Supporting and Sustaining the Current and Future Workforce to Care for People with Serious Illness: Proceedings of a Workshop (2024)
Chapter: Proceedings of a Workshop
Proceedings of a Workshop
INTRODUCTION1
Providing high-quality care for people living with serious illness requires an adequately sized and well-trained and prepared workforce comprising a range of health professions, such as physicians, nurses, social workers, pharmacists, direct care workers, chaplains, and physical and occupational therapists. However, there is a significant shortage of professionals to meet the increasing numbers and far-ranging needs of those who are seriously ill—a shortage projected to worsen as a result of the aging of the workforce and the challenges to health professional well-being (Kamal et al., 2017, 2019; Lupu et al., 2018). These factors underscore the importance of supporting and sustaining the current and future workforce to care for people with serious illness.
To explore a broad range of workforce-related issues, the Roundtable on Quality Care for People with Serious Illness hosted a public workshop, Supporting and Sustaining the Current and Future Workforce to Care for
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop has been prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
People with Serious Illness, held on April 27–28, 2023. This workshop explored strategies and approaches to address major challenges, such as health professional well-being, workforce shortages, and advancing the diversity, equity, and inclusion (DEI) of the workforce caring for people of all ages and all stages of serious illness. This workshop builds on the roundtable’s 2019 workshop, Building the Workforce We Need to Care for People with Serious Illness (NASEM, 2020).
The 1.5-day workshop unfolded across eight sessions. The first session featured a panel of members of the interdisciplinary care team sharing their lived experience caring for people with serious illness, which had been made even more difficult by the COVID-19 pandemic. These firsthand accounts were followed by an overview of the workforce that cares for people with serious illness—who they are, the roles they play, and the challenges they face. The third session examined ways to better support the well-being of the health care workforce. The fourth session featured a discussion on how to create a caring and compassionate environment for patients and those who care for them. The fifth session highlighted an important segment of the workforce caring for people with serious illness: the direct care workforce. The final session explored another key challenge, advancing diversity, equity and inclusion in the workforce caring for people with serious illness.
The second day of the workshop began with a session highlighting several examples of promising models and innovative approaches to workforce recruitment, training, and retention. The final session featured several experts who shared their perspectives on some promising strategies to support the vital work of those caring for people with serious illness.
This Proceedings of a Workshop summarizes the presentations and discussions. The speakers, panelists, and participants presented a broad range of views and ideas. Box 1 summarizes suggestions from individual participants for supporting and sustaining the workforce to care for people with serious illness. Appendixes A and B contain the workshop Statement of Task and workshop agenda, respectively. The speakers’ presentations (as PDF and audio files) have been archived online.2
___________________
2 For additional information, see https://www.nationalacademies.org/event/04-27-2023/supporting-and-sustaining-the-current-and-future-workforce-to-care-for-people-with-serious-illness-a-workshop.
OPENING REMARKS
Peggy Maguire, president of the Cambia Health Foundation, shared that the workshop was dedicated to the late Jared Randall Curtis; before succumbing to amyotrophic lateral sclerosis, he was a pulmonary critical care and palliative medicine physician and a prolific researcher and mentor to many in the field of serious illness care. After receiving his diagnosis, Curtis shared four life lessons: (1) work with people you like or even love, (2) take sabbaticals to recharge, (3) live every day like you have a terminal illness, and (4) focus on what is important and prioritize family (Curtis, 2022). Maguire said that she had the opportunity to interview Curtis after his diagnosis, and he told her that his greatest legacy was the people whose
lives he had touched through his work. “Today, through this workshop, we pay tribute to him by working to improve serious illness care and support the workforce,” explained Maguire.
Brynn Bowman, chief executive officer of the Center to Advance Palliative Care, observed that this workshop takes on a huge and extremely complicated facet of health care, at a time when the broader health care workforce faces serious challenges. Noting that workforce shortages existed well before the COVID-19 pandemic, Bowman pointed out that many have left the field over the past 3 years, and for those who remain, life is not yet back to normal. “There is a lot of lingering trauma, moral distress, and exhaustion that we are still coping with,” observed Bowman. “That really
is the backdrop for all of the conversations we will hear over the next day and a half,” she added.
JoAnne Reifsnyder, professor of health services leadership and management at the University of Maryland School of Nursing, remarked that acute care–based palliative care, community-based palliative care, and hospice care have provided a road map for delivering person-centered and family-centered interprofessional care for people with serious illness. She added, however, that serious illness exists beyond those settings and includes care provided in nursing homes, mental health institutions, pharmacies, homes, and by programs such as the Program of All-Inclusive Care for the Elderly (PACE). “We can learn from our palliative care colleagues about workforce issues, barriers, and successes,” observed Reifsnyder. “In turn, our palliative care colleagues … can learn from folks who are delivering care in other settings to people with serious illness about what we need to do to shore up and sustain our workforce for the future.”
Reifsnyder explained that the term “direct care workforce” refers specially to people at the bedside, such as CNAs, direct care workers, home care workers, and community health workers. Members of the direct care workforce, she said, are underpaid and often need to take multiple jobs to sustain themselves or leave the health care setting. “That is not healthy for them and that is not sustainable for the serious illness workforce,” emphasized Reifsnyder. For that reason, she said, the workshop would examine the system changes needed to enable those critically important individuals to bring their best to their jobs and be recognized for that. In addition, she said, a theme throughout the workshop would be the issues and actions that the health care enterprise has or has not taken to support DEI in health care settings broadly and the serious illness care workforce specifically.
On a final note, Reifsnyder noted that supporting and sustaining the workforce will require radically rethinking, not merely tweaking, the aims of serious illness care and developing innovative solutions to provide serious illness care while ensuring attention is paid to the well-being of the workforce delivering that care. “We know that while some systems might be modified, others will be probably disrupted and redesigned entirely,” she noted. Accomplishing this radical rethinking will require transformational leadership at the micro and macro levels, she added.
VOICES FROM A WORKFORCE IN CRISIS
The opening session featured a discussion moderated by Victoria Leff, palliative care consultant on health care provider wellness and an adjunct instructor at the University of North Carolina at Chapel Hill, about ongoing workforce challenges from the perspectives of members of the interdisciplinary team caring for people with serious illness. Leff opened the discussion by asking John Tastad, chaplain and spiritual care and advance care planning coordinator at Sharp HealthCare in San Diego, CA, to talk about how providing such care over the past 3 years has affected him and his colleagues. Tastad explained that he has been a hospice chaplain for 22 years and is the coordinator for a spiritual care team that works with seriously ill people in palliative care and hospice. In preparing for the workshop, he asked his colleagues to give him an idea of what the last few years were like, and they used words such as “tired,” “worried,” “vulnerable,” “frustrated,” and “impermanence.” Tastad noted that a significant challenge has been dealing with the sense of incredible powerlessness to help anyone in a significant way.
Tastad explained that when providing spiritual care, the best intervention is to be “a kind, thoughtful, and compassionate presence that aligns with the patient’s values, beliefs, and religious perspectives.” This requires “swinging into that context,” and when that is impossible or a barrier is present, caregivers feel tired, worried, vulnerable, impermanent, frustrated, and powerless. He recalled how he was asked to come to a dying patient’s home to administer Catholic last rites, and after donning all his personal protective equipment (PPE), “[m]y glasses fogged up because of the rain and the mask and I couldn’t connect,” said Tastad. “I did my best to behave like a priestly presence that provided comfort to the afflicted and the dying.”
Tastad recounted that after returning to his car, removing his PPE, and driving away, he began to cry and could not stop. The intense emotions, he explained, came from feeling distanced from the person he was there to help and a sense of powerlessness. “I think we’re still feeling that now in serious illness care, probably in some different ways as we deal with staffing issues,” among other concerns, he noted. Tastad concluded by saying he was grateful for the “chaplain seat at the table as the interdisciplinary care team member,” and he asked workshop participants to hug a chaplain that they know.
Sharon Chung, a clinical therapist at the Center for Grief & Loss in St. Paul, MN, explained that they left the hospital setting in the fall of 2020
because, like many social workers, they felt moral injury because of “the lack of moral obligation of many of our health care systems.” Chung explained that this feeling had become “an ongoing sense of perpetuating harm and medical trauma that I was unable to stop or mitigate in my role as a social worker.” Chung described feeling powerless and “devalued by people in positions of power.” Perhaps most heartbreaking for Chung was what they termed the “ableist attitude” about what determined quality of life. This attitude translated into messages that “[i]f someone wasn’t able to walk or talk, then it really wasn’t a quality of life worth saving,” described Chung.
Chung emphasized that in leaving that hospital, they did not resign from health care but rather shifted to a different care setting. In their role as a psychotherapist, they have tuned into the harm, trauma, and the immense grief and loss that they and others feel as health care providers and caregivers for people with serious illness. Chung shared that they were fearful that in leaving the hospital setting, they would step away from palliative care. However, their new role has only deepened and enriched their ability to work on the front lines of serious illness care. Chung explained that about 25 percent of their caseload is health care providers, 20 percent are caregivers of people living with serious illness, and 30 percent are people living with serious illness. Chung shared that they find it enriching to work with all these different groups of people.
Shawndra Ferrell, system clinical manager for advance care planning and shared decision making in serious illness at Advocate Aurora Health in Downers Grove, IL, said she, too, recently left the hospital setting and shifted into an administrative role. She said it was distressing to make that decision because it felt that she was somehow abandoning the hospital she had worked at for nearly 4 years as the sole palliative care provider, both before and during the pandemic. “You develop that care and compassion for the community and for each one of those patients, and then, somehow, when you can’t handle it anymore, you leave,” Ferrell observed, “but it also means you leave them hanging, or at least that’s how it feels.” She pointed out that although no one made it seem like she was abandoning them, she still has that feeling.
Ferrell believes the health care community today is paying more attention to the importance of self-care for health professionals and supports the notion that “it is okay to not be okay.” Although she appreciates that hospitals set aside rooms for staff to take a break, for many overwhelmed by the pressures and challenges, it is impossible to take in positive messages. Ferrell did not realize that she was struggling until she started needing a
break between each consult. “It was getting harder and harder to start over and say the same things with the next group of people as if you didn’t spend 2 hours pouring it all out for the last patient.”
Ferrell explained that she has discovered ways to support communities while not being on the front lines. She tells herself that perhaps she took her previous role as far as she could, and it was time for someone else to take over. Ferrell recalled that the “lightbulb moment” for her was that as much as she and her colleagues care for and take a holistic approach to the patient, it is also important to consider the whole person providing that care. That was what was missing for her and something she did not know how to do. Ferrell said a year after changing jobs, she is still learning that it is important to care for oneself.
Rachel Adams, physician executive director of the palliative care service line at MedStar Medical Group and division chief for palliative care at MedStar Georgetown University Hospital, said her palliative care story dates to her adolescence, when members of her small family began becoming seriously ill, including her father, who died of cancer when she was 18. She recalled many complicated interactions with the health system during her father’s illness. From this experience, she knew she wanted to be a healer and protector. “I wanted to make others feel seen and heard. I wanted to find narrative in moments of loss with patients and families, and I wanted to create space for people to land and feel safe,” explained Adams.
Adams characterized the COVID-19 pandemic as a huge disrupter, causing intense conflict in her roles everywhere she turned. “I was confused about my identity with others and in my physician role,” she said. Before COVID, Adams rarely felt unsafe in the hospital and was never worried about exposing her family to danger. However, she became fearful of in-person interactions with her patients— “the people I meant to protect”—colleagues, and her family. “I wasn’t afraid of my family, but I was afraid for my family. My kids hadn’t signed up to be health care workers,” she explained. This fear for her family’s health contributed to “a time of deep, deep sadness, and it still makes me sad,” Adams noted.
Adams described the experience of one of her patients, an immunocompromised nurse who was admitted with COVID and continued testing positive over a month-long stay. Given her active case of COVID, she was not allowed to see her daughters or have any visitors, which left her feeling depressed and alone. Adams noted that her patient benefited from chaplaincy services, even though the chaplain had to offer prayers from outside her room via video or audio. Eventually, when it was clear that she was not
going to survive, only one family member was allowed to visit. Adams said she is still affected by experiences such as this and the distress that families, patients, and clinicians experienced. A trainee she mentored is still talking about the phone calls she had to make to tell families they could not see their loved one at the end of life.
Another concern that Adams shared relates to the loss of faith in science and medicine and how that is affecting clinicians. She lost a friendship with someone who became deeply opposed to masks and vaccines, even after she told him stories that contradicted his belief that patients dying of COVID would have died of something else anyway. “We continue to express care for one another, but our friendship is irrevocably changed and informed by mistrust,” said Adams, who wonders what this means for the nationwide schism of medical distrust.
Emphasizing that she still loves being a doctor, particularly working in palliative care with interprofessional teams, Adams remarked that “I have beautiful, successful stories about how we overcame barriers during COVID,” she explained, and how “we found novel ways to nourish human spirits.” She is grateful for the knowledge she gained from her experiences during the pandemic, particularly a better understanding of medical mistrust on the part of Black Americans and marginalized communities. She also has a heightened appreciation for health care workers who continue to show up for people in need.
LaToya Francis, a CNA at Inspire Rehabilitation and Health Center in Washington, DC, and nursing student at the University of the District of Columbia Community College, said she appreciated being invited to speak because she feels that CNAs are among the most undervalued workers in health care. She observed that although the other panelists spoke about shifting from clinical care to different positions to protect their mental health or protect themselves physically from COVID-19 or any other disease that might affect them, the ability to make such a change is a luxury that most CNAs do not have. Francis noted that she is constantly worrying about exposing her family to the virus, “which definitely affects my mental health, thinking about what I am going to bring home to my 3-year-old son who is immunocompromised and has asthma.”
Francis noted that she recently stopped working at a facility that was not meeting basic needs for PPE, which put staff in the dangerous position of having to reuse masks and exposing patients to potential infection. “Do you know how that feels on a day-to-day basis? To not be respected that much, to not get clean masks outside every room appropriately as
they should be,” asked Francis. “Hospitals care more about saving money in any way, shape, or form, or trying to monitor people from stealing masks.”
Francis emphasized that this is the kind of trauma CNAs deal with on a daily basis, whether it is not having adequate PPE or being the only CNA on a floor with 16 patients and trying over a 12-hour shift to provide total care without any help turning or cleaning each one. Compounding these challenges is that Francis, a single parent with two children, has great difficulty finding childcare while working two jobs to support her family. As an example, she said she would get off a 12-hour shift at 7 in the morning and then spend a few hours as an employee of a home care company. Even with multiple jobs, she has trouble paying her rent.
Noting that many facilities pay less than $20/hour to CNAs, health care workers charged with caring for patients with serious illness or dementia, Francis pointed out that “CNAs are leaving the field and going to jobs like Amazon, McDonald’s, even Walmart” that are “not as stressful” and “pay a little bit better.” Francis shared how degrading it is to have to tell her children that she cannot afford to get them a treat from the ice cream truck. “The ice cream truck shouldn’t be a luxury for somebody that’s taking care of critically ill people on a daily basis,” said Francis. Her low-paying job has resulted in housing insecurity for her and her children.
Francis explained that with the help of family and friends, she began nursing school in May 2022 to obtain the necessary training to find a better-paying position. Francis pointed out that pay and inadequate staffing affects patient care, noting how important it is to have “two or three more people to work with on a night shift” rather than a facility insisting that staffing is adequate. She remarked, “If we had better pay, we would have better staffing. It goes hand in hand. Get better staffing in these facilities and watch how much better-quality care we can give.”
Panel Discussion
Leff opened the discussion by commenting that she worries that although Francis feels she is not being heard, health care leadership may not want to hear what Francis has to say. Chung emphasized that the sense of trauma and harm the medical system perpetuates for both patients and caregivers highlighted by several of the speakers should resonate with all attendees. “What just strikes me in everyone’s story is that there are layers of loss,” observed Chung. The feeling of powerlessness, sense of abandoning
patients and teams by leaving the hospital setting, and fear of bringing harm home to family members can all feel like a loss, Chung added.
Chung pointed out that one of the biggest falsehoods to come out of the pandemic was the idea of health care heroes. “To think that our strength and our self-care is enough to carry us through is such a falsity,” they said. “I think there needs to be a significant shift from strength-based care to grief-informed and trauma-informed care.” Cultivating resiliency, they said, is informed by the trauma and grief of providers, patients, and caregivers. Focusing on grief and loss creates the opportunity to understand some of the life choices people have had to make that brings them to the place of working with them in a serious illness context. “When we can really see some of the lifestyle choices that people have made through a lens of grief and trauma, it really then allows us to see the whole person, to see the history, the trauma, the legacy of history and loss and trauma that has shaped people to where they are when we are sitting with them face to face,” explained Chung.
Referencing Adams’ and Francis’ remarks about underserved areas and care for patients from underrepresented populations, Ferrell pointed out that every health care system in the country has new initiatives to better address these needs. However, Ferrell questions the data that indicate people are more satisfied with their care and is concerned that surveys are not asking the most appropriate questions that would enable health systems to truly understand patient satisfaction. In fact, she said, she sees evidence that the situation has not improved. For example, she received a call from a patient’s family who started by calling her “sis.” “You hear that, and you immediately understand he’s not looking for the nurse practitioner who’s taking care of his loved one. He is trying to connect to somebody, to the part of me that he hopes looks like him and he is like ‘sis, tell me the truth,’” said Ferrell. Emphasizing the importance of trust, Ferrell pointed out that that person hoped that he could trust Ferrell to tell him the truth, which contributed to her struggle when she left the hospital setting, because she worried that the next person who called looking for someone to trust would not have “sis” around to speak with them.
Ferrell emphasized that those who care for people with serious illness are still in a space where they must find support among themselves. She emphasized that health care was “a broken and imperfect system prior to COVID” and that the pandemic “shown a bright light on all the things we already knew.” Ferrell added: “We’re still doing the work … but the workforce itself is struggling.”
Adams found it unacceptable for anyone to have a job that does not allow them to feel whole or carry out its basic functions. Survival should not be part of the job, she emphasized, so the question is how to do more than survive—to actually thrive. She noted that most nurses she works with graduated only a year or two before yet are already dealing with complex cases. Her worry is that it will be difficult to retain them. “I just think that the workforce right now is really ill prepared to manage some of what they’re facing, and I worry about them,” said Adams.
Ferrell remarked that nurses today are “fighting an entirely different beast” than what she experienced when she first became a nurse 26 years ago. She suggested that a solution is to work in an interdisciplinary team so that one person need not do all the work and new team members will have coworkers to answer questions they might have.
Leff noted that the problems the panelists raised are not new to anyone in health care but were significantly amplified by the pandemic. She hoped that the panelists’ presentations would inform the discussions throughout the workshop and remind everyone of the many areas to which attention must be paid. Leff thanked the panelists for their “courage and vulnerability.”
Audience Q & A
Workshop attendee Allie Shukraft, from Atrium Health, asked the panelists for suggestions on how to help early-career direct care workers who may experience moral distress because of what they view as decisional misalignment between what the patient and family are choosing and what their health care teammates believe they would choose in that instance, particularly if the teammates do not recognize or misunderstand the cultural factors that play into decision making process. Francis said she would keep advocating for the patient and doing her best to serve as the voice of the patient. She also recommended not backing down if told that it is wrong to advocate for the patient, which is something CNAs experience regularly. Ferrell said bedside workers need to advocate for themselves and bring in others, such as a chaplain, social worker, ethics team member, or someone from the risk management office, to help them cope with their distress.
Ferrell emphasized that it is important for bedside workers to remember that they are part of a team and rely on the resources that teammates can provide. “If you can’t get those resources, make somebody listen and ask them to get them for you, because you’re not going to get it if you just
sit there and suffer in silence,” said Ferrell. She added that when moral distress is not addressed, the worker can carry that from patient to patient and from work to home. Ferrell stressed the importance of “advocating for yourself and building a personal team, even if you don’t feel like you have a team.” Adams agreed that relying on team members is great advice. She also said that the palliative care team is often a group that others throughout the hospital recognize as one that will listen to the patient and amplify the patient’s voice.
Tastad noted that groups across the country, such as the California Coalition for Compassionate Care, work to get ahead of the moral distress from the “bedside guessing games” and decision making by holding skillful conversations with patients that inform decision making well before a crisis. In so doing, fewer clinicians have to face the moral distress or trauma that comes from having to make these difficult choices when caring for their patients. Leff added there should be an effort to tell people when they begin this work that it will be difficult and cause moral distress and they will need to work with their colleagues and have support from each other and their institutions. “If you’re not experiencing moral distress in this work, I’m worried about you,” noted Leff.
An audience member from the Norfolk Community Services Board asked what it would look like if panelists’ stories about the challenges they face in their positions prompted action to address those challenges. Francis replied that more facilities would allow for flexible work schedules to accommodate staff that must work multiple jobs to support their families and secure childcare for nontraditional working hours and better training opportunities would be provided for CNAs to grow and have opportunities to advance. She noted that her facility is trying to start a certified medical technologist program that would alleviate some of the nurses’ burden and allow for CNAs or certified nursing technicians to receive a salary increase and career boost. It would also help CNAs gain additional experience necessary for furthering their nursing careers.
