Rethinking Race and Ethnicity in Biomedical Research (2025)
Chapter: 5 Reconceptualizing the Use of Race and Ethnicity in Biomedical Research
5
Reconceptualizing the Use of Race and Ethnicity in Biomedical Research
This chapter provides conceptual underpinnings for the committee’s recommendations provided in Chapter 6. The status quo approach to using race and ethnicity in biomedical research has generally relied on the U.S. Office of Management and Budget (OMB) race and ethnicity categories. This chapter opens with a summary of some of the limitations of using the OMB categories in biomedical research studies. The following section brings together several concepts introduced in previous report chapters in a discussion of the committee’s path forward. Importantly, there are alternatives to using the OMB categories throughout the development and execution of biomedical research studies, and one way to improve and reconceptualize the use of race and ethnicity is to think critically about which concepts and measures are most relevant to a given research context. The majority of the chapter introduces strategies for replacing the use of race and ethnicity with other more meaningful concepts and measurements of social and biologic factors that affect people’s health.
CURRENT USE OF THE OMB RACE AND ETHNICITY CATEGORIES IN BIOMEDICAL RESEARCH
Biomedical researchers in the United States who incorporate race and ethnicity information frequently collect, analyze, and report those data based on classification schemes set out in the OMB Statistical Policy Directive No. 15 (OMB, 1997, 2024). The OMB categories are used across federal government agencies and, having become ubiquitous, are also used by many nongovernmental institutions, such as health care systems (see Chapter 2 for background on the origin and evolution of the OMB categories). Though the OMB has stated that these categories are not anthropologically or scientifically based designations, in practice they are sometimes used in those ways, which can perpetuate misconceptions about race and ethnicity.
Misconceptions About the Use of the OMB Categories in Research
In an effort to ensure that diverse groups of people are recruited for research, funders such as the National Institutes of Health (NIH) often require the use of the OMB categories for reporting recruitment statistics.1 It is worth repeating that although Directive 15 specifies that the categories should not be considered as scientific, biological, or anthropological in nature, their use in research contributes to their conflation with biological meaning and importance. More generally, the way in which people encounter the OMB categories in research and medicine lends them a perceived but misplaced importance (Epstein, 2008).
Misconceptions about the OMB categories continue to permeate scientific research and affect health outcomes. Directive 15 notes, “The categories represent a social–political construct designed for collecting data on the race and ethnicity of broad population groups in this country, and are not anthropologically or scientifically based” (OMB, 1997). “The racial and ethnic categories set forth in the standards should not be interpreted as being primarily biological or genetic in reference” (OMB, 1997). The NIH policy on reporting race and ethnicity data for participants in clinical research repeats these disclaimers about its more detailed definitions (NIH, 2001). These key distinctions for the use of the OMB categories were also noted in a 2023 report on population descriptors from the National Academies of Sciences, Engineering, and Medicine (the National Academies) (NASEM, 2023).
Researchers have long been able to collect information on additional categories, but more granular data are often not collected or are “rolled up” into the standard minimum OMB categories for reporting purposes. Directive 15 has always indicated that additional data may be collected. In 1977, the OMB stated, “In no case should the provisions of this Directive be construed to limit the collection of data to the categories described above” (OMB, 1977). This was reiterated in with the 1997 revisions. “This classification provides a minimum standard for maintaining, collecting, and presenting data on race and ethnicity for all Federal reporting purposes” (emphasis added) (OMB, 1997). Even though the OMB categories are a minimum set of categories and some agencies encourage collecting more granular data, the previous lack of a requirement to collect more detailed information implied that the standard OMB categories were sufficient. The 2024 standards now require agencies to collect more granular subcategories, though it remains to be seen how this standard will be implemented in biomedical research and what its effects may be. Furthermore, in practice, granular data must collapse or “roll-up” to the standard OMB categories. The Department of Health and Human Services (HHS), for example, collects the categories Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, and Other Asian, all of which roll up to the Asian OMB standard category (OMB, 2024).
As introduced in Chapter 2, the OMB revised Directive 15 in 2024. Among updates to terminology and other revisions, the OMB added the category Middle Eastern or North African, defined as “[i]ndividuals with origins in any of the original peoples of the Middle East or North Africa, including, for example, Lebanese, Iranian, Egyptian,
___________________
1 For example, see NOT-OD-01-053 and related policies for including women and members of racial and ethnic minority groups as participants in research: https://grants.nih.gov/policy/inclusion/women-and-minorities.htm (accessed October 15, 2024).
Syrian, Iraqi, and Israeli” (OMB, 2024, p. 22191). As such, Middle Eastern or North African is defined with a combination of geography and national origin, reflecting an overall trend in the policy to predominantly define categories based on national origin (see Box 2-3). National origin is only one aspect of racial and ethnic identity, as will be further explored in this chapter. The full effects of implementing this system of categories remain to be seen for biomedical research but will depend on how the policy is operationalized for health research by government agencies such as HHS and NIH. Federal agencies, including NIH, are required to submit an Action Plan on Race and Ethnicity Data to the OMB by September 28, 2025; these action plans will be made publicly available (OMB, 2024).
There is a prevailing misconception that reporting recruitment statistics according to the OMB categories means that the corresponding scientific analysis must be done with the same categories. Although funding organizations may require the use of the OMB categories for reporting purposes, additional categories or variables may be used in study design and analysis (NASEM, 2023). In their 2023 report, the National Academies Committee on the Use of Race, Ethnicity, and Ancestry as Population Descriptors in Genomics Research cautioned
against the use of typological categories, such as the racial and ethnic categories established by the U.S. Office of Management and Budget in Statistical Directive 15, for most purposes in human genomics research. While the use of these categories may be required of researchers under certain circumstances (for example, in describing participants in studies receiving federal funding), the fundamentally sociopolitical origins of these categories make them a poor fit for capturing human biological diversity and as analytical tools in human genomics research. Furthermore, use of these categories reinforces misconceptions about differences caused by social inequities. (NASEM, 2023, p. 104)
The continued use of the OMB categories in research contexts carries the risk of perpetuating these misunderstandings.
MOVING TOWARD RACISM-CONSCIOUS RESEARCH
An overemphasis on the OMB categories in research has been at the expense of rigorous investigation of other concepts related to race. Because it is frequently used as a proxy for other factors of interest, race often serves to collapse a wealth of information about individuals, communities, and health. While acknowledging how past harms and flawed research have affected the past and current evidence base in biomedical research, the committee’s path forward is grounded in a recognition of the multiple dimensions—social, biological, environmental, behavioral—that affect people and their health, including racism (see definitions in Box 2-2).
For much of the past, race-based approaches in science and medicine essentialized race, reinforcing the belief that there are innate, race-based biological differences between groups of people. Numerous historical examples of race-based medicine continue today and contribute to harms and inequitable care (Vyas et al., 2020; Yearby, 2020a). Some of these are examined in Chapter 3. For example, current practices of race adjustment in pulmonary function testing are tied to the erroneous belief that Black
people have weaker lungs than White people, which served as a justification for slavery (Braun, 2014; Scanlon and Shriver, 2010). These race-based adjustments prevent Black people from receiving equal access to care.
Recognition of the harms of race-based medicine have led some to call for a “race-neutral” approach—that is, taking race out of clinical care entirely. Race neutral, also known as “colorblind,” policies or approaches disregard the role of structural discrimination, fail to account for differential effects on people and groups, and can worsen health inequities (Delaney et al., 2021; Okah et al., 2022; see also Bliss, 2012; Brown et al., 2023; Hatch et al., 2016). In response to arguments for race-neutral approaches, others have suggested that race should continue to be used to track the impacts of racism on members of racial and ethnic minority populations (Geronimus, 1992; Krieger, 1999; Kuehn, 2024). As discussed throughout Chapters 3 and 4, there is no simple solution, as removing race without evaluating potential consequences can result in ignoring important social factors that influence health or even exacerbate disparities (Tipton et al., 2023).
Race-conscious medicine is an attempt to address this complexity. Race-conscious medicine emerged from a recognition of the historical role of race in perpetuating racism in science and medicine (Cerdeña et al., 2020; Hernandez-Boussard et al., 2023; Wright et al., 2022). Cerdeña and coauthors frame race-conscious medicine around race as a social and power construct that can be used to measure racism, rather than race, as the exposure leading to poor health outcomes (Cerdeña et al., 2020). Even so, the term race-conscious medicine can be misconstrued by seeming to emphasize race as an individual attribute of a patient. For instance, in clinical care, race-conscious medicine can be understood to mean having an awareness of race in order to narrow down likely risks of disease. Awareness of a patient’s race is a criterion or heuristic that physicians have long been trained to use to assess disease probabilities. However, the attendant risk of race-conscious medicine is that relying too much on race in the care of patients can be misguided, reinforce racialized stereotypes, and continue to reify race as a biological variable (Braun et al., 2007; Fashaw-Walters, 2023; Khazanchi et al., 2023; Moscou and Baker, 2018; Olufadeji et al., 2021). Recognizing the practical concerns in clinical care, race-conscious medicine may continue to have a limited role as better tools are developed to identify and interrogate disease risk more directly and accurately.
Race consciousness acknowledges that race can play a role in health, not due to inherent biological differences between racial groups, but rather due to social determinants of health (SDOH). While this is an important distinction, it does not engage with underlying drivers of structural inequities. Therefore, an alternative to race-consciousness is needed. Since much of the existing evidence base for race-based approaches is tied to the discriminatory belief that members of minoritized racial and ethnic groups are inferior to White people, perpetuating racism, the committee suggests the phrase racism-conscious medicine and research. A racism-conscious approach means acknowledging discriminatory historical and modern practices that have led to flawed research and clinical standards, making it challenging or impossible to disentangle from the current evidence base (see Box 5-1). As introduced in Chapter 2, racism occurs at multiple levels—not only in interpersonal acts of discrimination or prejudice but also in macrolevel systems and social structures. Biomedical research needs to be conducted
BOX 5-1
Defining Race-Based, Race-Neutral, Race-Conscious, and Racism-Conscious Approaches to Biomedical Research
These various approaches differ in how they handle the concept of race, ranging from explicitly incorporating it, to ignoring it, to acknowledging it in a nuanced manner that addresses broader social and structural determinants of health.
Existing Approaches
Race-based biomedical research explicitly incorporates race as a factor and is rooted in a mistaken presumption of biological differences across racial or ethnic groups. This approach essentializes race, reinforces racial stereotypes, and fails to integrate the numerous social and environmental factors that contribute to health outcomes.
Race-neutral biomedical research omits race as a factor, emphasizing that race is a social construct with no biological basis. Although the intention may be to avoid potential biases or oversimplifications by eliminating race as a factor, this approach risks overlooking or underestimating how societal factors related to race, such as racism, affect health outcomes.
Race-conscious biomedical research acknowledges that race can affect health outcomes, not because of inherent biological differences, but due to social, economic, and cultural factors. This approach involves designing studies, policies, or interventions that consider these broader SDOH, without reducing research participants to their racial identities; however, the term risks reifying race and being misconstrued as race-based in practice.
Committee’s Suggested Approach
Racism-conscious biomedical research emphasizes how various forms of racism have contributed to health disparities and the need to address structural drivers of inequity directly to achieve equitable health outcomes.
with an awareness of the broader social system and structural inequities. Because science is systematic, there is an assumption that it is also neutral and bias free. However, this belief has allowed the scientific community to ignore racially discriminatory practices entrenched within it and the ways in which science has reinforced racism within society, including via invalid ascriptions of race made over time in scientific research. A fundamental shift in thinking is necessary to grapple with the mechanisms and social forces that affect health—giving rise to the committee’s approach of racism-conscious research.
Racism-consciousness provides the first step in preventing the continued misuse of race—namely, acknowledgement and understanding of how discriminatory societal practices have influenced biomedical research—and allows researchers the opportunity to begin to rectify the harm caused by these practices. Pulse oximetry, as discussed in Chapter 3, offers an illustrative example. Failing to attend to how medical devices operated across different skin tones resulted in inaccurate measurements for many patients with darker skin. A University of Michigan study demonstrated that Black patients had nearly three times the frequency of occult hypoxemia undetected by pulse oximetry as did White patients (Sjoding et al., 2020). This has spurred racism-conscious research to identify technologies to more accurately measure hypoxemia that are not affected by or can adjust to skin color. Upholding the principle of equity requires correcting structural unfairness in social systems and distribution of benefits and burdens (see Chapter 2, section “Guiding Principles”). Research that redresses health inequity requires an awareness and understanding of the systems and structures that create and perpetuate inequity.
