Reusable Health Care Textiles for Use in Personal Protective Equipment: Proceedings of a Workshop (2024)
Chapter: 7 Decision-Making Support
7
Decision-Making Support
The sixth session of the workshop featured a case study of a reusable isolation gown pilot program and outlined a decision-support framework that health care organizations could consider in exploring the incorporation of more reusable health care textiles (HCTs) into operations. Jacqueline Daley, senior director of infection prevention at Providence St. Joseph Health in Irvine, California, moderated the session and provided a brief overview of the decision-support framework for the adoption of reusable personal protective equipment (PPE). The framework features four categories—strategic analysis, tactical analysis, operations analysis, and impact assessment—and each category involves engagement with personnel from various areas of expertise (see Figure 7-1). Daley emphasized that using the framework requires a collaborative effort and added that the framework is intentionally generic to enable health care facilities to use organization-specific data within the categories.
CASE STUDY: DECISION PROCESS TO INCORPORATE MORE REUSABLE ISOLATION GOWNS IN HEALTH CARE OPERATIONS
Elizabeth Schenk, executive director of environmental stewardship at Providence Health, and Jack Holmberg, senior infection preventionist at Providence Health, described a reusable isolation gown pilot program implemented at a Providence Health medical center. They outlined the impetus for the program, a literature review, the pre-implementation process, rollout of the program, evaluation, and next steps. Schenk noted that Providence Health is a health system comprising 51 hospitals and 1,000
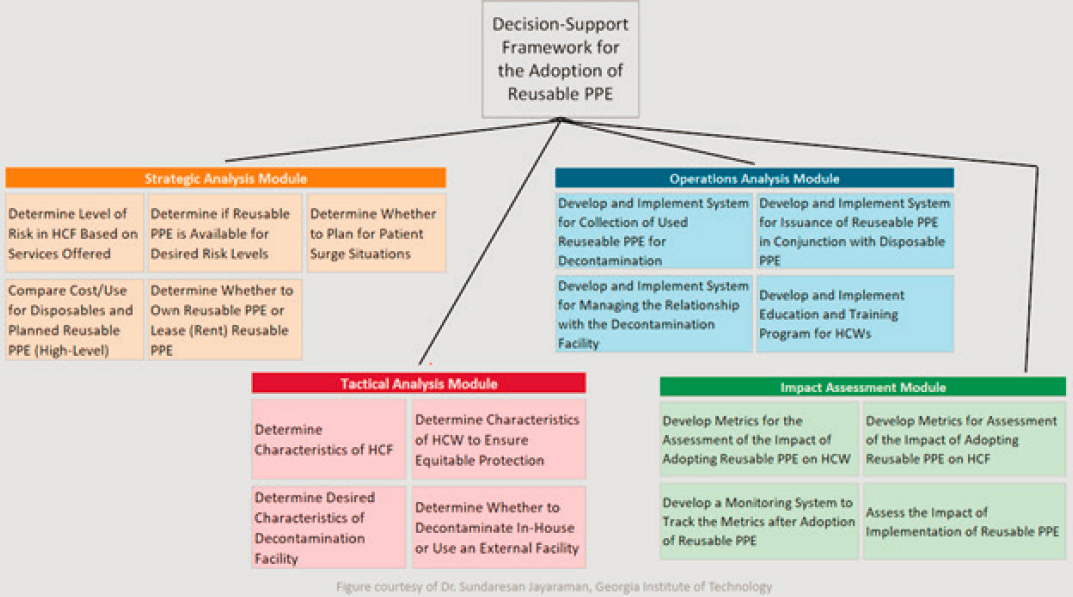
NOTES: HCF = health care facility; HCW = health care worker; PPE = personal protective equipment.
SOURCE: Presented by Jacqueline Daley on March 5, 2024, at the Reusable HCTs for PPE Workshop. Figure created by Sundaresan Jayaraman for the workshop (unpublished).
clinics across seven western U.S. states. In recent years, Providence Health has made a commitment to driving environmental stewardship via three pillars: mitigation, adaptation, and advocacy. The mitigation pillar focuses on addressing drivers of pollution and climate change via waste optimization, energy and water efficiency, sustainable agriculture, reducing use of harmful chemicals, and decreasing carbon emissions. Providence Health established a goal of diverting more than 50 percent of its waste from landfills and hazardous waste treatment by 2030. The health system categorizes waste as disposed, diverted, or avoided. Disposed waste is sent to landfills or sent for treatment as hazardous or biohazardous waste. Diverted waste is composted, recycled, or donated, processes that generate value from waste and lower carbon output. Avoided waste applies to products eliminated from use, such as disposable PPE that is replaced with reusable HCTs. Schenk explained that in working toward increasing the proportions of diverted and avoided waste, Providence Health tracks and measures system changes and associated reductions in disposed waste.