OVERVIEW OF THE CURRENT AND FUTURE STATE OF THE HEALTH CARE WORKFORCE
In the workshop’s second session, Bowman provided a broad overview of all different components of the workforce that care for people with serious illness, and the key current and future challenges. She emphasized that although the workshop was not focused on the pandemic, it would be
impossible to have a workshop about the workforce without acknowledging the pandemic’s intense and enduring impact on patients, families and the workforce.
Bowman pointed out that the pandemic drew attention to the existing crisis of health care worker burnout (Surgeon General of the United States, 2022). According to the National Council of State Boards of Nursing, 20 percent of nurses nationwide are projected to leave the profession in the next 5 years (Martin et al., 2023). More than half of all nurses report feeling drained several days a week or every day, with fatigue and burnout most marked among nurses with less than 10 years of experience. “Our nursing workforce has had experiences so distressing and so exhausting and feel so little supported that they’re considering leaving the profession,” said Bowman.
Another stressor is providers’ increasing administrative burden. A national study of office-based physicians found that they spend an average of 1.84 hours a day on documentation and administrative duties outside of work hours (Gaffney et al., 2022). “That is time spent not practicing connecting with patients, not using that hard-fought, expensively gained skillset, but instead putting in administrative time based on a complicated and archaic payment system,” said Bowman. She also pointed to the results of a survey showing that only 45 percent of frontline clinicians trust their organization’s leadership to do what is right for patients and only 23 percent trust their organization’s leadership to do what is right for workers (Medlock et al., 2022). Undoubtedly, she said, these figures correlate with burnout felt by so many health care professionals.
Bowman noted that when considering the serious illness care workforce, palliative care teams and specialists immediately jump to mind; adult and pediatric specialists, home health aides, primary care teams, geriatric teams, family caregivers, staff at long-term care organizations and hospice organizations, and hospital staff are also included. In short, said Bowman, nearly everyone in the health care workforce cares for someone with serious illness at some point.
Bowman outlined the key components of a framework for an optimized workforce to care for people with serious illness:
- Adequate number of people representing the right mix of disciplines to provide the care patients with serious illness need;
- Workforce diversity that reflects patient demographics;
- A workforce that is available when patients need care;
- A workforce appropriately trained to meet patient needs;
- A system that supports the serious illness care workforce by providing the time, space, resources, and support to provide the services needed by those with serious illness; and
- A system that formally and explicitly prioritizes professional well-being.
Reviewing the components of the framework, Bowman cited a significant increase in the number of specialty certified hospice and palliative medicine physicians for both children and adults over the past couple of years. The current figure of more than 7,100 adult hospice and palliative care physicians translates to a ratio of approximately one for every 1,600 patients who might need them. For other professions such as nursing, the situation is even more dire. The pioneering nurses working in palliative care, for example, are starting to retire, but the pipeline has not been backfilled adequately, Bowman stressed.
Taken together, said Bowman, these numbers indicate that palliative care teams are inadequately staffed. According to the National Palliative Care Registry, only 41 percent of adult inpatient palliative care programs across the nation have a full interdisciplinary team, defined as chaplains, social workers, nurses, advanced practice nurses, and physicians (Rogers and Heitner, 2019). Moreover, nearly 20 percent of adult-serving programs do not have a dedicated physician, over 30 percent do not have a dedicated, full-time social worker, and nearly half do not have a dedicated chaplaincy full-time equivalent position.
Data also reveal that palliative care staff are not adequately trained, said Bowman. According to the Palliative Care Quality Collaborative and National Palliative Care Registry, 21 percent of inpatient palliative care programs have no specialty certified staff, and nearly half of registered nurses and advanced practice registered nurses on palliative care teams are not specialty certified. “We see these gaps, and this is alarming because we have a patient population with very complex needs, and we are the line of last resort in many cases,” said Bowman.
Despite the absence of data on the diversity of palliative care workforce specifically, Bowman said it is safe to assume based on health care writ large that the current serious illness care workforce is not as diverse as the patient population. Bowman noted that there are multiple research efforts underway to understand precisely who makes up today’s palliative care workforce and multiple initiatives to attract diverse clinicians to the serious illness care
specialty, but these will take years to bear fruit (Bell et al., 2021; Quigley et al., 2019).
A 2021 survey of 150 palliative care program leaders found that 43 percent of respondents were moderately or extremely concerned about the emotional well-being of their teams, and 93 percent reported some level of concern (Rogers et al., 2022). Bowman found it interesting that 69 percent of their programs had supported the well-being of non-palliative-care colleagues. Overall, she said, despite gains over the last decade, the workforce is not large, well-trained, or well-supported enough, particularly in the face of significantly increasing demand.
Bowman suggested an effective national workforce strategy for palliative care would start by expanding the specialty pipeline of people being trained and certified by focusing on students from preprofessional programs and midcareer individuals who resonate with the work they see palliative care teams providing. This would be coupled with an explicit effort and investment in attracting diverse professionals to the specialty. It is also important to train all clinicians in the core skills of palliative care, given that there will never be enough palliative care specialists to care for every patient. “There is no reason that we shouldn’t be able to provide person-centered care and attention to quality of life in every interaction that patients have with the health system,” said Bowman. A final component of the strategy involves efforts to leverage value-based payment to achieve interdisciplinary care.
Bowman emphasized the importance of providing basic education in palliative care skills for all nonspecialists who care for people of all ages with serious illness. Such basic education would include, for example, how to have a skilled conversation about the individual’s prognosis and understand a patient’s fears and concerns. Education and training are also needed for how to set goals, manage pain and symptoms, and support caregivers. Bowman noted that several institutions do a good job with this type of education in preprofessional clinical education programs.
Bowman pointed out that Aquifer,3 a medical education organization that provides nearly every U.S. medical school with curriculum modules on clinical care topics that have rarely made it into the standard curriculum, is finalizing a palliative care curriculum to which all of its medical school clients will have access. To inform this project, Aquifer staff conducted
___________________
3 See https://aquifer.org/courses/aquifer-excellence-in-palliative-care (accessed September 15, 2023).
focus groups and a national survey of medical students. Medical students, Bowman stressed, want training in palliative care skills in order to
- help them understand the differences between palliative care and hospice to recognize a patient who needs palliative care;
- better manage care transitions, learn how to approach serious illness conversations and navigate patient/family/team conflicts;
- learn about ways to manage pain;
- manage the risks from opioids; and
- understand ways to address the spiritual and cultural concerns their patients might have.
Given this broad range of interest, the problem, noted Bowman, is not that clinicians in training do not think palliative care is important but rather that current curricula do not prioritize it.
Bowman noted that education resources are available and suitable for clinicians interested in basic palliative care education, including material from Ariadne Labs,4 the California State University Shiley Haynes Institute for Palliative Care,5 the End-of-Life Nursing Education Consortium,6 and the Center to Advance Palliative Care.7 Eighteen certificate programs exist nationwide for those who may not have the time, capacity, or need for full specialty training, along with one Ph.D. program offered by the University of Maryland and a variety of continuing education opportunities in communication, symptom management, and other palliative care skills. She noted that most people using the Center to Advance Palliative Care’s educational materials are non-palliative-care clinicians. She explained that the number of people using those materials has more than tripled, from less than 50,000 in 2016 to approximately 175,000 in 2022. Other organizations offering similar materials report the same trend (PHI, 2022). “There seems to be a growing understanding that these skills are important, that we have education gaps, and that they need to be filled,” said Bowman. Nonetheless, she said, most of these education initiatives for midcareer clinicians depend on them being passionate enough to find the educational opportunities themselves or ensuring that their teammates can connect
___________________
4 See https://www.ariadnelabs.org/serious-illness-care/ (accessed September 7, 2023).
5 See https://csupalliativecare.org/ (accessed September 7, 2023).
6 See https://www.aacnnursing.org/elnec (accessed September 7, 2023).
7 See https://www.capc.org/ (accessed September 7, 2023).
with these programs. While a growing number of training programs exist, clinicians are not currently required to acquire such skills, noted Bowman.
Shifting the focus to the direct care workforce, Bowman next explained that direct care workers provide intimate, day-to-day services for individuals with serious illness. Compared to physicians, they are disproportionately female and non-White (see Figure 1) and include personal care aides, home health aides, and nursing assistants across long-term care settings. Their median annual salary is $21,700, with 43 percent relying on public assistance (PHI, 2022). “As a country, we should be embarrassed that this is the case,” said Bowman. “We are undervaluing these positions that provide such critical care to our older and sick [patients] and patients living with disabilities.” The consequence is that turnover was 65.2 percent in 2020 (Holly, 2021).
Bowman noted that the payment landscape is trying to evolve to enable more care being provided through home and community-based services, which will require an even larger direct care workforce. Although that workforce has grown over the past several years, the number of people who need those services has grown faster (Kreider and Werner, 2023). As a result, the ratio of workers to potential recipients has worsened over the last decade, Bowman explained.
Bowman connected the lack of adequate direct care workers to the fee-for-service payment system that prioritizes the work of billable clinicians and limits access to in-home services and nonmedical services, such as personal care and support for social needs that improve patients’ quality of life. In contrast, she noted, a value-based payment system allows for staffing flexibility to better meet social and spiritual needs and pushes care out of the hospital and into the home and community, which has led to the proliferation of independent provider organizations that are laser focused on meeting patient needs at home and avoiding hospitalizations.
Data on supplemental benefits provided by Medicare Advantage (MA) plans indicate that a growing number of MA plans are providing home-based palliative care benefits to their patients (see Figure 2). Bowman pointed out that it is unclear exactly what some of these plans mean by home-based palliative care, and there is no accountability in terms of whether the home-based palliative care services meet national quality guidelines.
Bowman pointed out that within the bifurcated system of traditional health care, more disruptors are aggressively pursuing value. She suggested that this is the “payment tail wagging the care delivery dog.” She further
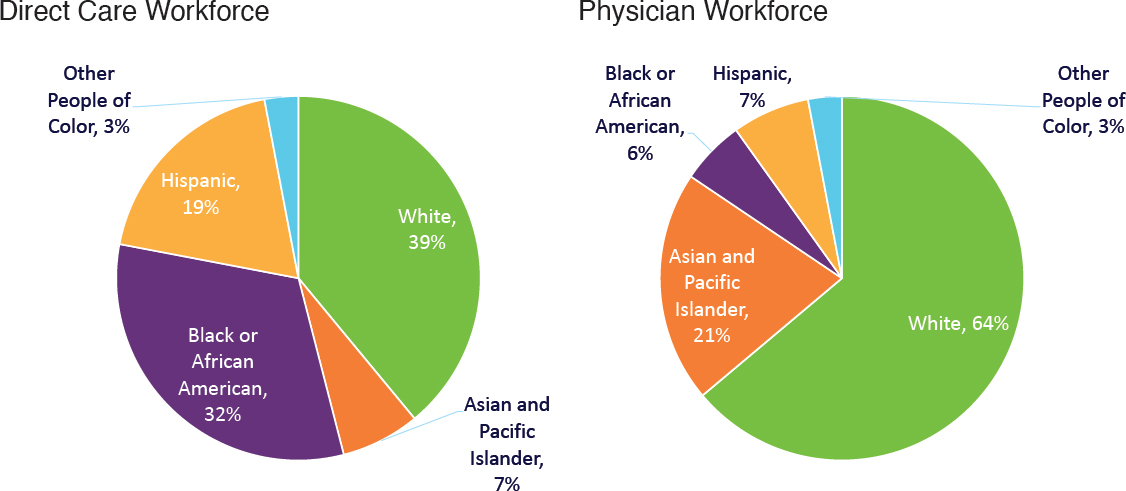
SOURCES: Presented by Brynn Bowman on April 27, 2023 (AAMC, 2023; PHI, 2022).
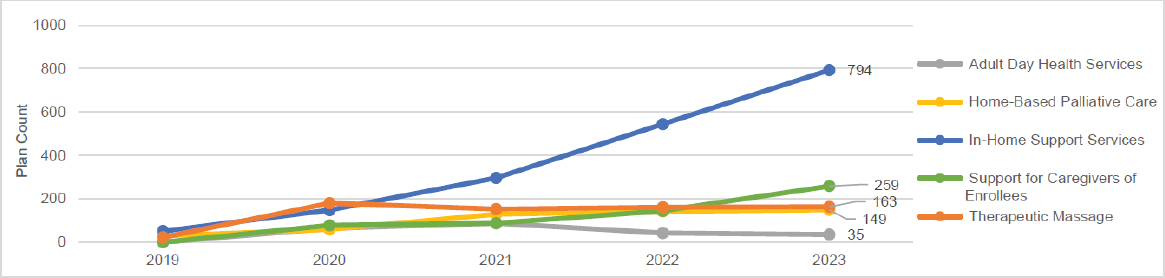
SOURCES: Murphy-Barron et al., 2022. Review of Contract Year 2023 Medicare Advantage expanded supplemental healthcare benefit offerings. Reprinted with permission from Milliman. Presented by Brynn Bowman on April 27, 2023.
pointed out that in a system that provides one set of services to one patient but not another depending on who is paying for their health care, it should come as no surprise that this has led to moral distress and burnout for health care workers.
Turning to policy opportunities to support the workforce, Bowman noted that the Palliative Care Hospice Education and Training Act (PCHETA) would expand the pipeline of people getting trained to be hospice and palliative care specialists. First introduced in 2012 with six cosponsors in the Senate and 39 cosponsors in the House of Representatives, PCHETA has been reintroduced six times. Whether this bill passes and is signed into law is now a matter of prioritization, said Bowman. The Patient Quality of Life coalition and advocates in the field continue to push for it, which would provide funding for national education centers to expand the workforce. Bowman also cited the Resident Physician Shortage Reduction Act, which would offer some loan forgiveness for people to train in specialties experiencing shortages.
Bowman pointed out that at the state level, Illinois HB3571, introduced in February 2023,8 would create a community-based hospice and palliative care professional loan repayment system, which would make it easier for people to opt into these jobs. In Minnesota, SF2786 would provide workforce grants for people working in long-term care. “At the state level, there are options for creativity and for innovation around workforce incentives,” said Bowman.
A growing number of states now require clinicians to engage in palliative care–relevant continuing education to keep their licensure: 39 state-specific requirements on opioid prescribing, 20 on general pain and symptom measurement, and 12 on palliative care, memory care, and end-of-life care. At the federal level, the Medication Access and Training Expansion Act of 20219 requires all providers registered with the Drug Enforcement Agency to complete 8 hours of training on opioid or other substance use disorder by the time they submit their next registration submission. This requirement, said Bowman, should raise the tide on safe and appropriate pain management for patients with serious illness and others.
Although the workforce situation seems dire, Bowman highlighted a few bright spots on the horizon. The Biden administration, for example,
___________________
8 Available at https://ilga.gov/legislation/BillStatus.asp?DocTypeID=HB&DocNum=3571&GAID=17&SessionID=112&LegID=148743 (accessed October 10, 2023).
9 Medication Access and Training Expansion Act of 2021, HR 2067. 117th Cong., 1st sess.
has focused on the direct care workforce, and President Biden signed an executive order that includes measures to improve access to long-term care and bolster job protections for those who work in skilled nursing. One provision attempts to tie reimbursement to worker retention rates in skilled nursing facilities. Several states have increased minimum wage requirements for direct care workers or tied wages to experience in the profession (Abbasi, 2022).
Bowman also pointed out that the University of Pennsylvania has a program that uses a new training model to expand the midcareer palliative care pipeline. This program allows midcareer physicians to complete a competency-based, rather than a time-based, fellowship. This program required the university to get an exemption from the American Board of Internal Medicine. Bowman noted that several states are piloting this program.
Although this is not specific to serious illness care, the health professions are attracting a more diverse group of people, which Bowman said will benefit patients with serious illness. She also noted that health care professionals are demanding better working conditions and better conditions for their patients and in some cases are unionizing (Bowling et al., 2022).
Returning to the framework she proposed for building an optimized workforce to care for people with serious illness, Bowman said none of the six elements are close to being met. As far as what it would take to have an adequate size and mix of disciplines, federal legislation could help widen the pipelines, and local leadership could launch and expand training programs. Diversity is increasing, but Bowman believes it is the responsibility of national organizations focused on palliative care and patients with serious illness to prove to clinicians that this is a good place to work and a welcoming field.
In closing, Bowman emphasized that payment reform is required to have a workforce that is available when and where patients need care, but prioritizing professional well-being does not require expensive investments. “We just have to care,” said Bowman. She shared that what makes her optimistic is that taking steps to support and develop the workforce is feasible. What is required is for bold leadership to look at the health care workforce situation, declare it broken, and then endorse bold solutions to make a difference Bowman concluded.
SYSTEMS-LEVEL APPROACHES TO SUPPORTING THE WELL-BEING OF THE HEALTH WORKFORCE
The third session of the workshop explored the well-being of the workforce caring for people with serious illness. The panelists discussed specific factors that support a happy, healthy, adequately trained, and appropriately prepared workforce. Session moderator Joseph Rotella, chief medical officer at the American Academy of Hospice and Palliative Medicine, opened the discussion by reflecting back on the first session of the workshop, sharing that he heard a “primal scream” from the brave panelists, which called to mind the visual imagery of Edvard Munch’s famous painting.
Rotella said he often hears the “canary in the coal mine” metaphor when people talk about the well-being of those who provide care for individuals with serious illness. In Rotella’s view, the workforce is represented not by the canary but by the coal miners who spend every day in very dangerous conditions. Rotella pointed out that, unlike a dangerous coal mine, the health care system cannot be shut down.
Highlighting the importance of not blaming health care professionals for being what others may view as insufficiently resilient, Rotella emphasized that “[t]he truth here is that really good, strong people get churned up in this current broken system, and we need to focus not on the victims but really on the system that is failing them.” He referred to Leff’s statement that this work will trigger moral distress and burnout. Rotella himself experienced major burnout well before the pandemic even with all the resources at his disposal. He credited nurses, chaplains, and social workers for getting him through this difficult period in his professional life.
Rotella explained that the National Academy of Medicine’s Action Collaborative on Clinician Well-Being and Resilience’s National Plan for Health Workforce Well-Being10 provides a solid framework on which to build efforts to improve clinician well-being. The NAM Collaborative was initiated against the backdrop of rising rates of physician suicide (more than twice as high as that of the general public). Moreover, nearly one-quarter of intensive care unit (ICU) nurses had signs and symptoms of post-traumatic stress disorder (Mealer et al., 2007). The National Plan for Health Workforce Well-Being outlined seven priority areas for health care systems to support the workforce (National Academy of Medicine, 2022):
___________________
10 See https://nam.edu/initiatives/clinician-resilience-and-well-being/national-plan-for-health-workforce-well-being/ (accessed October 10, 2023).
- Create and sustain positive work and learning environments and culture;
- Invest in measurement, assessment, strategies, and research;
- Support mental health and reduce stigma;
- Address compliance, regulatory, and policy barriers for daily work;
- Engage effective technology tools;
- Institutionalize well-being as a long-term value; and
- Recruit and retain a diverse and inclusive health care workforce.
Rotella noted that for organizations that are not ready to take on all seven areas, the consensus is to work on institutionalizing well-being as a long-term value. “Not just because it saves money, not just because we take better care of patients if we are thriving, but because we deserve it,” said Rotella.
Rotella also called attention to the Surgeon General’s Framework for Workplace Mental Health and Well-Being,11 which stresses physical and psychological safety, connection, community to fight loneliness and isolation, work–life harmony, opportunities for growth, and mattering at work. Rotella observed that the last item is about dignity, meaning, and having clinicians realize that they make a difference, concluding that “we can take the whole person approach that we take all the time in palliative care and hospice and apply it to worker well-being.”
Well-Being of the Pediatric Palliative Care Workforce
Rachel Thienprayoon, associate professor of anesthesia and pediatrics and medical director of StarShine Hospice and Palliative Care at Cincinnati Children’s Hospital Medical Center, said that the entire pediatric workforce is caring for children and teenagers with serious illness because the nation is in the midst of an unprecedented mental health crisis in children and teenagers. This crisis has overwhelmed general practice pediatricians, emergency departments, the psychiatric system, and, most of all, parents, many of whom are also clinicians. She noted that the winter of 2022–2023 was terrible in terms of very sick children. Pediatric hospitals were full, and pediatric ICUs nationwide were on diversion status because they were at capacity. Thienprayoon noted that the pediatric workforce is also dealing with gun violence, the leading cause of death among children in the United States.