As the research community moves toward an ideal of greater shared decision making in science and medicine, it will be critical to bring racial and ethnic minority communities and participants harmed by these practices into research decision making (Fashaw-Walters, 2023). This will mean fully contextualizing an individual, moving beyond race-consciousness to context- and person-consciousness in order to begin rectifying the historical and modern-day harms to build toward a better future.
Realizing this vision for the future of biomedical research will require articulating and measuring the other concepts and factors for which race is often a proxy (Box 5-2). These factors can all play a role in health. The following sections detail some of
BOX 5-2
Race, Ethnicity, and Related Concepts
Race and ethnicity categories are often used as proxies for the true concepts or variables of interest. In addition to self-identified race and ethnicity, related concepts include:
- Relational aspects of race
- Structural racism
- Social determinants of health (e.g., environment)
- Ethnic and cultural practices (e.g., language, religion)
- Immigration status and degree of acculturation
- Indigeneity
- Skin color and pigmentation
- Known ancestry
- Genetic markers; genetic variation
- Social and stress-related biomarkers
- Other biomarkers and biological indicators
these concepts and provide tools for considering them in research contexts. Building from the committee’s conceptualization of racism-conscious medicine, the next sections continue with structural racism and SDOH. The chapter proceeds with ethnicity and indigeneity, which are closely entwined with race. Next the chapter distinguishes skin color from race and discusses the multidimensionality of race. One dimension of race is ancestry, so the chapter continues with a discussion of ancestry and multiracial and multiethnic identity. The chapter concludes with a discussion of the relationship between race, ethnicity, and biomarkers.
STRUCTURAL RACISM
Researchers using race may be using the construct as a proxy for social exposures that affect health, such as structural racism. In 2010, the federal government recognized that structural discrimination is one of the root causes of health disparities (Yearby, 2020a). Structural discrimination—meaning macro level conditions such as residential segregation—limits the conditions and well-being of less privileged groups (including racial and ethnic minority groups, women, LGBTQIA+ individuals, older people, people with disabilities, people who have low incomes), which keeps these groups from reaching their full health potential (Williams and Mohammed, 2009; Yearby, 2020a). Policies and law (that is, the political process, standards, regulations, and guidance) are tools used to perpetuate structural discrimination by structuring systems in a discriminatory way, which has been associated with health disparities (Dawes, 2020; NASEM, 2024; Yearby, 2020a, 2020b). Figure 5-1 highlights how structural discrimination, such as racism, is associated with health disparities.
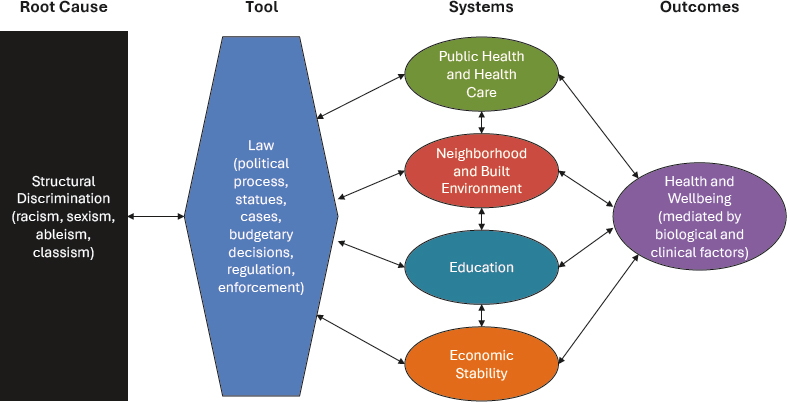
SOURCE: Adapted with permission from Yearby (2020b). Structural racism and health disparities: Reconfiguring the social determinants of health framework to include the root cause. Journal of Law, Medicine & Ethics 48(3):518–526. © Cambridge University Press, reproduced with permission.
Structural racism is one form of structural discrimination. Structural racism has been defined as “the macrolevel systems, social forces, institutions, ideologies, and processes that interact with one another to generate and reinforce inequities among racial and ethnic groups. The term structural racism emphasizes the most influential socioecological levels at which racism may affect racial and ethnic health inequities. Structural mechanisms do not require the actions or intent of individuals” (Gee and Ford, 2011, p. 3). Structural racism also includes discrimination based on color and national origin.
In recent years, there has been an exponential increase in the term structural racism in health-related publications (Dean and Thorpe, 2022), partially due to growing interest in structural racism as a mechanism and driver of population health (Bailey et al., 2017). As much as structural racism can be challenging to define (Bailey et al., 2017; Dean and Thorpe, 2022), the concept has been difficult to measure, with the literature featuring a wide variety of approaches (Dean and Thorpe, 2022; Hardeman et al., 2022). With the variety of ways that structural racism can operate, there is no single optimal way to measure it (Jahn, 2022), but given the multidimensional and interactive qualities of structural racism, index measures consisting of multiple indicators may be best suited to capturing key nuances (Dean and Thorpe, 2022). Box 5-3 describes some possible strategies for measuring structural racism for epidemiological and biomedical research applications.
Given evidence for racism as a driver of health disparities (see Chapter 3), biomedical research could benefit from directly interrogating the role of structural
BOX 5-3
Possible Ways to Measure Structural Racism
- Index measures that aggregate multiple indicator variables (Adkins-Jackson et al., 2022; Jahn, 2022; Urban Institute, 2023)
- Latent construct approach or latent variable modeling (Adkins-Jackson et al., 2022; Brown and Homan, 2024; Jahn et al., 2023; Urban Institute, 2023)
- Psychometric evaluation to test measures for relevance over historical eras and life-course time (Adkins-Jackson et al., 2022; Szanton et al., 2022; Thorpe et al., 2019; Urban Institute, 2023)
- Consider
- The level(s) at which racism is operating and how to be precise in measurement.
- Developing measures with indicators that are specially targeted to how structural racism presents itself in specific contexts.
- Developing structural racism measures for use at different levels of geography of exposure or unit of intervention.
See also Table 1 in Dean and Thorpe (2022).
racism. Structural factors include policies and practices from institutions, organizations, and systems and are distinct from interpersonal racism and implicit bias, which have typically garnered more attention (Carter et al., 2022; Gee and Ford, 2011; Weinreb, 2023). Increasing awareness of structural racism and how it works can lead to studying its effects in new ways in biomedical research. Pathways linking racism to health outcomes are complex and merit further investigation of how structural factors drive persistent health disparities. Not only is structural racism itself linked to poor health outcomes, but it also influences social factors, such as the SDOH, which are associated with individuals’ health and well-being. As one example of this type of approach, Carlos et al. (2022) proposed social genomics as one potential pathway linking structural racism and discrimination and breast cancer outcomes.
SOCIAL DETERMINANTS OF HEALTH
Closely related to structural discrimination are SDOH. In 1906, W.E.B. DuBois noted that social conditions, not biology, affected the health of Black Americans, causing racial inequities in mortality rates (DuBois, 2003; see also White, 2011). Almost 100 years later, the Institute of Medicine issued the landmark report Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare which highlighted the impact of racial discrimination on social conditions, such as mortgage lending, access to housing, employment, and criminal justice, which were associated with racial health disparities (IOM, 2003; NASEM, 2024; Yearby, 2020b). This report along with a 2008 report from the World Health Organization were instrumental for the development of the social determinants of health framework in the United States (WHO, 2008; Yearby, 2020b). In 2024, the National Academies revisited Unequal Treatment by publishing a new report, Ending Unequal Treatment: Strategies to Achieve Equitable Health Care and Optimal Health for All. The new report found that while some progress has been made between 2003 and 2024 to raise awareness, conduct research, and form policies to address inequities, health care inequities had only slightly narrowed, a trend that has been inconsistent (NASEM, 2024).
SDOH are part of the U.S. HHS Healthy People 2030 Initiative to improve the health and well-being of individuals in the United Sates (HHS, 2021). SDOH include five key social factors: economic stability, education, social and community context, health and health care, and neighborhood and built environment (HHS and OASH, 2024). SDOH were added to the Healthy People Initiative as a means to identify and eliminate the causes of health disparities (HHS and OASH, 2024).
In 2011, Braveman et al. argued that health disparities “are a specific subset of health differences of particular relevance to social justice because they may arise from intentional or unintentional discrimination or marginalization and, in any case, are likely to reinforce social disadvantage and vulnerability” (Braveman et al., 2011, p. S150). The 2030 Healthy People Initiative seemingly adopted this approach, when it noted that SDOH were central to achieving health equity, in which “everyone has the opportunity to attain full health potential and no one is disadvantaged from achieving this potential because of social position or any other socially defined circumstance” (CDC, 2024;
see also Braveman, 2023; HHS and OASH, 2024). The Healthy People Initiative sets national goals, while SDOH provide measurable objectives that the federal and state governments use in their work with communities to achieve health equity (HHS and OASH, 2024).
Identifying social and community context as a component of the SDOH indicates that discrimination—such as institutional, interpersonal, and intrapersonal racism—causes challenges and harm to individuals that negatively affect their health. For example, American Indians and Alaska Natives (AIANs) experience profound disparities in SDOH, with the highest poverty rates of all racial and ethnic groups in the United States (26.2 percent in 2016) and high rates of homelessness (Solomon et al., 2022). Data also show that 21 percent of Black individuals work in jobs with high risk for injury or illness compared with only 13 percent of White people (Yearby, 2020b). In biomedical research, the SDOH framework could be useful for identifying social factors relevant to a given line of inquiry. Compared with how race has often been collected as a single variable in research, SDOH are multiplex, and studying them can be challenging because scientists will need to consider a variety of potentially relevant factors. More exploration is needed to further develop the evidence base for biomedical researchers to rely on in this domain.
ETHNICITY
The SDOH that correlate with health disparities affect populations in the United States based to a great degree on their perceived race, ethnicity, and indigeneity. There has been far more research on the connections between race, SDOH, and health disparities than there has been with groups identified ethnically (Ford and Harawa, 2010).
In the United States, the concepts of race and ethnicity are difficult to disentangle. They are often treated as synonyms, as is evidenced by the increasing use of the term ethnicity to replace the term race in Medline-indexed studies (Afshari and Bhopal, 2010) and by the tendency of some Hispanic or Latinx people to use these terms to describe their race (Noe-Bustamante, 2021). By combining the race and ethnicity questions into one, recent changes to the OMB Directive 15 standards now enable respondents to choose solely Hispanic/Latino, without requiring selection of a separate race category. Despite the emphasis on Hispanic/Latino ethnicity in the United States system, there are other ethnic populations in the United States (e.g., Hmong, Armenian). Of course, one limitation is that data about other ethnic groups and communities in the United States have not been as consistently or systematically collected.
For purposes of this report, the committee has defined ethnicity as a socially and politically constructed term used to describe people from a similar national or regional background who share common national, cultural, historical, and social experiences. An ethnic group is often defined based on shared values, behaviors, heritage, or language. Ethnicity also varies across historical, political, and geographic contexts. Ford and Harawa (2010) define ethnicity as “a context-specific, multilevel (i.e., group-level, individual-level), multifactorial social construct that is tied to race and used both to
distinguish diverse populations and to establish personal or group identity.” It is apparent in both definitions that ethnicity encompasses multiple factors that vary over time and place. Its use in the United States often involves the social or political grouping of individuals, either self-identified or assigned by society, based on shared culture, language, religion, ancestry, and diet.
Based on these definitions, it is evident that using ethnicity in biomedical research is challenging. Compounding the challenge, a person’s ethnic identity evolves over the life course. A person’s ethnic identity also varies depending on the context. For example, Ford and Hawara noted (2002), “One may identify as Hispanic at work, Latino within his civic organizations, Mexican at home, and American when visiting Mexico” (p. 6; see also Harris and Sim, 2002). The fluidity and nuance of someone’s ethnicity belies the OMB’s long-running binary classification system consisting of Hispanic/Latino or Not Hispanic/Latino.2 Self-identification among ethnic groups, moreover, may exhibit generational changes over time. Remarks shared with the committee illustrate this evolution of identity and how this information can be collected for research: “Because myself, as Dominican, . . . I’ve learned about the generational differences between my mom, calls herself Hispana, because that’s what she was when she first came to the United States as she checked off a box. Then I learned to say I’m Latina, I’m not really Hispanic. And then my kids are Latinx, but you would not know that unless you first asked open-ended questions” (Danurys “Didi” Sanchez in remarks to the committee on March 14, 2024).