Holmberg outlined the multidisciplinary process of implementing a reusable gown pilot program at Providence Willamette Falls Medical Center (PWFMC). He described that in 2020, the medical center ordered 39,000 reusable gowns in response to PPE shortages caused by the COVID-19 pandemic. Reusable gowns offer independence from supply chain fluctuations in addition to advantages such as waste reduction, carbon reduction, cost savings, comfort and breathability, durability, and fluid resistance. However, once available, there was a return to disposable gown use across many departments. To achieve the Providence Health sustainability goal of diverting and/or avoiding over 50 percent of its waste by 2030, PWFMC explored these advantages as part of a strategic analysis process to determine whether to implement an ongoing reusable gown program, said Holmberg.
Decision-Support Analyses and Assessment
The first step of the strategic analysis was performance of a literature review, which yielded a study by McQuerry et al. (2021) indicating that reusable gowns offer increased protection, substantial cost savings, superior breathability, and sustainability in comparison to disposable gowns, Holmberg stated. Furthermore, PWFMC already had decontamination and laundering processes in place, a consideration relevant to the tactical analysis and operations analysis. Evaluation of initial concerns led to questions regarding gown fluid resistance and comfort, ability to effectively clean the gowns, risk of health care-associated infection (HAIs), and whether shifting to reusable gowns constituted a process change. Examination of the reusable gown life cycle generated additional logistical questions, such as how a reusable HCT program at their facility would handle
gown delivery, collection, transportation, and tracking. Holmberg and colleagues learned that PWFMC Environmental Services (EVS) staff are responsible for delivering and stocking linens; therefore, a reusable HCT program would not burden managers with the responsibility of ordering gowns. Used gowns could be placed with regular laundry after doffing, and EVS and nursing staff would handle collection. After collecting soiled gowns, EVS would transport them to PWFMC’s laundry co-op, where they would be washed at a minimum temperature of 160 degrees for 25 minutes to ensure effective cleaning. The specific reusable gowns used at PWFMC have a use life of 100 wash cycles and are tracked via scanning tags on the gowns. Holmberg added that the laundry co-op ensures gown integrity via inspections.
Pre-implementation and Implementation
Holmberg described the pre-implementation process, which involves conducting a risk assessment and providing executive leadership with the critical information in a format they are familiar with as a way to ensure that everyone is on the same page. Nursing and infection prevention professionals inspected the gowns and conducted a workflow walkthrough to provide feedback or concerns regarding donning and doffing procedures and the comfort and breathability of the gowns. Executive leadership then discussed and approved the reusable gown pilot program. This stage also involved initiation of ongoing evaluation of HAIs and numbers of isolation gowns used.
The pilot initially began in the intensive care unit (ICU) with 25 reusable gowns stocked daily by EVS. The donning and doffing procedures followed guidance from the Centers for Disease Control and Prevention, with the exception of adjusting the instruction to discard the removed gown into a waste container to placing it in a laundry bin (CDC, 2014). Given that the soiled reusable gowns are placed with the regular laundry, doffing procedures did not require a process change, although the units replaced open hampers with hampers with lids. He noted that PWFMC continued to make disposable gowns available for situations requiring transmission-based precautions (e.g., providing care to patients with fecal incontinence) as these patient interactions increase HCW risk of contact with infectious enteric agents and possible transmission (CDC, 2024; Louther, 1996). HCWs providing care to a patient with Clostridioides difficile (C. diff) or carbapenem-resistant Enterobacterales (CRE) and incontinence may feel more protected wearing a disposable gown, and PWFMC wants employees to feel safe while performing their duties.
Education about the program was communicated to HCWs via safety huddles, newsletters, email, and rounding. The 2022 rollout began in
the ICU before expanding to the medical/surgical unit, the emergency department, the labor and delivery unit, and ultimately to patient care areas within the entire medical center. Holmberg added that implementation in each unit was staggered by approximately a month to allow any issues or concerns to be addressed prior to further expansion.