___________________
11 See https://www.hhs.gov/surgeongeneral/priorities/workplace-well-being/index.html (accessed September 12, 2023).
Thienprayoon noted that there are challenges specific to the pediatric palliative care workforce. As an example, she shared that when she asked these clinicians to name their greatest source of stress and suffering, they said it was the way their colleagues disrespected and devalued them. “It assaults our dignity when a minority of our colleagues do not respect our training and our expertise in the role that we play for families, and we have not grappled with that at this level of the field historically,” she said.
Another source of stress is the tremendous financial strain under which this workforce operates. Thienprayoon noted that the 2018 National Palliative Care Registry survey indicated that 60 percent of pediatric palliative care programs were working beyond their capacity to meet patient needs (Rogers et al., 2021), which still holds today. Working above capacity, she added, is leading to burnout and people leaving the field before it has a chance to grow, creating an ongoing threat to the field.
Thienprayoon explained that compassion means recognizing that another person is suffering, making empathic connections, and acting in a way to relieve that suffering. However, organizational compassion in health care must also account for predictably recurrent sources of suffering for clinicians. She explained that this means measuring and preventing sources of suffering at a systems level, rather than just responding. She noted that the Surgeon General’s model for addressing health care worker burnout at the organizational level is centered on the worker’s voice and equity, with each of the model’s five essential domains based on essential human needs, such as wanting to be valued and having a sense of community and social connection with one’s coworkers. Operationalizing those domains, said Thienprayoon, requires advancing organizational commitment to clinician well-being. She noted that her institution is piloting the Healing Healthcare Initiative developed by the Schwartz Center for Compassionate Healthcare.12 This initiative aims to get organizational leaders involved in clinician wellness at the systems level.
At the team level, research has shown that creating space for debriefing in formal and informal ways is critical to caring for the team, themselves, and others (Leff, 2021). One way her institution focuses on teams is through unit-based Schwartz Rounds.13 “We provide that space for smaller teams to come together and talk about difficult patient situations or just
___________________
12 See https://www.theschwartzcenter.org/hhi/ (accessed September 12, 2023).
13 See https://www.theschwartzcenter.org/programs/schwartz-rounds/ (accessed September 12, 2023).
what we’re talking about here, the stresses of working in health care right now,” said Thienprayoon.
At the individual level, Thienprayoon and some of her colleagues received Stress First Aid14 training, which uses the seven Cs (Nash et al., 2011):
- Check: assess, observe, and listen;
- Coordinate: get help and refer as needed;
- Cover: get to safety immediately;
- Calm: relax, slow down, and refocus;
- Connect: get support from others;
- Competence: restore effectiveness; and
- Confidence: restore self-esteem and hope.
Thienprayoon said the goal is to instill this model throughout the institution’s culture over the next several years. The hope is this will encourage clinical staff to check on one another throughout a normal workday and have the tools to respond in a way that is helpful in stressful times.
Well-Being of the Nursing Workforce
Ernest Grant, immediate past president of the American Nurses Association (ANA) and interim vice dean for diversity, equity, and inclusion at Duke University School of Nursing, referred to the shortage of health care personnel and other limited resources during the pandemic, and asked where those who remain in the workforce can turn for help. He noted the experiences Francis recounted in the first session are what every U.S. health care worker is experiencing today, regardless of the care setting. “Are we using our resources in the right way to help support these individuals or is there something else that we need to do?” asked Grant.
One challenge to addressing staff shortages is attracting and retaining a diverse group of clinicians, particularly young ones. “We need to get younger people and more diverse people to consider a career in health, and the old models that we have been using to try to attract them are failing,” said Grant. With a shortage of approximately half a million nurses, nursing schools are only graduating some 250,000 a year, and not all of them
___________________
14 See https://www.theschwartzcenter.org/programs/stress-first-aid-landingpage/ (accessed September 12, 2023).
will pass the National Council of State Boards of Nursing licensing exam. Further exacerbating the workforce shortage is the fact that nurses and nursing assistants are leaving the field to find more lucrative jobs.
Grant also pointed to the need for employers to provide resources that address the physical and psychological impact on health care team members. He wondered whether employers are listening to what their workforces are saying regarding what they need in terms of support. “The days of the old pizza party, the donuts, the pat on the back, those are long gone,” said Grant, referring to steps health care systems used to consider adequate to support their clinical staff. He recounted that he tells chief nursing officers to actively listen to what their employees are telling them, do something about it, and then let staff members know what steps they have taken to address their concerns. “If a person feels that they have been heard, the most important thing is to keep those lines of communication open,” said Grant.
Grant underscored the importance of developing new models of care. For example, many new payment options include nurses as part of room and board, and others on the clinical team can charge independently for the work they do. “There is something wrong with that particular model,” Grant observed, adding that payment models are even making it difficult for advanced practice nurses to practice at the top of their license and use the skills their education has provided them.
Grant explained that during his last 6 months as ANA president, the organization established a workforce task force to begin to address some of these issues. After conducting nationwide listening sessions, ANA identified six priorities for action: (1) create a healthier and safe work environment, in terms of both adequate staffing at all levels and protecting staff from abusive patients and family members; (2) integrate DEI into a broad range of management functions; (3) create flexibility in work schedules and roles; (4) address burnout and moral distress; (5) implement innovative care models that perhaps integrate technology and other innovations that reduce the time clinicians spend documenting care; and (6) improve compensation programs across the organization.
In closing, Grant shared that he wrote a letter to the Secretary of Health and Human Services in September 2021 asking him to declare the nursing shortage a crisis and bring all relevant stakeholders to the table to address short- and long-term solutions. He is still waiting to hear back. “It is time for us to come together at the table and start implementing these [initiatives] instead of just proposing [them],” Grant concluded.
Well-Being of the Long-Term Care Workforce
Bret Stine recently retired as the executive director of the Keswick Multi-Care Center in Baltimore, which includes a 242-bed nursing center, community programs, and wellness services. Stine pointed out the difficulty with the latter two is that they survive on grants, with no easy way to bring in sufficient revenues to cover their services. Stine noted that the center also receives funding from the largest foundation in Maryland devoted to supporting older people, allowing it to develop resources that other long-term care facilities cannot afford and continue operating despite losing money operationally. Stine pointed out that the daily rate at Keswick is $600, and few people save enough money to support themselves in long-term care for even 6 months, let alone 2+ years; it is largely funded by Medicaid and Medicare, which, in Stine’s view has created financial challenges for those running such programs.
Stine explained that the changes in resident acuity require more staff overall and enhanced skill levels among staff. Some residents, for example, may have complex medical conditions that require five people. Stine called for reinstating timed studies to provide an accurate reflection of the time required to care for each resident to determine whether staffing levels are sufficient. He also raised the need to be more creative with scheduling and training. For example, staff have mandatory training they must repeat annually. “I would argue with you that a 10-, 15-, 20-year employee, and those are getting harder to find, does not need to hear the same session on residents’ rights every single year,” noted Stine.
In terms of workforce shortages, Stine noted out that social workers are in short supply in long-term care facilities. Characterizing them as more valuable than ever today, Stine observed that many social workers are leaving long-term care out of frustration with overburdensome regulations or having to serve as quick discharge machines for patients undergoing rehabilitation. On a final note, Stine explained that due to hospital staffing shortages, “patients that should be on palliative care” are being sent to long-term care facilities.
Well-Being of the Clinical Workforce in Rural Areas
Patricia Fogelman, medical director of palliative medicine at Nittany Health/Mount Nittany Medical Center in State College, PA, pointed out that a key aspect of health care in rural areas is that although geographic
coverage space is often broad, population density is often lower. She noted that this means that patients are traveling 1–2 hours to a hospital, whether that is a 30-bed critical access facility or a medical center such as hers. Geographic coverage space also affects organization’s resources. “It is hard to try and do community-based palliative care delivery when nurses may have to travel 200 miles in a day to just see four patients,” she said.
Fogelman explained that when the pandemic began, it became evident that preserving her organization’s four-person palliative care team—herself, two nurse practitioners, and a social worker—was critical. Fogelman did this by shifting to time-limited rotations of 2 weeks in the ICU, which proved to be the sweet spot between 1 week, which was too short to build relationships, and 3 weeks, which was causing burnout. In addition, staff had daily meetings to check in with one another regarding workload and patient case intensity, and if someone was having trouble, someone else would help out. Weekly lunches gave staff time to have longer, more informal interactions and to try to normalize life to some extent. “We could hear about our social worker’s wedding planning or the one nurse practitioner, who was my new hire, had a very sassy 5-year-old that she was happy to entertain us with stories about,” said Fogelman.
Acknowledging the strong opinions both for and against technology, Fogelman stressed that in rural health care settings, it is imperative to leverage whatever can help bring people closer to each other and help families feel connected and engaged. As the pandemic worsened, her hospital had a no visitation policy for those at the end of life that she and her colleagues said was unacceptable. With critical care and medical leaders, they worked out a compromise that allowed 1-hour visits from family members. Fortunately, noted Fogelman, the hospital had sufficient PPE to support that compromise.
Fogelman explained that her team also began providing iPads at the bedside. She initiated a fundraiser on her social media accounts, receiving a donation of 50 iPads from a local Verizon store, and the chief information officer was able to assure existing hospital iPads were in use and available through the COVID units. Her efforts ensured a bedside iPad for every patient in the hospital, and her team started scheduling iPad visits with families. The rationale, Fogelman explained, was to prioritize connections and the humanity that must come first in medicine.
Fogelman explained that interdisciplinary rounds, which included her and a critical care team member, ICU social worker, chaplaincy, and bedside nurse, became standard during the pandemic and served to streamline the
process. “We were able to hit the high notes of each point, each patient, identify what their needs are, and then focus our next couple of hours on those family meetings and things like that,” said Fogelman. With grant funding, Fogelman and the team’s social worker also built a palliative care resource library with materials recommended by the American Academy of Hospice and Palliative Medicine. The library served as an important repository of supportive resources to patients, caregivers, and even children.
Fogelman said the accomplishment she is most proud of is increasing the awareness of the impact of COVID on all those who work in a health facility. She described how, in partnering with the chaplain, she launched a systemwide COVID support group that meets once a week, including nurses, food service workers, and those workers who keep the facility running. “I think we lost perspective for a little bit about how deeply [the pandemic] affects all of the members of the health care team,” said Fogelman.
Panel Discussion
Rotella opened the panel discussion with the observation that he found himself connecting the dots between the well-being of clinicians and taking good care of patients. “If you want clinicians to be happy, make sure you are taking good care of their patients,” remarked Rotella. “If you want CNAs to feel rewarded, make sure that if it takes five CNAs to take care of a patient, that there are five CNAs.” Fogelman agreed and said that whole-person care does not start and stop with the patient but extends to the entire system of caring around them. Stine mentioned a need for more refined training for health care workers on ways to be more empathetic and sensitive, and deal with conflict, given that patients are not always at their best. Providing that training helps staff morale and helps health care workers develop a stronger bond with the people for whom they are caring.
Fogelman commented that most students are not receiving this type of training, so new hires do not have a framework or the knowledge to guide them. Her organization is implementing such training in palliative care and basic communication skills. This is very important, she explained, because failing to equip the people who spend the most time at the bedside—nurses and other care partners—with these skills and some empowerment means that they will not function well, which will lead to patient dissatisfaction with care.
Rotella pointed out another key theme was the importance of human connection. For example, while “sympathy pizza [parties]” are not the solu-
tion to boosting employee well-being, staff gathering routinely for lunch was effective. Similarly, acquiring iPads was not magic, but using them to foster human connection was. He asked panelists to expound on how they infuse humanity into their daily workflow, whether as an individual, team, or organization. Grant replied by citing Madeleine Leininger’s culture of caring theory, which emphasizes that culture and caring are essential concepts in nursing (Busher Betancourt, 2015; Lancellotti, 2008) and that if one is to be involved with the patient or community, they must be part of the community. In addition to having a caring culture, it is important to have a culture where everyone’s needs and thoughts are appreciated and addressed when moving forward as a team. “It’s like an all-for-one and one-for-all type of a situation,” explained Grant.
Thienprayoon said she worries that medical training for both physicians and nurses can be dehumanizing. She recounted how she was surprised when her brother, a radiology resident, sent pictures of him holding his newborn son, given the culture of medical training demands that residents go right back to work. In her view, medical training strips away compassion and isolates one’s identity as a physician, pharmacist, or nurse in a way that when that identity is threatened, it threatens one’s core as a human. “We cannot show up for patients if we do not feel like full human beings,” cautioned Thienprayoon.
Stine shared that his organization initiated a committee for culture change and found it to be difficult work. A survey the committee conducted found that staff loved the way the organization handled COVID-19 and felt safe but did not think that management listened to or cared about them until the pandemic struck. The most important finding from that survey was that despite the challenges the pandemic triggered and the burnout that accompanied it, almost 100 percent of the staff reported that they felt that what they do is important. Input from feedback groups provided a glimpse of the staff’s social challenges, so the organization partnered with the Dwyer Foundation, which provides wraparound services for people whose social disadvantages prevent them from coming to work. For example, a staff member’s abusive boyfriend broke her home’s door down, damaging the hinges, and she did not want to leave her children. The foundation sent a carpenter who installed a new door and lock.
Rotella asked the panelists how they create significant change when they are not in a top leadership position. Fogelman said she has learned that it is better to ask for forgiveness rather than permission. In keeping with that lesson, Fogelman—without consulting her organization’s leadership—
pulled together a three-person team to provide a quicker, more agile response to patient needs. She also noted that her organization’s systemwide support group got started because of what she was seeing in her day-to-day interactions. The key point is to consider ways in which to make an impact or solve a problem and then act.
Thienprayoon explained that she launched several activities to affect clinician experience and was exhausted from the efforts and felt she was not making significant progress. “It is hard to advocate from the middle or not from the top,” she said. Importantly, in the wake of her exhaustion, colleagues picked up the torch and applied to be a pilot site for the Healing Healthcare Initiative. Thienprayoon argued that the approach should be to do what one can but to protect oneself at the same time. She also noted how stories from individual staff members can make a profound difference, though it often takes patience to see signs of change.
Stine emphasized the importance of leadership getting to know each staff member as an individual person beyond their professional role and how that contributed to staff feeling more connected. He also stressed that it is critical to take time to explain to those whom the change will affect why it matters. For Grant, this comes down to actively listening and keeping the lines of communication open, to take the time to explain why doing things in a certain way is important. Thienprayoon added that system leaders deserve compassion, too.
Fogelman commented that acts of kindness function like “doses of spiritual care,” so any way to bring that idea into one’s daily activities will be helpful for sustaining well-being. She recalled how she had a partner in pulmonary critical care who thanked every single person as she would walk out of the hospital, regardless of who they were. When asked why she did this, she replied that every coworker needs to know what she sees in them, what she values in them, and that she appreciates the job they are doing. Fogelman said that was such a profound message that she now makes a point of doing the same thing. Similarly, Grant recalled that the CEO of a hospital system he worked at would make rounds day and night and ask staff how they and their family were doing. Everyone who worked at the hospital, regardless of position, felt they could talk with the CEO.
Rotella, referring to Thienprayoon’s statement about the need to change medical education, agreed there is too much “hero narrative” in training, with the hero being the person who takes 10 admissions at night and then goes to the operating room and sews up an aortic dissection, only to be right back to admitting people. The hero, he noted, is never the person who takes
a mental health day. Given that, he asked the panel for their ideas on how to deal with cultural programming that makes people feel like a failure if they take care of themselves. Thienprayoon responded that leaders should model healthy behavior and set a tone that their organization supports staff self-care efforts, and people must model that behavior to one another and give each other permission to be more than a doctor or nurse.
Grant shared the belief that sometimes one must save oneself from oneself. “You do have to give yourself permission to do that, otherwise moral distress and everything else just piles on, and it affects you not only physically but psychologically as well,” explained Grant. “We are not doing ourselves or those that we care for any good when we do not pay attention or listen to our body.” It is important to not feel that one is letting others down when taking care of oneself.
Stine agreed, saying it is key for leaders to demonstrate that behavior. “We do not do enough to encourage our staff to take time off because we are constantly battling with the schedule, but burned-out people cannot do their job. Tired people can’t,” said Stine. He added that he finds it interesting that truck drivers are regulated regarding the miles or hours they can work, but health care workers are expected to work 24 hours a day, 7 days a week.
Rotella asked the panelists what they would do if they had a magic wand to make one thing happen immediately and one thing that would be a first step in the right direction. Fogelman said she would implement palliative care education into undergraduate curricula across disciplines to ensure that graduates had at least the basic tenets. Her first step would be to build palliative care training modules for physicians and advanced practice providers and implement a curriculum for her institution’s family medicine and internal medicine residency program and nursing internship program.
Stine noted that he would improve morale and satisfaction by supporting family members having a difficult time dealing with the inevitable. Going forward, he noted the need for palliative care teams to address religious and ethnic and cultural issues when working with families given the nation’s increasingly diverse population. Stine noted that education is key to having happier staff who will stay in the field. Grant said his magic wand would restructure health care so that everyone had equal access to palliative care. Thienprayoon said she would put the patient back in the center of the clinical experience, which requires decreasing the time clinicians are required to spend in the electronic health record.
Audience Q & A
Kashelle Lockman, a palliative care pharmacy specialist at the University of Iowa College of Pharmacy, noted that although community pharmacists provide palliative care to people living with serious illness, most palliative care teams do not yet include pharmacists, despite research indicating that doing so improves the quality of care (Cortis et al., 2013; Malotte et al., 2021). She added that 26 percent of the 35 pharmacy residency positions in palliative care and pain management did not fill all of their open slots in 2022, and burnout may be part of the reason. Coordinating medication across providers is an important role for community pharmacists and contributes to burnout, which will affect access to care, particularly in rural areas.
Lockman asked the panel for thoughts on what can be done as an interprofessional coalition to solve the problem of burnout. Rotella replied that the National Academy of Medicine’s Action Collaborative is a crosscutting group that includes pharmacy organizations as active members. “In that particular collaborative, the voice of pharmacy was as strong as any other,” said Rotella. Thienprayoon said the Pediatric Palliative Care Task Force includes pharmacists among its interdisciplinary members. It is considering conducting a field-level burnout survey that would include all professionals who care for children with serious illness. The goal would be to feed the results to professional organizations, including those for pharmacists, to help them develop the right interventions to support each different role on the palliative care team.
Reifsnyder asked the panelists for the actions they would recommend if they had the ear of their organization’s CEO. Fogelman said she suggested to the leadership of her organization during the pandemic that it offer a meal that staff could take home at the end of their shift to eliminate one thing that they have to do after a long day at work. Stine said his organization does the same thing. To alleviate shortages, he would suggest offering vocational training and reaching into high schools to promote interest among students in joining the field.
Grant remarked that if he had access to organizational leadership, he would bring a list of problems and possible solutions, which he hopes would open a dialogue that could lead to action. Thienprayoon said she published a piece about being burned out, and it quickly found its way to her organization’s leaders, who contacted her to see if she was all right. “That reminded me that I was cared about as a human being,” she said. The
important thing, she said, is to speak the truth about how one is doing and to do it in a language of suffering rather than burnout. Grant added that it is crucial to remember that everyone experiences burnout and moral suffering differently, making it imperative to have one-on-one conversations to determine the key issues that are having the biggest impact on each individual and what can be done to best help them.
An unidentified participant asked Grant how the different professions could provide a pathway for individuals to enter the field that can also support them financially. Grant replied that the North Carolina Institute of Medicine’s Nursing Workforce Task Force is exploring whether scholarships would provide an avenue for CNAs, licensed practical nurses, and medical office assistants to move into a registered nurse role. Grant noted that Congress is considering providing more funding for nursing faculty and clinical sites as one step for increasing enrollments in nursing schools. Some schools, he said, are offering weekend and night courses for existing staff, but that is a slow process.
Grant suggested that outreach efforts to promote nursing as a career should be extended to elementary schools. Another organization he belongs to, for example, has adopted a third-grade class for which he volunteers about once a month. “They see this 6'6" Black guy and they say, ‘he’s a nurse?’ Maybe I can be one, too,’” said Grant. “You get them thinking along that path.” He has also been talking with the Boys and Girls Club of America about inviting diverse nurses into their programs and promoting the concept that nurses do make a difference.
CREATING A COMPASSIONATE, CARING ENVIRONMENT FOR PATIENTS AND CLINICIANS
The fourth session of the workshop featured a conversation among Beth Lown, chief medical officer at the Schwartz Center for Compassionate Healthcare, JoAnne Reifsnyder, and Donna Stevens, palliative care and leadership consultant and cofounder of Leaderly Consultants. Lown opened the session by remarking that the workforce is not only burned out but suffering from anxiety, depression, the symptoms of post-traumatic stress disorder, suicidal ideation, and even heartbreak. “I think that the systemic issues, [such as] the financial structures that prioritize volume over patient centeredness, strain our sense of calling and our sense of professionalism, and it breaks our hearts,” said Lown. “I think that is partly why people are leaving in droves.”