One of the main reasons for incorporating ethnic identification in biomedical research is the substantial public health, policy, and population health research indicating that certain ethnic groups in the United States exhibit disparate health outcomes. These disparities stem from various factors, including discrimination in health care, unequal access to resources, and the stress-related impacts of discrimination. These stressors often arise from unequal access to protective SDOH in the United States. For example, data show that 33 percent of Hispanic children in the United States reside in households below the poverty line (Wight et al., 2011). Moreover, if a child’s parent is an immigrant, the likelihood of living in poverty is even higher, with 27 percent of children living in poverty among immigrant parents compared with 19 percent when their parents were not immigrants to the United States (Wight et al., 2011). In addition, ethnicity can be linked to behavioral markers (e.g., diet, tobacco use, physical activity) that influence health in minority populations (Halbert and Allen, 2021).
Previous research, however, has seldom delved into the dimensional (e.g., sociocultural) or relational social constructs that underlie ethnic disparities. There is an emergence, though, of attempts to address this gap (Nandi and Platt, 2009; Umaña-Taylor and Shin, 2007). Some measurable elements that can aid in identifying constructs that might contribute to health disparities in biomedical sciences include ethnic
___________________
2 As of 2024, the OMB has broadened what can be considered an ethnicity by enabling people to choose their race(s), ethnicity(ies), or both, and to provide greater specificity about the sub-categories that reflect their identity. Note that virtually all of the sub-categories refer to nations or country of origin.
self-identification, surname (due to discrimination based on one’s name), religion, and language (Ford and Harawa, 2010).
Ethnicity is also intertwined with immigration, citizenship, and nationality. Attributes such as immigration status can warrant distinct measurement (Asad and Clair, 2018; Van Natta et al., 2018). Accounting for individual-level experiences of acculturation should be balanced by recognition of the importance of historical traumas and political policies (Samari et al., 2021; Viruell-Fuentes et al., 2012). Measuring the impacts of political policies is crucial because immigrant status alone may not capture the effects of discriminatory policies on non-immigrant groups. For example, when immigration or security-related policies or laws are enacted that affect an ethnicized group, it can affect their sense of belonging as a group, social support, experiences of discrimination, and familial connections (Johnson et al., 2024; Perreira and Pedroza, 2019). This impact extends to naturalized citizens as well as individuals born in the United States, including limitations on travel to and from the United States for both the affected groups and their family members residing outside the country.
INDIGENEITY
Another concept related to, yet distinct from, race is indigeneity, which emphasizes a connection to geographic location over time. There were tens of thousands of people indigenous to northern North America before European colonization. Many nations and their descendants are found in what is now known as the United States. This unique history is unlike that of any other racial or ethnic group in the United States. Only the Indigenous people of northern North America have lineages of families who lived for millennia on these specific lands, shaping cultural, medicinal, physical, spiritual, governmental, and societal structures. Only these Indigenous people have a history of sovereignty before contact with Europeans and, due to that sovereignty, had treaties drawn between sovereigns in Europe and including the U.S. Congress until 1871. And only Indigenous nations have retained that inherent sovereignty. Inherent sovereignty is the most basic principle of federal Indian law. It means that “the powers lawfully vested in an Indian Tribe are those powers that predate New World discovery and have never been extinguished” (Green and Work, 1976, p. 311).
This concept is critical because “it confirms the extra-constitutional status of [I]ndigenous nations as the original sovereigns of the Americas and does not treat [T]ribal nations as merely one of several ethnic groups” (Wilkins, 2006, p. 908). These 574 Nations3 have a federal government-to-government relationship stemming from Chief Justice Marshall’s Indian Law Trilogy of the early 1800s (Fletcher, 2014). This so-called federal trust responsibility (Department of the Interior, 2014) “is a well-established legal obligation that originates from the unique, historical relationship between the United States and Indian Tribes. The Constitution recognized Indian Tribes as entities distinct from states and foreign nations.” Therefore, only an
___________________
3 https://www.bia.gov/service/tribal-leaders-directory (accessed August 20, 2024).
enrolled AIAN individual can access Indian Health Service care or Bureau of Indian Affairs/Bureau of Indian Education services.4 One must prove one’s enrolled status. No other ethnic or racial group has such a relationship. As such, there are many laws pertaining only to AIANs or their lands. It is important to note that there are many more individuals who may have heritage or lineage in one of these Tribes but are not enrolled members. As such, they are not AIANs by the legal definition. It is the Tribes themselves who determine who is or can become a member. Congress determines who is a Tribe. The legal status of federally recognized Tribes leads to unique considerations for conducting biomedical research with AIAN Tribes (see Chapter 4 for more information on documented best practices).
AIAN ancestry is also measured by a concept known as blood quantum, which was integrated into federal law in 1887, for the purpose of dividing communal Indian lands into parcels and thereby pushing the concept of private land ownership onto Indians. Blood quantum cannot be measured directly but is typically inferred based on family lineage and has been used for sociopolitical purposes, underscoring the social construction of race in the United States (Rodriguez-Lonebear, 2021). As discussed in Chapter 2, race and ethnicity are social constructs, without a basis in biology. Despite its colonial and racist roots, blood quantum is used by many Indian Tribes to determine individual Tribal membership (Rodriguez-Lonebear, 2021), and the Bureau of Indian Affairs still requires that each AIAN submit paperwork proving that they are entitled to a Certificate of Degree of Indian or Alaska Native Blood, known as a CDIB. Some Tribes rely on provable lineage such as having an ancestor who appears on the Dawes rolls and can be directly traced back (National Archives and Records Administration, 2016).
These formal processes for determining AIAN ancestry and legal status can be at odds with other forms of measurement such as racial or ethnic self-identification (Garroutte, 2003). Self-identification can be fraught, given the distinct legal status of federally recognized Tribes. Indeed, once the U.S. census switched to enumeration using self-identification after 1960, the size of the American Indian population began to grow rapidly. Some welcomed the growth as a revival (Nagel, 1995), while others noted that the new identifiers seemed to be better off in terms of socioeconomic status, which could hide long-standing disparities between American Indians and other Americans (Snipp, 1986). Indigenous self-identification is also among the most fluid racial or ethnic identities, not only in the United States but around the world (Liebler et al., 2016; Shalley et al., 2023), with people who live in urban areas and have mixed ancestry being particularly likely to identify differently at different points in time; however, identity fluidity both within and across generations is much lower for people who live on or near Tribal lands, highlighting the importance of accounting for place in understanding differing outcomes and experiences within the AIAN population (Liebler, 2010).
___________________
4 https://www.bia.gov/service/tribal-leaders-directory and https://www.ihs.gov/forpatients/faq/ (both accessed August 20, 2024).
Adding to the complexity around self-identification as AIAN is that the OMB definition differs from the legal definition of American Indian. The OMB has taken a more expansive approach since 1997 (OMB, 1997; Snipp, 2003). The 2024 revision defines the AIAN category to “[include] all individuals who identify with any of the original peoples of North, Central, and South America” (OMB, 2024, p. 22187). This definition describes people who are Indigenous to the Americas and who have a shared experience of colonization. However, the legal definition of American Indian refers to membership with a Tribe as defined by Congress. The fact that these two definitions use the same term “American Indian” can lead to contradictions or misinterpretation in research. As an example, the OMB would include Aztec and Maya under AIAN. However, these populations are not domestic dependent nations5 within the boundaries of what is now known as the United States, so they do not meet the legal definition of American Indian. It is important to be cognizant of these different definitions in research contexts to ensure clear, accurate interpretations of research findings.
There is also a well-known bias in many health and vital statistics calculations for AIANs in the United States because they typically combine self-identification data from the census (in the denominator) and data from death certificates or cancer registries (in the numerator), which often rely on racial classification by others. Self-identified AIANs report being regularly misidentified in everyday interactions (Davis-Delano et al., 2021) and are frequently recorded as White in these data systems, which means their mortality rates and other health disparities estimates are misleading (Gartner et al., 2023; Jim et al., 2014; Rhoades, 2005). This underscores the importance of both understanding data provenance and ensuring consistency in data collection methods for race and ethnicity whenever possible. More generally, as Huyser and Locklear argue, “because there are multiple modes of affiliation to Tribal communities, a multiple-lens approach is useful to understand the full scope of the lives and life chances of AIAN peoples” (Huyser and Locklear, 2023, p. 250; see also Liebler, 2018).
SKIN COLOR AND PIGMENTATION
Skin color is often seen as synonymous with race or, at minimum, treated as the key criterion influencing categorical racial attribution. Recent research across the social and biomedical sciences complicates this view, however, conceptualizing skin color as one among many measures or dimensions that are related to perceptions of race and racism. In particular, there is a growing multidisciplinary literature on colorism that examines skin color variation to better understand both within- and between-group inequality across a range of socioeconomic and health outcomes (Branigan and Hall, 2023; Dixon and Telles, 2017; Laidley et al., 2019; Monk Jr., 2021; Stewart et al., 2020; Sweet et al., 2007). Collectively, this research indicates that skin color can be used either alongside other dimensions of race to identify more complex patterns of inequity or on its own
___________________
5 https://www.justice.gov/otj/about-native-americans (accessed August 20, 2024).
to capture a broader range of variation in human skin color, tone, reflectance, or some combination of the three.
Longstanding debates about the historical origins of race and racism, including its particular manifestation in the United States (Frost, 1990), hinge in part on how researchers interpret color distinctions made all the way back to antiquity (Jablonski, 2012), and whether (or when) they should be understood as expressions of prejudice (e.g., Derbew, 2022; Snowden, 1983). Is race just a rough categorical representation of continuous human variation in skin color, one that indexes privileging of lighter skin over darker skin, or should racial and color prejudices be seen as related but analytically distinct mechanisms for maintaining hierarchical relations? Some aspects of skin color are influenced by genetics and are thus inherited, but the same skin color phenotype (e.g., light skin) can be traced back to multiple lines of evolution in different populations, which may have different genetic bases for the trait; there is not a simple one-to-one relationship between skin color and genetic architecture (Jablonski, 2021; Norton et al., 2006). Skin tones are also shaped by environment, including proximity to the equator, as well as differing cultural valuations that may privilege lightness, darkness, or tanned skin (Dixon and Telles, 2017; Jablonski, 2004; Jablonski and Chaplin, 2000, 2010). The latter are often linked to variation in socioeconomic status between people who work indoors versus outdoors and between those who can or cannot afford skin care products that either change or maintain their skin tone (Glenn, 2008; Hunter, 2007). Research in social psychology also identifies contextual variation in how people weigh skin color, with differences in the magnitude of implicit skin color biases around the world (J. M. Chen and Francis-Tan, 2022) and people in some countries relying more on skin color to make categorical racial attributions than in others (J. M. Chen et al., 2018). The range of skin color variation observed within self-identified racial categories also differs by country, with some countries exhibiting more expansive notions of whiteness, blackness or ‘mixedness’ than others (McNamee, 2020). Thus, despite noted historical connections between skin color and racial ideology (Jablonski, 2021), treating skin color as the straightforward physical or biological component that underpins both racial classification and contemporary animus is unsupported by existing research across disciplines.
Theoretical and conceptual debates about the connections between skin color and categorical race aside, accurately representing human skin color is relevant to a range of biomedical research. This is perhaps most evident in dermatology, but with expanded importance across specialties given the proliferation of wearable medical devices. The Fitzpatrick skin typing system is the most common approach to assess and categorize skin color. The system was originally developed to measure photosensitivity and is still used in dermatology (Ware et al., 2020), partially because it is convenient and requires no special equipment. However, the Fitzpatrick scale has long had its critics. Even with the addition of two categories to account for darker skin in 1988 (Fitzpatrick, 1988), the scale is relatively insensitive to variation in darker skin tone and can result in underestimating dermatological conditions or misdiagnosis in people with more highly pigmented skin (Fenton et al., 2020). Furthermore, the Fitzpatrick scale and its common use in clinical practice can contribute to conflating race and ethnicity with
skin pigmentation (Ware et al., 2020). The von Luschan skin color chart has similar limitations as well as a troubling history, as it was used in unethical research in Nazi Germany.6 Even so, it is still in use today.
