bring words and share experiences about that role, which then taps right into research,” said Kent. On a final note, Kent wondered why researchers are not figuring out ways to meet potential participants at places where they spend a lot of time waiting around, such as infusion centers. Reaching people in those situations might make them more likely to participate, she said.
Audience Question and Answer Session
Donovan led off the audience question and answer session by commenting that there is a great deal of knowledge about what works for family caregivers in certain settings or with certain populations. She cautioned against requiring every intervention to go through the process of descriptive research to pilot studies to efficacy studies and then to implementation. “I feel like we need to break that chain to say that the research we have done to this point has demonstrated critical elements that we know, probably in combination, need to be done, and it is now up to us to start saying let us start at the implementation level and do good science at the implementation level,” said Donovan.
Donovan noted that the NIH Office of Behavioral and Social Sciences Research has started a rapid-cycle research consortium that is trying to understand how to conduct scientific research alongside implementation, and she wondered about other ways to get findings into practice more quickly. “How do we get our review committees at the national level,” asked Donovan, “to begin to recognize both the value of taking established elements of existing interventions with demonstrated efficacy and trying to put them into implementation, which is a whole different ballgame?”
Robinson-Lane recommended including implementation scientists on the research team to provide the appropriate language and framing for large-scale funding. Wolff noted that the National Institute on Aging has a variety of funding mechanisms that allow investigators to pursue a
smaller-scale pilot project to demonstrate feasibility followed by a subsequent larger-scale trial without having to go back to a scientific review committee. The NIH Collaboratory, Wolff added, has also demonstrated a commitment to building the science related to family caregiving and providing a variety of funding mechanisms for junior faculty to build skills and obtain career development awards.
Angove, speaking from the caregiver perspective, said caregivers need help and support today and that those in the communities she works with are frustrated with the slow pace of science. This underscores the need to embed robust evaluation into ongoing projects to accelerate the process of moving research into practice.
Van Houtven suggested forming an advisory panel as a way to include additional members to the team planning the intervention. In addition to implementation scientists, caregivers, and patients, it is also important to have partnerships within the health system to ensure a chance of adopting a program when the research is complete. Moreover, including a health economist at the beginning of a project can identify implementation cost.
Responding to a question regarding nomenclature and how settling on terms and definitions can play a role in convincing people to pay attention to caregiving, Kent noted that if standardization is needed, it would be helpful to have more federal research funders support such efforts. She believes that the federal government should have an office of caregiving research and policy to set those standards. Angove said she thinks “caregiver” is a great word that should be used more, and normalized and socialized through and for those who are caregiving.
Participant Warren Hebert, from the Home Care Association of Louisiana and an adjunct with the Rutgers Institute for Health, Health Care Policy, and Aging Research, asked about progress made in the discussions about including a family caregiver section in every patient’s plan of care. Wolff cited a major initiative around patient eCare planning led by the Agency for Healthcare Research and Quality and the National Institute of Diabetes and Digestive and Kidney Diseases in conjunction with the Health Level 7 organization.53 Wolff explained that the issue, as she understands it, is that caregiving can change over time, in terms of both care needs and who is in the role. Wolff shared that any attention to creating an entry in the care plan would have to recognize that caregiving is a construct that evolves over time and fluctuates according to care needs.
___________________
53 See https://ecareplan.ahrq.gov/ (accessed August 5, 2022).
Judy Salerno, from the New York Academy of Medicine, emphasized Robinson-Lane’s comment about involving caregivers early in the research process and suggested taking that a step further by co-creating the research proposal with them before submitting it. She also noted the importance of valuing people’s time. Her organization, for example, has a set hourly reimbursement rate for participants. She added that sometimes working with established community members is not the best way to get input from people on the ground with the lived experience you want to capture. Her organization, for example, goes to public housing and talks to tenant associations to elevate the community voice in a different way.
POLICY OPPORTUNITIES TO SUPPORT FAMILY CAREGIVERS
The final session explored policy opportunities to support family caregivers and was co-moderated by Amy Melnick, executive director of the National Coalition for Hospice and Palliative Care, and Rani Snyder, vice president of programs for The John A. Hartford Foundation. To provide background for a moderated discussion on policy opportunities, Susan Reinhard, senior vice president and director of the AARP Public Policy Institute and chief strategist for the Center to Champion Nursing in America and Family Caregiving Initiatives, first explained that policy could be a law, regulation, budget, or executive order and also big, small, or incremental. She noted that despite the clear need to do more in the policy space to support caregivers, she wanted to celebrate the gains in the policy realm, with more to come. She said that more than 200 state laws and regulations affecting some 40 million people are on the books.
As a community health nurse, Reinhard noted that policy is personal, in part because advocacy is a standard practice in nursing. She pointed out that schools of nursing emphasize advocacy and policies as a way of helping not only individuals but groups, communities, families, and society at large. Reinhard shared that she came to realize, as New Jersey’s deputy commissioner of health and senior services, that good policies depend on strong research. She was thinking about programs run by her office for which caregiver eligibility for certain services, such as respite, depended on how many ADL and IADL deficiencies their patient had. However, these qualifications were based on research on ADLs and IADLs that was not designed for family caregivers but rather as measures of functional improvement in people who had strokes and other neurological issues. In reality, these are
often interpreted as measures of the intensity of caregiving, so this serves as an example of a policy decision based on research.
Reinhard pointed to an AARP project, Home Alone, which looked at the tasks that caregivers were doing in the home (Reinhard et al., 2012, 2019). It found that almost half of the more than 42 million U.S. caregivers were performing medical and nursing tasks, with more than a third doing wound care and three quarters providing medication management, including administering injections. Given these findings, Reinhard and her colleagues coined the phrase “medical nursing tasks” to describe what these caregivers were doing.