Lown explained that her organization was founded on the premise that care of the caregiver was essential to compassionate care. She shared that the founder, a health policy and health law attorney who died from lung cancer, had realized that exquisite moments of compassion and small acts of kindness made the unbearable bearable; he asked his family to start a center to ensure that compassion would not be extinguished from health care.
One of the first programs the center started was Schwartz Rounds, which Thienprayoon had mentioned in the previous session. Schwartz Center staff instruct others how to implement Schwartz Rounds and teach facilitation skills that can create what Lown called “courageous space[s]” that allow people to talk about what it is like to care for patients and their families day after day, have tough conversations about their experiences and how to deal with them, and share stories of joy and conflict. Lown noted that research shows that Schwartz Rounds increase a sense of perceived or felt compassion, teamwork, and the ability to put oneself in their coworkers’ shoes. Research also found that people who participate in Schwartz Center rounds, compared to people who do not, score significantly lower on the 12-item version of the General Health Questionnaire, indicating lower levels of psychological distress (Dawson et al., 2021; Maben et al., 2018).
Lown explained that the U.S. National Center for Post-Traumatic Stress Disorder (NCPTSD) developed Stress First Aid.15 The Schwartz Center collaborated with NCPTSD to offer Stress First Aid as a self-care and peer-support program to Schwartz Center members.
Turning to the other panelists, Lown asked Reifsnyder to share stories from the front lines that illustrate the emotional distress of health care workers. Reifsnyder noted that from 2012 to 2022, she led a large company providing skilled nursing and long-term care at some 300 sites in 25 states, and it was the hardest job she ever had. Early on in the pandemic, one site had a COVID-19 outbreak and started receiving threats that frightened staff. Though she ordered security to be put into place, this was the beginning of dealing with anger prevalent in many communities across the country. It was also clear that direct care workers, such as Francis and others in skilled nursing facilities, were not seen as heroes and were being blamed for spreading the virus.
Reifsnyder described the tense situation for staff who were the ones holding dying people’s hands, afraid for themselves and their families, while
___________________
15 See https://www.theschwartzcenter.org/media/Stress-First-Aid-Self-Care-Organizational-NCPTSD10.pdf (accessed September 12, 2023).
being blamed. “What became clear within the first several months to me and to others I was working with is that the trauma of this was going to take a long time to heal,” said Reifsnyder. “We did not know what recovery was going to look like, but we thought it better start now, and put [the first] Stress First Aid [program] and some other structures in place to try to help people get through” that difficult time.
Reifsnyder stressed that that although the public health emergency has been discontinued, COVID-19 is not over for people working in skilled nursing facilities. She pointed out that every skilled nursing and long-term care facility today would report that it is struggling with staffing, even as it has returned to prepandemic levels at hospitals and ambulatory care settings. “There is still a lot of work to be done there; not only are they not healing from the trauma, [but] there are [also] not even enough of them. It was soul crushing to them,” said Reifsnyder. Lown remarked that so many health care workers did their best under the most difficult conditions during the pandemic, which was admirable, inspiring, and courageous. She noted that these same workers are being retraumatized continuously by the systems in which they must function.
Stevens, who led the Lehigh Valley Health Network palliative care team for 16 years, pointed out that the network was an early adopter of palliative care concepts. It also started one of the first palliative care inpatient units in the nation and one of the first home-based palliative care practices at a time when most people were not familiar with palliative care. The goal was to optimize advanced complex illness support through a systemwide palliative care structure.
Stevens traced the impact of the pandemic on staff, beginning with the initial phase when the team was wanted, needed, and appreciated. Then came the second surge, she explained, characterized by anger over vaccines and vaccine hesitancy and the lack of visiting hours for loved ones. During that time, calls for Schwartz Rounds increased significantly, with staff experiencing the extraordinary need for a release valve for all of their emotions. Stevens said that one of the Schwartz Rounds focused on interpreters in the hospital system, which are members of the palliative care team whose trauma is often overlooked. Stevens explained that Schwartz Rounds gave staff the “opportunity to kind of talk about their stories and how it completely overtook their own identity, and they did not know who they were anymore.” Stevens shared that often the interpreters could not separate what they said from what the patient discussed, and almost felt like they were actually living the patients’ experiences themselves, which left them crying their entire way home because
they had no idea what to do with that emotional burden, nor how to go home and care for their children and deal with their families. “It was so moving to me in terms of what they gave and how passionately they feel about their profession and what they are contributing to the team,” explained Stevens.
Stevens spoke about trauma experienced by another group of health care professionals, respiratory therapists, who despite their key role, did not receive much praise during the pandemic, Stevens observed. During one Schwartz Rounds for this group, Stevens heard a seasoned respiratory therapist recount how traumatized he and his colleagues were because all they were doing were vent withdrawals, which ordinarily would be rare. He broke down and said he did not know who he was anymore and did not recognize himself. He described a trip to the grocery store when he heard someone say something about not getting the vaccine and he lost control, started yelling at this person, and then broke down crying.
Lown suggested that the situation that Stevens recounted describes trauma, noting that the definition of trauma is an event or series of events that disrupts the integration of self and one’s sense of identity, whether physical, psychological, emotional, or spiritual. Lown said it is unclear what depths of traumatization and post-traumatic stress disorder health care workers have experienced and whether their lingering traumatic stress may reach clinical significance.
Lown remarked that although health care workers have been “surveyed to death,” it is the power of stories to uncover things that surveys could not reveal. She asked Stevens to talk about needs that health care workers have identified to keep themselves afloat. Responding that most workers have said they need to be seen and heard, Stevens explained that one approach Lehigh Valley Health Network took was to hold weekly COVID-19 updates at which an infectious disease clinician would talk about the latest science. This provided staff with a grounding that they could all share, tied staff together clinically, and offered a way to cut through all the circulating misinformation. She added that other elements the health network implemented during COVID-19 did not work as well, but the weekly clinical and medical overview was helpful for everyone, perhaps because it connected the staff.
Stevens described a pivotal moment on the palliative care team during the angry phase of the pandemic—what Stevens referred to as the “senseless death” phase—featured racial divides and vented hostility on the team, which was new. “It was a sign of all the stress and all that was happening during that particular wave,” of the pandemic, explained Stevens. Her response was to lean into that and use safe or compassion spaces to help
everyone understand what things felt like from others’ perspectives, to feel included, and to not be afraid of making a mistake or being judged for being different. “We made that a point with everyone individually to really think about how that looks for them and we started to build a credo,” explained Stevens. “We started to build mission statements to really think about who we were as a team. We knew the world outside of us was going crazy, but how could we really connect and feel like we were strong enough as a team to address some of these other interfaces better.”
While focusing on developing those mission statements, her team developed the habit of having retreats to give staff a break and help staff connect and feel stronger as a team. Stevens said these efforts to form connections, prioritize mental health, and listen to and see the different stresses each individual was facing were very helpful. Lown emphasized that the information about what staff needs must come from the workers themselves. Otherwise, leadership develops programs without great staff uptake and become frustrated. “That is the argument for inclusion in determining what is going to be offered,” emphasized Lown.
Reifsnyder shared that her organization started talking about normalizing and structuring for compassion; its national quality strategy was already centered on compassion and zero harm, and it had started Schwartz Rounds in some sites and had a compassionate caregiver of the year award. She noted that many things that staff said they needed were easy to provide. “In a crisis, as we learned, there are things that seem like they would be impossible to do in a large organization, or even a small one, and we did them,” said Reifsnyder. For example, staff said they needed information and did not want to receive it through memos or cascading messages that went through layers of hierarchy but rather from the chief medical officer and chief nursing officer. In response, the organization held twice-weekly Zoom calls for every leader in the company and answered every question. The leaders relayed that information directly to their staff, and staff felt reassured that they could ask questions and talk about their experiences. Today, said Reifsnyder, the organization is starting to address other issues, such as recovery.
Lown observed that there is something anchoring and stabilizing about seeing leaders being transparent about what they do and do not know. She described being influenced by a paper that identified five essential elements that people need in the immediate and mid-term stages of a disaster—whether it is from terrorism, gun violence, or nature (Hobfoll et al., 2007)—and that these key pillars are built into Stress First Aid:
- Safety: a place to feel safe,
- Ability to calm,
- Sense of self and community efficacy,
- Connectedness, and
- Hope.
Lown asked the panelists to speak about systemic organizational initiatives that in their experience have been effective. Reifsnyder said there will need to be disruption and reconfiguring of many aspects of health care policy to enact strategies and approaches already known to work in terms of being present and authentic with people. One thing she believes is most important is to make compassion an organizational imperative and then structure the organization to make that a reality, recognizing that it can be difficult to do so across large organizations.
Reifsnyder identified preconceived notions about compassion, as a key obstacle to progress, particularly since health care staff already think of themselves as being compassionate. The challenge, Reifsnyder emphasized, is for staff to be compassionate with one another, not only with patients and families. Reifsnyder shared that she talks with teams about compassion as theoretically an infinite resource, unlike anything else in health care. “It does not cost you anything, and you cannot use it all up, at least theoretically,” said Reifsnyder. She added, however, that “practically speaking, that is not true because people who feel used up themselves cannot bring their full selves, their authentic selves. They cannot practice with compassion if they feel used up.” Schwartz Rounds, she added, provide a great way to establish a planned, organized structure for expanding on and operationalizing the concept of compassion.
Reifsnyder pointed out that a key step is to engage leaders in training around compassion and psychological safety. One fundamental of leadership, said Reifsnyder, is having the managerial courage to get out and round with staff members to give feedback regularly, both positive and corrective. In her experience, change can be slow at first, but as an organization works in that direction, people start to get it. “It was not long before lots of people were talking about compassion in some of the structures that we had put in place,” she said.
Stevens pointed out that it is also important to operationalize strong connections. “I really believe the team connection is the only thing that keeps people going,” she said. “We really have to think about—very pointedly and formally—who is on your team and making sure that there
are strong ways to be together as humans.” For Stevens, this means seeing and hearing people as individuals on the team and getting into the weeds in terms of understanding what they need specifically regarding leadership. She noted that given the cost of staff turnover, the investment of time in these basic leadership elements are invaluable as far as how a team will function.
For inpatient staff, Stevens noted that her organization holds what she called “nutritional rounds,” where team members get together for lunch every day regardless of how busy they are so they can check on each other. Although this type of activity is more challenging to manage with outpatient staff, Stevens noted that her organization works to make sure they are connecting with each other as well. Reifsnyder emphasized that if only one priority is possible, it would be to institutionalize well-being across an organization.
Lown asked the panelists to talk about things that give them hope. Stevens shared that people like Francis give her hope, especially their dedication to holding people’s hands regardless of how difficult it has been. That people have shifted to new roles, knowing they want to stay committed to health care, also gives her hope because it suggests they are resilient enough to figure out how to get beyond their trauma. Finally, that the Surgeon General is talking about this issue gives her hope that the health care community is finally discussing the things that make a difference, such as the focus on mental health and well-being in patients, families, caregivers, and professional staff.
Reifsnyder explained that she teaches in a graduate nursing program, which enrolls nurses who have been working 2–5 years, mostly in bedside positions in hospitals. These students are coming back to school to pursue a graduate degree in leadership. She pointed out that the older generations of nurses say that today’s younger nurses are not as committed as they were, but the reality—and what gives her hope—is that these young nurses are questioning the idea that they must take everything on if they want to get ahead, that a balance between work and the rest of life is impossible. She tells her students that self-care is not self-indulgence. It is as necessary as breathing, and she tries to model this for the students.
Posing the final question to the panelists, Lown asked about what is needed to advocate for shifting values and make the necessary investments to support the workforce. Reifsnyder identified institutional commitment to compassion and well-being; increased federal investment in the direct care workforce; and the importance of meaningful shared governance,
which involves asking staff to not only ask their leaders for solutions but also identify problems. “People can learn how to do this, and it might be in their discomfort zone for a while, and that is where the magic happens, when we go into our discomfort zones,” she said. “That just makes a world of difference when you actually engage people in the decisions that are going to impact them.”
Stevens, citing Stacie Sinclair of the Center to Advance Palliative Care, said that recovery may not be possible while still in the system, which suggests that one step would be to offer 3-month sabbaticals. Doing so, said Stevens, would be less costly than filling vacated positions, as would easing workloads by setting limits and rethinking all the nonclinical and administrative tasks that staff must complete.
Lown noted that an easy step for organizations is to eliminate the requirement for an individual to disclose whether they have ever received treatment or therapy for any mental health disorder when applying for credentialing or licensing. This requirement, said Lown, violates the American Disabilities Act, and a toolkit is available with tips on how to remove it.16
During the Q & A session, Ernest Grant shared that he often receives letters or e-mails from nurses who say they would seek mental health counseling except they are afraid it will appear on their insurance or license renewal, even though it could have been for something unrelated to work, such as a marital problem. “We need to figure out some way to change the thought on this to where it is acceptable—actually applaudable to recognize that … [an individual] needs help,” said Grant.
Reifsnyder said the stigma associated with taking care of mental health is often subtle. For example, she hears people telling young health care workers they cannot be experiencing burnout because they have not been in the field long enough. The problem is that each individual experiences burnout or suffering differently. “Bringing compassion,” she said, “means I do not impose how I think about suffering on someone else. I let them tell me about their suffering.”
Stevens, who spent the first half of her career in inpatient psychiatry, said the more the conversation about workplace environments includes a recognition that mental health is important, the better, and she believes health care is moving in that direction. Lown noted that the National Academy of Medicine’s plan for improving the well-being of the health care
___________________
workforce includes an anti-stigma campaign.17 In addition, the Centers for Disease Control and Prevention is working with the National Institute for Occupational Safety and Health on developing public messaging as part of an anti-stigma campaign.18
DIRECT CARE WORKERS: INDISPENSABLE, UNDERVALUED, AND IN SHORT SUPPLY
The fifth session, moderated by Howard Gleckman, senior fellow at the Urban Institute, explored the role of direct care workers,19 a critical yet underappreciated component of the workforce, the unique challenges they face, and the disproportionate effects of the pandemic that they experienced. Jeffrey Wellman, director of Care Force Development at the National Association of Health Care Assistants, began by explaining that direct workers have a variety of titles, depending on where they sit in the continuum of care, but their scope of practice and the tasks they deal with daily are reasonably consistent. Women account for approximately 86 percent of this workforce, and many direct care workers are single heads of households.20
Kezia Scales, vice president of research and evaluation at PHI, pointed out that there are approximately 4.7 million direct care workers in the United States, and that number has been increasing and will continue to grow rapidly (PHI, 2022). Despite some diversity in what direct care workers do across settings, there is a consistent focus on assisting with activities of daily living (ADLs) and/or instrumental activities of daily living (IADLs). ADLS include getting up in the morning, getting dressed, bathing, toilet care, eating, and repositioning. IADLs can vary enormously for those in private homes and can include housekeeping, meal preparation, scheduling and attending appointments, community engagement, and/or supported employment.
___________________
17 See https://nam.edu/initiatives/clinician-resilience-and-well-being/national-plan-for-health-workforce-well-being/ (accessed September 11, 2023).
18 See https://blogs.cdc.gov/niosh-science-blog/2022/05/24/mental-health-initiative/ (accessed September 11, 2023).
19 According to the Bureau of Labor Statistics classifications, direct care workers include personal care aides, home health aides and nursing assistants. For more information, see https://www.phinational.org/policy-research/key-facts-faq/ (accessed September 11, 2023).
20 See https://www.phinational.org/wp-content/uploads/2020/01/Its-Time-to-Care-2020-PHI.pdf (accessed September 11, 2023).
“When we start to really look at what it is that direct care workers do, we see the incredible complexity of the role,” remarked Scales. What are often called “basic” tasks require a complexity of skills and competencies, including a range of interpersonal and problem-solving skills, she said. Direct care workers also need medically or clinically adjacent knowledge regarding what to look for, what a change of status, might signify, and how to communicate effectively with the individual, family members, and other members of the interdisciplinary team. “There is a real intersectional skill set required for direct care,” emphasized Scales.
Madeline Sterling, assistant professor of medicine at Weill Cornell Medicine, explained that when she started conducting research on home care workers, patient after patient referred her to their home care worker for details on their condition and what was going on in their home. This person has real insight into what is happening, including changes in the patient’s symptoms and when it may be time to reach out to a doctor or go to the hospital, Sterling explained.
Scales added that the triad of the patient, family members, and paid direct care workers forms the core of team-based home care. Maintaining and managing the relationship between direct care workers and family members can be challenging, but that relationship is critically important because family members have information about the patient that the workers need to have to provide the best care. Likewise, direct care workers have knowledge that family members can build on and benefit from. “There is a lot of potential synergy and collaboration there, but there is also potential for conflict, for miscommunication, […] for mismatched expectations about the role of the paid direct care worker in that context and who knows the individual best and who spends the most time with them,” explained Scales. “There is a lot of emotion and identity bound up in that as well,” Scales observed. One of the competencies required of direct care workers is the ability to navigate those relationships and deal positively with the inevitable conflicts that arise. She noted that the need for these skills underscores the importance of training, preparation, and support for direct care workers to enable them to do their job well.
To illustrate that point, Gleckman recounted how when his father was ill, he needed more help than his mother could provide, so they hired an aide. “My mother’s attitude was, ‘Who is this woman? What is she doing living in our house?’ The aide did a marvelous job navigating that, but I think it is a very common situation and kind of an unremarked-upon part of the work that home care aides do,” he said.
Wellman explained that direct care workers working in a facility face a different set of challenges. For example, those in a home care setting will deal with one person at a time, but those in a facility may be responsible for 12–20 people, half of whom might need assistance with bathing on a given day, and others might require supportive ambulation. He said a good nursing assistant can handle caring for eight relatively independent individuals, but that workload would be too much if they had eight patients requiring moderate to maximum assistance.
The stressors in a home care environment differ from those in a facility, added Wellman; direct care workers have to understand the care plan more fully because they do not have the direct line of supervision that they would have in a long-term care facility, for example. Direct care workers in the home care environment have more autonomy and less control and oversight, which Gleckman said could be both good and bad. In addition, Wellman added, they can access resources in their client’s natural setting, something that those in a facility may be unable to do.
When asked about the shortage of direct care workers and how it developed, Scales said that this is a long-standing issue that was amplified by the pandemic. She explained that with the U.S. population aging and living longer with complex conditions and serious illness, the demand for direct care workers is growing, yet the nation’s population dynamics are such that fewer people are available to fill those positions. In addition, the challenges of the job make it difficult to attract people to the field and support them appropriately so they may thrive. What is particularly acute today, said Scales, is the competition from other employers, such as Amazon, Target, and Walmart, that have more flexibility to increase wages, offer retention bonuses, and provide more secure or stable schedules.
Underscoring the impact of workforce shortages, Sterling pointed out that family caregivers are struggling and overwhelmed. She emphasized that patients are more complex to manage than they were 5 years ago, but they still want to stay at home and age in place. Add in the challenges that arose during the pandemic and a worker shortage, and it is no surprise that long-term care is in crisis. “This needs serious attention … from a policy perspective,” said Sterling, “[t]his requires broad-scale financing, wage increases, and just helping family caregivers navigate.” Physicians, she added, have not received training about home care or these workers. Sterling’s research has shown a lack of awareness among physicians about the basics of home care, including who is going to provide it and for what duration. In addition, home care is not integrated into primary care and the broader health care system.
Wellman posited that if organizations “did the math,” they would see that the money they spend because of staff turnover could be put toward raises for employees, which could reduce turnover. He explained that the majority of short-term turnover occurs within the first 30–60 days. “If you can get them past that 60-day mark, they are going to be well on their way to becoming part of your tenured team,” said Wellman. One contributor to the high initial turnover rate is that the post-acute and skilled nursing environment is physically and emotionally demanding from the beginning. Another factor is that the onboarding process for new employees is rushed, and the orientation and training process is not systematic, which leads to important information being left out. To address this latter issue, his organization created a certified preceptor course that teaches nursing assistants to be teachers, mentors, and coaches for new team members. Wellman added that the organization is also communicating to its members the importance of viewing each new employee as a vital asset, not a burden or challenge.
In terms of turnover among long-term employees, Wellman explained that workers are leaving for a variety of reasons, including to take a better position elsewhere, to go to school, or because they have endured so much physical distress that they can no longer do the job. Gleckman added that being a nursing home or home care aide is one of the most dangerous occupations in the nation, due primarily to the physical demands related to lifting patients but also mental health issues, such as depression (U.S. Bureau of Labor Statistics, 2022).
Gleckman noted that the Biden administration is expected to propose minimum staffing levels for nursing homes. “We cannot continue to expect our CNAs to be caring for 22 people on a shift and expect that the people who are living in those nursing homes are receiving adequate care and that the CNAs are able to do their jobs and survive,” said Scales. “We need to have enough staff in nursing homes to ensure that residents and staff are not in immediate jeopardy. That has to be the bottom line in the industry.” The worry about such mandates is that they will pull more people out of home care to staff nursing homes, plugging one leak but creating another, said Gleckman.