Evaluation
After implementation, PWFMC conducted evaluation and impact assessment processes to identify any increases in HAI rates, calculate waste and cost reductions, and determine HCW satisfaction with the reusable gown program, said Holmberg. The HAI committee used 2021 HAI rates as a baseline for comparison with rates after the program was implemented in 2022. PWFMC had two cases of hospital-onset C. diff in 2021 and five cases in 2022, constituting a slight increase after the adoption of reusable gowns. However, the committee reviewed the 2022 cases and found some ordering inconsistencies. In 2023, PWFMC only identified one case of hospital-onset C. diff, and the committee concluded that the reusable gown program did not cause an increase of C. diff cases. In examining rates of catheter-associated urinary tract infections (CAUTIs), PWFMC had one case in 2021, two cases in 2022, and another two cases in 2023. Thus, the HAI committee did not identify a significant increase in CAUTI due to use of reusable gowns. Furthermore, Holmberg noted that an outbreak review found that no outbreaks involving respiratory or gastrointestinal pathogens such as COVID-19, influenza, or C. diff occurred in 2023.
Holmberg highlighted that an evaluation of overall waste reduction indicated a clear decrease from 2021 to 2023. In 2022, PWFMC laundry delivered 2,565 reusable gowns; this figure increased to 4,225 reusable gowns in 2023. Given that each gown can be laundered 100 times, fewer than 50 reusable gowns eliminated the need for 4,225 disposable gowns in one year. He outlined that PWFMC continues to use approximately 2,000 disposable gowns per week, resulting in consumption of 3,000 kilowatt hours of energy, 1,500 pounds of generated carbon dioxide emissions, 50 gallons of water, and 150 pounds of waste. Holmberg explained that in comparison with single-use isolation gowns, calculations indicate that use of reusable gowns decreases energy consumption by 30 percent, carbon dioxide emissions by 30 percent, water usage by 40 percent, and waste by 95 percent.
Potential Considerations and Next Steps
Holmberg acknowledged some disadvantages of reusable gowns. The gowns used at PWFMC, which are rated Level 2 by Association for
the Advancement of Medical Instrumentation (AAMI) standards, are not impervious to fluid barrier penetration. Therefore, PWFMC only uses the reusable isolation gowns as PPE for patient care and not for procedures. In contrast to some designs of disposable gowns that have tear-away closures for easy removal, reusable gowns do not break away, making the doffing procedure slightly more involved. He reiterated that disposable gowns may be preferred for contact enteric isolation or patients with fecal incontinence. After implementing the pilot program, a PWFMC policy update removed the wording “gowns are single use” to facilitate implementation of reusable gowns. An expanded literature review of recently published studies found support for reusable gowns and identified performance issues in disposable gowns (Davis and Haberland, 2023; Easter and Dabbain, 2023). Holmberg described the adoption of reusable gowns at PWFMC as a success, with next steps including potential regional expansion of the program and developing a standard operating procedure for reusable gowns at the regional and central division levels.
PANEL DISCUSSION
Health Care Systems’ and Organizations’ Perspectives
Skip Skivington, vice president of health care continuity and support services at Kaiser Permanente, provided the perspective from a large-scale health care system. He described the importance of PPE in protecting staff and patients during day-to-day operations and during surge events. He recalled that during the PPE supply shortage caused by the COVID-19 pandemic, standard procedures were not feasible, so the health center was forced to adapt practices based on available resources. His position entails planning for such surge scenarios. Barbara DeBaun, improvement advisor at Cynosure Health, offered a small-scale health care organization perspective. She began her career as an infection preventionist in 1978, before the HIV epidemic and COVID-19 pandemic. DeBaun remarked that over the decades, she has witnessed many HCWs compromise their safety by not wearing PPE appropriately when they perceive it to be uncomfortable or as impairing their ability to successfully complete a procedure. For example, HCWs sometimes snip the tips off their gloves if they are uncomfortable or seem to make it more difficult to start an intravenous (IV) line, and HCWs have poked holes in N95 respirators that feel too hot or cloying. She commented that safety expectations have changed since the 1970s, when HCWs wore short-sleeved gowns used by several HCWs over multiple days and hung on IV poles in between uses. Despite changes in safety protocols, PPE wearers may not comply with current PPE procedures if they are not involved in decision making and
do not understand the rationale behind procedures. Therefore, engaging users in PPE program planning is critical to the program’s success, said DeBaun. Emphasizing the value of including users in planning, Daley noted one of her mantras, “nothing about me without me.”