The advocacy team at AARP thought this research had identified a new problem, but it was an existing problem that had not been named. Naming it, however, had important implications for policy because it gave the advocacy something “new” to talk about that could be used to get policy makers’ attention. AARP developed model legislation and engaged in advocacy work that eventually led to the passage of the Caregiver Advise, Record, Enable (CARE) Act,54 which translated research findings into policy at the federal and state levels (Reinhard and Ryan, 2017). Reinhard noted that 40 states passed accompanying legislation in the first 3 years after the act, and 45 states and territories have now done so.
Using data that defined the scope of the problem and the broad impact on people of all ages, races, and ethnic groups was critical to passing the CARE Act. Reinhard explained that AARP parsed the data so that it was obvious that the challenges of caregiving affected everyone. It also emphasized the huge gap between what caregivers were expected to do and what they are trained for, which helped validate the feeling caregivers had—many were afraid they were going to make mistakes doing something they were never trained to do—and also let them know that those feelings were common and that they were not alone. This work triggered what Reinhard said felt like a movement among caregivers who realized they deserved to receive training.
Reinhard described how this raised awareness led to caregivers telling their stories, which also helped with legislative efforts. In fact, said Reinhard,
___________________
54 The CARE Act requires hospitals to identify and record the name of the family caregiver in the medical record, inform them when the patient is to be discharged or transferred, and provide them with education and instruction on the medical tasks they will need to perform at home. See https://www.aarp.org/politics-society/advocacy/caregiving-advocacy/info-2014/aarp-creates-model-state-bill.html (accessed July 18, 2022).
Oklahoma was the first state to pass CARE Act legislation because of stories, including the governor’s own, soon followed by stories from the sponsors of the legislation. She added that the bill was simple and did not require an appropriation. Reinhard also noted that it offered a policy solution that crossed party lines and actually served as a unifying experience in many states. In fact, many legislators, she recalled, were grateful for the opportunity to sponsor and pass their state’s legislation. The CARE Act, after all, spans social, economic, and geographic divides and applies equally to caregivers in urban and rural areas. “That kind of unifying policy message is very important,” said Reinhard, as was media attention and advocates’ passion. She noted that some state hospital associations were not happy about these bills, but they really could not oppose them; all they could do was withhold support.
Reinhard pointed out that getting states to pass and act on the CARE Act was a joint effort involving many stakeholders and powered by a strong strategy for widespread diffusion that included a shared vision. It was also important that advocates at the state level were flexible and accepted that laws had to reflect each state’s situation while sticking to the main features or pillars of the act. While the result is that some states have stronger laws than others, these laws shine a spotlight on the problem and act as a general call to action that is still motivating action in the few states that have yet to pass CARE Act legislation.
Discussion
In a brief discussion session, session co-moderators Amy Melnick and Rani Snyder asked Reinhard if the states have implemented their CARE Act legislation and how to track if hospitals are complying with it. Reinhard replied that her group has been conducting an environmental scan that includes a research protocol and site visits. One of the first things the team learned was that many hospitals did not know what the CARE Act was. The site visits provided information to the hospitals and added meetings with consumers to disseminate information about the act and what consumers should expect from hospitals. She noted that in Georgia, which had recently passed its CARE Act legislation in April 2022, AARP will be running an implementation campaign in collaboration with local organizations and advocates.
Michael Reese-Wittke, vice president for policy and advocacy at the National Alliance for Caregiving, asked Reinhard to talk about ways of coupling what the CARE Act does with implementation and assessments.
Reinhard said that AARP collects family caregiver assessments as part of its long-term services and supports scorecard, but hospitals are generally still not incorporating these into the electronic health record as standard procedure. She added that CARE Act requirements should be part of state contracts with managed care organizations, which Tennessee has done.
Salom Teshale, policy associate with the chronic and vulnerable populations team at NASHP, discussed its work in tracking implementation of the RAISE Act recommendations, noting that one opportunity for outreach on the state level would be to create family caregiving task forces that could assemble recommendations to submit to their state legislatures. The task forces could integrate the family caregiver voices to ensure that their interests are addressed throughout the process of developing recommendations and not just during implementation.
In terms of exemplars, Teshale said that every state has different populations, needs, and approaches to how it thinks about supporting family caregivers. California, through caregiver resource centers established in the 1980s, is providing a set of services and supports targeted to caregivers of people with adult onset cognitive issues. These centers, which are partially state funded, provide caregiver navigation, assessment, and information about counseling and other supports that can help that specific caregiver population. “That is a nice example of care navigation and assessment that gets at what a caregiver’s specific need is,” explained Teshale.
Reese-Wittke spoke about the National Alliance for Caregiving’s perspective on RAISE Act implementation, particularly in terms of state alignment. He noted that the language in the act is broad and states can interpret the recommendations in different ways. He predicted that the strategy will not be a one-size-fits-all approach. He also said that even before the RAISE Act council formed, state task forces had started creating their own plans for caregiving. Those plans are more granular and more specific about how to implement the recommendations within their state structures. California has its network of resource centers, for example, but other states do not yet have that type of infrastructure.
Devin Plote, policy analyst for clinical innovation at the association of health insurance providers (AHIP), noted that it supports many of the recommendations outlined in the advisory committee’s report to Congress. These include expanding telehealth and technology services to better support and supplement home care, increasing access to and awareness of mental health services and respite services, and implementing programs that address social determinants of health. AHIP also supports increasing
funding for home and community-based services; better incentivizing the direct-care workforce through wage increases, training, and opportunities for career growth; and raising awareness about resources available through advance care planning and programs, such as Medicaid’s Money Follows the Person demonstration project. Plote said that AHIP’s role as an advocacy association is to continue working with policy makers at the federal and state levels to develop programs and legislation that address these goals.
Melnick, commenting on the meager amount of funding appropriated for RAISE Act implementation, asked Reese-Wittke and Reinhard to talk about any efforts to support more funding, given the bipartisan support for the act. Reese-Wittke replied that the funding piece demonstrates the difficulty he sees in the federal landscape more broadly. For example, it took almost a year after passage for Congress to appropriate funding to convene the advisory council and hire support staff. In addition, the act sunsets after 3 years, which the community had to work hard to get extended, given that it took a year to fund the advisory council’s activities.