Scales emphasized that such mandates cannot be viewed solely as a provider-level problem. “We need the staffing mandates, and we also need as much information, best practices, technical assistance, and everything else to support providers in doing what they need to do to be able to recruit and retain enough nursing assistants to meet the mandates,” said Scales. In her opinion, a national recruitment campaign is needed to recruit staff, along
with a conversation about how nursing homes and other long-term care services are financed and whether the available money is being invested in creating quality jobs to provide quality care.
From a research perspective, Sterling is generating evidence to show the value of the direct care workforce for financial and health outcomes. Such evidence is sorely lacking, she explained, noting the importance of measuring the contributions of home care workers to patient care and the impact on patient outcomes. This evidence will help to secure funding to support the workforce and their essential care, she explained (Sterling et al., 2018, 2020a, 2020b).
Gleckman asked the panelists for their ideas on how to focus more on measuring outcomes and less on process (i.e., having a certain number of staff providing a certain amount of care). Wellman said it should be possible to look at the needs of a group of people and develop a formula that calculates how much nursing support is needed given the number of people with a certain level of acuity. He believes that long-term care organizations and provider groups will be anxious about measuring outcomes because there is no clear answer to how many CNAs are needed to provide care for a group of individuals with a certain level of acuity.
One problem with recruitment, said Wellman, is the way long-term care organizations recruit new staff members. Often, recruiters turn to employment websites, such as Indeed.com, but that is an impersonal and passive method. His team has an ongoing recruitment project in Arizona using a multipronged approach over different media sources. “It is a little bit difficult to recruit,” said Wellman, “but I do not think it is nearly as difficult as we think it is. I just think we have not come up with the right formula yet to get people’s attention.”
Gleckman asked about helping direct care workers work to the top of their license. Sterling pointed out that home care aides have a scope of care that can change depending on their role and how they are paid. In her view, aides could do more and should be recognized as important members of the health care team. In terms of models of advanced roles, Sterling’s team is conducting one of the first clinical trials with a large home care agency on how training on heart failure scope of care affects workers’ job satisfaction and self-efficacy with caregiving (Sterling, 2023). The study is also examining the impact of turnover among home care aides on patients with heart failure. In Sterling’s view, “for some of these complex conditions where we know this workforce is heavily engaged and has potential to do more and want to, I think it is a win-win for aides and for patients.” She added that
her experience engaging with the home care workforce has revealed that aides are enjoying learning new skills, are applying those skills to patient care, and find being recognized as a member of the health care team to be “incredibly powerful.”
Scales commented that many direct care workers are interested in accruing more skills and having those skills recognized. She explained that PHI is committed to identifying the best approaches to engage adult learners. One key approach is to draw on life experiences in training rather than simply ticking a box to fulfill requirements. Scales noted opportunities to upskill the entire workforce. Other potential approaches include creating career advancement opportunities for direct care workers within the scope of their role, without having to change rules and laws.
Scales described trials of several advanced roles for direct care workers that PHI is conducting, such as transition specialist aide, a nursing home–based CNA position involved in the transition of care process starting with discharge from the hospital to the nursing home and then from the nursing home to home. She pointed out that having a transition specialist aide who knows the patient and their needs involved at every transition can lead to more successful moves to the home and reduce hospital readmissions. The main challenge, she explained, is to demonstrate evidence of impact for the workforce, patients, and payers to make the case for more upstream investments that pay off for the system in terms of improved quality outcomes and reduced costs. Gleckman noted the dearth of research that connects high-quality long-term care with cost savings for the health care system.
Gleckman pointed out that the average hourly wage for a nursing home-based CNA is about $17.40,21 according to the Bureau of Labor Statistics. For home care workers, it is $14.50,22 which is less than the minimum wage in many states and less than the $19.60 that veterinary technicians make.23 “What does it say about our culture when we pay people more to take care of our cats than we pay them to take care of our mothers?” asked Gleckman.
Inadequate pay for home care workers, in Sterling’s view, is indication that “society has a big problem.” She emphasized that “[t]his is not low-skilled work. This is really important work and I think we need to value that.” She noted that her team’s research, before the pandemic, revealed
___________________
21 See https://www.bls.gov/oes/current/oes311131.htm (accessed September 11, 2023).
22 See https://www.bls.gov/oes/current/oes311120.htm (accessed September 11, 2023).
23 See https://www.bls.gov/oes/current/oes292056.htm (accessed September 11, 2023).
that home care aides make less than aides in other care settings (Guerrero et al., 2020).
For Scales, the financing issue is indicative of broader systemic problems: “We do not have a system that has identified our population needs for long-term care and how are we going to pay for them. We have a system where we have ended up with Medicaid as the de facto payer.” She said that despite a huge cultural issue that needs addressing regarding the value of the people who receive these services and those who provide it, a serious structural flaw remains in how care is paid for. “Can we continue to tinker around the edges with the system that we have right now, or do we need” to transform our approach to “covering these services that builds in a livable and competitive wage for those who do the work?” asked Scales. Regardless of the answer, Scales emphasized that the nation needs to devote much more resources to meet the long-term care needs of people with serious illness.
Audience Q & A
Maguire wondered about creative solutions that would augment the paid direct workforce with technology or volunteers, such as AmeriCorps or Community Care Corps volunteers, high school students, or newly retired people looking for a sense of purpose. Scales agreed that a range of approaches must be taken to address the shortage on all fronts. She suggested another opportunity beyond broadening recruitment efforts is to pay more family caregivers as a way to expand the workforce by integrating them. Scales pointed out that technology can help in ways that do not involve robots providing care, such as improving scheduling and communication. Sterling agreed, noting that the pandemic showed how powerful virtual visits and telemedicine can be. Her team is collaborating on a project on how to create equitable solutions to provide this workforce with technology. She added that a national scoping review that the collaborators conducted found that many applications are used for tracking, documenting, and scheduling but not supporting the workforce and direct care (Kuo et al., 2022).
Sterling remarked that she would like to see technology that could assume tasks such as taking blood pressure and adding it to the electronic health record or monitoring the care plan. The key will be making technology that benefits the workforce, enhances their ability to do their jobs, and serves as a retention tool. Her team is designing technologies that would
provide home health aides with remote assistance for tasks such as wound care and checking for edema.
Marian Grant, a health policy consultant, asked about the share of the direct care workforce that is unlicensed and to what extent immigration policy affects the workforce. Scales clarified that the direct care workforce is not licensed, for the most part. She explained that nursing assistants in nursing homes and home health aides paid through Medicare must be certified according to federal requirements. The majority of workers in home care, however, are not certified and receive different levels of training, depending on the state and program. In addition, there is a “gray market” for direct care workers in which households pay for their services using private funds. Scales noted that the challenge is that direct care is a diverse and fragmented landscape, which “makes it difficult to understand who we are talking about, where they work, what their job conditions are, [and] what the challenges and opportunities are, but then also to enact system-level solutions.” As a result, there is little opportunity to have a high-level directive that can affect this workforce overall. “We know the challenges well, but the solutions tend to be very incremental because, for example, they only impact a particular segment of the workforce in a particular state in one Medicaid program,” said Scales.
Scales noted that approximately 26 percent of the direct care workforce and closer to one-third of the home care workforce was born outside of the United States. This makes immigration policy an essential part of this conversation, she stressed. Gleckman added that a special visa for nurses was once available, although that program seems to have expired. “It would be interesting to see if we could recreate that and maybe expand it to include aides,” he said.
ADVANCING DIVERSITY, EQUITY, AND INCLUSION IN SERIOUS ILLNESS CARE
Arika Patneaude, director of bioethics and palliative care at Seattle Children’s Hospital, opened the final session of the first day of the workshop. She pointed out that as a Black, Jewish, Indigenous woman, she comes from a long line of storytellers, so she would start the session with a story. In the spring of 2020, she recounted, a confluence of events affected society and the entire workforce who continued to show up to work. Patneaude noted that many individuals in the serious illness workforce “come from historically and currently marginalized communities and include people of
color, individuals who identify as two spirit LGBTQI+, socioeconomically disadvantaged individuals, and people without the option to work from home or even take a sick day because they would not get paid.”
Patneaude noted the huge human toll of COVID-19 around the world, which led to broad concern about how to support all the health care workers who cared for patients who died. Patneaude noted that these workers are experiencing long-term psychological effects that may worsen. At the same time that the pandemic was having such a deadly impact, George Floyd, a Black man, was killed by the police, which was captured in the widely broadcast video of the last 8:46 minutes of Floyd’s life. Floyd’s murder while in police custody ignited another iteration of “racial reckoning,” in which the whole world served as witnesses to the brutality that Black people have endured for more than 400 years, observed Patneaude. Up until that point, she explained, layers and layers of brutality had been denied, downplayed, or disbelieved, but for those 8:46 minutes, there was no denying the impact of the “racial epidemic.” Patneaude commented that while Floyd’s murder may have been a shock for many, that was not the case for many Black people, for whom these types of experiences have been shared through an oral tradition that spans many decades. “Finally, there was no denying it by non-Black people,” said Patneaude, who noted how non-Black people began reaching out, telling their Black colleagues, neighbors, and community members that they see them, hear them, and believe them. Black Lives Matter yard signs started appearing on lawns, and protests took hold in cities nationwide; some of these included or were organized by health care workers in their scrubs and/or white coats.
Patneaude described how health care workers were viewed as heroes for working on the front lines to care for patients during the pandemic and for their role in the protests as part of the racial reckoning. She noted that low rates of virus transmission during protests where many participants wore masks confirmed that masks were effective (Neyman and Dalsey, 2021). She pointed out that major corporations and many health care organizations made broad statements supporting the Black Lives Matter movement, committed to fight racial injustice, incorporated DEI and justice into their staffing policies and organizational culture, and promised to create more inclusive cultures, become antiracist, and hire more workforce members from historically and currently marginalized communities.
Referencing work by the McKinsey Institute for Black Economic Mobility, Patneaude pointed out that Fortune 1000 companies and institutions pledged billions of dollars to support fighting racial injustice but have
little to show in actual action (Armstrong et al., 2023). Noting that the money pledged has been difficult to trace, Patneaude asked: “Have we all been [subject to] performative allyship or woke-washing, when companies appropriate the language of social activism into marketing materials?” In contrast, she noted organizations making a real effort and positive impact. For example, Seattle Children’s Hospital took many steps toward being transparent to the community and public about its complicity and even engagement in racism and the concerted efforts it was taking to correct the harm. As part of this transparency, the organization publishes quarterly updates on a public-facing antiracism website.24
Patneaude emphasized that through the pandemic and this version of racial reckoning, workforce members in serious illness care, including those from communities most affected by COVID-19, continued to show up for work every day, and many died from the virus. The World Health Organization estimates that 80,000–180,000 health care workers died from COVID-19 from January 2020 to May 2021 (WHO, 2021). Then came some hope, explained Patneaude, when on December 14, 2020, the first U.S. COVID-19 vaccine was administered to Sandra Lindsay, a Black ICU nurse at Long Island Jewish Medical Center. “The irony of this—a health care worker, a Black woman, receiving the first vaccine in the U.S. just gives me chills for many, many reasons,” said Patneaude, who explained that she and everyone else brings their lived experiences to work, including multiple-generations-long impacts of racism, xenophobia, sexism, homophobia, and transphobia within society and in the workplace.
Patneaude noted that in the year following the day George Floyd was murdered, police in the United States killed 229 Black people (Mapping Police Violence, 2023). According to NBC News, hate crimes against those of Asian descent in the United States in 2021 had increased 339 percent nationwide over the prior year (News, 2022). She also noted that an April 2020 survey found that up to 47 percent of U.S. health care workers planned to leave their positions by 2025 (Goodchild et al., 2022).
Patneaude cited many reasons to focus on increasing and sustaining the diversity of the health care workforce, starting with it being the right thing to do, and a diverse workforce is better equipped to care for a population becoming more diverse with each passing year. Moreover, data show that patients and their loved ones have better experiences and outcomes, including reduced pain, with racial concordance between provider and
___________________
24 Available at https://www.seattlechildrens.org/about/commitment-anti-racism/.
patient (Anderson et al., 2020). One study revealed, for example, that a 10 percent increase in Black representation in the workforce was associated with a 30.61-day increase in life expectancy for Black individuals, a reduction in Black all-cause mortality of 12.71 deaths per 100,000 people, and a 1.2 percent lower disparity between Black and White all-cause mortality rates. The association with life expectancy was strongest in counties with high rates of poverty, observed Patneaude (Snyder et al., 2023).
Patneaude outlined several key principles that could serve as a foundation upon which to build an antiracist organization committed to maintaining a diverse workforce for the good of everyone—workforce members, patients and their families, caregivers, and communities:
- Being intentional about engaging in antiracism work;
- Maintaining transparency by showing the good, the bad, and the ugly, including objective measurement as part of a dedicated system;
- Investing in the process with financial and personnel resources;
- Infusing sustainability, as this work is not one and done but continuous and ongoing; and
- Being authentic and not performative.
Recalling a panelist in an earlier workshop session, Patneaude observed: “As LaToya said this morning—and this is such a metaphor for how our workforce is valued—the ice cream truck should not be a luxury for those who care for others,” said Patneaude. She then asked the session panelists—all leaders of national organizations focusing on serious illness—to discuss what their associations and organizations were doing to advance DEI in the workforce.
Wendy-Jo Toyama, chief executive officer of the American Academy for Hospice and Palliative Medicine (AAHPM), said that the organization’s robust history of working in the DEI space was a key reason she joined AAHPM. The organization has held listening sessions with members, engaged consultants, allocated resources, and developed a strategic plan to address DEI issues. In particular, AAHPM has focused on creating a sense of belonging and inclusion, which a 2019 McKinsey & Company survey showed is a differentiator in an organization’s success in advancing diversity (Dixon-Fyle et al., 2020). After listening to members, the organization created affinity work groups, celebrating and focusing on culture and ethnicity at its national meetings, for example. Toyama said that when she joined AAHPM a month before George Floyd’s murder, her goal was to look at its work and determine how
to take that to the next level. She noted that AAHPM has defined diversity and inclusion as an organizational value, which enabled it to issue a statement swiftly after George Floyd’s murder. “I did not have to ask the board’s permission [and] get it reviewed,” said Toyama.
Toyama explained that the 2019 McKinsey survey placed organizations involved in DEI initiatives into five categories: diversity leaders, fast movers, resting on laurels, moderate movers, and laggards. When Toyama joined AAHPM, she felt that it was resting on its laurels. To move into the leadership category, AAHPM held more listening sessions, conducted a survey, and increased resources and time for DEI. She noted that AAHPM is also developing a new DEI strategic plan that aims to emphasize health equity and social justice. However, she added that AAHPM still needs to work on increasing representation at the leadership level, something all medical associations are facing, noted Toyama. She explained that AAHPM’s board has been looking at how the organization nominates people to the board and develops leaders. “I think there is more difficult work that needs to be done there,” observed Toyama.
Anne Kelemen, board chair for the Social Work Hospice and Palliative Care Network (SWHPN), said a first step in focusing on antiracism work is acknowledging privilege. “As a White woman, I recognize that I am in a very privileged body and I am treated differently when I walk into spaces,” said Kelemen. She noted that SWHPN has engaged in antiracism work in all its practices over the last 18 months, including hiring two antiracism consultants to help the board identify overlooked areas and unrecognized biases. “As social workers, I think we really even have not done our own work within our social work discipline to recognize the White supremacy that exists within our social work field,” she observed.
Kelemen pointed out that SWHPN’s efforts to advance antiracism starts with the important task of each individual engaging in their own reflective work. She added that hiring the consultants helped the organization work through several issues. “I am really excited [about] the place that we are at now, but [we] also recognize that this is not a checklist,” she said. “We are not done with our work.”
Michelle Webb, president of the Hospice and Palliative Nurses Association (HPNA), said the thing she is most proud of is that HPNA is approaching this work as a marathon, not a sprint. HPNA has focused on building a sustainable infrastructure to continue the work and equip its members to follow suit. A member survey on the status of the work revealed that further guidance was needed to accomplish the work.
Webb explained that at the direction of HPNA’s board, the organization formed a Diversity, Equity, Inclusion, and Belonging (DEIB) task force to lead its journey. The association has incorporated advancing DEIB as a strategic priority and is identifying a DEIB consultant. Webb added that as a member organization, her team saw opportunities to lean into the idea that this work is something people choose to be involved in. “We wanted to make sure we knew what they wanted and needed, and we are providing that support,” said Webb. The task force is now a standing committee and has developed an HPNA DEIB style guide. For Webb, antiracism and DEIB work is centered on integration, alignment, and prioritization. “We have looked at, over the long term, how to integrate this work in a way that it becomes just the way we do things,” she explained.
Webb cited research identifying five stages of DEI maturity: being aware, compliant, tactical, integrated, and sustainable (Washington, 2022). Often, she said, people start out being performative and driven by compliance with various legal requirements. They then move to a place where DEI work becomes tactical because it is connected to business initiatives and outcomes, integrated throughout an organization’s internal and external activities, and sustainable through efforts that continuously improve and evolve. HPNA is in the tactical stage and looking at how to put resources in place for its members. HPNA’s efforts include evaluating how it authentically represents DEI in everything it does.
Webb shared that HPNA has committed strongly to creating safe spaces for difficult conversations. “You really have to have those difficult conversations that allow you to heal and grow and learn together,” said Webb. One example is the DEIB standing committee creating a safe space at the beginning of every meeting it holds. This leads to members sharing their stories—a powerful force for change—about their personal or professional DEI experiences. These stories can inform HPNA’s work or reflect what it still needs to do. “It’s really a space to also elevate the voices of those who have not had a voice [and] stories that have yet to be consistently elevated in conversation and to really just get comfortable with being uncomfortable in some of these spaces,” said Webb.
Webb acknowledged that HPNA cannot guarantee a completely safe space but added that it can create brave spaces where people can step up and do the work. Given her common experience of being the only executive leader of color in a particular setting, protecting and creating those brave spaces has been important for HPNA and its efforts. The goal, she said, is to build a strong framework for the organization to support its members
and those showing up in spaces where they may not feel there is diversity, equity, or even inclusion.
Ernest Grant noted that ANA, at 127 years old, is the nation’s oldest professional nursing organization. Over its lifetime, it has had only three African American presidents, the first in the 1970s and the second 20 years later. Grant was elected in 2018 as the first African American male president. Grant shared that up until the late 1950s, nurses of color could not be official members. One of Grant’s first tasks as president was to begin to address the organization’s history of racism, an effort propelled by the murder of George Floyd. ANA formed the National Commission to Address Racism in Nursing25 to address the issue from four perspectives:
- Nursing education: like a newborn baby, nobody is born prejudiced but rather learns that through textbooks, professors, and the way things are done.
- In the clinical space: Black and White individuals receive different levels of care.
- Nursing research: research dollars are not allocated equitably to people of color.
- Policy: policies that prevent people of color from advancing in their careers must be addressed.
The commission comprises 39 organizations; the presidents of ANA, National Black Nurses Association, National Association of Hispanic Nurses, and National Coalition of Ethnic and Minority Nurse Associations serve as coequal chairs. Grant pointed out that ANA’s commitment to addressing racism in nursing is evident in its strategic plan and the resources it has allocated. ANA is working with minority nursing organizations to join its efforts. “I like to call it a journey because, to me, a journey does not end. It is something that we have to go on together,” said Grant. He shared that ANA, after a unanimous vote by its membership assembly, issued an apology for its past racist behavior (ANA, 2022), followed up by apologizing directly to the National Black Nurses Association, which was celebrating its 50th anniversary. ANA has gone to other minority nursing organizations to apologize for its past racist behavior, noted Grant.
___________________
25 Additional information is available at https://www.nursingworld.org/practice-policy/workforce/racism-in-nursing/national-commission-to-address-racism-in-nursing/.
Panel Discussion
Patneaude asked Toyama why she thinks that organizations continue to rest on their laurels in terms of antiracism and DEI work. Toyama said she has been encouraged that more efforts have been sustained than she expected, and she suggested that some did the work only for performative reasons. Toyama noted that this work is difficult to measure but hopes that organizations will start feeling comfortable collecting data, measuring progress, and being transparent about results. AAHPM is analyzing data on submissions to its journal and plans to publish the results. Frankly, she said, she is nervous that the results will not look great, but “[t]hat is okay, because that is how you build accountability.” Recognizing the political climate that politicizes the work, Toyama stressed that research has shown that improving health equity for one group helps everyone. She added: “I think there are these false narratives that are being spoken.”
Patneaude said that accountability was not among the key principles the workshop planning committee developed, even though the group discussed its importance. She asked the panelists to discuss mistakes they have made personally or professionally and the lessons they learned. Webb observed that she finds balancing grace with accountability to be a challenge. She reiterated that she has engaged in difficult conversations with individuals throughout her career from the perspective of frequently being the only or one of the few leaders of color in health care organizations and been frustrated by the lack of private progress and the lack of accountability. “There have been times when I have been more gracious than accountable because I know these are individuals who care about me,” said Webb, “yet unless they are held accountable, […] growth does not happen.” Another mistake Webb has made was not realizing she will have to walk slowly with some people to develop them as an ally and must run with others. “I need to be in both of those groups in order to do the work, in order to sustain myself, and to thrive rather than just survive,” said Webb.