Given these problems, there have been attempts to develop more inclusive scales, such as the Monk skin tone scale (Monk, 2023). Others advocate more quantitative methods (Verkruysse et al., 2024), such as the Melanin index or CIELab system more commonly used in industry, which do not map to racial and ethnic categories. These methods are more objective and sensitive to variation; however, they are less convenient than color scales and do require more specialized equipment. Moreover, different methods can diverge in their measurement of the same skin tone. In research where skin pigmentation is relevant, such as pulse oximetry and optical sensors, methods attempting to precisely measure skin tone and pigmentation are more suitable than using social labels, such as race or ethnicity, as a proxy. Measurements should also align with the mechanism used by the device—for instance, measurements of reflectance (how light bounces off the skin) or transmittance (how light shines through the skin and tissues).
Considerable effort has also gone into testing and developing skin color measures for use in social surveys to understand complex patterns of inequality. These measures have evolved from simple nominal scales (“light,” “medium,” “dark”), initially used to understand colorism among Black Americans (Keith and Herring, 1991), to incorporating a broader range of variation that can be used to understand the role of skin color in both within- and between- group inequality. In the early 2000s, the Massey–Martin scale introduced a color card that interviewers would use to help standardize their observations of respondents’ skin color for face-to-face surveys. This 10-point scale, represented by a series of hands ranging in color from a very light white to very dark black, was initially developed for the New Immigrant Survey (Massey and Martin, 2003) and has since been adopted by the General Social Survey and the 1997 National Longitudinal Survey of Youth, among other data sources. These data have yielded important evidence regarding the nature and extent of colorism in the contemporary United States (Adames, 2023; Bailey et al., 2014; Han, 2020; Katz et al., 2020). The Massey–Martin scale has been critiqued, however, both for its lack of inclusivity (e.g., representing shades between white and black rather than variation in color, per se) and inability to fully eliminate interviewer variation (Abrajano et al., 2023; Cernat et al., 2019; Hannon and Defina, 2020). As a result, some researchers incorporate technical measures obtained through either a handheld colorimeter or spectrophotometer (Gordon et al., 2022; Ostfeld and Yadon, 2022). Others have developed more inclusive color palettes, such as the Monk Scale developed in collaboration with and currently being used by Google (Monk, 2023); see also the PERLA and PRODER palettes developed for use in Latin America (Solís et al., 2023; Telles, 2014).
As with other measures or dimensions of race, there is no one correct way to measure skin color that spans research questions or applications. Recent research highlights the challenges of skin color measurement while pointing to the strengths and weaknesses of different approaches (Campbell et al., 2020; Dixon and Telles, 2017; Gordon et al.,
___________________
6 https://collections.ushmm.org/search/catalog/irn564926 (accessed October 15, 2024).
2022; Heldreth et al., 2024; Khan et al., 2023; Piña et al., 2023). For example, measures obtained using devices likely will be most useful for technical applications—from wearable medical devices to self-driving cars—where variations in color and skin reflectance that are not visible to the naked eye are still relevant to achieving equity and reproducibility of rigorous scientific results. Measures of skin color as recorded by an interviewer or other observer could be most relevant for understanding explicit discrimination, while measures of skin color reported by the individual in question can represent that individual’s own perceived social position (Gravlee and Dressler, 2005; Monk Jr., 2015). Researchers also must carefully consider the relationship between skin color and socioeconomic status and whether they aim to assess their combined effects or establish their separate contributions to a particular outcome (Abascal and Garcia, 2022; Solís et al., 2023). Although best practices for measurement in this area are still in development, it is indisputable that skin color has an important role to play in biomedical research. Incorporating skin color measures can make technical applications more precise as well as highlight the limits of categorical approaches to understanding human variation.
RELATIONAL ASPECTS OF RACE
In addition to codifying the categories of race and ethnicity that are recommended for federal data collection, OMB Statistical Directive 15 also represented a shift from relying on racial classification by others to a focus on self-identification (Snipp, 2003). Thus, another legacy of Directive 15 has been the perception that self-identification, using the OMB categories, is the “gold standard” measure of race and ethnicity (Jarrín et al., 2020; Wallman et al., 2000). This assumption has led some researchers to focus on the level and consequences of “misclassification”—that is, when a measure of self-identification is not concordant with another way of gathering racial or ethnic data (Hahn et al., 1992; Kressin et al., 2003). However, a growing body of research in the social sciences emphasizes the multidimensionality of race and ways of examining both how the multiple measures (or dimensions) differ and how they can interact.
Scholars have demonstrated the benefit of thinking about race multidimensionally and have outlined a typology for disaggregating an individual’s “race” into separate components, from their known ancestry to their skin tone to how they are perceived by others (Roth, 2016). Making these distinctions is, in part, about conceptual precision: being clear about which aspect of a person’s racialized experience is being considered and why. Importantly, a multidimensional approach also recognizes that how people describe themselves using standard racial or ethnic categories may not be the most relevant measure across all contexts and research studies. Two measures that aim to capture the relational or interaction-based aspects of race and racialization are perceived race and reflected race. Using measures such as these helps direct research attention away from treating race as a static characteristic of an individual, or what someone is, to treating race as a dynamic aspect of social interactions and a consequence of racism, which makes how people are perceived and treated by others especially salient.
Perceived race is measured by how someone else would describe the person of interest and, until Directive 15, was typically the default way of assigning research
participants to racial categories. In the U.S. census, race was recorded by an enumerator up until 1960, when the Census Bureau began mailing forms to Americans for self-completion. Many large national surveys still relied on the interviewer’s assessment of the respondent’s race as recently as the 2000s (Saperstein, 2006). Some have argued that perceived race is a more relevant measure than self-identification if the aim is to capture the effects of racial discrimination (e.g., Telles and Lim, 1998). Others have noted the irony of the U.S. census switching from perceived race to self-identification around the same time (following the Civil Rights Movement) that it began using federal racial data for anti-discrimination efforts (Morning and Sabbagh, 2005; Snipp, 2003). Recent research does show that studies using perceived race versus self-identification can come to different conclusions about the nature and extent of racial inequality (Saperstein, 2006, 2012). Studies that consider the intersection of perceived race and self-identification also find that racial disparities in outcomes such as arrests and home ownership—for which police officers and lenders, respectively, are key gatekeepers—are better attributed to perceived race than self-identification (Penner and Saperstein, 2015; Saperstein et al., 2016). For example, among U.S. young adults who had never been arrested, those who were perceived as Black by the survey interviewer but did not self-identify as Black were three times more likely to subsequently be arrested than those who self-identified as Black but were not perceived as Black (Penner and Saperstein, 2015). These findings underscore the importance of not only disaggregating measures of race but also using them in tandem to help isolate potential mechanisms perpetuating racial inequality. In a similar way, using multiple measures of race could augment precision in investigating mechanisms that perpetuate and exacerbate health disparities. Measures of perceived race are available in several large national surveys that conducted face-to-face interviews, including the 1979 National Longitudinal Survey of Youth, the 1997 National Longitudinal Survey of Youth, the 1996 and 2000 waves of the General Social Survey, and the National Longitudinal Study of Adolescent to Adult Health.
Reflected race is a more recently proposed measure that aims to understand how a person thinks they are racially categorized by others. The term comes from the social psychological concept of reflected appraisals or how people feel they are seen by others more generally (Felson, 1985; Gallagher et al., 2022). It can be treated as a proxy for perceived race in studies, such as online surveys, where obtaining an interviewer or other external classification is not practical. Reflected race is also a unique measure that can differ from both the actual perceptions of others and how the person self-identifies, with important implications for mental health as well as the likelihood of perceiving racial discrimination (Sosina and Saperstein, 2022; Stepanikova and Oates, 2016). An early measure of reflected race, dubbed “socially assigned race” (Jones et al., 2008), was collected as part of an optional Reactions to Race module for Behavioral Risk Factor Surveillance (BRFSS). Recognizing that people may be perceived differently in different contexts, more recent studies rely on more focused measures that specify how someone would be categorized by “a stranger passing by on the street.”7 Some research highlights that experiencing “racial identity contestation” (Vargas and Kingsbury, 2016),
___________________
7 Also called street race, see Lopez et al., 2018.
or feeling like your identity is not validated by others, can have negative effects on mental health (Albuja et al., 2019). Overall, the growing body of work on reflected race shows that how people think they are perceived racially is associated with a host of outcomes, including mental and physical health, with people who think they are seen as White reporting better outcomes (Abuelezam et al., 2022; Stepanikova, 2010). In addition to the BRFSS measure, reflected race questions have previously appeared in the Pew Survey of Multiracial Adults, the New York Longitudinal Survey of Wellbeing, and the Portrait of American Life Study, among other surveys.
GENETIC MARKERS AND ANCESTRY
The relationship between genetics and race or ethnicity is used to different ends depending on the research question of interest and the data at hand. Despite repeated calls for their disambiguation, this conflation of distinct constructs persists in biomedical research. The social constructs of race and ethnicity continue to be used incorrectly as proxies for genetic ancestry, which in turn is sometimes used as a surrogate for specific genetic markers that are thought to be more common in particular groups than in others. Fortunately, this practice is declining in more recent research given increasing awareness of the weak relationship between social constructs and biological markers, although it persists in published literature (Swilley-Martinez et al., 2023). In genetics research, the use of “race” to both describe and define groups has declined with the simultaneous increase of “ancestry” and “ethnicity,” indicating a movement toward precision in describing the salient aspects of group differences (Byeon et al., 2021).
To avoid the inappropriate use of race and ethnicity as proxies of genetic variation, several concepts must be disambiguated. First is the concept of genetic ancestry, which is defined as “the paths through an individual’s family tree by which they have inherited DNA from specific ancestors” (NASEM, 2023, p. 4; see also Mathieson and Scally, 2020). This concept refers to a longitudinal view of shared genetics through a family tree. Genetic ancestry is distinguished from genealogical ancestry by the inheritance of DNA along a specific lineage. Individuals can have genealogical ancestors in their family tree from whom they have not inherited any DNA due to a biological process known as recombination down the generations. In practice, most genetics research does not directly measure multiple generations on a family tree and therefore cannot directly measure genetic ancestry. Instead, genetic similarity is quantified by estimating “the genetic resemblance between individuals that reflects the extent of shared genetic ancestry” (NASEM, 2023, p. 4; see also Coop, 2022). In practice, these estimates are then used to cluster individuals into “genetic ancestry groups,” which are assumed to model a level of homogeneity that meets statistical assumptions with respect to allele frequencies and linkage disequilibrium, or correlation, patterns between variants. Genetic ancestry groups are then used as analytical units in stratified analyses that are meant to seek to control for these differences in genetic architecture as well as unmeasured potential environmental (non-genetic) confounders. Readers interested in a deeper exploration of genetic ancestry and genetic similarity should refer to NASEM (2023).
The standard practice of using “genetic ancestry groups,” which often are delineated at a continental level (e.g., “European,” “Asian,” and “African”), problematically conflates the concepts of genetic ancestry and race (Byeon et al., 2021; Cerdeña et al., 2022a; Lewis et al., 2023), which propagates the use of these concepts in race-based medicine (Bentz et al., 2024; Cerdeña et al., 2022b). Additionally, this practice has been misappropriated by extremists as proof of biological races to further their supremacist agenda (Carlson et al., 2022). These beliefs have been reinforced through the messaging of direct-to-consumer genetic ancestry testing, such as the companies 23andMe and AncestryDNA, which reify race as a biological reality (Phelan et al., 2014). These tests do not directly estimate “genetic ancestry” as defined above, but rather what proportion of the customer’s genome is similar to the company’s reference data (Royal et al., 2010). It is important to dispel these beliefs, as is recommended in a recent NASEM report which said, “When grouping people in studies of human genetic variation, researchers should avoid typological thinking” (NASEM, 2023, p. 103). This recommendation applies to biomedical research broadly.