Reese-Wittke noted the greater opportunity for success at the state level. That is why his organization started to look at what the state task forces were doing and how they were interacting with their legislatures. Getting federal funding to support state implementation of RAISE Act recommendations, said Reese-Wittke, will take a coalition of advocates and the state task forces to decide which parts of the RAISE Act to first seek funding for.
Melnick asked the panelists to comment on the opportunities to use policy levers to improve caregiving policies from the perspective of equity. Reinhard responded that one problem that work on hospital safety scores identified is the difficulty of collecting demographic data. Hospital registrars typically do not ask a patient about their race or ethnicity and simply assume. Since self-identified data on demographics are the gold standard, this is a major problem that the caregiving field will have to address. At AARP, efforts are ongoing to oversample multicultural groups to ensure their representation in its findings. Teshale echoed Reinhard’s comments about data and noted that many states are interested in understanding more about the demographics of their caregivers. New York, for example, evaluated its Alzheimer’s disease caregiver support initiative program using the cognitive and caregiver modules of the Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System55 as a way to
___________________
55 Additional information is available at https://www.cdc.gov/brfss/index.html (accessed September 28, 2022).
better understand the populations the program is serving. Teshale pointed out that certain state Medicaid plans offer self-directed or consumer-directed programs. Such programs provide the opportunity to receive culturally competent care from caregivers who speak the care recipient’s native language, for example, and have an understanding of their cultural background.56
Plote, addressing Melnick’s question about benefit design and other innovations that health plans are considering, said that they are leaning into value-based care and payment arrangements as a form of innovation. Such payment arrangements leverage the work of the entire care team to achieve the improved outcomes that result from whole-person care. In contrast, she said, traditional fee-for-service arrangements do not always recognize the important work of members of the care team, such as the caregiver, outside of the office visit.
In terms of benefit design in Medicare and Medicaid plans, changes being seen include incorporating benefits that address social determinants of health and social risk factors and being able to classify these benefits as medical expenses versus nonmedical or administrative costs. Plote noted that being able to classify services that address social determinants of health as medical expenses creates a much wider pool of funding, since only 15 percent of all premiums paid to health plans can be used for administrative and nonmedical expenses, a policy known as the “medical-loss ratio.” Medicare Advantage plans, thanks to the Chronic Care Act of 2018 and the Centers for Medicare & Medicaid Services’ (CMS) broadening of the definition of chronic care, are able to offer supplemental benefits for chronic illness. These benefits can address social determinants, such as transportation, meal services, home modification, and caregiver support.
For Medicaid, Plote continued, managed care plans use their own reserve funds in addition to home- and community-based services, and long-term services and support, to offer benefits that can address issues related to the social determinants of health. It is up to states to determine what they will reimburse, however, with only 37 states plus the District of Columbia specifically including caregiver support services in their Medicaid
___________________
56 States are exploring how the Medicaid program can support beneficiaries with long-term care needs through consumer-directed care or self-directed programs, for example, which allow family members to be paid for providing care to people in home and community-based settings. For more information, see https://www.nashp.org/wp-content/uploads/2021/04/paying-family-caregivers-April2021.pdf (accessed September 28, 2022).
contracts. Plote noted that AHIP has been developing suggested revisions to data standards and demographic data collection to better align how people self-identify and capture information on their social needs.
Audience Question and Answer Session
Kirch described how, while caring for her brother with lung cancer, her mother with ALS, and her disabled husband, she has had to learn how to handle oxygen and breathing support machines, a bilevel positive airway pressure machine, tube feeding, urinary catheters, dialysis, blood draws, physical and occupational therapy, communication coordination for an organ transplant, procuring the organ donor, and the psychosocial support her two teenage sons need to get through all of this while in school and living their lives. “That is just a short summary of what every day looks like on top of a full-time job, so you can think about the role that I play and the savings that means for the health system,” said Kirch. She commented that none of those savings trickle down to her other than as a tax deduction for medical expenses, which are about $73,000 a year. She then asked about a way to include caregivers and patients at the table as insurance providers think about benefit design. She acknowledged that value-based purchasing can generate savings but emphasized that caregivers do not see those savings.
Plote noted that health insurance providers are trying to craft benefits that can help the caregiver in their daily lives, such as providing respite services, addressing social determinants of health, and advocating for paid leave policies. Reinhard remarked that providing more services to the patient decreases the burden on the caregiver. Kirch acknowledged the challenge of passing money through to caregivers and suggested insurance providers could lower deductibles or out-of-pocket caps to reward them for their services. Kirch called for the community to be more creative about policy development and think about solutions that are simple. “If we are documenting caregivers now, thanks to [the CARE Act], and we are building a strategy, thanks to the RAISE Act, let us now honor what we have learned by developing a policy with the Senate Finance Committee and the entitlement programs instead of just going the authorization route as our next phase,” said Kirch. She also suggested considering social needs navigation in the next phase of policy development.
Asked about any programs at the state level to pay caregivers, as in Minnesota, Teshale mentioned self-directed programs for multiple populations—children and youth with special health care needs, people
with disabilities, and older adults—in various states. She pointed out that Connecticut, Virginia, and Florida are examples of different structures for such programs and how they lay out their payment structure. One consideration within a Medicaid self-directed program, she said, is determining what level of care qualifies for paying a parent or spouse.
A question submitted online by Anny Fenton from the Dana-Farber Cancer Institute asked the panelists to speak to the impact of policies they have supported. Reese-Wittke replied that he and his team are looking at policy options to expand the caregiver support infrastructure into other sectors of health care. CDC, for example, has an infrastructure to conduct population health surveillance that could provide data to understand who caregivers are and where the caregiving field can better develop evidence on how to reach them. He added that opportunities exist to bridge silos and sectors across different health care settings. The public health community, for example, could consider the burden that some caregivers face as a social determinant of health.
Reinhard said that her organization sent requests to the governors’ offices in the states that passed CARE Act legislation to reach out to hospitals and say they expect them to implement this law. Several governors did follow through, and her team needs to do that again. She has also had conversations with the Joint Commission to determine whether it is checking to see if hospitals are implementing state law. This is not policy, but it needs to happen, she said.