Grant said that when ANA issued its apology to the National Black Nurses Association, its response was to accept the apology but watch for ANA’s future actions. His comment to the National Black Nurses Association was that ANA cannot do this work alone. He explained the importance of allyship and getting people to understand that a White person’s voice may be stronger than his own. “As a person of color, if I call it out, it is going to be, ‘oh, you’re disruptive again’ or ‘you are that angry Black man,’” explained Grant. However, when a White colleague says that the situation
is not right and must be corrected, change starts to happen, and the long journey can move forward.
Grant shared that his mistake was not appreciating the scope of resistance to change. Some ANA members have even questioned why it is getting involved in antiracism and DEI work or accused the organization of labeling them as racist. Grant explained that his response to these comments is that ANA is not calling a person a racist; rather, it is raising awareness, doing something to change the system and right a wrong that U.S. society has perpetuated for many years.
Kelemen said one mistake is to not call out a microaggression and have an effective way to apologize to the person who experienced it. She explained that she took a continuing education course on the art of apology and learned that the right way to apologize is to say something like, “I am sorry. I was in that meeting, and I saw that happen, and I wish that I did this, and I am going to do better next time.” That approach gets to accountability rather than triggering shame and what she referred to as “White women tears.” Her hope is for people to get better about having these conversations that can lead a White person to reflect internally and have a sense of urgency to act. Toyama acknowledged that mistakes are inevitable, but “[y]ou cannot let the fear of making mistakes have you not do this work.”
Patneaude asked each panelist to share one commitment their organization will make and stand by to support diverse workforce members in the field. Kelemen said SWHPN is committed to continuing to show up in spaces, having these conversations, and going beyond performative acts by including DEI in all of its work. Webb said HPNA’s commitment is to stay the course for the long haul. Its next step is to diversify its leadership team and membership and embrace the whole humanity of everyone in HPNA and all the people it serves. The organization is also committed to being accountable for its impact and intent and acknowledging that diversity is not enough, that inclusive spaces need to be built where people feel they belong.
Toyama said AAHPM is involved in an 18-month learning cohort called “Equity Matters.” As part of that, AAHPM is launching its NextGen Scholars for Equity in Hospice and Palliative Medicine, which will sponsor eight scholars. The goal is to create mentoring and sponsorship opportunities. “We are very hopeful that will begin, in a small way, to build [a] more diverse workforce,” said Toyama. Grant said ANA will continue to work with state nursing associations to promote diversity and equity at all levels and encourage institutions to identify those policies that prevent people of color from advancing as leaders and work to address them.
Audience Q & A
Marisette Hasan, a registered nurse involved with hospice and palliative care for 35 years, said the workforce sees what needs to be done within organizations to address DEI but feels like it is being muzzled because leaders have not yet prioritized dealing with these issues. She asked the panelists for their ideas on what can be done to help senior leadership lead from the front. Kelemen suggested that organizations hire an antiracism consultant, which SWHPN found valuable to help it make changes. Toyama agreed about the importance of hiring a DEI functional expert or antiracism consultant because they can say things someone in the organization might not feel comfortable saying. She also suggested finding champions who step forward to say this work is important to them and engage in narrative storytelling, which can be a good way to change people’s openness to thinking about why DEI is important.
Hasan also asked the panelists to talk about what their organizations are doing at the state level. Toyama said AAHPM does not have state chapters, so it collaborates with volunteer leadership groups. She noted that her prior organization had a state grant program that funded innovative state-level programs aiming to create a greater sense of diversity and belonging. Webb pointed out that HPNA has committed resources to support its state chapters and their leaders, who ask for advice on how to engage in acts designed to improve DEI.
Patneaude recounted that she wrote a letter to the chief executive officer of her organization in which she explained what it was like to be Black and work at Seattle Children’s Hospital. One thing she said was that she felt she had to leave her “true identity” at the door. Toyama said she shared a similar feeling after the murders of people of Asian descent in Atlanta, which prompted the organization to make space for her and two colleagues to share their stories with others in the organization.
Workshop participant Masami Tabata-Kelly, a Ph.D. student at the Heller School for Social Policy and Management, asked the panelists to identify the evidence needed to advance DEI in serious illness care and discuss what they hope the next generation will be able to accomplish. Toyama, addressing the research question, said it would help to have more studies demonstrating the connection between an administration tackling inequity, improved care for everyone, and reduced levels of moral stress for the workforce. Responding to the second part of the question, Ernest Grant said that it is second nature for millennials and Gen-Xers to have friends who are of
different races and ethnicities, and they are therefore quick to stand up and say something when they see something wrong. Toyama said she wants to see the younger generations hold those from older generations accountable.
Phillip Rodgers, from the University of Michigan, pointed out that those who have built the systems of power should be most responsible for changing them. He noted the importance of allyship and sponsorship and said when he has tried to sponsor colleagues from historically marginalized groups, he has had some successes and some clumsy failures. It has gone well, he said, when he finds the right opportunity for the right person with the right skills and aspirations and helps them get out of their comfort zone. It does not go well when he makes false assumptions about them. He then asked the panelists for practical guidance they would give to those in power on how to effectively sponsor and bring to the table historically excluded voices.
Toyama suggested that leaders should ask questions rather than wait for individuals to come to them with an issue. Kelemen observed that leaders need to acknowledge their place of privilege and work with others to build relationships, bring people into the workplace, and effect change. Grant said to not lump everyone into one category. “Yes, I am a Black male, but that does not mean I have the lived experience of every Black male that is out there,” he said. Rather, it is important to get to know an individual and their personal journey. In closing, Patneaude suggested that one should assume that everyone from a historically marginalized group has had a relevant experience yet also appreciate (as Grant pointed out) that each person’s lived experience will be different.
DEVELOPING PROMISING MODELS/INNOVATIVE APPROACHES TO WORKFORCE RECRUITMENT, TRAINING, AND RETENTION
The second day of the workshop opened with a session that featured practical interventions to adopt in the near term to improve recruitment, training, and retention for the interdisciplinary workforce caring for people with serious illness. The presentations aimed to identify specific areas in which to focus time, resources, and attention to develop a more resilient and sustainable workforce. Joseph Shega, executive vice president and chief medical officer at VITAS Healthcare and session moderator, pointed out that achieving well-being requires having the skill set to not only do the job well but also make a meaningful impact.
Programs to Support Direct Care Workers
Robert Espinoza, executive vice president of policy at PHI, explained that his organization focuses its efforts in three areas: strengthening the workforce through research and advocacy; designing interventions related to training, advancement, recruitment, and retention strategies; and advocacy and public education at the state and federal levels. Espinoza pointed out that PHI draws its knowledge from its experience on the ground developed in partnership with policy makers, industry leaders, employers, and workers and keeping its eye on what the field is studying regarding models and innovations for the direct care workforce and serious illness.
Espinoza noted that as discussed in an earlier session, direct care workers are increasingly supporting the diverse and complex clientele needing long-term services and supports and in different long-term care settings. They support older adults and people with disabilities in a broad range of long-term care settings, including private homes, residential care settings, such as assisted living, and nursing homes. He said the direct care workforce, with approximately 4.7 million members, is larger than that of any other occupation in the United States (PHI, 2022).
Espinoza reiterated Francis’s message from the first session that many direct care workers struggle with economic insecurity because of inadequate compensation, training, and advancement opportunities and other challenges. In addition, employers struggle to recruit and retain workers, and older adults and people with disabilities struggle to receive high-quality care, particularly if they are living with serious illness. PHI estimates that between 2020 and 2030, nearly 8 million job openings in direct care—1.2 million of which will be new positions—will need to be filled (PHI, 2022). Espinoza said retirements will account for some percentage of that, but many workers are leaving direct care for occupations in the fast food and retail sectors, as noted in an earlier workshop session.
When thinking about workforce interventions that support people with serious illness, Espinoza said it is important to also consider other benefits that accrue, such as improving the financial security of direct care workers. Effective interventions can also bring some stability to the sector. He pointed out that innovation is important in any sector, especially in long-term and direct care, and so is evaluation and a robust evidence base. Often, said Espinoza, a workforce intervention will be innovative in multiple ways, but what is missing is a strong evaluation of to whether the intervention is effective, whether it creates inadvertent harms, and how can
that information be shared to inform the entire sector. “An evidence base is so critical to how we think about moving forward,” he observed.
Referring back to the earlier session, Espinoza explained that research has shown that home care workers are increasingly providing both long-term and post-hospitalization support to individuals with heart failure (Sterling et al., 2020b). They have a critical role in monitoring, observing, recording, and reporting relevant changes in a client’s condition, such as high blood pressure, chest pains, or swollen ankles. However, many home care workers report feeling overworked, undervalued, and unprepared due to insufficient training (Sterling et al., 2018). Espinoza noted that home care workers are underrecognized by their health care colleagues, policy makers, and the economy. Moreover, home care workers report that care communication is fragmented and a critical impediment to supporting people with heart disease. In addition, although home care workers report that they love the nonmonetary rewards and essence of the job, they do not necessarily love the quality of the job, how much they are paid, and how they are being supervised (Sterling et al., 2020a).
Home care workers, said Espinoza, are dedicated to their clients and families but often caught in the middle between the desires of the client and their family members. “We have not focused enough as a country on strengthening that relationship between family caregivers and direct care workers through either policy practice or research,” he said. Home care workers spend an incredible amount of time solving problems and resolving conflict, which often requires emotional labor, negotiating skills, and ensuring that solutions are person centered and involve the family.
Espinoza pointed out that home care workers find caring for the patient with heart failure to be frightening and unpredictable in the same way that the patients find living with heart disease to be frightening and unpredictable. Patients are often involved in self-care without a solid understanding of the disease process or training. Espinoza pointed out that often home care workers are not integrated into the care team and so are probably not informing the elements of the patient’s care plan, despite their firsthand experience and what they know about their patients. He added that research speaks to the importance of interventions that provide heart failure–specific training and aim to improve the communication across members of that interdisciplinary care team, all of which could lead to better patient outcomes (Stawnychy et al., 2023). “The more we invest in the field—in understanding, funding, and evaluating these kinds of interventions—the
more prepared we will see this workforce,” said Espinoza. He noted the importance of measuring these interventions’ effect on patient or care outcomes and evaluating the extent to which they support employment outcomes, job satisfaction, retention, and cost savings.
Espinoza then turned to another intervention developed by PHI, which addresses care connection and care integration (Campbell et al., 2021). The intervention involves integrating direct care workers into the interdisciplinary care teams and having them serve as key players in care coordination. Moreover, the intervention also involves having direct care workers take on an advanced role both in direct care, such as dementia specialist, care transition specialist, or peer mentor, and beyond direct care into administrative and management positions or moving up the nursing career ladder.
Espinoza explained that the pilot Care Connections program provided 14 direct care workers with 240 hours of training to serve as Care Connections Senior Aides and trained three registered nurses to oversee them. Over the first 18 months of the pilot program, the trained direct care workers supported over 1,400 patients, resulting in an 8 percent reduction in the rate of emergency department admissions, a notable reduction in family caregiving strain, and a notable improvement in job satisfaction among the direct care workers. Espinoza noted that while the advanced role interventions for direct care workers needs testing on a larger scale, PHI has created a guide for developing care integration senior aides that includes ideas for training direct care workers to take on advanced care roles, training ideas for their colleagues on how to respect and value them in these roles, and specific return-on-investment measures (Dieppa and Espinoza, 2022).
Espinoza also shared a third intervention that focuses on training direct care workers to be dementia specialists, for which there is a significant need. He noted that by 2050, approximately 14 million older Americans will be living with Alzheimer’s disease (Scales, 2019). Researchers developed a dementia care specialist training program that provides information on the global features of dementia symptoms and disease progression, ways to manage challenging behaviors and communication problems, contributors to caregiver stress and how to manage caregiver needs, and how to refer members and caregivers to community resources (Flatt et al., 2018). The researchers noted that some managed care plans use the specialists in a formal way, such as having them serve on the care team and consult on care coordination, and others use them less formally as consultants who provide education or advice to care managers and staff. “This is a great example of
addressing people with serious illness through the direct care workforce while creating an advanced role that is so sorely needed and that elevates their compensation, provides a true career ladder, and keeps them in these roles,” said Espinoza.
Midcareer Hospice and Palliative Medicine Fellowship Consortium
Mollie Biewald, associate professor of geriatrics and palliative medicine at the Icahn School of Medicine at Mount Sinai, described a fellowship program developed at the University of Pennsylvania that focuses on midcareer physicians who want to move into palliative care without abandoning their current position (Dingfield, 2020; Periyakoil et al., 2022). Such a fellowship, said Biewald, creates an opportunity to expand the pool at a time when there is an estimated shortage of 6,000–18,000 board-certified palliative care physicians to join the existing palliative care teams (Lupu, 2010). She added that the Accreditation Council for Graduate Medical Education approved this time-variable, competency-based hospice and palliative care fellowship in 2019. The American Boards of Internal Medicine, Emergency Medicine, and Family Medicine have also approved this program, so any physician other than a pediatrician or anesthesiologist can apply.
Biewald explained that a traditional hospice and palliative medicine physician fellowship is a 12-month, full-time position with specific clinical requirements, such as 4 months in an inpatient palliative care setting, some home hospice visits, and a certain amount of time spent in long-term care settings. It comes with a trainee salary, which is substantially less than most physician positions. As long as the fellow meets the requirements at the end of the fellowship, they graduate and are eligible to sit for the board exam.
The process for the midcareer fellowship (see Figure 3) begins with a meeting with the program director to do a deep dive into an applicant’s skills and create an individualized learning plan focusing on the palliative care areas to which they need exposure, explained Biewald.
Biewald explained that the fellows then join a palliative care team part time for clinical rotations, where they are rigorously supervised and assessed. When each rotation ends, the program uses several assessment tools to determine where the fellow is in the trajectory. They also meet with a preceptor at another one of the partner sites once a month to do a chart-stimulated recall (a structured discussion in which they bring cases from their own practice and talk through the palliative medicine principles that
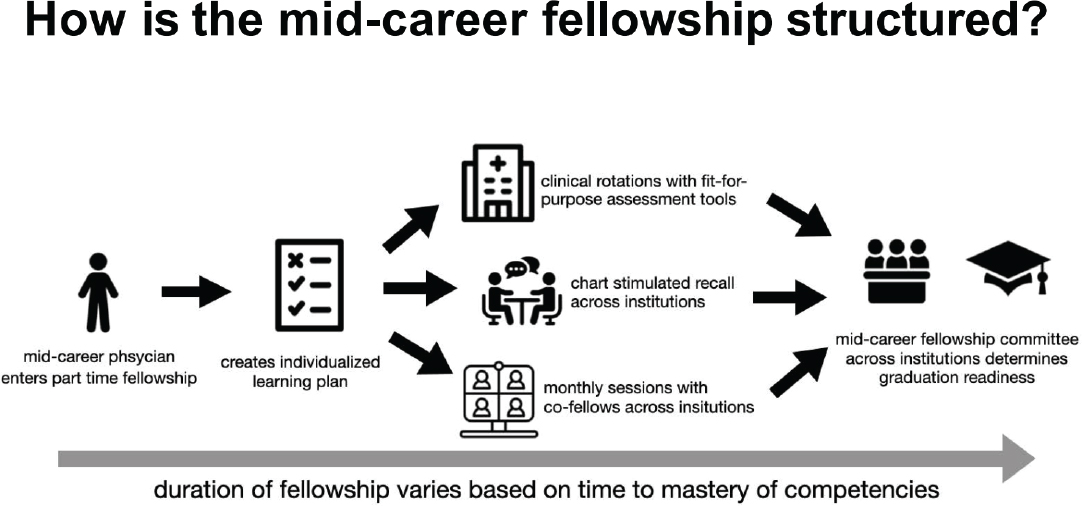
SOURCE: Presented by Mollie Biewald on May 28, 2023.
could apply to them). In addition, they get together once a month with the other fellows and the attending physicians from all the institutions involved to build community and engage in education and leadership sessions.
Once the local program director sees that the fellow is near the point of graduation, the fellow will assemble a portfolio of their completed work and present it to the fellowship committee, which decides on graduation readiness. Biewald explained that as this is a competency-based fellowship, the time to complete it is based on how long it takes for the fellow to show they are ready for independent practice as a palliative care physician. She highlighted that this is a part-time fellowship that allows the fellow to continue in their primary practice. This is important for several reasons, including that the fellows maintain their salary and benefits and can incorporate the skills they are learning into their primary practice.
Biewald said this type of program can benefit the nation’s health care system by helping alleviate the shortage of trained palliative care physicians in areas where recruitment is a challenge. “With this model, you could train physicians in your own health system that have already settled [into] place and then potentially retain them to practice in [the palliative medicine] field after graduation,” said Biewald. She pointed out that as of February 2023, the pilot program has had 17 physicians at seven institutions: the University of Pennsylvania, Mount Sinai in New York, Washington University in St. Louis, Massachusetts General Hospital, George Washington University, Kaiser Permanente Southern California, and the University of Minnesota. Five fellows had completed the fellowship successfully, and another cohort was nearing graduation readiness. The fellows who graduated took 12–24 months to complete the program. She noted each site has implemented the fellowship in its own way. One site, for example, converted its palliative care fellowships to an all-midcareer model, while her institution had one or two midcareer fellows in its total cohort of fellows.
Highlighting some lessons learned, Biewald noted that local context is key to success. “The way that each site has implemented this fellowship has been really different based on the resources that are available at that site, who is available to precept [the] fellows, [and] what their clinical rotations look like,” said Biewald. “It has been really important to have flexibility.” Flexibility in scheduling has also been important, given that the fellows still spend 80 percent of their time in their attending physician jobs.
Another lesson is that a learner-specific curriculum is important for midcareer trainees. One fellow at her institution, for example, has been the physician in charge at a long-term care facility, so the typical requirement
to spend a month in that setting would not benefit that individual, but the other fellow at her institution had never worked in that setting, so doing so was an important part of their fellowship.
Biewald explained that to succeed after the pilot ends in 2025, the program will need supports, such as centralized coordination through the American Board of Medical Specialties or the cosponsoring committee, which is a group of leaders from the boards, to make sure that it is implemented successfully with some standards. They will also need to support the program directors running the fellowship, as Biewald explained, the physicians supervising these fellows take on a significant workload, given the amount of assessment and administrative work involved. She noted a need for additional assessment tools to ensure the program is rigorous and longitudinal research to track the fellows’ careers and determine whether they are more satisfied after completing their fellowship.
Biewald concluded with some takeaways. This project, she said, has succeeded across all seven sites with different learners from internal medicine, emergency medicine, and family medicine backgrounds. Its success implies real potential to expand the palliative medicine physician workforce, with some fellows taking full-time palliative medicine jobs and others integrating their new skills into their primary practices. There is also the potential to grow and help the workforce in other fields facing workforce shortages.
Striving for Goal-Concordant Care: Teaching Serious Illness Communication Skills
Tom Priselac, president and chief executive officer of the Cedars-Sinai Health System and Bradley Rosen, vice president for physician alignment and care transitions at Cedars-Sinai, discussed their institution’s program to improve serious illness communication skills, which are key to goal-concordant care. Priselac explained that nearly 50 percent of the patients his institution serves are on Medicare and another 10–12 percent have Medi-Cal. As a result, it has many patients with serious illness, which makes this program a critical element for fulfilling its mission of being California’s leading treatment center for such patients.
Priselac explained that Cedars-Sinai has 2,300 physicians and runs 88 residency and fellowship training programs that, in 2022, had 491 trainees. It has the largest concentration in California of Medicare patients over age 80, with Medicare/Medi-Cal dual-eligible patients accounting for 43 percent of Medicare inpatient hospital days. In 2022, the system
had over 1 million outpatient and emergency department encounters, with the emergency department accounting for approximately 90,000 of those. Priselac noted that the program Rosen would describe, which is not a one-off initiative, is guided and steered by the institution’s quality council and integrated with Cedar-Sinai’s overall quality and clinical efficiency work: “There is great value in making sure that is how a topic like this is approached from an organizational standpoint.”
Rosen explained that Cedars-Sinai has conducted several projects on goal-concordant care since launching its first effort in this area in fiscal year 2014. The first step was to define what egregious harm looks like at the end of life and identify interventions to prevent it. That project evolved into looking further upstream to identify and intervene earlier in a patient’s clinical trajectory. Rosen pointed out that at the time, the institution also revamped its palliative medicine program and renamed it “supportive care medicine.” Other successful projects since then have focused on integrating goal-concordant care projects into the Heart Institute, ICU, cancer enterprise, emergency department, neurology department, and other areas that the institution’s quality council identified as areas of opportunity for intervention. “Through all of this work, a common theme emerged clearly, which is that clinician comfort and experience with serious illness communication are major barriers to delivering goal-concordant care,” said Rosen, who added that serious illness communication is generally not built into medical education or residency training.