There are several scenarios in which the use of racial or ethnic identity as a proxy for genetic similarity fails to capture either genetic or environmental factors. The first example of this is the group “Asian,” which typically denotes individuals with ancestry from the continent of Asia, comprising East Asia, Southeast Asia, and South Asia (Lee and Ramakrishnan, 2020), although the predominant group to which it refers depends on socio-cultural context with respect to historical immigration patterns (Aspinall, 2003). This is reflected in genetic data of large-scale studies, such as the UK Biobank (UKB)8 and NIH’s All of Us Research Program.9 In the UKB, individuals coded as “Asian or Asian British” corresponded to countries of origin in South Asia (India, Pakistan, Bangladesh), while “Chinese” is a category outside of the Asian/Asian British category. In contrast, the analogous category of “Asian” in the All of Us Research Program consisted of mostly East Asian individuals, although combined with substantial numbers of South Asian participants as well. The genetic backgrounds from these individuals, even at a subcontinental-level (such as China versus Japan within East Asia) have been found to demonstrate substantial population substructures (GenomeAsia100K Consortium, 2019; IGSR, 2024; Tian et al., 2008) which are not appropriate to combine if statistical methods require relative homogeneity or for the estimation of population-specific allele frequency for clinical genetics (Chan et al., 2022). For example, researchers estimated the genetic risk for familial hypercholesterolemia across autosomal dominant genetic variants among patients in Singapore and found that Chinese participants had significantly higher genetic risk (1.05 percent) compared with Indian (0.15 percent) and Malay (0.25 percent) participants, driven primarily by a higher prevalence of LDLR carriers among Chinese participants (0.76 percent) (Chan et al., 2022). Therefore, researchers using the broad racial category of “Asian” as a proxy for genetic similarity may fail to account for complex substructure with misleading or erroneous results or may obfuscate the genetic architecture of interest. Concurrently, “Asian” as a grouping to control for
___________________
8 https://biobank.ctsu.ox.ac.uk/crystal/field.cgi?id=21000 (accessed October 15, 2024).
9 https://www.nature.com/articles/s41586-023-06957-x (accessed October 15, 2024).
environmental factors is also not appropriate, given the extensive heterogeneity between populations (Budiman and Ruiz, 2021), such as rising income disparities (Kochhar and Cilluffo, 2018).
These dynamics are compounded in recently admixed populations, particularly within the ethnic categorization of “Hispanic and/or Latino.” Across the Americas, these groups have recent ancestry in multiple continental and subcontinental regions, primarily Africa, Europe, and the Americas (Bryc et al., 2010; Conomos et al., 2016; Homburger et al., 2015; Moreno-Estrada et al., 2013, 2014). Numerous studies of their genetics have demonstrated the varied composition of populations both between and within current national borders. For example, work conducted in a single study, the Hispanic Community Health Study (HCHS)/Study of Latinos (SoL), estimated participants’ admixture proportions, or proportion of their genome that was estimated to be similar to inferred genetic ancestries (Conomos et al., 2016). They found substantial heterogeneity between groups, such as higher levels of what they estimated to be African ancestry in Dominican and Puerto Rican participants and higher Amerindigenous ancestry in Central American participants. It is important to note that these studies of genetic ancestries are further complicated by complex immigration patterns that vary by time and geography. Within HCHS/SoL, Cuban participants were estimated to have over 80 percent European ancestry. However, this is reflective of both who immigrated to the United States and selection bias for which households would have participated in this study, as demonstrated by comparing these participants to genetic studies done within Cuba, which estimates the average European ancestry proportion to be 71 percent (Fortes-Lima et al., 2018). This demonstrates that the use of Hispanic and/or Latino as a salient genetic category is inappropriate and ineffectual to capture assumed levels of similarity that would be considered appropriate for genetic studies. In addition, the incorporation of environmental (e.g., non-genetic) variables into genetic risk estimation models contribute additional layers of heterogeneity with intersectional differences between groups. For example, a study within HCHS/SoL found that a genetic score for body mass index demonstrated significant heterogeneity between Hispanic/Latino groups, which was modified differentially by age at immigration (McArdle et al., 2021). Taken together, these caution against the use of racial or ethnic categories as signifiers of genetic similarity, or homogeneity, especially when considered across environmental contexts in genomic and non-genomic studies.
Another complication within genomic studies is the consideration of multiracial individuals. These participants differ from admixed populations as defined above. While most present-day human populations are to some extent admixed, meaning having ancestry from two or more previously isolated populations, recently admixed populations in the United States are conceptualized as those with mixture between groups previously separated at a continental level. In the United States, the two largest groups are populations of African Americans and Hispanic/Latino groups. These groups are the result of continuous mixture over the past several hundred years due to forces of colonization, forced enslavement, and complex immigration patterns across the Americas (Bryc et al., 2015; Gouveia et al., 2020; Mathias et al., 2016; Schroeder et al., 2015). As a result, their genomes form a mosaic of previously isolated ancestries,
or haplotypes, which can be studied using statistical genetics methods. In contrast, multiracial individuals are defined by having more recently mixed ancestry, within only a few generations, which requires different considerations from both the standpoint of their identification with monoracial (e.g., purportedly single-race) groups as well as appropriate modeling of their genomes, which would have much larger haplotypes, including entire chromosomes from a single ancestry in some biracial individuals. Due to these complications, multiracial individuals are often excluded from analyses, both genetic and non-genetic, and have limited access to medical innovations, which rely on discrete groupings (Martschenko et al., 2023; Phillips et al., 2007).
APPROACHES TO ANALYZING DATA FROM MULTIRACIAL INDIVIDUALS
This section contains material adapted from a piece commissioned for the committee.
In 2000, the U.S. census allowed Americans to officially self-identify with more than one racial group for the first time (U.S. Census Bureau, 2001). Two decades later, the self-identified multiracial population is measured at 33.8 million—nearly a 500 percent increase—and represents over 10 percent of the U.S. population (U.S. Census Bureau, 2001, 2021, 2023). The dramatic growth in multiracial reporting can be attributed to a number of factors, from an increase in interracial marriage to increasing acceptance of multiracial identities (Lo Wang, 2021; Tavernise et al., 2021). However, the biggest change over the past decade was in how the U.S. Census Bureau captured and coded race and ethnicity responses, producing a sudden jump from 9 million people, or a 276 percent increase, since 2010 alone (Reynolds, 2021). This sensitivity to changes in data collection and coding underscores a point that demographers have long stressed: that census counts based on self-identification reflect “a” multiracial population not “the” multiracial population (Harris and Sim, 2002; see also Goldstein and Morning, 2000). As previous research has shown, the size of the multiracial population depends on both how it is defined and how the data are collected. The largest estimates of multiracial Americans (about 18 percent of the U.S. adult population) come from asking people about the race(s) of their parents, grandparents, great-grandparents, and earlier ancestors, while the smallest estimates come from asking people if they identify explicitly as “mixed or multiracial,” with the number of people who select two or more responses from a list of single race or ethnicity categories for self-identification falling somewhere in between (Morning and Saperstein, 2018; Patten, 2015). Although these measurement issues appear most stark when considering people who self-identify as multiracial, they highlight broader conceptual and operational challenges for researchers who are intending to use race and ethnicity in biomedical studies.
Just as it is important conceptually to disentangle genetic measures of ancestry from genealogical ones, it is also necessary to disentangle both genetic and social understandings of ancestry from self-identification using racial or ethnic categories. Although often conflated, each of these measures captures something different about a
person’s socialization and life experience that is relevant to their health. As discussed above, genetic measures of ancestry reflect similarities and differences in how alleles and haplotypes are distributed across human populations. Genealogical measures of ancestry include pedigrees or family trees that trace kinship across generations using vital records, such as birth, marriage, and death certificates kept by religious institutions and local and national governments. These official genealogical documents may differ from more informal notions of ancestry that are passed down in families. Finally, individuals’ known ancestry can differ from what they self-report on surveys. Historically, in the United States both laws and customs shaped how people’s ancestral backgrounds affected their treatment in society, the most infamous of these being the “one-drop rule” that defined Americans with any known African ancestry solely as Black (Davis, 2010). Views of racial “mixing” and multiraciality have changed significantly over time from something illegal that needed to be hidden to an aspect of one’s identity to celebrate. This history, and the changing stakes of racial classification, is reflected in differences across generations in both awareness of multiracial ancestry and the willingness to report multiracial identification in surveys (Johfre and Saperstein, 2019). Patterns of multiracial self-identification also vary by gender, the specific racial backgrounds involved, and how far back in a person’s family tree the first racial “mixing” occurred (Xu et al., 2021). The use of direct-to-consumer genetic ancestry testing is increasingly shaping people’s understanding of their ancestry and their likelihood of translating that ancestry awareness into racial or ethnic self-identification in surveys as well (Johfre et al., 2021). This complexity shapes the identities of both monoracial and multiracial people and underscores the importance of carefully considering which concepts and measures of race, ethnicity, and ancestry are most relevant for a given research question.
To date, however, not only does most biomedical research continue to conflate various measures of ancestry and racial or ethnic self-identity, but also multiracial participants are routinely excluded in studies seeking to identify racial disparities in health. This exclusion leaves significant gaps in our understanding of health risks, including those that might differentially affect multiracial people, and consequentially underinvestment in addressing them (Lam-Hine et al., 2024). The few studies that do include a multiracial category in analysis operationalize it differently, creating challenges for interpreting results (Lam-Hine et al., 2024). A variety of different approaches are in use in the literature (Table 5-1), and uncertainty around how to define and categorize multiracial identity likely prevents greater inclusion of multiracial and multiethnic populations in biomedical research.
Relevant to the biomedical context, health care systems are collecting more granular race and ethnicity data, including from people who self-identify as multiracial or multiethnic, and have begun using these data to stratify measures of quality with the goal of ensuring equitable care (Wang, 2024). Yet, there are few standards in place for how best to categorize people who identify as multiracial or multiethnic. The same dataset can yield different results depending on the methodology for analyzing multiracial individuals. For example, electronic health record data from a Connecticut hospital of approximately 666,000 people include about 38,000 people (5.7 percent)
TABLE 5-1 Multiracial Categorization Schemes Currently in Use in the Literaturea
| Categorization Schemes and Descriptions | Considerations for Use |
|---|---|
| Use a single category called “multiracial” for everyone who chooses multiple categories | |
|
Pros: Straightforward; can examine attributes common to multiracial experience. Con: Nuanced information about multiracial identity and experiences could be lost. Example: Studying racial identity affirmation and belonging because individuals identifying with more than one race tend to report relatively low levels of racial identity affirmation and belonging and systematic exclusion from racial identity-affirming communities. |
| Sort into all categories selected | |
|
Pro: Could be useful when examining a circumstance or mechanism where component racial backgrounds could influence outcomes. Con: Can complicate some analyses because group percentages will not add to 100%. Example: Additive + Multiracial could be well suited to studying racial discrimination because multiracial individuals can experience discrimination directed at their multiracial or component racial backgrounds. |
| Select the single least advantaged category | |
| Hypodescent: Recategorizing multiracial respondents into their most socially disadvantaged racial group. Note: Hypodescent reflects the historical “one-drop rule” that continues to shape some multiracial identification today. |
Pro: Could be useful when examining risk factors and stressors that are more likely to be experienced by less socially advantaged groups. Cons: Recategorization may not reflect participants’ identity; may be more challenging to define compared with other approaches because social advantage and disadvantage are relative. Example: Studying racial and ethnic differences in exposure to traumatic events and development of depression. |
| Select the single most advantaged category | |
| Hyperdescent: Recategorizing multiracial respondents into their most socially advantaged racial group. | Pro: Could be helpful when examining circumstances where multiracial individuals’ experiences are similar to those of their most socially advantaged component group. Cons: Recategorization may not reflect participants’ identity; may be more challenging to define compared with other approaches because social advantage and disadvantage are relative. Example: Studying unmet psychiatric treatment needs because multiracial Americans access psychiatric treatment at rates similar to White Americans. |
| Select the single rarest (least common) category | |
| Rarest: Recategorizing multiracial respondents into their least populous racial group. | Pro: Can improve power in estimates for smaller groups that include many multiracial members, such as Native Hawaiian or Pacific Islander and American Indian or Alaska Native. Con: Could aggregate people who do not share exposures into one category. |
| Participants select a single category that they most identify with | |
| Best Race: Recategorizing multiracial respondents into the single race that they identify best with. | Pros: Could be useful when examining racial discrimination; can reflect socially assigned race, which may be relevant to the line of inquiry. Cons: Could lose information about multiracial identity; this scheme should be used with caution as many multiracial people do not identify with a single race and may refuse to do so. |
| Analyze subcategories of multiracial identity | |
|
Pro: Can help uncover nuances of multiracial identity and experience. Con: Low statistical power due to many small categories (using disaggregated White/nonWhite multiracial could help with low power but risks reinforcing White as the norm). Example: Examining racial discrimination, particularly if using a measure that includes multiracial-specific forms of discrimination alongside more traditionally measured ones. |
a This review focused on schemes that can be coded using the 1997 OMB Statistical Policy Directive No. 15 self-reported racial and ethnic categories: American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, and White for race; Hispanic or Latino or Not Hispanic or Latino for ethnicity.