User Perspective
Katherine Townsend, professor at Nottingham Trent University, recalled working as a fashion designer and becoming aware of sustainability concerns and body issues related to mass fashion production, topics she explored in her practice-based doctoral thesis (Townsend, 2003). From 2015 to 2017, Townsend applied an approach she developed in her thesis to a project called Emotional Fit, a co-design engagement with a group of women who felt ignored by the fashion system. This project yielded a set of “emotionally durable” garment designs and a participatory methodology devised to explore and act on the physiological and psychological effects of clothing on the aging, changing, and active body. Such projects inform her current research on reusable PPE. During the COVID-19 pandemic, she learned of the lack of suitable isolation gowns and wrote a proposal entitled “Redesigning PPE: Enhancing the Comfort and Safety of Healthcare Workers Wearing Isolation Gowns to Treat Patients with COVID-19,” which was granted funding by the Arts and Humanities Research Council (2024). Working with a team from Nottingham Trent University and the University of Maribor in collaboration with Anze Ltd., a surgical apparel manufacturer, and Revolution-ZERO,1 a specialist in reusable HCTs who is developing modular decontamination hubs, Townsend researched and developed a reusable isolation gown system. Research methods included a review of procured gowns available to HCWs in local and national hospitals, interviews with clinical team leads, an illustrated online survey for HCWs, and wearer testing by nurses and surgeons in four National Health Service hospitals (Townsend et al., 2022). The research identified issues related to donning, doffing, poor fit, and thermal discomfort. Townsend and colleagues addressed these issues through reshaping, modifying fastenings and trims, and refabricating using a polyester carbon graft fabric with a high water-resistance level retained through a minimum of 100 wash cycles. She noted that UK legislation limits laundering of reusable PPE to 75 use cycles. Designed within a circular system that incorporates a take-back-and-repurpose scheme, the gowns will launch in 2024 (Townsend et al., 2023).
___________________
1 Information about Anze Ltd is available at https://anze.co.uk/ (accessed May 7, 2024). Information about Revolution-ZERO is available at https://www.revolution-zero.com/ (accessed April 10, 2024).
Considerations in Application of the Decision-Support Framework for Adoption of Reusable PPE
Daley asked whether the common elements of the decision-support framework for the adoption of reusable PPE—strategic analysis, tactical analysis, operations analysis, and impact assessment—are sufficiently flexible and adaptive to apply to a range of health care settings, such as hospitals, clinics, and outpatient settings. Skivington stated that these elements are foundational and must be considered in implementing a reusable PPE program. Beyond these elements, large health systems must also consider regulations as they apply both in normal conditions and in emergency situations. Although regulations are rigid in terms of not allowing deviations from safety practices, the HCW alterations to PPE highlighted by DeBaun do occur. He remarked that he understands the desire for comfortable, mobile PPE, but altering PPE poses a safety risk and fails to comply with regulations, which can carry repercussions for the workplace. Patients are a health system’s priority and when an HCW is not safe, neither is the patient, he emphasized. Given the ever-increasing costs of health care, health care systems work to limit costs to pass savings onto consumers. PPE is one of the drivers of health care costs, and while PPE is necessary, purchasing fewer options is beneficial from a cost perspective, said Skivington. Standardization is challenging and multiple factors may affect an HCW’s willingness to use a PPE item, including rational or irrational bias against wearing it. The modernization of PPE could aid a health care system’s ability to supply PPE that keeps HCWs and patients safe and that HCWs are willing to use. Numerous considerations should be factored into a decision to change a PPE program. Skivington remarked that although it is not feasible to please everyone all the time, a health system’s goal is to keep everyone as safe as possible.