Applebaum articulated that it is impossible to overestimate the long-term benefit of linking distress screening with the CARE Act’s provision to document caregiver data. She also was pleased to hear about the recommendation to do that in the home care and hospital-at-home settings. She asked Reinhard about penalties for institutions that do not implement the CARE Act. Reinhard said she did not think any of the state bills included penalties. A few states do incorporate implementation into their survey process, which could result in a fine or penalty. In her opinion, this is more a matter of educating and training staff and hospital administration.
Carol Peden, from the Blue Cross Blue Shield Association, said that insurers are committed to collecting better data to reduce disparity and improve equity. Her organization, for example, released a position paper on the ethical and transparent use of data to reduce disparities (BCBSA, 2022). This is a complicated issue because in some states, insurers are not allowed to ask for race, ethnicity, and language data. Her organization is pushing for a national coalition to align standards to improve understanding of these
disparities and enhance approaches to address them. Peden also noted that the National Quality Forum Measures Application Partnership developed a new rule to collect data related to disparities at the hospital level, which hospital executives could subsequently use to develop a plan to reduce such disparities.57
Jennifer Olsen, from the Rosalynn Carter Institute for Caregivers, asked the panelists to suggest one person or organization that could help advance progress toward funding caregivers. The suggestions included engaging family caregiving advocates or a lobbyist and involving the disability community, which has been incredibly effective at achieving policy change. Suggestions for federal actors included the CMS Administrator, the HHS Secretary and those in Congress who voted against legislative provisions for paid family leave.
WORKSHOP WRAP-UP
Oyer, representing Campbell as well, summarizing points emphasized by speakers and participants, started with research being foundational to policy. Research opportunities include identifying, measuring, and testing interventions that matter most to family caregivers and determining what important facts health systems must know about them. He also highlighted the importance of involving caregivers at the beginning of the design and implementation phases. Equity, eliminating systemic racism, and creating cultural congruity all matter greatly, which means that representation in research matters. It is important, then, to collect caregivers’ self-identified race, ethnicity, and disability status. In addition, the research agenda must be designed to impact society, the community, and policy, as well as individuals. To move from silos to bridges requires involvement of multiple disciplines, institutions, and funders; common data elements, definitions, and terminology; and for the Office of the National Coordinator to issue guidance for the next round of data standards to include information about caregivers.
Regarding policy opportunities, Oyer noted the idea of establishing a caregiver institute or office within NIH. He recounted that the policy solu-
___________________
57 NQF convened a Health Equity Advisory Group on behalf of the Centers for Medicare & Medicaid Services (CMS) to provide input on the measures under consideration with the goal of reducing health differences closely linked with social determinants of health. For more information see: https://www.qualityforum.org (accessed October 14, 2022).
tions need to cross party lines and geographic divides, and strong strategies for diffusion of solutions are required, with flexibility built into policy implementation. Involving the Joint Commission in policy enforcement could substantially affect implementation. Legislation is needed to provide caregiver supports, which the insurance industry supports, and expand telehealth, mental health services, and respite care.
Oyer called out the need for innovative insurance benefit designs through value-based contracting that values the work of the whole team, including the caregiver. Benefit changes could also include provisions that would lower deductibles or out-of-pocket spending caps as a means of compensating caregivers for their unpaid work. Finally, Oyer noted that at the state level, task forces should work to get state funding to implement the RAISE Act.
CAREGIVER REMARKS
Two family caregivers, Dannell Shu and Abena Apau Buckley, concluded the workshop with their reflections. Buckley, who cared for her husband and two small children when he was diagnosed with glioblastoma, started by saying that something that would have improved her caregiving experience and quality of life would have been to have more aligned support from paid case management coordinators. That would have helped her spend less time dealing with health care administration and more time with her husband. When she thinks about the time she spent with her husband, she feels it was an honor to care for him with support from family. She ended up paying out of pocket for the last 6 months of his life for someone to help with chores around the house so that she could spend more time with him.
Buckley emphasized that better compensation for support services is needed. Her grandmother is recovering from a stroke, and the compensation for service providers, such as home health care aids and transportation companies, is so low that employee turnover is high, when services are provided at all. As a result, her grandmother is getting care from people who do not understand her and have little time to spend with her. Buckley is also spending too much time finding people who can provide the support her grandmother needs.
For Buckley, attending this workshop, hearing people talk about the challenges, and getting to meet and talk to people advocating for solutions gives her hope for the future. She shared that she did not even know that
caregiving was a topic being discussed by so many groups. As far as sharing with the professionals in the audience where they might have missed the mark, Buckley said that sometimes the focus is on the details that are important to health care providers but too complex to meet the needs of caregivers and family members. She suggested focusing more on the quality of current efforts to support caregivers and thinking hard about how to more fully incorporate their voices.
On a personal level, being compensated for caring for a loved one is critical. She shared that she was lucky that people at her husband’s and her offices donated hours so that he could be at home and still receive a paycheck. “Not everyone has that,” she said. Creating a caregiver advocate role outside of the insurance company who can help take care of gaps in service is critically important, too, she said. She credited insurance companies for doing their part, but their lens is on the bottom line, which she understands. “We need someone who is focusing on the family members and more funding and accountability for those caregiver support services so that they can do their jobs better,” said Buckley.
Buckley reinforced the need for telling stories and having advocates who can talk about caregivers and bring their perspective to the table. She also called for researchers to think about different kinds of metrics, such as the frustration and suffering that take the caregiver away from their family members, that can help them better incorporate the caregiver perspective in their work.
At the corporate level, Buckley would like to see some way to give companies data showing that if they consider the caregiver perspective and pay for certain services, it would save them money in the long run. At the federal level, she noted that the Biden Administration recently issued an executive order on customer experience that focuses on life experiences as a driver for agencies and departments to start working together, but caregiving is not one of those life experiences. “I would push for caregiving to be one of those experiences because then it would give the authority for you all to get both funding and support for the work that you do,” she said.