NOTE: These are existing approaches, and care should be taken before selecting and using one.
SOURCE: Adapted from Forthal, Sarah (2024). A mechanism-driven approach to categorizing multiracial participants in biomedical research (Appendix C). Work commissioned by the Committee on the Use of Race and Ethnicity in Biomedical Research at the National Academies of Sciences, Engineering, and Medicine.
who self-identify as multi-racial/ethnic, but there are various ways to organize the information (Wang, 2024). Using the methodology based on a paper from the Centers for Disease Control and Prevention (CDC), any person who identifies as Hispanic, regardless of how they identify themselves racially, are categorized as Hispanic, and any who identify as multiracial and not Hispanic would be excluded (Yoon, 2021). Applying a different methodology to the same Connecticut hospital dataset, someone who identifies as multiracial is categorized into the race with the lowest prevalence in the measured population (Mays et al., 2003). For example, in this Connecticut hospital dataset, a person who identifies as Asian and Black would be categorized as Asian (Wang, 2024).
The use of racial categories assumes a shared within-group social identity (Jackson, 2023). However, this is particularly challenging to assume for multiracial individuals, who share identities with multiple groups and may primarily identify with one, all, or none of their component monoracial groups (Vinluan and Remedios, 2020). Further, different racial identities may be more or less salient for multiracial people in different contexts (Pauker et al., 2018). For example, some multiracial people primarily identify as members of their most minoritized monoracial group due to historical or political reasons (Davenport et al., 2022; Iverson et al., 2022). Ultimately, researchers cannot simply assume that all multiracial people identify with a separate “multiracial” identity, nor that they identify with any monoracial identity. Multiracial people are also exposed to systemic racism, both on the basis of their multiracial and specific racial backgrounds, which increases their risk of several health conditions (CDC, 2018a,b; J. C. Harris, 2016; Lam-Hine et al., 2024; Merrick et al., 2018; SAMHSA, 2021). Though relevant to all racial groups (Iwamoto and Liu, 2010; Neblett Jr. et al., 2012), racial identity affirmation and belonging is particularly prevalent in the multiracial health literature, given common experiences of identity denial and questioning in this population (Albuja et al., 2019, 2020; Fisher et al., 2019; Franco et al., 2021; Jackson, 2023; Nalven et al., 2021; Sanchez, 2010). Thus, the many ways that multiracial backgrounds shape environmental or social exposures are not easily captured by traditional research methods, which rely on drawing fixed and discrete lines between groups for comparisons that are often essentialist in nature (Kaufman, 1999; Mays et al., 2003). For these reasons, there is likely no single best multiracial categorization scheme for all biomedical research purposes. Instead, as with other racial and ethnic categorization decisions (Guluma and Saperstein, 2022; Howell and Emerson, 2017; Shiao, 2019), the most appropriate multiracial categorization scheme will depend on the outcome of interest and the hypothesized mechanism linking race and racism to health.
BIOMARKERS OF STRESS AND OTHER PHYSIOLOGICAL PROCESSES
Rather than using race and ethnicity categories as proxies for studying physiological mechanisms of health and disease, it is far preferable to investigate the phenomenon of interest directly, when possible. Biomarkers are physiological indicators used to assess and monitor biological processes related to health and well-being. These markers can signify various processes, including (1) as a surrogate endpoint for a disease, (2) a biological mechanism, or (3) an indicator of future disease risk. As it relates to
biological mechanisms, biomarkers not only offer insights into future disease risk but also can indicate exposure to various factors. For instance, hormonal biomarkers such as cortisol, norepinephrine, and epinephrine have been used to signal exposure to stressors.
Related to the neuroendocrine, immune, and cardiovascular systems, stress biomarkers are associated with health and disease risk (Dowd and Goldman, 2006). The cumulative physiological effects due to chronic stress or life events, known as allostatic load, can affect immune system functioning, which can result in increased oxidative stress levels and damage to DNA (Djuric et al., 2008). Chronic environmental stress and the consequent oxidative stress on cells and tissues is also linked to aging (Liguori et al., 2018). Allostatic load can be measured via biomarkers, such as levels of cortisol, epinephrine, cholesterol, and interleukin 6, along with blood pressure, among many others (Dowd and Goldman, 2006; Guidi et al., 2021).
In the context of race and ethnicity within biomedical sciences, biomarkers have been instrumental in exploring the effects of adverse exposures on populations, particularly in relation to stressors linked to racialization. For example, researchers have found that exposure to discrimination correlates with immune and inflammatory biomarkers, such as C-reactive protein and IL-6, among other immune markers (Chen et al., 2023; Lawrence et al., 2022; McClendon et al., 2021). The relationship between stress biomarkers and health disparities has led to the hypothesis of “weathering”—that is, that members of racial and ethnic minority groups experience accelerated aging and physical deterioration due to chronic stress (Geronimus et al., 2006; Noren Hooten et al., 2022). Further, there is a significant amount of research indicating that a wide range of stressors, including socioeconomic disadvantage, influence immune-related biomarkers (Kautz et al., 2023; Lam et al., 2021; Muscatell et al., 2020). Moreover, emerging studies suggest that stressful exposures at the neighborhood level, such as living in previously redlined and segregated neighborhoods, also affect these biomarkers (Broyles et al., 2012; Iyer et al., 2022; Simons et al., 2018). Consequently, differences in these biomarkers across racial and ethnic groups can often be traced back to varying levels of stressor exposure at both individual and neighborhood levels. Since these stress-related mechanisms operate similarly across all populations, differences in biomarkers across racial and ethnic groups do not indicate inherent biological differences between groups. Like genetics research, the field of biomarker research, especially when examining issues related to race and ethnicity, is susceptible to biological essentialism. Therefore, it is important to clearly articulate the question of interest and, whenever possible, to measure the factors of interest that may result in variation in biomarker values across groups rather than a measuring proxy such as race or ethnicity.
Aside from stress-related measures, biomarkers vary across every clinical domain. BRCA1 and BRCA2 genes are well-known examples that are associated with increased risk of breast cancer. Hemoglobin A1c is a biomarker for diabetes and is used to both diagnosis and monitor the condition. In some cases, differences that seem correlated with race are accounted for once the biological mechanism is known and a corresponding biomarker can be measured. In ophthalmology, for example,
glaucoma is more prevalent among Black than among White populations. Much of this difference was explained, however, by variation in the thickness of the central cornea (Brandt et al., 2001). Identified as a risk factor for glaucoma, thinner corneas are associated with a higher propensity to develop glaucoma (Brandt et al., 2001; Hyman and Mehta, 2004; Wang et al., 2014). This measurable biological construct may account for at least some of the increased risk of glaucoma noted among Black populations (Brandt et al., 2001).
In an example from cardiology, researchers examined health disparities in major adverse cardiovascular events and major hemorrhage after percutaneous coronary intervention (Cai et al., 2019). Disparities in outcomes were often attributed to race; however, after adjusting for other nonclinical and clinical factors, the results indicated that race was not a significant risk factor. Differences were instead attributable to other risk factors, including socioeconomic status, comorbidities, and coronary heart disease severity (Cai et al., 2019).
Biomedical research has demonstrated variability in stress-related biomarkers across racial and ethnic groups. These stress-related mechanisms are phenomena that can be found in all human physiology, and differences are attributable to unequal exposures to stressors, disadvantage, racism, and discrimination. Stress-related exposures can be differentially distributed within and between racial and ethnic groups, so race and ethnicity are poor proxies for these biomarkers. Similarly, it is important to be wary of attributions to race in biomedical contexts and studies of other biomarkers; the existence of a health disparity does not mean that there is a difference in health due to race or ethnicity. More work is needed to continue investigating biomarkers that can more directly interrogate biological processes that may underly health disparities, uncover mechanisms of disease, and avoid the risk of biological essentialism.
CHAPTER SUMMARY AND CONCLUSIONS
This chapter opened by examining the use of the OMB categories in biomedical research. Based on the information presented in this and earlier chapters, the committee provides the following conclusions:
Conclusion 5-1: The OMB categories are a minimum set of categories unique to the United States. The OMB categories are often required for inclusion reporting purposes in research. However,
- the OMB categories are a sociopolitical construct with no biological basis.
- the OMB categories are a minimum set of categories, but federal agencies and the scientific community can collect more detailed information.
- the OMB categories do not need to be used for scientific analysis, even if they are required for reporting recruitment statistics.
Conclusion 5-2: Reporting requirements from NIH and other funders of biomedical research often rely on the OMB categories for ensuring a racially and ethnically diverse sample population. This reliance on the OMB race and ethnicity categories
for reporting has contributed to the categories becoming enmeshed in science and medicine.
Conclusion 5-3: The 2024 revisions to the OMB’s Directive 15 on collection of data on race and ethnicity include adding the category Middle Eastern or North African and requiring the collection of more detailed subcategories by default. These changes to the standards will improve the quality of demographic data for some research purposes but do not completely resolve limitations to the use of the OMB categories for biomedical research.
- The OMB relies on a set of racial and ethnic categories that are increasingly defined by regional or national origin in the 2024 policy. However, these measures alone may be insufficient for measuring diversity in biomedical research or addressing research questions of interest.
- The OMB categories, including the revised 2024 standards, were not designed for health research, and interpretation of the policy by NIH and others will influence how the updated standards apply in biomedical research.
- Achieving diversity in biomedical research participation should not be limited to representation across the OMB categories.
Implementing the new OMB standards will reveal new challenges, particularly when it comes to operationalizing the collection of subcategories and coding write-in responses. As Directive 15 notes, regular reviews of the policy will be necessary.
The chapter continued with the committee’s articulation of racism-conscious research, an answer to the need for an approach that directly acknowledges and addresses how racism has affected biomedical research practices and contributed to health disparities. Based on evidence presented in this and previous chapters, the committee concluded:
Conclusion 5-4: Although race is not biological, it continues to be relied upon as a blunt tool, heuristic, or variable in medicine to assess patients’ disease risk. Much of the existing evidence base in biomedical research that involves humans and uses White or European populations as the standard grew out of race-based approaches that perpetuate discriminatory presumptions.
Conclusion 5-5: Genetic differences among groups of people are not racial differences. Genetic differences may have meaning in biology and a role in medicine and research. Race, though, is not a substitute for unseen or unmeasured biological predictors of interest.
Conclusion 5-6: Racism-conscious research invokes an awareness of how unfounded racial assumptions and racism have affected biomedical research, resulting in harms and inequitable treatment and care.
The chapter then explored other concepts and variables which are often conflated with race. These other concepts or measures can be more precise or better suited to the scientific line of inquiry. An overemphasis on race, specifically the OMB categories, has collapsed rich heterogeneity into simple labels that can make doing rigorous research that teases apart nuanced mechanisms of interest challenging or impossible. Some of the concepts explored in this chapter, such as ethnicity, are closely related to race. Common use of race and ethnicity interchangeably has exacerbated confusion among researchers and the public, but these concepts are nuanced and need to be disentangled to elucidate the specific characteristics or processes of interest. Other concepts like structural racism and social determinants have been linked to health outcomes. Race has multiple dimensions, including not only self-identification but also relational or interaction-based aspects of race and racialization, that contribute to experience. Limitations to self-identified race, such as for the AIAN population, have been largely overlooked. In other cases, race has sometimes been relied on to capture unspecified variation, and further investigation into biomarkers, physiological mechanisms of action, and environmental factors may serve to better explain differences and phenomena in biomedical research. Due to the prolonged emphasis on race, there is less evidence on the use of related concepts in biomedical research, and more exploration and examination is warranted. Along with the committee’s recommendations, Chapter 6 introduces best practices for measuring these concepts in the context of biomedical research (see “Approaches and Metrics to Strengthen Inquiry about Race, Ethnicity, and Related Concepts”).