DeBaun underscored myriad human factors involved in the success of a reusable PPE program, noting that one size does not fit all, and heavier duty barrier protection is more appropriate for certain procedures than others. She remarked that operating rooms are kept at cool temperatures—despite cold patients having worse outcomes—because of the amount of PPE HCWs need to safely perform surgery. Surgical procedures often require a high level of barrier protection, and the lack of breathability can make users uncomfortably warm. In turn, this discomfort can pose a safety risk and operating rooms are therefore kept cold, said DeBaun. Describing her 15 years of clinical experience working in small rural hospitals and critical access hospitals (i.e., hospitals licensed for 25 or fewer beds), DeBaun stated that many small health care centers lack the infrastructure and buying power of large health care systems. Consequently, the factors that health systems consider as they
make decisions about PPE can vary depending on the size of the organization. DeBaun commented that the elements of the framework apply to systems of various sizes, but the application will look different for small versus large health care systems.
Emotional Fit Considerations of PPE
During the height of the COVID-19 pandemic, some HCWs wore double or triple layers of PPE, Daley recalled, noting the emotional aspects of the crisis. She asked Townsend about the aspects of “emotional fit” that systems should consider in making decisions about the PPE they supply to employees. Townsend described how emotive issues initially drew her to the research area of PPE design. Like all humans, HCWs come in all shapes and sizes, yet health systems may only supply employees with single-use PPE in one size. She noted that this was particularly true during the COVID-19 pandemic, and it created challenges for petite and larger nurses. Given that most nurses are female, with as many as 80 percent of nurses in the United Kingdom being women, attention to sizing challenges is usually directed at females. However, when she conducted a pilot program at a local hospital, the most petite nurse on staff was male. Townsend used this example to underscore the importance of being inclusive and avoiding making assumptions regarding size. She emphasized that this situation called for a more customized approach, noting that the line of PPE she has co-designed comes in sizes ranging from extra small to 5-extra-large. Townsend acknowledged that stocking a large variety of sizes can be cost prohibitive for smaller organizations. However, organizations should consider ordering the sizes they need for their current employees and shift the sizes ordered as needs and personnel change.
Townsend commended the PWFMC pilot program on incorporating training and opportunities to engage HCWs in the process. Too often, the voices of the people who wear HCTs are not heard when selecting HCTs, she maintained. The PPE shortage during the COVID-19 pandemic sparked outcry, but the issues went deeper than quantity, as many garments were not fit for purposes of the people who needed to wear them. Townsend echoed DeBaun’s comments about how thermal comfort may impact an HCW’s performance, noting that the stress of wearing PPE that does not appropriately offer coverage and mobility could likewise affect job performance.
Skivington highlighted the need to consider the specific employee population when supplying PPE. To illustrate, he described how an H1N1 surge caused a shortage of N95 respirators. California supplied N95 respirators from a state stockpile, but the majority of the fit tests failed. Criticism was directed at Kaiser Permanente for not properly training staff on how
to fit test, but this was unfounded, because fit testing is a daily process. An investigation revealed that the state had stockpiled N95 respirators designed for the construction industry, but the construction version is different from medical N95 respirators and was unfamiliar to HCWs.
HCW Engagement to Increase Adoption of Reusable Medical Gowns
Daley asked Schenk and Holmberg how they generated support to move the reusable gown pilot program forward. Holmberg highlighted the value of literature supporting the use of reusable HCTs. Additionally, a reusable gown program had previously been implemented in another Providence Health facility, providing traction for the PWFMC initiative. Efforts to engage HCWs before the rollout of the pilot program—such as conversations with nurse managers, bringing gowns to units for HCWs to try on, and soliciting feedback—seemed to lower resistance to the program. The HCW concerns included whether doffing gowns would require a new doffing location, the lack of a breakaway closure, and the gowns being harder to tie than disposable versions. As questions and concerns arose, Holmberg and his colleagues problem solved the challenges; this responsiveness to feedback generated clinical buy-in, which in turn strengthened the case made to leadership. Moreover, the pilot program began on a small scale, within a six-bed ICU unit, and the program solicited and responded to feedback before expanding to other units. This incremental approach allowed corrections and adjustments to be made in real time. Holmberg acknowledged that the slow rollout resulted in only 2,500 reusable gown uses in 6 months, slightly more than the 2,000 disposable gowns PWFMC uses per week, but he expressed optimism that building a foundation of support will benefit the program as it continues to expand.
Schenk highlighted an unpublished study conducted by Providence Health in November 2023, in which investigators surveyed 1,100 health professionals across all disciplines in the health care system using the Climate, Health, and Nursing Tool (CHANT), a tool to assess awareness, motivation, and behaviors related to climate change and health. The CHANT survey indicated substantial awareness about climate and health among HCWs at Providence Health; this awareness was coupled with concern and motivation to act, but few respondents were aware of the environmental stewardship initiative. Schenk attributed this to the difficulty in reaching all bedside HCWs in a large, complex health system, given how busy nurses are and the variance in their communication styles. She described the reusable gown program as aligning the commitment to prioritize patient safety with a growing commitment to the safety of the planet.