Shu said she seconded every word Buckley shared and reiterated the mantra, “Nothing about us without us. Nothing about family caregivers without the involvement of family caregivers,” she said, noting that the workshop had been exceptional in that regard. This needs to be the norm in every piece of research, policy, program, and care setting, she said.
Shu said it is imperative to implement strategies to identify caregivers and to use the intensity index at every clinic session, whether it is at a well-
child check for her son or her annual physical. “Just as the pediatrician documents my child’s height, weight, and body mass index, we need to chart and document those numbers and those scales because caregiving is fluid, and the needs and the intensities are fluid,” said Shu, who added that requires knowing who the caregivers are.
One thing that gives her hope, she said, is this workshop, having these conversations that included caregivers, and repeatedly stressed co-creation with caregivers. Co-creation, she said, makes research, policy, programs, and care stronger. She then challenged everyone to look at their professional schedules over the next 2 weeks and, wherever a patient is involved, to ask themselves where the caregivers, plural, are. Most situations, she said, have more than one caregiver, and it is not always the same person who brings the patient to an appointment.
In terms of where the caregiving field is missing the mark, Shu pointed out the lack of in-depth discussions about respite. Caregivers are drowning, she said, and they need relief now. Another missing piece is support for children and siblings who are caregivers. The Childhood Bereavement Estimation Model58 found that 1 in 13 children under the age of 18 will experience the death of a sibling or parent, which doubles for people 25 years and younger. She noted that with a 4-year-old and a medically complex 7-year-old in her family, the 4-year-old had figured out minor caregiving skills, as the whole household was involved in caregiving.
Shu said researchers need to understand that the conversations she has with other mothers in her situation are qualitatively different from the conversations they are having with health care providers, researchers, and policy makers. She challenged the workshop participants to think about how to bring caregivers to the table together with those who have the authority to take action.
Having given family caregivers the final word, the workshop adjourned.
REFERENCES
AARP and National Alliance for Caregiving. 2020. Caregiving in the United States 2020. Washington, DC: AARP. https://www.aarp.org/content/dam/aarp/ppi/2020/05/full-report-caregiving-in-the-united-states.doi.10.26419-2Fppi.00103.001.pdf (accessed August 5, 2022).
___________________
58 See https://judishouse.org/research-tools/cbem/#:~:text=In%20partnership%20with%20the%20New,the%20time%20they%20reach%20adulthood (accessed August 25, 2022).
ACL (Administration for Community Living). 2021. Implementing the RAISE Family Caregivers Act. Washington, DC: Administration for Community Living.
Applebaum, A. J., E. E. Kent, and W. G. Lichtenthal. 2021. Documentation of caregivers as a standard of care. Journal of Clinical Oncology 39(18)1995-1958.
Azoulay, E., F. Pochard, N. Kentish-Barnes, S. Chevret, J. Aboab, C. Adrie, D. Annane, G. Bleichner, P. E. Bollaert, M. Darmon, T. Fassier, R. Galliot, M. Garrouste-Orgeas, C. Goulenok, D. Goldgran-Toledano, J. Hayon, M. Jourdain, M. Kaidomar, C. Laplace, J. Larché, J. Liotier, L. Papazian, C. Poisson, J. Reignier, F. Saidi, and B. Schlemmer. 2005. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. American Journal of Respiratory Critical Care Medicine 171(9):987–994.
Barlow, J., C. Wright, J. Sheasby, A. Turner, and J. Hainsworth. 2002. Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling 48(2):177–187.
BCBSA (BlueCross BlueShield Assocation). 2022. The ethical and transparent use of data to reduce health disparities. Chicago, IL: Blue Cross Blue Shield Foundation.
Boele, F. W., J. M. Weimer, A. L. Marsland, T. S. Armstrong, C. W. Given, J. Drappatz, H. S. Donovan, and P. R. Sherwood. 2022a. Correction to: The effects of Smartcare on neuro-oncology family caregivers’ distress: A randomized controlled trial. Support Care Cancer 30(8):7041.
Boele, F. W., J. M. Weimer, A. L. Marsland, T. S. Armstrong, C. W. Given, J. Drappatz, H. S. Donovan, and P. R. Sherwood. 2022b. The effects of Smartcare on neuro-oncology family caregivers’ distress: A randomized controlled trial. Support Care Cancer 30(3):2059–2068.
Boucher, N. A., M. Shepherd-Banigan, K. McKenna, R. E. Delgado, K. Peacock, C. H. Van Houtven, M. Van Noord, and N. R. Sperber. 2021. Inclusion of caregivers in veterans’ care: A critical literature review. Medical Care Research and Review 78(5):463–474.
Breitbart, W., H. Pessin, B. Rosenfeld, A. J. Applebaum, W. G. Lichtenthal, Y. Li, R. M. Saracino, A. M. Marziliano, M. Masterson, K. Tobias, and N. Fenn. 2018. Individual meaning-centered psychotherapy for the treatment of psychological and existential distress: A randomized controlled trial in patients with advanced cancer. Cancer 124(15):3231–3239.
Bruening, R., N. Sperber, K. Miller, S. Andrews, K. Steinhauser, G. D. Wieland, J. Lindquist, M. Shepherd-Banigan, K. Ramos, J. Henius, M. Kabat, and C. Van Houtven. 2020. Connecting caregivers to support: Lessons learned from the VA Caregiver Support Program. Journal of Applied Gerontology 39(4):368–376.
Campbell, G. B., M. M. Boisen, L. C. Hand, Y. J. Lee, N. Lersch, M. C. Roberge, B. Suchonic, T. H. Thomas, and H. S. Donovan. 2020. Integrating family caregiver support into a gynecologic oncology practice: An ASCO quality training program project. Journal of Clinical Oncology Practice 16(3):e264–e270.
Chimowitz, H., M. Gerard, A. Fossa, F. Bourgeois, and S. K. Bell. 2018. Empowering informal caregivers with health information: Opennotes as a safety strategy. Joint Commission Journal on Quality and Patient Safety 44(3):130–136.