REFERENCES
Abascal, M., and D. Garcia. 2022. Pathways to skin color stratification: The role of inherited (dis) advantage and skin color discrimination in labor markets. Sociological Science 9:346–373.
Abrajano, M., C. S. Elmendorf, and K. M. Quinn. 2023. Measuring perceived skin color: Spillover effects and likert-type scales. Journal of Politics 85(1):320–327.
Abuelezam, N. N., A. G. Cuevas, S. Galea, and S. S. Hawkins. 2022. Contested racial identity and the health of women and their infants. Preventive Medicine 155:106965.
Adames, A. 2023. The cumulative effects of colorism: Race, wealth, and skin tone. Social Forces 102(2):539–560.
Adkins-Jackson, P. B., T. Chantarat, Z. D. Bailey, and N. A. Ponce. 2022. Measuring structural racism: A guide for epidemiologists and other health researchers. American Journal of Epidemiology 191(4):539–547.
Afshari, R., and R. S. Bhopal. 2010. Ethnicity has overtaken race in medical science: Medline-based comparison of trends in the USA and the rest of the world, 1965–2005. International Journal of Epidemiology 39(6):1682–1683.
Albuja, A. F., D. T. Sanchez, and S. E. Gaither. 2019. Identity denied: Comparing American or White identity denial and psychological health outcomes among bicultural and biracial people. Personality and Social Psychology Bulletin 45(3):416–430.
Albuja, A. F., D. T. Sanchez, and S. E. Gaither. 2020. Intra-race intersectionality: Identity denial among dual-minority biracial people. Translational Issues in Psychological Science 6(4):392–403.
Asad, A. L., and M. Clair. 2018. Racialized legal status as a social determinant of health. Social Science & Medicine 199:19–28.
Aspinall, P. J. 2003. Who is Asian? A category that remains contested in population and health research. Journal of Public Health Medicine 25(2):91–97.
Bailey, S. R., A. Saperstein, and A. M. Penner. 2014. Race, color, and income inequality across the Americas. Demographic Research 31:735–756.
Bailey, Z. D., N. Krieger, M. Agénor, J. Graves, N. Linos, and M. T. Bassett. 2017. Structural racism and health inequities in the USA: Evidence and interventions. The Lancet 389(10077):1453–1463.
Bentz, M., A. Saperstein, S. M. Fullerton, J. K. Shim, and S. S.-J. Lee. 2024. Conflating race and ancestry: Tracing decision points about population descriptors over the precision medicine research life course. Human Genetics and Genomics Advances 5(1):100243.
Bliss, C. 2012. Race Decoded: The Genomic Fight for Social Justice. Redwood City, CA: Stanford University Press.
Brandt, J. D., J. A. Beiser, M. A. Kass, and M. O. Gordon. 2001. Central corneal thickness in the ocular hypertension treatment study (OHTS). Ophthalmology 108(10):1779–1788.
Branigan, A. R., and M. Hall. 2023. Colorism in the rental housing market: Field experimental evidence of discrimination by skin color. Social Psychology Quarterly 86(3):275–297.
Braun, L. 2014. Black lungs and White lungs: The science of White supremacy in the nineteenth-century United States. In L. Braun (ed.), Breathing race into the machine: The surprising career of the spirometer from plantation to genetics. Minneapolis, MN: University of Minnesota Press.
Braun, L., A. Fausto-Sterling, D. Fullwiley, E. M. Hammonds, A. Nelson, W. Quivers, S. M. Reverby, and A. E. Shields. 2007. Racial categories in medical practice: How useful are they? PLOS Medicine 4(9):e271.
Braveman, P. A. 2003. Monitoring equity in health and healthcare: A conceptual framework. Journal of Health, Population and Nutrition 21(3):181–192.
Braveman, P. A., S. Kumanyika, J. Fielding, T. Laveist, L. N. Borrell, R. Manderscheid, and A. Troutman. 2011. Health disparities and health equity: The issue is justice. American Journal of Public Health 101(S1):S149–S155.
Brown, M. K., M. Carnoy, E. Currie, T. Duster, D. B. Oppenheimer, M. M. Shultz, and D. Well-man. 2023. Whitewashing race: The myth of a color-blind society. Oakland, CA: University of California Press.
Brown, T. H., and P. Homan. 2024. Structural racism and health stratification: Connecting theory to measurement. Journal of Health and Social Behavior 65(1):141–160.
Broyles, S. T., A. E. Staiano, K. T. Drazba, A. K. Gupta, M. Sothern, and P. T. Katzmarzyk. 2012. Elevated C-reactive protein in children from risky neighborhoods: Evidence for a stress pathway linking neighborhoods and inflammation in children. PLOS One 7(9):e45419.
Bryc, K., C. Velez, T. Karafet, A. Moreno-Estrada, A. Reynolds, A. Auton, M. Hammer, C. D. Bustamante, and H. Ostrer. 2010. Genome-wide patterns of population structure and admixture among Hispanic/Latino populations. Proceedings of the National Academy of Sciences 107(Suppl 2):8954–8961.
Bryc, K., E. Y. Durand, J. M. Macpherson, D. Reich, and J. L. Mountain. 2015. The genetic ancestry of African Americans, Latinos, and European Americans across the United States. American Journal of Human Genetics 96(1):37–53.
Budiman, A., and N. G. Ruiz. 2021. Key facts about Asian origin groups in the U.S. Pew Research Center, April 29. https://www.pewresearch.org/short-reads/2021/04/29/key-facts-about-asian-origin-groups-in-the-u-s/ (accessed August 5, 2024).
Byeon, Y. J. J., R. Islamaj, L. Yeganova, W. J. Wilbur, Z. Lu, L. C. Brody, and V. L. Bonham. 2021. Evolving use of ancestry, ethnicity, and race in genetics research—A survey spanning seven decades. American Journal of Human Genetics 108(12):2215–2223.
Cai, A., C. Dillon, W. B. Hillegass, M. Beasley, B. C. Brott, V. A. Bittner, G. J. Perry, G. V. Halade, S. D. Prabhu, and N. A. Limdi. 2019. Risk of major adverse cardiovascular events and major hemorrhage among White and Black patients undergoing percutaneous coronary intervention. Journal of the American Heart Association 8(22):e012874.
Campbell, M. E., V. M. Keith, V. Gonlin, and A. R. Carter-Sowell. 2020. Is a picture worth a thousand words? An experiment comparing observer-based skin tone measures. Race and Social Problems 12:266–278.
Carlos, R. C., S. Obeng-Gyasi, S. W. Cole, B. J. Zebrack, E. D. Pisano, M. A. Troester, L. Timsina, L. I. Wagner, J. A. Steingrimsson, I. Gareen, C. I. Lee, A. S. Adams, and C. H. Wilkins. 2022. Linking structural racism and discrimination and breast cancer outcomes: A social genomics approach. Journal of Clinical Oncology 40(13):1407–1413.
Carlson, J., B. M. Henn, D. R. Al-Hindi, and S. Ramachandran. 2022. Counter the weaponization of genetics research by extremists. Nature 610(7932):444–447.
Carter, S. E., Y. Mekawi, and N. G. Harnett. 2022. It’s about racism, not race: A call to purge oppressive practices from neuropsychiatry and scientific discovery. Neuropsychopharmacology 47(13):2179–2180.
CDC (U.S. Centers for Disease Control and Prevention). 2018a. Summary health statistics, body mass index: National Health Interview Survey. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_A-15.pdf (accessed June 26, 2024).
CDC. 2018b. Summary health statistics, respiratory diseases: National Health Interview Survey. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_A-2.pdf (accessed June 26, 2024).
CDC. 2024. Social determinants of health. https://www.cdc.gov/health-disparities-hiv-std-tb-hepatitis/about/social-determinants-of-health.html (accessed August 9, 2024).
Cerdeña, J. P., M. V. Plaisime, and J. Tsai. 2020. From race-based to race-conscious medicine: How anti-racist uprisings call us to act. The Lancet 396(10257):1125–1128.
Cerdeña, J. P., V. Grubbs, and A. L. Non. 2022a. Genomic supremacy: The harm of conflating genetic ancestry and race. Human Genomics 16(1):18.
Cerdeña, J. P., V. Grubbs, and A. L. Non. 2022b. Racialising genetic risk: Assumptions, realities, and recommendations. The Lancet 400(10368):2147–2154.
Cernat, A., J. W. Sakshaug, and J. Castillo. 2019. The impact of interviewer effects on skin color assessment in a cross-national context. International Journal of Public Opinion Research 31(4):779–793.
Chan, S. H., Y. Bylstra, J. X. Teo, J. L. Kuan, N. Bertin, M. Gonzalez-Porta, M. Hebrard, R. Tirado-Magallanes, J. H. J. Tan, J. Jeyakani, Z. Li, J. F. Chai, Y. S. Chong, S. Davila, L. L. Goh, E. S. Lee, E. Wong, T. Y. Wong, S. Prabhakar, J. Liu, C. Y. Cheng, B. Eisenhaber, N. Karnani, K. P. Leong, X. Sim, K. K. Yeo, J. C. Chambers, E. S. Tai, P. Tan, S. S. Jamuar, J. Ngeow, and W. K. Lim. 2022. Analysis of clinically relevant variants from ancestrally diverse Asian genomes. Nature Communications 13(1):6694.
Chen, E., T. Yu, G. H. Brody, P. H. Lam, B. J. Goosby, and G. E. Miller. 2023. Discrimination and inflammation in adolescents of color. Biological Psychiatry: Global Open Science 3(2):204–212.
Chen, J. M., and A. Francis-Tan. 2022. Setting the tone: An investigation of skin color bias in Asia. Race and Social Problems 14(2):150–169.
Chen, J. M., M. C. P. De Paula Couto, A. M. Sacco, and Y. Dunham. 2018. To be or not to be (Black or multiracial or white). Social Psychological and Personality Science 9(7):763–772.
Conomos, M. P., C. A. Laurie, A. M. Stilp, S. M. Gogarten, C. P. McHugh, S. C. Nelson, T. Sofer, L. Fernández-Rhodes, A. E. Justice, M. Graff, K. L. Young, A. A. Seyerle, C. L. Avery, K. D. Taylor, J. I. Rotter, G. A. Talavera, M. L. Daviglus, S. Wassertheil-Smoller, N. Schneiderman, G. Heiss, R. C. Kaplan, N. Franceschini, A. P. Reiner, J. R. Shaffer, R. G. Barr, K. F. Kerr, S. R. Browning, B. L. Browning, B. S. Weir, M. L. Avilés-Santa, G. J. Papanicolaou, T. Lumley, A. A. Szpiro, K. E. North, K. Rice, T. A. Thornton, and C. C. Laurie. 2016. Genetic diversity and association studies in U.S. Hispanic/Latino populations: Applications in the Hispanic Community Health Study/Study of Latinos. American Journal of Human Genetics 98(1):165–184.
Coop, G. 2022. Genetic similarity versus genetic ancestry groups as sample descriptors in human genetics. arXiv 2207.11595.
Davenport, L. D., S. Iyengar, and S. J. Westwood. 2022. Racial identity, group consciousness, and attitudes: A framework for assessing multiracial self-classification. American Journal of Political Science 66(3):570–586.
Davis, F. J. 2010. Who is Black?: One nation’s definition. University Park, PA: Pennsylvania State University Press.
Davis-Delano, L. R., S. L. Strother, and J. P. Gone. 2021. Perceived indicators of American Indian identity in everyday interaction: Navigating settler–colonial erasure. Ethnic and Racial Studies 45:2025–2048.
Dawes, D. E. 2020. The political determinants of health: Baltimore, MD: Johns Hopkins University Press.
Dean, L. T., and R. J. Thorpe. 2022. What structural racism is (or is not) and how to measure it: Clarity for public health and medical researchers. American Journal of Epidemiology 191(9):1521–1526.
Department of the Interior. 2014. Reaffirmation of the federal trust responsibility to federally recognized Indian tribes and individual Indian beneficiaries. https://www.doi.gov/sites/doi.gov/files/migrated/news/pressreleases/upload/Signed-SO-3335.pdf (accessed August 5, 2024).
Derbew, S. F. 2022. Untangling blackness in Greek antiquity. New York: Cambridge University Press.