DeBaun stated her appreciation of the pilot program’s incremental change approach that incorporates feedback from frontline staff. She recalled working during an Ebola epidemic and discovering that HCWs maintained the integrity of donning procedures, but doffing practices created opportunities for exposure to the deadly virus. She remarked that having people try on the gowns, practice tying and untying them, and providing feedback before they are asked to use them on the job could decrease the issues she saw with Ebola. Noting that she lives in San Francisco, where awareness of recycling and environmental practices is higher than in some parts of the country, DeBaun emphasized the diversity of levels of environmental awareness, which can present additional challenges to sustainability efforts. She stated that aligning safety of the patient, HCW, and the planet is a tremendous challenge facing health care.
Skivington remarked that Kaiser Permanente is a heavily unionized organization, and engaging labor during planning stages helps to accelerate change within their system. Developing union buy-in early on reinforces a commitment to frontline workers, thereby lowering potential for resistance. Townsend echoed the importance of engaging HCWs in handling and wearing reusable gowns ahead of implementation of a reusable HCT program. Involving management can facilitate this process, given how busy nurses are during shifts. She described difficulty in scheduling gown testing with two university hospitals in Nottingham and accruing feedback with two local hospitals in the East Midlands, which led to testing much farther away in South West England. Townsend remarked that although this travel was challenging, her team made the trip because of the value of expert feedback provided by nurses wearing the gowns. This expert feedback is integral to modifying the design of a product to work as well as possible for the end users, she added.
HCW Confidence and Compliance with PPE
The COVID-19 pandemic affected the spectrum of health care, including hospitals, acute care, teaching hospitals, critical access hospitals, and long-term care, said Daley. Given the various scenarios that may present in different settings, she asked about methods of ensuring HCW safety and reassuring staff that the supplied PPE is appropriate. Daley added that risk anticipation may be relevant, noting that anecdotal reports such as an HCW getting splashed in the eye during a procedure raises questions as to competency in anticipating risks. Holmberg suggested that the first step is to establish understanding of the rating of specific PPE and what that rating signifies. For example, the reusable gowns used at PWFMC have an AAMI Level 2 rating, which is equivalent to that of disposable gowns typically used at the health care center. Levels 3 and 4
gowns offer substantially more fluid resistance, but they are less breathable. The pilot program only implemented reusable gowns in areas where Level 2 gowns are appropriate for anticipated risk, thereby relieving HCWs of assessing risk in relation to reusable gown use. Given that direct patient care constitutes most of the gown usage, implementing reusable gowns for patient care offers balance to the continued use of disposable gowns for surgery and procedures at PWFMC. Holmberg noted that the hospital makes disposable gowns available on all units so that HCWs feel comfortable performing their duties, should they feel that a single-use gown is more appropriate for a given situation. Holmberg remarked that an education deficit leads to poor risk assessment; he highlighted the value of ongoing education and training in fostering staff accuracy in assessing risk. Townsend echoed that disposable PPE is appropriate in some situations and she advised taking an open, measured approach to increasing the use of reusable HCTs.
DeBaun described how long-term care settings operate under different recommendations than other health care settings. For instance, these recommendations advise HCWs to use enhanced barrier precautions for any high-contact duties, such as assisting a resident with bathing or toileting or providing care to a patient with a urinary catheter. She remarked that the recommendations specifically for long-term-care settings are contributing to an increase in the number of gowns used. Skivington commented that Kaiser Permanente has infection control committees that are rigorous in examining the risks involved in day-to-day hospital activities. The health system also has a national sourcing standards team that meets with the infection control committees monthly to discuss PPE product selection and to ensure that any updates or changes in standards are implemented. Each time a high-risk patient receives hospital care, Kaiser Permanente provides a detailed list of recommendations for the safe handling of the patient. He spotlighted high rates of compliance among HCWs, noting that ongoing education and reinforcement fosters compliance, especially when it includes explanations of why specific safety precautions are warranted. Skivington emphasized that the use of technology and design to improve the comfort of PPE would benefit HCWs and further increase compliance.