Choi, C. W., R. A. Stone, K. H. Kim, D. Ren, R. Schulz, C. W. Given, B. A. Given, and P. R. Sherwood. 2012. Group-based trajectory modeling of caregiver psychological distress over time. Annals of Behavioral Medicine 44(1):73–84.
Choi, H., M. Heisler, E. C. Norton, K. M. Langa, T.-C. Cho, and C. M. Connell. 2021. Family care availability and implications for informal and formal care used by adults with dementia in the U.S. Health Affairs 40(9):1359–1367.
Cilliers, P. 1998. Complexity and Postmodernism: Understanding complex systems. London, England and New York, NY: Routledge.
Czeisler, M., A. Drane, S. S. Winnay, E. R. Capodilupo, C. A. Czeisler, S. M. Rajaratnam, and M. E. Howard. 2021a. Mental health, substance use, and suicidal ideation among unpaid caregivers of adults in the United States during the COVID-19 pandemic: Relationships to age, race/ethnicity, employment, and caregiver intensity. Journal of Affective Disorders 295:1259–1268.
Czeisler, M., E. A. Rohan, S. Melillo, J. L. Matjasko, L. DePadilla, C. G. Patel, M. D. Weaver, A. Drane, S. S. Winnay, E. R. Capodilupo, R. Robbins, J. F. Wiley, E. R. Facer-Childs, L. K. Barger, C. A. Czeisler, M. E. Howard, and S. M. W. Rajaratnam. 2021b. Mental health among parents of children aged <18 years and unpaid caregivers of adults during the COVID-19 pandemic—United States, December 2020 and February–March 2021. Morbidity and Mortality Weekly Report 70(24):879–887.
Donovan, H. S., S. M. Sereika, L. B. Wenzel, R. P. Edwards, J. E. Knapp, S. H. Hughes, M. C. Roberge, T. H. Thomas, S. J. Klein, M. B. Spring, S. Nolte, L. M. Landrum, A. C. Casey, D. G. Mutch, R. L. DeBernardo, C. Y. Muller, S. A. Sullivan, and S. E. Ward. 2022. Effects of the Write Symptoms interventions on symptoms and quality of life among patients with recurrent ovarian cancers: An NRG oncology/GOG study (GO-0259). Journal of Clinical Oncology 40(13):1464–1473.
Donovan, H. S., and S. Ward. 2001. A representational approach to patient education. Journal of Nursing Scholarship 33(3):211–216.
Donovan, H. S., S. Ward, P. Sherwood, and R. C. Serlin. 2008. Evaluation of the Symptom Representation Questionnaire (SRQ) for assessing cancer-related symptoms. Journal of Pain and Symptom Management 35(3):242–257.
Donovan, H. S., S. E. Ward, S. M. Sereika, J. E. Knapp, P. R. Sherwood, C. M. Bender, R. P. Edwards, M. Fields, and R. Ingel. 2014. Web-based symptom management for women with recurrent ovarian cancer: A pilot randomized controlled trial of the Write Symptoms intervention. Journal of Pain and Symptom Management 47(2):218–230.
Donovan, H. S., S. E. Ward, M. K. Song, S. M. Heidrich, S. Gunnarsdottir, and C. M. Phillips. 2007. An update on the representational approach to patient education. Journal of Nursing Scholarship 39(3):259–265.
Epping-Jordan, J. E., S. D. Pruitt, R. Bengoa, and E. H. Wagner. 2004. Improving the quality of health care for chronic conditions. Quality and Safety in Health Care 13(4):299–305.
Epps, F., and I. C. Williams. 2020. The importance of religiosity to the well-being of African American older adults living with dementia. Journal of Applied Gerontology 39(5):509–518.
Epps, F., G. Brewster, K. Alexander, J. Choe, V. Heidbreder, and K. Hepburn. 2019. Dementia-friendly faith village worship services to support African American families: Research protocol. Research in Nursing Health 42(3):189–197.
Epps, F., K. Alexander, G. S. Brewster, L. J. Parker, M. Chester, A. Tomlinson, A. Adkins, S. Zingg, and J. Thornton. 2020a. Promoting dementia awareness in African-American faith communities. Public Health Nursing 37(5):715–721.
Epps, F., J. Choe, K. Alexander, and G. Brewster. 2020b. Designing worship services to support African-American persons living with dementia. Journal of Religion and Health 59(4):2163–2176.
Epps, F., V. Heidbreder, K. Alexander, A. Tomlinson, V. Freeman, and N. Williams. 2021. A dementia-friendly church: How can the African American church support families affected by dementia? Dementia (London) 20(2):556–569.
Epps, F., M. Moore, M. Chester, J. Gore, M. Sainz, A. Adkins, C. Clevenger, and D. Aycock. 2022. The Alter program: A nurse-led, dementia-friendly program for African American faith communities and families living with dementia. Nursing Administration Quarterly 46(1):72–80.
Ferrell, B., and E. Wittenberg. 2017. A review of family caregiving intervention trials in oncology. A Cancer Journal for Clinicians 67(4):318–325.
Freedman, V. A., and J. L. Wolff. 2020. The changing landscape of family caregiving in the United States. In Paid Leave for Caregiving: Issues and Answers, 11-30. Washington, D.C.: American Enterprise Institute.
Fried, T. R., E. H. Bradley, J. R. O’Leary, and A. L. Byers. 2005. Unmet desire for caregiver-patient communication and increased caregiver burden. Journal of the American Geriatrics Society 53(1):59–65.
Fried, T. R., and J. R. O’Leary. 2008. Using the experiences of bereaved caregivers to inform patient- and caregiver-centered advance care planning. Journal of General Internal Medicine 23(10):1602–1607.
Fried, T., M. Zenoni, and L. Iannone. 2016. A dyadic perspective on engagement in advance care planning. Journal of the American Geriatrics Society. 65(1):172-178.