The first step in creating the serious illness communication skills program was to survey all clinicians across Cedars-Sinai to get a better understanding of their own training experience, what they perceived to be the training environment and culture, and whether they saw value in providing these education and resources. A large majority—88 percent of attending physicians and 94 percent of all clinicians—responded affirmatively to the latter.
The curriculum Rosen and his colleagues developed ensured that all the institution’s clinicians had access to communication skills education to achieve goal-concordant care. He noted that research has shown that improving serious illness communication skills reduces clinician burnout rates in that “having more meaningful engagements with patients and feeling like you are practicing the way you want to practice and connecting with patients helps you feel better about your work, and you are less likely to burn out” (Berg, 2017; Boissy et al., 2016; Wert et al., 2023).
Rosen and his colleagues also designed the curriculum to address the fact that many clinicians have different practices. By working with depart-
ment leadership and other clinical leaders, they classified all the physicians at Cedars-Sinai into one of three categories based on proximity to and likelihood of caring for patients with serious illness and designed a program for each category (see Figure 4).
For clinicians who rarely care for patients with serious illness, such as pathologists, dermatologists, and radiologists, Program C provides basic education on communication skills. Program B, which includes Program C, is for clinicians who care for patients with serious illness but are not primarily responsible for initiating or leading goals-of-care discussions, such as general surgeons, infectious disease specialists, gastroenterologists, and orthopedic surgeons. Program A, which includes materials from Programs B and C, is for those clinicians who are directly and primarily responsible for patients with serious illness, such as oncologists, emergency department physicians, intensivists, geriatricians, and hospitalists.
Rosen explained that over the past several years, the institution has conducted an awareness campaign that included systemwide special events focused on serious illness care and communication. For example, Diane Meier, who founded the Center to Advance Palliative Care, spoke in February 2021 on “listening for the heart of the matter” to connect with serious illness patients. These awareness-raising events are a component of Program C, Rosen explained. Program B uses the Center to Advance Palliative Care’s communication skills e-modules and has conducted several department-specific sessions using the five training modules.
Rosen explained that Program A includes Ariadne Labs’ guide on serious illness communication (Ariadne Labs, 2023) delivered in a small-group setting, with a role play–based education curriculum, which allows people to practice using the conversation guide. Rosen’s team trimmed the training down to about 2.5 hours, which increases the likelihood that busy clinicians will participate. Rosen noted that 103 physicians and advanced practice providers have completed Program A, and the team has trained six internal trainers, including three to teach other trainers.
Rosen’s team is now studying the effect of this curriculum using pre- and post-surveys and rolled out an institutional review board–approved survey for all inpatient and emergency department nurses to better understand their perceptions of the culture of serious illness care at Cedars-Sinai. Nurses see more caregiver and family distress and know more about what patients are thinking and feeling, so they can be good judges of how well physicians are responding to and addressing what is important to the patient and family. More recently, Rosen and his colleagues have begun to explore
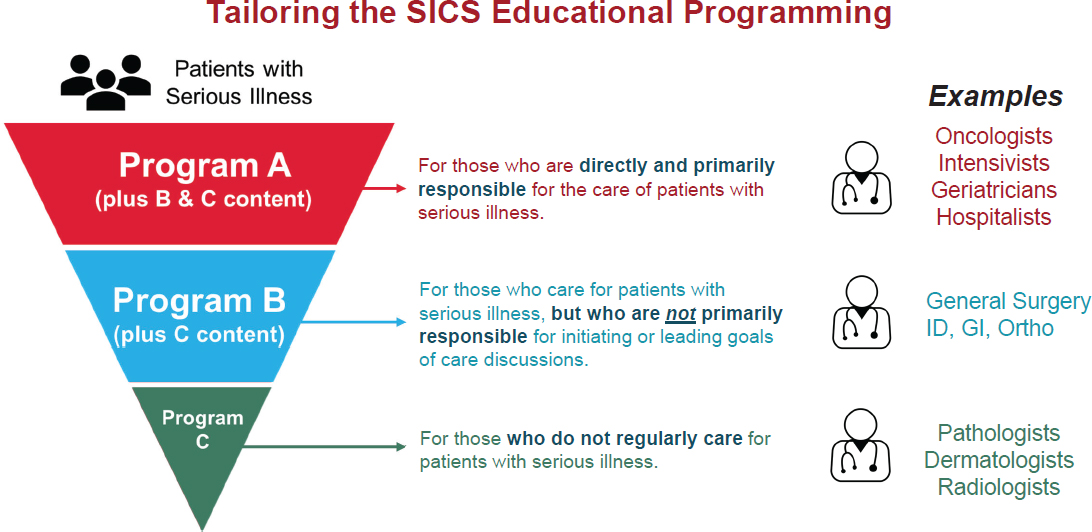
SOURCE: Presented by Bradley Rosen on May 28, 2023.
whether they can use artificial intelligence, natural language processing, and machine learning algorithms to identify seriously ill patients in real time.
In terms of lessons learned, Rosen said leadership endorsement and support are critical, as is providing dedicated time for clinicians to engage and learn. As many clinicians do not believe they need training—they do think others need it—incorporating the Center to Advance Palliative Care’s modules into staff meetings or normal department meetings has been valuable. Institutional support and resources are needed for administrative support to organize and keep the program moving and have funds to pay for the training and role-playing actors. Rosen noted that the program has sometimes paid clinicians to take the training, which he feels is worthwhile, given the importance of the training. Another lesson, added Rosen, was the value of hardwiring goal-concordant care into the way the institution does quality and performance improvement work.
Going forward, the plan is to continue a broad rollout of the program’s education efforts, which Rosen said remains a challenge because everyone is so busy. He hopes to expand training to other disciplines, such as nursing and social work, and other frontline clinicians with an opportunity to engage meaningfully with patients, their families, and their caregivers. There will be a concerted effort to measure what works, refine the program, and solidify plans to sustain this effort over the long term. Finally, Rosen and his team will continue efforts to implement mechanisms for real-time identification of and interventions for seriously ill patients.
Healing Healthcare Initiative Pilot Program
Lown opened the session’s final presentation by providing some background on the Schwartz Center for Compassionate Healthcare, a national organization whose mission is to put compassion at the heart of health care. She explained that it uses programs, education, and advocacy to support the mental health and well-being of the health care workforce so it can provide compassionate care to patients and families. As Lown noted earlier, the Schwartz Center’s evidence-based programs and resources have proven to be versatile, sustainable, and effective across diverse settings. She shared that research has found that psychological distress among people who take part in Schwartz Rounds is significantly lower than for those who do not participate (Dawson et al., 2021).
Lown reemphasized that the need for healing among clinicians is critical, as they are exhausted, stretched thin, and burned out at best and
anxious, depressed, and suffering from traumatic stress at worst. This is causing hospitals and health systems to experience unprecedented worker turnover and shortages that directly affect an organization’s financial stability and the quality and safety of its patient care activities. “I think that the values and the financial, and infrastructure, and policies that guide health care do not align with why people are called to do medicine, nursing, and all the other kinds of helping professions,” said Lown. “That is a really serious source not just of moral distress but of significant heartbreak and despair.”
For those and other reasons, the Schwartz Center in January 2023 launched its Healing Healthcare Initiative pilot, an education and support program for C-suite executives and clinical and administrative executive leaders. This initiative, explained Lown, guides health care leaders to reimagine their organization’s operations so they can find strength and safety in prioritizing their well-being and deliver equitable, safe, and compassionate patient care. The program has two primary goals: to provide the resources, information, mentorship, and guidance that people need to do this work and a safe space for reflection, team building, and honest conversations.
Lown explained that the Healing Healthcare Initiative framework is based on an extensive literature review, the evidence on how to recover from trauma, how an organization can become trauma preventive rather than trauma inducing, and the Substance Abuse and Mental Health Services Administration’s concept of trauma.26 The framework focuses on six principles:
- Psychological and physical safety: leaders will help create an environment that people can trust to insulate them as well as possible from psychological and physical harm;
- Inclusion, voice, and choice: involving and including health care workers in decisions that will affect their ability to provide relationship-based, high-quality care without administrative burden;
- Diversity and equity: leaders participate in and commit resources to promoting equity and dismantling all forms of structurally embedded discrimination;
- Team cohesiveness and collaboration: workers have opportunities to learn about and from one another to foster mutual respect, knowledge sharing, and perspective taking;
___________________
26 See https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4816_litreview.pdf (accessed September 11, 2023).
- Trust and trustworthiness: sharing organizational and operational information and decisions to maintain trust; and
- Mental health and well-being supported by the other five principles.
These principles, explained Lown, are all integrated with the involvement and engagement of organizational leaders and health care workers through training, education, assessment, and monitoring.
In describing the program, Lown pointed out several components to build community, facilitate learning, and promote action across the six pilot sites. Cohort meetings, Schwartz Rounds, learning collaboratives, and expert-led sessions help create community among health care leaders to share promising practices and learn from one another. Online resources and education, learning collaboratives, leadership learning sessions, and mentoring support health care leaders’ work to break down silos in their organizations and facilitate peer learning across organizations in the Healing Healthcare Initiative community. Team-building sessions and implementation planning supplies health system leaders with the tools they need to identify and implement the right solutions to enhance the experience for all who provide and receive care. During the action phase of the 1-year pilot program, Lown noted that the teams will think about what they are doing now in terms of their programs, operations, and strategies and how they might begin to think about embedding one or two of the key principles into what they do as an organization.
The Schwartz Center issued a competitive application to its members and selected six sites that include a mix of adult and pediatric sites, academic and public hospitals, and a rehabilitation and research institute. Lown explained that an organizational practice survey was developed that asked the sites to outline what they are doing in terms of programs, policies, practices, and resource allocation; how they are measuring their efforts related to each key principle; and whether they have performance goals or key performance indicators for any of the principles. “In truth, really, that was missing across the board for all of the key principles,” said Lown.
A leadership survey explored whether leaders had the practical tools and support for each key principle and if they thought they knew what health care workers in their organizations needed to support these. Lown shared that there was remarkable diversity of responses across the leadership teams. “They themselves are not all totally on the same page with what they are doing and where they should be going,” said Lown, which led to the goal of integrating people across organizational silos. “We know people are
doing great things, but they are doing [them] in pockets and they are not integrating across the organization or the system,” observed Lown. “That is really hampering their efforts and part of the reason they do not see anything really changing.”
Lown said the program will conduct a health worker survey, and each site will organize a program organizational committee to help identify problems, set goals, co-create solutions, and implement plans. They will also create a compassion dashboard of key performance indicators for the one or two key principles on which they choose to focus during the 1-year pilot. She added there is no expectation for long-term outcomes during the 1-year pilot, but she is hoping there will be some implementation and lessons learned to take forward. The program provides each site with leader survey displays that include heat maps regarding the extent of agreement among team members.
Highlighting some of the lessons learned, Lown noted that the chief executive officer has to buy into the pilot for teams to participate. Another lesson is that the leaders in the program are hungry for guidance and want to do the right thing. Lown explained that they want concrete, practical steps they can take. An additional lesson is the ideas that will get traction require discussion, reflection, and relationship building within the team and across the organization.
Lown noted that one team, as it went through identifying its organization’s values, realized that mental health and well-being were not articulated as a core value. One of the leaders concluded that should be an organizational value and that the organization needs to put resources behind it. She also commented that leaders are not immune to suffering, know large numbers of staff are leaving the field, and want to do the right thing. Lown hopes that the Schwartz Center can contribute in some small measure to address workforce needs beyond the pilot.
Lown listed some policy levers and changes needed to achieve the program’s objectives:
- Investing in meeting the mental and behavioral health needs of the nation;
- Ensuring adequate health workers and time to address patients’ needs, which will require payment model reform to increase time with patients and support to meet their medical and social needs;
- Educating and deploying a diverse workforce in proportion to population needs, which will require adopting national strategies
- for health worker education and accreditation that will address anticipated shortages and providing incentives to select health workers from and train them in rural and underserved areas;
- Strengthening accreditation requirements to include demonstration of positive work and learning environments that are free of racism and discrimination based on gender, race, ethnicity, sexual identification, and ability; and
- Investing in research on interventions that promote the key principles of the Healing Healthcare Initiative.
Panel Discussion
Session moderator Joseph Shega asked the panelists how the pandemic informed, helped scale, and changed what their programs were doing. Rosen responded that the pandemic disrupted everything Cedars-Sinai’s Serious Illness Communication Program was trying to do. However, he and his colleagues realized relatively quickly that many clinicians were looking to the organization’s supportive care medicine team and the educational steering committee for guidance on how to approach caring for COVID-19 patients. One unique factor that made it particularly difficult to care for those patients was the lack of any idea about what the trajectory would be for many of these patients. This made it even harder to have conversations about goals of care, Rosen explained, as many had not had serious illness before they became acutely ill. “I think the work we had done over the years leading up to the pandemic really served us well in terms of anchoring people with how to approach some of these difficult situations,” said Rosen.
Espinoza said that the pandemic amplified and made visible the direct care workforce’s long-standing challenges in terms of inadequate compensation, workforce shortages, lack of training standards, and other issues. He believes that bringing these issues to the fore has created opportunities for interventions to address them. The pandemic also left direct care and long-term care workers with emotional stress and grief compounded by the lack of grief support and bereavement leave, paid family and medical leave, and the ability to seek reprieve and emotional support for that stress and duress. At the same time, the pandemic, at least temporarily, led to significant financial resources being available to improve these jobs, but he fears that as pandemic relief funds dry up, any improvements will disappear. It is unclear, said Espinoza, what this means for the training landscape, direct care workers’ compensation and ability to survive, and the next crisis to
hit health care, given that the needs of the direct care workforce are not temporary.
Biewald observed that from the perspective of the midcareer fellowship, the pandemic drew attention to the value of palliative medicine. Many physicians who had never had a goals-of-care conversation before were suddenly forced to do so and realized that they either did not have the skills they needed or that they loved doing so, prompting them to pursue that kind of training.
To Lown, the burnout epidemic, which started before the pandemic, is an occupational syndrome, not an individual failing. As a result, it must be addressed at the systems level. She stressed that she hopes everyone will focus on the problem at the societal level to align the values with what patients and the workforce need.
Shega asked the panelists to list steps, gleaned from their interventions, he could bring to his chief executive officer to reduce workforce burnout or affect the workforce positively. One step, said Biewald, would be to create avenues for workers to gain further training and advance their careers. Rosen said it is important for the workforce to feel cared for and supported, because then they can give their best. One option is to institute Schwartz Rounds, which his institution did to give its workforce an outlet and a means of “refilling their tanks.”
For the direct care workforce, Espinoza suggested adopting his organization’s job quality framework and 29 concrete strategies for improving supervision, offering grief support and bereavement leave, and ensuring that employees receive a livable wage, among others. He reemphasized that workers often leave to find better-paying jobs. It is important to understand both the living wage and competitive wage for a given location. “That often requires a systematic wage analysis of the region from which workers are being drawn,” concluded Espinoza.
Audience Q & A
Bowman underscored the importance of scaling the work the panelists discussed and the role that stories about why clinicians work in palliative care can play in doing so. She asked the panelists to share stories about why people are entering programs such as the midcareer fellowship and the Cedars-Sinai training program. one. Biewald said one reason people seek to participate in the fellowship program is that they want training to help them become meaningfully connected to a larger cohort of physicians.
Rosen noted that many practicing clinicians do not realize that they need additional training to improve their skills, so stories that serve to underscore the importance of training to system leadership are helpful.
Carol Peden, from the BlueCross BlueShield Association, suggested Biewald add anesthesiology and pediatrics to the list of specialties that can participate in the midcareer fellowship program because of their intensive care aspects and that the other panelists do not forget surgical patients, particularly emergency general surgical and laparotomy patients, because of the high associated death rate. She noted her organization was about to publish the third part of the International Enhanced Recovery Guidelines for emergency laparotomy procedures, which will be the first enhanced recovery guidelines to include a focus on end-of-life care.
Biewald replied that the program would soon recruit its first surgeon. She noted how important the program could be a promising model for surgeons, particularly in light of research indicating that barriers to fellowship training for surgeons include the concern that stepping away from surgical practice for a year might have a negative impact on a surgeon’s skill set. She added that her program has started working with the Anesthesia Board to approve the fellowship program (Salyer et al., 2023). Rosen remarked that his program included anesthesiologists at the program A and B levels, and they were “semi willing participants.” His team has had great engagement with his institution’s trauma surgeons, which led the program to engage with attending physicians in the surgical ICU and other surgical subspecialties who have started to take an interest in the subject. Some attendings have started using some of the guidelines regarding when to have goals-of-care conversations.
More recently, said Rosen, the head of his institution’s liver transplant program, who for years had equated goals of care and palliative medicine with giving up, hospice, and death, invited the supportive care medicine team into the care of all transplanted patients or patients on the transplant list in the surgical ICU. Getting to this point, he said, has taken years, but there is progress on this front.
Amy Melnick, from the National Coalition for Hospice and Palliative Care, asked Priselac and Rosen whether had they shared their stories with the heads of other hospitals and whether other hospitals are interested in replicating their program. She also asked Biewald whether any other institutions are offering midcareer fellowships. Priselac replied that the short answer to her question is yes. “There are a number of professional groups that I happen to participate in around the country,” said Priselac, “and
the interest in this topic has grown in all of those settings.” Priselac also commented that although the shift to a value-based care system creates the platform around which this work can occur, challenges arise when systems and payers execute the approach to value-based care poorly.
Rosen added that his team’s collaboration with the Center to Advance Palliative Care has been strong, with discussions across institutions. In addition, the director of Cedars-Sinai’s palliative care fellowship has been talking with colleagues at other institutions, which is helping to spread the word about the program. Biewald explained that the mid-career fellowship program is still in the pilot phase, so it is limited to its current seven sites, but excitement is building about scaling it after 2025, when the pilot finishes and releases its data. “There is a lot of potential for this as a pathway for people who have been practicing palliative medicine for years but are not board certified,” said Biewald.
Rodgers asked Biewald about payment for the time that clinicians spend in the fellowship program. Biewald replied that each site had its own procedures. For example, one fellow had grant funding, and another received 20 percent of their salary through the general medical education office. In terms of administrative support, the program has been relying on staff that already have program director and program coordinator roles. However, she added, a meaningful scaling will need to have a mechanism to provide additional administrative support.
Rodgers then asked Priselac and Rosen whether they had ideas on how they will measure when the program has achieved goal-concordant care, which will be important for implementing it in a busy practice where seriously ill patients receive care in the ICU, the emergency department, and home. Rosen replied that he and his colleagues have thought about measuring goal-concordant care, which is difficult. “The reality is that people can be receiving goal-concordant care and receive more care. They can still go to the ICU, but they can still receive very aggressive care,” said Rosen. He noted the importance of providing medically effective care, which differs from goal-concordant care. He also mentioned the importance of having goals-of-care conversations early so clinicians get an early understanding of who the patients are and what is important to them, which makes conversations about difficult decisions a little easier to manage. Priselac agreed that goal-concordant care is an area where measuring outcome effectiveness is challenging. There are indirect measures, such as patient satisfaction, but assessing effectiveness is limited to asking the question of why a result contradicts what was expected. He said this is not the best way, but it might be the best available approach.
THE SERIOUS ILLNESS CARE WORKFORCE: A CALL FOR RADICAL TRANSFORMATION
The workshop’s closing session brought together several experts to consider ways to best support all members of the workforce caring for people with serious illness. Moderated by James Tulsky, professor of medicine at Harvard Medical School, chief of the division of palliative medicine at Brigham and Women’s Hospital, and the Poorvu Jaffe chair of psychosocial oncology and palliative care at the Dana-Farber Cancer Institute, the session aimed to pull together the key themes discussed throughout the workshop.
Tulsky noted that one challenging workforce issue is that people are spending too much time doing things they are not best suited for or are not working at the top of their licenses or skill sets. While technology could address this, Tulsky pointed out that many people are worried that it might add to their workload. Tulsky asked the panelists for ideas on how technology might change workflows or the nature of jobs and how to ensure that it supports high-quality care.
Tammie Quest, director of the Emory Palliative Care Center and professor of emergency medicine at the Emory University School of Medicine, described how during the pandemic, Emory took about 2 weeks to radically transform care delivery and increase the use of technology. “I believe that for a lot of our workforce, the use of technology is an answer to some of the burdens that they see,” observed Quest. For example, social workers are now scarce in inpatient settings, and as lower-paid members of the palliative care team, they can benefit from the convenience and ability to provide better care that technology affords. For Quest, adopting technology is about evolving as a field to believe that an integrated model of in-person care and telehealth can build the resilience and depth of the workforce. “This is really about us being able to evolve as a field to believe that we can have integrated care models” that feature in-person and remote care, observed Quest.