Schenk commented that HCW resistance to reprocessed equipment sometimes appears. She discussed a quality improvement project conducted at Providence hospitals to understand surgeon and perioperative staff resistance and barriers to using reprocessed materials and supplies, which revealed that providing HCWs with more knowledge and explanation reduced anxiety and addressed many of the participants’ concerns. Educational efforts require data on outcomes, cost, and environmental effects such as carbon emissions. She remarked that HCWs may be less
concerned about the hospital saving money than they are about decreasing pollution. Therefore, metrics related to environmental effects should be incorporated into staff training and education.
Misperceptions Regarding Reusable and Disposable PPE
Daley commented on a common assumption that plastic is always more protective than cloth. Given that disposable and reusable gowns are rated with the same standards, she asked how this assumption can be changed. Skivington stated that people often have the perception that if a product comes straight from a package and has never been used, it is cleaner than a product that has been used and processed. Disposable products have attained a confidence level that reusable products have not. DeBaun remarked that many people believe that plastic provides better barrier protection than other materials regardless of whether evidence supports this belief. She added that some single-use gowns offer little barrier resistance, noting that such products were used during the COVID-19 pandemic when PPE shortages forced health care facilities to supply HCWs with any available PPE. The assumption that plastic is always protective is a dangerous misconception that needs to be dispelled, said DeBaun. Daley added that she received unfamiliar PPE during the COVID-19 pandemic, including a disposable gown with ties that attached in the center of the abdomen. She underscored that standards testing for barrier classification for isolation gowns does not extend to cuffs, hems, or bindings (e.g., ties), noting that the integrity of the garment could be compromised based on how these items are attached to the gown (e.g., stitched). This is particularly important when these are attached to areas where pressure commonly occurs, possibly leading to fluid penetration to the wearer’s clothing and/or skin.
Holmberg commented that doctors and nurses respond to data. Recent studies indicate that the tensile strength and fluid resistance of disposable gowns are not as high as commonly presumed; they also indicate that reusable gowns do offer protection and safety. Sharing data with HCWs can increase confidence and acceptance of reusable HCTs. He remarked that as an infection preventionist, he understands that there is a stigma against reusable products and that shifting an entrenched assumption can be difficult. He approaches this assumption by drawing a comparison between reusable gowns and surgical instruments, which are reprocessed between uses. DeBaun emphasized the value of the PWFMC program evaluation infection reviews. She noted that data measuring the effects of a change can be profoundly influential, particularly in a data-driven field such as health care. Schenk added that many HCWs are concerned about the amount of plastic waste generated by the health care
industry and its contribution to microplastics pollution. Advancing the technology of PPE offers solutions for both safety needs and the issue of microplastics, she stated. Townsend remarked that education is needed to shift the perception that newness equates to protection. She underscored the importance of developing mechanisms to recycle and repurpose reusable gowns to divert them from landfills at the end of the life use cycle. Extending the utility of gowns into the post-use phase is the key method of reducing harm to the environment and fostering a “circular system,” said Townsend.
PPE Demand Surge Considerations
Given that health care centers experience surges from causes ranging from infectious diseases to natural disasters to trauma from multivehicle crashes, Daley asked how to address surges in demand for PPE, noting that the PPE supply shortages early in the COVID-19 pandemic indicated a lack of pandemic preparedness. DeBaun replied that the COVID-19 pandemic supply shortages demonstrated that inadequate preparedness efforts provided a false sense of security. For instance, PPE supply stockpiles were not always kept up to date and, when the crisis hit, some stores of supplies had degraded and were no longer effective. The field of health care is much better at responding during a crisis than continually maintaining a state of preparedness, she maintained. Skivington added that when the COVID-19 pandemic disrupted supply chains, U.S. reliance on imported PPE contributed to supply shortages. He referenced a recent article highlighting that the investment made in domestic PPE production in response to the pandemic has evaporated and hospitals are once again purchasing PPE from foreign suppliers (Tita, 2024). Now that PPE is in ready supply and health care systems have established buffer stock, hospitals have returned to offshore purchasing. Skivington predicted that this dynamic will result in PPE shortages the next time a surge shifts the supply-and-demand curve. Daley commented on the importance of inventory management that involves a “first in, first out” cycle where the stockpile is continually used and replenished.