Fried, T. R., M. Zenoni, L. Iannone, J. O’Leary, and B. T. Fenton. 2017. Engagement in advance care planning and surrogates’ knowledge of patients’ treatment goals. Journal of the American Geriatrics Society 65(8):1712–1718.
Fried, T. R., M. Zenoni, L. Iannone, and J. R. O’Leary. 2019. Assessment of surrogates’ knowledge of patients’ treatment goals and confidence in their ability to make surrogate treatment decisions. JAMA Internal Medicine 179(2):267–268.
Gore, J., J. Toliver, M. A. Moore, D. Aycock, and F. Epps. 2022. A mixed-methods formative evaluation of a dementia-friendly congregation program for Black churches. International Journal of Environmental Research and Public Health 19(8).
Greenhalgh, T., J. Raftery, S. Hanney, and M. Glover. 2016. Research impact: A narrative review. BMC Medicine 14(1):78.
Guadagnolo, B. A., D. G. Petereit, and C. N. Coleman. 2017. Cancer care access and outcomes for American Indian populations in the United States: Challenges and models for progress. Seminars in Radiation Oncology 27(2):143–149.
Harmon, B. E., S. H. Kim, C. E. Blake, and J. R. Hébert. 2014. Health care information in African American churches. Journal of Health Care for Poor Underserved 25(1):242–56.
Inouye, S. K., S. T. Bogardus, Jr., P. A. Charpentier, L. Leo-Summers, D. Acampora, T. R. Holford, and L. M. Cooney, Jr. 1999. A multicomponent intervention to prevent delirium in hospitalized older patients. New England Journal of Medicine 340(9):669–676.
Inouye, S. K., S. T. Bogardus, Jr., D. I. Baker, L. Leo-Summers, and L. M. Cooney, Jr. 2000. The Hospital Elder Life program: A model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life program. Journal of the American Geriatrics Society 48(12):1697–1706.
Inouye, S. K., D. I. Baker, P. Fugal, and E. H. Bradley. 2006. Dissemination of the Hospital Elder Life program: Implementation, adaptation, and successes. Journal of the American Geriatrics Society 54(10):1492–1499.
Jackson, S. L., R. Mejilla, J. D. Darer, N. V. Oster, J. D. Ralston, S. G. Leveille, J. Walker, T. Delbanco, and J. G. Elmore. 2014. Patients who share transparent visit notes with others: Characteristics, risks, and benefits. Journal of Medical Internet Research 16(11):e247.
Leykum, L. K., L. S. Penney, S. Dang, R. B. Trivedi, P. H. Noël, J. A. Pugh, M. E. Shepherd-Banigan, M. J. Pugh, R. Rupper, E. Finley, J. Parish-Johnson, R. Delgado, K. Peacock, A. Kalvesmaki, and C. H. Van Houtven. 2022. Recommendations to improve health outcomes through recognizing and supporting caregivers. Journal of General Internal Medicine 37(5):1265–1269.
Ma, J. E, J. Grubber, C. J. Coffman, V. Wang, S. N. Hastings, K. D. Allen, M. Shepherd-Banigan, K. Decosimo, J. Dadolf, C. Sullivan, N. R. Sperber, and C. H. Van Houtven. 2022. Identifying family and unpaid caregivers in electronic health records: Descriptive analysis. JMIR Formative Research 6(7):e35623.
Merriam-Webster. (n.d.). Intersectionality. In Merriam-Webster.com dictionary. https://www.merriam-webster.com/dictionary/intersectionality (accessed October 19, 2022).
Morales, L. 2019. For many Navajos, getting hooked up to the power grid can be life-changing. NPR Morning Edition. https://www.npr.org/sections/health-shots/2019/05/29/726615238/for-many-navajos-getting-hooked-up-to-the-power-grid-can-be-life-changing (accessed August 29, 2022).
Mudrazija, S., and R. W. Johnson. 2020. Economic impacts of programs to support caregivers: Final report. Washington, DC: Urban Institute.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Families caring for an aging America. Edited by R. Schulz and J. Eden. Washington, DC: The National Academies Press.
NASEM. 2021. Meeting the challenge of caring for persons living with dementia and their care partners and caregivers: A way forward. Edited by E. B. Larson and C. Stroud. Washington, DC: The National Academies Press.
The National Alliance for Caregiving, Public Policy Institute. 2020. Caregiving in the US 2020. The National Alliance for Caregiving. https://www.caregiving.org/caregiving-in-the-us-2020/ (accessed August 29, 2022).
Northouse, L. L., M. C. Katapodi, L. Song, L. Zhang, and D. W. Mood. 2010. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. A Cancer Journal for Clinicians 60(5):317–339.
Patient Advocate Foundation. 2021. Paving a pathway to engage underserved populations in research: Research Experience Survey results summary. https://static1.squarespace.com/static/616da4e0a5a5080a7f683e99/t/62ccc32e649ee5212116f709/1657586481592/Condensed+Survey+Analysis--June+%2721+.pdf (accessed August 29, 2022).
RAISE Family Caregiving Advisory Council. 2021. Recognize, Assist, Include, Support, and Engage (RAISE) Family Caregivers Act initial report to Congress. Washington, DC: Administration for Community Living.
Ramchand, R., T. Tanielian, M. P. Fisher, C. A. Vaughan, T. E. Trail, C. Batka, P. Voorhies, M. W. Robbins, E. Robinson, and B. Ghosh-Dastidar. 2014. Hidden heroes: America’s military caregivers. Santa Monica, CA: RAND Corporation.
Reblin, M., D. Ketcher, P. Forsyth, E. Mendivil, L. Kane, J. Pok, M. Meyer, Y. P. Wu, and J. Agutter. 2018. Outcomes of an electronic social network intervention with neuro-oncology patient family caregivers. Journal of Neurooncology 139(3):643–649.
Reblin, M., K. J. Wells, A. Otto, R. McCormick, L. Rodriguez, K. Walters, S. K. Sutton, B. Zebrack, P. Forsyth, and M. M. Byrne. 2022. Addressing a critical need for caregiver support in neuro-oncology: Development of a caregiver navigation intervention using eSNAP social resource visualization. Supportive Care in Cancer 30(6):5361–5370.