Ashley Leak Bryant, Francis Hill Fox Distinguished Professor in nursing at the University of North Carolina at Chapel Hill School of Nursing and assistant director of cancer research training and education coordination at the UNC Lineberger Comprehensive Cancer Center, said that her state is primarily rural, and technology would benefit many of her institution’s patients, families, and direct care workers. “I think technology is amazing, but everyone does not even have access even right now in 2023,” said Bryant. Quest noted that the standard telephone is still an option, and research has shown that telephonic interventions work without face-to-face
video (Chen et al., 2022), but payer models do not necessarily support telephonic visits.
Sachin Jain, chief executive officer of Scan Health Plan, said one of the “biggest pathologies” in health care has been that every introduction of technology has focused on taking analog processes and making them digital, as opposed to looking at a problem from a new perspective. Too many health professionals today self-describe as data entry analysts. “We have to think about whether all of that data [are] actually necessary,” said Jain, who added that some people are interested in capturing as much data as possible for reasons not necessarily connected to patient care or real quality improvement. In his view, it would be worth looking at which data are necessary, which are not, and whether passive collection would be effective for some data.
R. Sean Morrison, the Ellen and Howard C. Katz Professor and chair and director of the National Palliative Care Research Center at the Icahn School of Medicine at Mount Sinai, agreed with Jain and added that the health care industry will adopt a new technology that appears to solve a problem and implement it quickly and at a scale that does not happen in other industries. As a result, unintended consequences are identified much too late, as in the case of electronic health records. He worries about the enthusiasm around telehealth as a technological solution to providing care, particularly given the concerns that Bryant raised about those individuals without Internet access or smartphones. For him, a key question is whether a new technology will improve care for the most vulnerable populations; if so, it will work for most people. Morrison then proposed three other questions that need to be answered before deploying a new technology:
- Is there a real problem that needs solving?
- Does technology solve a problem for the most vulnerable populations?
- What are the possible unintended consequences?
Tulsky observed that Morrison’s comments highlight the tension between viewing the health care system as so broken that it needs rebuilding and the likelihood that rebuilding would create more problems. Tulsky pointed out that in his view, any radical restructuring of the health care system will involve changing the work people do. For example, the traditional way of providing mental health care has been via frequent, long appointments with expensive clinicians, which Tulsky said is highly ineffective and does not meet the needs of most people. Research has shown that collaborative care, which allows several people to be involved in patient care and
uses less time from the most expensive and least available clinicians, such as psychiatrists, is an effective approach (Gilbody et al., 2006; Møller et al., 2018), but it requires people to work in a new way, essentially changing their jobs. Tulsky explained that his institution has been trying to implement collaborative care for psychosocial oncology and palliative care and asking clinicians to provide outcome-driven care, which can create tension. “Adoption of these kinds of models can meet a lot of resistance in the workforce, and yet it may be the only way we can actually realize [solutions to] our workforce shortage problems,” said Tulsky. He asked the panelists for ideas on ways to engage the workforce in effective change.
Jain replied that the workforce largely feels unseen and unheard, which he believes results from toxic positivity and not acknowledging the deep issues that exist. Noting that it is normal to talk about how broken the system is at expert meetings, “I am not sure how normal it is within most health systems to actually engage the problems and talk about them as we experience them,” said Jain. As a result, health systems introduce changes in jobs, processes, and approaches without sufficiently motivating staff to solve the existing problem. The solution, said Jain, is to start speaking more authentically about the most challenging issues to get staff to engage, buy in, and work to address the problem.
Morrison pointed out that it is important to recognize the people who are innovators and have a broad view of their job description. It may be fruitful to identify them and ask them to create new models. He suggested that workforce innovations developed by partnerships between academia and large, not-for-profit health systems would be scalable, given that competition in the marketplace breeds copycats.
Industry, said Tulsky, uses early adopters to test new innovations with the acceptance that some people will leave the organization rather than change. Morrison replied, “We are losing people anyway. We have more turnover than we have ever had before…. We may lose people, but we may lose people because it is not the right fit and bring in the people that we want to have.” The thing to watch for, he added, is whether the turnover rate increases when a new technology is introduced.
Bryant emphasized that part of the reason that health care is experiencing a workforce crisis is because it does not invite the right people to the table when issues and possible solutions are first discussed. She called for inclusion of all health care workers, including “[e]nvironmental Services workers, pharmacy technicians, CNA, [and] others who are typically not even at the table, but these decisions are made about them and for them.”
She encouraged everyone developing committees to ensure that the people who need to be there are represented. If they are not, their absence should be acknowledged, emphasized Bryant. Quest shared that she continues to repeatedly hear that the best use of a palliative care team is in facilitation rather than direct patient care. “We have to sort of decide as a specialty what our job is and what sort of real value we are bringing to the table,” said Quest. These teams provide workforce support in different circumstances, she explained, such as compassion fatigue, and also teach fellows, both of which are not part of their primary role, but which other members of the health care team find valuable. “I would also say that we’ve not come to terms with the cost of doing business … which is actually supporting the workforce. And that cannot be an unfunded mandate. A radical idea would be that for every patient … that there is a wellbeing charge tax to their bill to actually support the programs we need to take care of the patients,” Quest suggested.
Tulsky asked Quest whether she believes that people entering the palliative care field want to be providing staff support rather than direct care or whether the field needs to identify those in both categories. Quest noted a tension between those two roles, and it will be necessary to start promulgating the idea that a palliative medicine fellowship will train clinicians how to care for patients with palliative care needs and how to teach others, and also support other members of the care team.
Referencing Jain’s characterization of the tendency for leaders to “normalize the abnormal,”27 Tulsky asked the panelists for ideas about ways to create an environment in which leaders are willing to address problems and promote change where needed. Jain said it is hard to see the situation in health care as anything other than a leadership crisis. Leaders, he said, have promoted the dangerous idea that health care is like every other industry and allowed analogies from other interests to enter the conversation. “We need to start training a generation of leaders who are actually comfortable with the idea that health care is a different endeavor,” said Jain. “It is a human endeavor that actually has a different set of rules and a different kind of physics associated with it and a different economics associated with it than other industries.”
Another issue, noted Quest, is that health care has not come to terms with the cost of doing business, which is supporting the workforce. “[This]
___________________
27 See, for example, Jain, Sachin, 10 Abnormal Practices We Have Normalized in U.S. Healthcare. Forbes, June 28, 2023.
cannot be an unfunded mandate,” said Quest. A radical idea would be to add a well-being charge to every patient’s bill that would support the programs needed for patient care. Tulsky worried about anything that adds cost to what is already the most expensive health care system in the world. Quest noted plenty of waste in the system to redirect some of it to education and training. The key is to fund training in a way that does not rely on the kindness and understanding of system executives to enact some of the programs discussed at the workshop, Quest added.
Morrison pointed out that health care is a big enough industry with a host of natural leaders. The challenge lies in identifying those natural leaders, and giving them the knowledge, skills, and technical assistance to succeed. “Most training programs today across all key specialties do not do this,” said Morrison. Health care, he said, is one of the few industries that believes philanthropy should fund leadership training rather than include it as a core aspect of the training workers receive. Morrison asked Biewald to describe Mount Sinai’s fellowship program. Biewald explained that Mount Sinai, under the direction of the vice chair for education, has started a 2-year geriatrics and palliative care leadership fellowship, known as the LEAP Program.28 She explained that the first year focuses primarily on clinical knowledge, and the second year is a degree program or advanced work in leadership and a capstone project. This year, the first two palliative care fellows at her institution will step into the leadership year.
Picking up on the leadership theme, Bryant underscored the need for bold leaders willing to do things differently, yet many leaders are not courageous in their support for change, given factors such as the impact on friendships, relationships, and the bottom line. “I think the elephant in the room when we are thinking about sustainable change is that there are relationships that may be broken” based on some core leadership values, Bryant observed.
Responding to the discussion about leadership, Jain said “I think we are confusing administration and leadership.” Leadership, he said involves speaking uncomfortable truths and challenging the status quo. However, much of what leadership programs are teaching is to function within an already broken system as opposed to empowering people to speak up and support more radical and transformative change that might go against a status quo from which everyone is profiting and doing well. Noting that
___________________
28 Additional information is available at https://icahn.mssm.edu/education/residencies-fellowships/list/leap-geriatrics-leadership.
leadership is different from title holding, Jain remarked that “[i]f you were to step outside health care and say what does leadership look like, I think we would be talking about Ghandhi and Martin Luther King.”
Tulsky noted that many programs discussed at the workshop have to do with training, and he wondered whether training is the answer: “can we train ourselves out of this problem?” Bryant replied that although she does not think one can overtrain, training must be ongoing, with booster sessions along the way. “You cannot just train one time and think people are going to remember,” she said, adding that mentoring should be a key piece. She highlighted a program focused on building the cancer clinical workforce that works with North Carolina Central University, a historically Black college and university (HBCU) located 10 miles from Chapel Hill. Bryant characterized the program as an innovative approach to collaborating with HBCUs and tribal institutions, explaining that “when I think of clinical trial diversity, it’s more than just underrepresented racial ethnic minorities.” She emphasized the need to think more broadly about workforce diversity, which will include ensuring diversity among regulatory associates, research assistants, and project managers.
Tulsky asked the panelists to propose short-term, realistic solutions that are not so big and overwhelming that they are nonstarters. Quest said she wants to see a new validated outcome measure for palliative care that reveals how much value palliative care adds to the system by enhancing others’ work in a way that makes them more effective; an example being how many more patients an oncologist can see given contributions of palliative care.
Jain proposed helping local health systems and organizations overcome their ambivalence about being paid differently and turn talk about value-based care into action. He would also like health care to quit normalizing the abnormal—prior authorization, for example—as the first step to addressing the abnormal and to stop accepting that the pace of change must take years. He said he is getting more comfortable with moving with more momentum in new directions as opposed to fetishizing pilot projects and then talking about them for years.
Morrison pointed out that many small innovations are available that work well that now need to be disseminated rather than having to reinvent the wheel. He noted that the Center to Advance Palliative Care has been a model of doing just that. He also said the nation needs to decide whether the growth of for-profit companies moving into health care is a good or bad thing. In his mind, it is a bad thing that a goal of health care might be to maximize return on investment to shareholders and not to put the needs
of patients and families first. Morrison pointed to accumulating data that show that when health care becomes a for-profit endeavor, quality decreases (Crowley et al., 2021; Paul et al., 2016). “We as a profession have to decide whether this is something that we are going to stand up and say ‘enough,’ or whether it’s going to be okay, because the shift to value-based care is an opportunity,” said Morrison. When asked about the next step, he said it would be to speak to patients’ and families in a concerted way about how health care costs are paid, and the differences, for example, between traditional fee-for-service Medicare and Medicare Advantage so the public can be better informed about changes that need to be made on a policy level to address existing problems.
Bryant shared her concern about the severe global nursing shortage. “We need to make sure we have the trained educators to continue to train nurses interested in caring for those with serious illness,” she said. “We have to rethink our models of care, particularly when it comes to how we are educating nurses.” She endorsed the idea of executive programs, accelerated programs, and weekend options, given that the traditional options are not solving the problem.
Asked to respond to the question he posed to the panelists, Tulsky responded that it is about restructuring care delivery along the lines of the collaborative care model. “We need to build those models for the work that we do, and then we need to just incessantly advocate for it,” he said. He reiterated that research has shown that collaborative care is effective for mental health care and that a fair number of health care systems have implemented it.
Audience Q & A
Karen Bullock, licensed clinical social worker and health equity researcher, commented that “we don’t want to continue to build these boxes that we try to force fit people into,” because that approach will not solve the current problems. Instead, what needs to be acknowledged is the diversity of need and the complexity that it brings. She added that she appreciated one of the panelist’s characterization of social workers as “a scarce resource” and underscored that social workers are “uniquely trained and prepared to contribute to interdisciplinary teams.”
Masami Kelly, from the Center for Surgery and Public Health at Brigham and Women’s Hospital and the Heller School of Social Policy and Management, observed that everything she heard throughout the workshop seemed
to indicate movement toward a new era of more deeply humanizing serious illness care. She asked the panel for ideas on how to expand organizational capacity to address the needs of health care workers given that change will need to happen at the individual, team, and organization levels. Bryant replied she sees more institutions adding a chief wellness officer to the executive suite. “We need to rethink and maybe even create new job descriptions for who else is missing for us really to tackle these concerns,” said Bryant.
Chung, who spoke in the first session, said they agreed with Jain’s comment about toxic positivity. They added that some of the radical transformation in palliative medicine is shifting care from a strength-based framework to a trauma-informed and grief-informed framework. Chung then asked the panelists for thoughts about interdisciplinary leadership and training and, if that kind of training exists, where those efforts are happening. Bryant said she agreed that more interprofessional training is needed, and her institution encourages students from different disciplines to work together. For Bryant, interprofessional, collaborative, team-based care is the “secret sauce” for why palliative care works the way it does, which is one reason the collaborative care model needs to be a core piece of the education model.
Quest said the challenge for the collaborative care model is that the current payment system does not reimburse the entire multidisciplinary team. “The inability for our social work colleagues, as well as our spiritual health colleagues, to be able to bill for what they do, I think, is a major barrier to the interdisciplinary team’s viability,” said Quest. She worries that the interdisciplinary team remains threatened. Changing the system to one that is value based will require policy reform, she added.
Jain cautioned that much of what passes as team-based care is people practicing alongside instead of with each other. “I think so much of what we are calling team-based care is actually labor arbitrage,” said Jain. “It is putting lower-skilled professionals in front of patients instead of higher-skilled professionals at every level, and then calling it team-based care.” He added that clinicians whom he knows with various types of training feel underequipped to engage in team-based care. This argues for teaching the precepts of team-based care from the beginning of medical education.
Carol Peden agreed with Jain’s comment to stop admiring and testing models of value-based care and just implement them. She noted her organization is considering using its research operation and data and perhaps partnering with academic institutions to examine these models in action. Rodgers also agreed that the time is right to implement value-based care models and innovate and asked Jain what he thinks payment and delivery
models will look like in the near future. Jain replied that as more Medicare beneficiaries move to Medicare Advantage—projections estimate that 70–90 percent of Medicare beneficiaries will be on Medicare Advantage plans in the next 5–10 years (Ochieng et al., 2023)—there is an opportunity to change how health care dollars are allocated (Christ, 2023; McWilliams, 2022).
That opportunity, said Jain, is to implement risk delegation to provider groups, which would address the problem that insurance companies pay medical groups in irrational ways that make it difficult for them to administer benefits that are pro-patient. Moreover, such a change would enable health care dollars to be spent more rationally. Medical groups would then do their own use management and partner with plans to identify which benefits might lead to better patient outcomes. In Jain’s opinion, allowing medical groups and health systems to control more health care dollars and organize and spend as they see fit to manage the total cost of patient care will lead to more appropriate use of palliative care. This shift will not be easy. “There is a historical resistance to that type of approach because it involves taking on the full health care dollar and then owning all the risk that is associated with it, whether it is high-cost transplants or genetic therapies, and so it is not to be entered into lightly,” said Jain.
Nevertheless, he said, making that transition will reduce more of the friction and create more of the freedom everyone is seeking. Jain said that when health systems own the total expenditure for patients, they will invest more in prevention, primary care, and chronic disease management. This transition would also treat hospitals as cost centers rather than revenue centers. “I think that is the model that we should be driving toward if Medicare Advantage ends up as prominent as it is likely to become,” he said.
Tulsky asked the panelists to talk about what most allows them to be optimistic about the future. Quest said she is most optimistic that the field can innovate, given how health care systems innovated so effectively during the pandemic. Morrison said he is most optimistic about the new generation of leaders who are impatient, willing to tackle hard problems, and unwilling to accept the status quo. Bryant, who sees herself as part of that new generation, agreed with Morrison. She is optimistic that these leaders can work with leaders in Congress to make needed policy changes. Jain said he is optimistic that health care is finally at a place where it is calling things what they are, which will lead to progress. “You cannot solve a problem unless you have actually appropriately defined it,” said Jain. Tulsky
concluded by saying he is also most optimistic about the people because the people who come from serious illness care make very good leaders.
VIDEO MONTAGE: VOICES OF THE SERIOUS ILLNESS CARE WORKFORCE
To close the workshop with an overarching sense of optimism, the planning committee assembled a montage of voices to deliver an optimistic message. Andy Awari, a hospice and palliative medicine physician, said what drew him and keeps him in palliative medicine is its philosophy of providing holistic, interdisciplinary care for patients and their families, which was not how he was trained. His training focused on physical diagnoses and treatment but not necessarily working as a team. “It has to be recognized that patients have needs that go above and beyond their physical ailments,” said Awari. They need psychosocial and spiritual support, and for that to be provided in a coordinated and holistic manner, it must involve other professionals.
Palliative care, said Awari, is the model that can provide that care, and it should be the idea to which all areas of health aspire. “I am hopeful that as time goes by, that will become our prevalent care model and the standard of care that we provide patients and families,” he said. Awari said he stays in the field because he believes it is important to continue to advocate and educate patients, families, and health care providers and make progress toward that goal.
Keara Barnaby, an oncology physician assistant, said she has always loved oncology because it gives her the chance to deliver comprehensive, compassionate care to her patients throughout their journey with cancer. However, she has seen over the last decade that providers have become so specialized and siloed in their individual areas that they do not look at the whole patient anymore. Barnaby said that in her quest for more tools to deliver better care, she enrolled in a palliative care master’s degree program and has appreciated the broad approach palliative care takes in working with patients. Although she has gotten so much from the program, both professionally and personally, the most important aspect is that it has helped her provide good, compassionate, and comprehensive care that affects her patients’ lives in a positive way.
Gabriella Patrone, a master’s degree student in palliative care, said although she is new to the field, she is hopeful about all that is to come, especially as people are living longer. In particular, she is optimistic about
the transition from focusing on how to cure a patient to learning how to meet a patient’s needs. At age 25, she hopes to be part of that change.
Kristin Watson, an outpatient cardiology pharmacist, said that although she is not a palliative care specialist, it has been imperative for her to learn about the integral aspects of the field so she can provide the best care to the patients she serves as a member of their health care team. She said all individuals with chronic, life-limiting diseases, such as heart failure, would benefit from support from a palliative care team. As that is not the reality, she has taken to learning aspects of palliative care that have improved her communication skills, including having hard conversations with patients and identifying goals of care. She has also learned how she can work with a patient to jointly support their physical, mental, and spiritual health. “In this post-pandemic era, I feel these skills are even more important to have,” said Watson.
Bruce Gutierrez, an emergency medicine physician finishing a 1-year fellowship in hospice and palliative medicine, said his day-to-day work in the emergency department often involved providing aggressive medical interventions to patients who may not have wanted it. During the pandemic, however, he had an elderly patient with severe respiratory symptoms who would have been intubated. He was able to have an urgent care discussion with her; based on her goals and values, she opted not to be intubated or resuscitated and died peacefully in the emergency department that day.
Palliative care, said Gutierrez, has allowed him to see patients with serious illness and their families as people first, which he said has been refreshing. “Focusing on what is most important to them and working together to figure out how to improve the quality of life has been a truly rewarding experience,” said Gutierrez. What excites him now is the opportunity to incorporate palliative care in the emergency department and make a difference in the lives of patients with serious illness and their families.
Closing Remarks
Bowman shared that the planning committee knew this would be a difficult workshop because the issues are so challenging. However, she said, “[The] voices of people who have chosen to enter the field because it is the place that they see themselves most at home inside of this big broken machine of U.S. health care really does make me feel optimistic and really appreciate all of our colleagues working together in this field.” She noted that the workshop discussed training and education, racism, immigration,
value, respect, compassion, innovation, and payment—many of the key issues that could contribute to the complexity of the workforce.
Bowman said it strikes her that talking about the health of the workforce is not a bad proxy for the health of the system itself, which is not good. She explained that she, her planning committee co-chair, and the rest of the committee spent a great deal of time thinking about how to manage the tension between what can be done today inside the system to make small but meaningful improvements and the knowledge that if the system is broken, it needs transformative change. The answer, she said, is both and not one or the other. She hopes that the workshop reenergized those who attended, provided practical ideas and solutions they can put in place in their organization today, and provided fodder and energy for the courageous voices thinking about the transformative change that health care needs to fix the situation. Reifsnyder pointed out that she heard from the speakers that if there is one thing that could happen, it would be to institutionalize wellbeing across health care organizations. “Perhaps there is one thing, just one thing, that each of us could do when we go back to work,” she concluded.
This page intentionally left blank.































































