Reinhard, S. C., C. Levine, and S. Samis. 2012. Home alone: Family caregivers providing complex chronic care. New York, NY: United Hospital Fund.
Reinhard, S. C., and E. Ryan. 2017. From home alone to the CARE Act: Collaboration for family caregivers. New York, NY: John A. Hartford Foundation.
Reinhard, S. C., H. M. Young, C. Levine, K. Kelly, R. Choula, and J. Accius. 2019. Home Alone Revisited. Washington, DC: AARP Public Policy Institute.
Riffin, C., J. M. Griffin, L. Brody, J. L. Wolff, K. A. Pillemer, R. D. Adelman, L. R. Bangerter, S. M. Starks, F. Falzarano, M. Villanigro-Santiago, L. Veney, and S. J. Czaja. 2022. Engaging and supporting care partners of persons with dementia in health-care delivery: Results from a national consensus conference. Public Policy & Aging Report 32(2):58–65.
Roth, D. L., L. Fredman, and W. E. Haley. 2015. Informal caregiving and its impact on health: A reappraisal from population-based studies. Gerontologist 55(2):309–319.
Shah, N. R., and A. Drane. 2021. How health systems can care for caregivers. NEJM Catalyst Innovations in Care Delivery 2(7).
Schulz, R., and S. R. Beach. 1999. Caregiving as a risk factor for mortality: The caregiver health effects study. JAMA 282(23):2215–2219.
Shepherd-Banigan, M. E., N. A. Boucher, K. McKenna, R. E. Delgado, C. Whitaker, L. Christensen, and N. R. Sperber. 2021. Family caregiver and provider perspectives on inclusive care: Aligning needs and expectations. Medical Care 59(11):961–969.
Sperber, N. R., N. A. Boucher, R. Delgado, M. E. Shepherd-Banigan, K. McKenna, M. Moore, R. Barrett, M. Kabat, and C. H. Van Houtven. 2019. Including family caregivers in seriously ill veterans’ care: A mixed-methods study. Health Affairs 38(6):957–963.
Stacey, R. 2001. Complex responsive processes in organizations learning and knowledge creation. Abingdon, Oxfordshire, England and New York, NY: Routledge.
Van Houtven, C. H., S. N. Hastings, and C. Colón-Emeric. 2019a. A path to high-quality team-based care for people with serious illness. Health Affairs (Millwood) 38(6):934–940.
Van Houtven, C. H., K. E. M. Miller, E. C. O’Brien, J. L. Wolff, J. Lindquist, M. Kabat, M. Campbell-Kotler, J. Henius, and C. I. Voils. 2019b. Development and initial validation of the Caregiver Perceptions About Communication with Clinical Team Members (CAPACITY) measure. Medical Care Research and Review 76(6):784–806.
Van Houtven, C. H., V. A. Smith, K. M. Stechuchak, M. Shepherd-Banigan, S. N. Hastings, M. L. Maciejewski, G. D. Wieland, M. K. Olsen, K. E. M. Miller, M. Kabat, J. Henius, M. Campbell-Kotler, and E. Z. Oddone. 2019c. Comprehensive support for family caregivers: Impact on veteran health care utilization and costs. Medical Care Research and Review 76(1):89–114.
Van Houtven, C. H., J. E. Ma, J. Grubber, M. Shepherd-Banigan, K. Lewis, L. Christensen, C. Richardson, M. Kabat, K. Decosimo, K. E. M. Miller, C. J. Coffman, T. Malo, K. D. Allen, and S. N. Hastings. 2022. Systematic identification of family caregivers in health systems: Proposed solutions from a caregiver-focused research study. Journal of the American Geriatrics Society 70(8):2435–2439.
Wang, Y.-Y., J.-R. Yue, D.-M. Xie, P. Carter, Q.-L. Li, S. L. Gartaganis, J. Chen, and S. K. Inouye. 2020. Effect of the tailored, family-involved Hospital Elder Life program on postoperative delirium and function in older adults: A randomized clinical trial. JAMA Internal Medicine 180(1):17–25.
Ward, S. E., R. C. Serlin, H. S. Donovan, S. W. Ameringer, S. Hughes, K. Pe-Romashko, and K. K. Wang. 2009. A randomized trial of a representational intervention for cancer pain: Does targeting the dyad make a difference? Health Psychology 28(5):588–597.
Werner, R. M., and C. H. Van Houtven. 2020. In the time of COVID-19, we should move high-intensity postacute care home. In Health Affairs Forefront. Washington, DC: Project HOPE.
Wolff, J. L., A. Berger, D. Clarke, J. A. Green, R. Stametz, C. Yule, and J. D. Darer. 2016. Patients, care partners, and shared access to the patient portal: Online practices at an integrated health system. Journal of the American Medical Informatics Association 23(6):1150–1158.
Wolff, J. L., J. Mulcahy, J. Huang, D. L. Roth, K. Covinsky, and J. D. Kasper. 2018. Family caregivers of older adults, 1999–2015: Trends in characteristics, circumstances, and role-related appraisal. Gerontologist 58(6):1021–1032.
Young, H. M., J. F. Bell, R. L. Whitney, R. A. Ridberg, S. C. Reed, and P. P. Vitaliano. 2020. Social determinants of health: Underreported heterogeneity in systematic reviews of caregiver interventions. The Gerontologist 60(Supplement_1):S14–S28.
Zaleta, A. K., M. F. Miller, E. E. Fortune, K. A. Clark, and E. C. Kranzler. 2021. HSR21–075: Cancersupportsource-caregiver: Psychometric properties of 2-item depression and anxiety risk screening measures for informal cancer caregivers. Journal of the National Comprehensive Cancer Network 19(3.5).



































































