Dixon, A. R., and E. E. Telles. 2017. Skin color and colorism: Global research, concepts, and measurement. Annual Review of Sociology 43(1):405–424.
Djuric, Z., C. E. Bird, A. Furumoto-Dawson, G. H. Rauscher, M. T. Ruffin Iv, R. P. Stowe, K. L. Tucker, and C. M. Masi. 2008. Biomarkers of psychological stress in health disparities research. The Open Biomarkers Journal 1(1):7–19.
Dowd, J. B., and N. Goldman. 2006. Do biomarkers of stress mediate the relation between socioeconomic status and health? Journal of Epidemiology and Community Health 60(7): 633–639.
DuBois, W. E. 2003. The health and physique of the negro American. 1906. American Journal of Public Health 93(2):272–276.
Epstein, S. 2008. Inclusion: The politics of difference in medical research. Chicago: University of Chicago Press.
Fashaw-Walters, S. A. a. M., Cydney M. 2023. Proposing a racism-conscious approach to policy making and health care practices. Health Affairs 42(10):1351–1358.
Felson, R. B. 1985. Reflected appraisal and the development of self. Social Psychology Quarterly 48(1):71–78.
Fenton, A., E. Elliott, A. Shahbandi, E. Ezenwa, C. Morris, J. McLawhorn, J. G. Jackson, P. Allen, and A. Murina. 2020. Medical students’ ability to diagnose common dermatologic conditions in skin of color. Journal of the American Academy of Dermatology 83(3):957.
Fisher, S., L. A. Wheeler, P. G. Arora, J. Chaudry, and J. Barnes-Najor. 2019. Ethnic identity and substance use in multiracial youth: The moderating role of support networks. Substance Use Misuse 54(9):1417–1428.
Fitzpatrick, T. B. 1988. The validity and practicality of sun-reactive skin types I through VI. Archives of Dermatology 124(6):869–871.
Fletcher, M. L. M. 2014. A short history of Indian law in the Supreme Court. https://www.americanbar.org/groups/crsj/publications/human_rights_magazine_home/2014_vol_40/vol--40-no--1--tribal-sovereignty/short_history_of_indian_law/ (accessed August 26, 2024).
Ford, C. L., and N. T. Harawa. 2010. A new conceptualization of ethnicity for social epidemiologic and health equity research. Social Science & Medicine 71(2):251–258.
Fortes-Lima, C., J. Bybjerg-Grauholm, L. C. Marin-Padrón, E. J. Gomez-Cabezas, M. BækvadHansen, C. S. Hansen, P. Le, D. M. Hougaard, P. Verdu, O. Mors, E. J. Parra, and B. Marcheco-Teruel. 2018. Exploring Cuba’s population structure and demographic history using genome-wide data. Science Reports 8(1):11422.
Franco, M., M. Durkee, and S. McElroy-Heltzel. 2021. Discrimination comes in layers: Dimensions of discrimination and mental health for multiracial people. Cultural Diversity and Ethnic Minority Psychology 27(3):343–353.
Frost, P. 1990. Fair women, dark men: The forgotten roots of colour prejudice. History of European Ideas 12(5):669–679.
Gallagher, M., K. Marcussen, and R. T. Serpe. 2022. Multiple identities and sources of reflected appraisals in identity theory. Social Psychology Quarterly 85(2):142–163.
Garroutte, E. M. 2003. Real Indians: Identity and the survival of Native America. Berkeley, CA: University of California Press.
Gartner, D. R., C. Maples, M. Nash, and H. Howard-Bobiwash. 2023. Misracialization of Indigenous people in population health and mortality studies: A scoping review to establish promising practices. Epidemiologic Reviews 45(1):63–81.
Gee, G. C., and C. L. Ford. 2011. Structural racism and health inequities: Old issues, new directions. Du Bois Review: Social Science Research on Race 8(1):115–132.
GenomeAsia100K Consortium. 2019. The GenomeAsia 100k project enables genetic discoveries across Asia. Nature 576(7785):106–111.
Geronimus, A. T. 1992. The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity and Disease 2(3):207–221.
Geronimus, A. T., M. Hicken, D. Keene, and J. Bound. 2006. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health 96(5):826–833.
Glenn, E. N. 2008. Yearning for lightness. Gender & Society 22(3):281–302.
Goldstein, J. R., and A. J. Morning. 2000. The multiple-race population of the United States: Issues and estimates. Proceedings of the National Academy of Sciences 97(11):6230–6235.
Gordon, R. A., A. R. Branigan, M. A. Khan, and J. G. Nunez. 2022. Measuring skin color: Consistency, comparability, and meaningfulness of rating scale scores and handheld device readings. Journal of Survey Statistics and Methodology 10(2):337–364.
Gouveia, M. H., V. Borda, T. P. Leal, R. G. Moreira, A. W. Bergen, F. S. G. Kehdy, I. Alvim, M. M. Aquino, G. S. Araujo, N. M. Araujo, V. Furlan, R. Liboredo, M. Machado, W. C. S. Magalhaes, L. A. Michelin, M. R. Rodrigues, F. Rodrigues-Soares, H. P. Sant Anna, M. L. Santolalla, M. O. Scliar, G. Soares-Souza, R. Zamudio, C. Zolini, M. C. Bortolini, M. Dean, R. H. Gilman, H. Guio, J. Rocha, A. C. Pereira, M. L. Barreto, B. L. Horta, M. F. Lima-Costa, S. M. Mbulaiteye, S. J. Chanock, S. A. Tishkoff, M. Yeager, and E. TarazonaSantos. 2020. Origins, admixture dynamics, and homogenization of the African gene pool in the Americas. Molecular Biology and Evolution 37(6):1647–1656.
Gravlee, C. C., and W. W. Dressler. 2005. Skin pigmentation, self-perceived color, and arterial blood pressure in Puerto Rico. American Journal of Human Biology 17(2):195–206.
Green, J. D., and S. Work. 1976. Comment: Inherent Indian sovereignty. American Indian Law Review 4(2):311–342.
Guidi, J., M. Lucente, N. Sonino, and Giovanni. 2021. Allostatic load and its impact on health: A systematic review. Psychotherapy and Psychosomatics 90(1):11–27.
Guluma, B., and A. Saperstein. 2022. Consistent divisions or methodological decisions? Assessing the U.S. racial hierarchy across outcomes. Race and Social Problems 14(3):189–207.
Hahn, R. A., J. Mulinare, and S. M. Teutsch. 1992. Inconsistencies in coding of race and ethnicity between birth and death in U.S. infants: A new look at infant mortality, 1983 through 1985. JAMA 267(2):259–263.
Halbert, C. H., and C. G. Allen. 2021. Basic behavioral science research priorities in minority health and health disparities. Translational Behavioral Medicine 11(11):2033–2042.
Han, J. 2020. Does skin tone matter? Immigrant mobility in the U.S. labor market. Demography 57(2):705–726.
Hannon, L., and R. Defina. 2020. The reliability of same-race and cross-race skin tone judgments. Race and Social Problems 12(2):186–194.
Hardeman, R. R., P. A. Homan, T. Chantarat, B. A. Davis, and T. H. Brown. 2022. Improving the measurement of structural racism to achieve antiracist health policy. Health Affairs 41(2):179–186.
Harris, D. R., and J. J. Sim. 2002. Who is multiracial? Assessing the complexity of lived race. American Sociological Review 67(4):614–627.
Harris, J. C. 2016. Toward a critical multiracial theory in education. International Journal of Qualitative Studies in Education 29(6):795–813.
Hatch, A. R. 2016. Blood sugar: Racial pharmacology and food justice in Black America. Minneapolis, MN: University of Minnesota Press.
Heldreth, C. M., E. P. Monk, A. T. Clark, C. Schumann, X. Eyee, and S. Ricco. 2024. Which skin tone measures are the most inclusive? An investigation of skin tone measures for artificial intelligence. ACM Journal on Responsible Computing 1(1):1–21.
Hernandez-Boussard, T., S. M. Siddique, A. S. Bierman, M. Hightower, and H. Burstin. 2023. Promoting equity in clinical decision making: Dismantling race-based medicine: Commentary examines promoting equity in clinical decision-making. Health Affairs 42(10):1369–1373.
HHS (U.S. Department of Health and Human Services). 2021. History of Healthy People. https://health.gov/our-work/healthy-people/about-healthy-people/history-healthy-people (accessed April 1, 2024).
HHS and OASH (Office of the Assistant Secretary for Health). 2024. Social determinants of health. https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed August 9, 2024).
Homburger, J. R., A. Moreno-Estrada, C. R. Gignoux, D. Nelson, E. Sanchez, P. Ortiz-Tello, B. A. Pons-Estel, E. Acevedo-Vasquez, P. Miranda, C. D. Langefeld, S. Gravel, M. E. Alarcón-Riquelme, and C. D. Bustamante. 2015. Genomic insights into the ancestry and demographic history of South America. PLOS Genetics 11(12):e1005602.
Howell, J., and M. O. Emerson. 2017. So what “should” we use? Evaluating the impact of five racial measures on markers of social inequality. Sociology of Race and Ethnicity 3(1):14–30.
Hunter, M. 2007. The persistent problem of colorism: Skin tone, status, and inequality. Sociology Compass 1(1):237–254.
Huyser, K. R., and S. Locklear. 2023. Reversing statistical erasure of Indigenous peoples: The social construction of American Indians and Alaska Natives in the United States using national data sets. In M. Walter, T. Kukutai, A. A. Gonzales, and R. Henry (eds.), The Oxford Handbook of Indigenous Sociology. New York: Oxford University Press. Pp. 247–262.
Hyman, G. F., and J. R. Mehta. 2004. The association of central corneal thickness and ethnicity. Investigative Ophthalmology & Visual Science 45(13):4493–4493.
IGSR (International Genome Sample Resource). 2024. The International Genome Sample Resource. https://www.internationalgenome.org/ (accessed April 18, 2024).
IOM (Institute of Medicine). 2003. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
Iverson, S., A. Morning, A. Saperstein, and J. Xu. 2022. Regimes beyond the one-drop rule: New models of multiracial identity. Genealogy 6(2):57.
Iwamoto, D. K., and W. M. Liu. 2010. The impact of racial identity, ethnic identity, Asian values and race-related stress on Asian Americans and Asian international college students’ psychological well-being. Journal of Counseling Psychology 57(1):79–91.
Iyer, H. S., J. E. Hart, P. James, E. G. Elliott, N. V. Deville, M. D. Holmes, I. De Vivo, L. A. Mucci, F. Laden, and T. R. Rebbeck. 2022. Impact of neighborhood socioeconomic status, income segregation, and greenness on blood biomarkers of inflammation. Environment International 162:107164.
Jablonski, N. G. 2004. The evolution of human skin and skin color. Annual Review of Anthropology 33(1):585–623.
Jablonski, N. G. 2012. Living color: The biological and social meaning of skin color. Berkeley, CA: University of California Press.
Jablonski, N. G. 2021. Skin color and race. American Journal of Physical Anthropology 175(2):437–447.
Jablonski, N. G., and G. Chaplin. 2000. The evolution of human skin coloration. Journal of Human Evolution 39(1):57–106.
Jablonski, N. G., and G. Chaplin. 2010. Human skin pigmentation as an adaptation to UV radiation. Proceedings of the National Academy of Sciences 107(Suppl 2):8962–8968.
Jackson, K. F. 2023. A critical scoping review of mental health and wellbeing research with multiracial subsamples 2012–2022. Journal of Racial and Ethnic Health Disparities. https://doi.org/10.1007/s40615-023-01811-2 [online ahead of print].
Jahn, J. L. 2022. Comparing approaches to measuring structural racism. American Journal of Epidemiology 191(4):548–551.
Jahn, J. L., D. Zubizarreta, J. T. Chen, B. L. Needham, G. Samari, A. J. McGregor, M. D. Douglas, S. B. Austin, and M. Agénor. 2023. Legislating inequity: Structural racism in groups of state laws and associations with premature mortality rates. Health Affairs (Millwood) 42(10):1325–1333.
Jarrín, O. F., A. N. Nyandege, I. B. Grafova, X. Dong, and H. Lin. 2020. Validity of race and ethnicity codes in Medicare administrative data compared with gold-standard self-reported race collected during routine home health care visits. Medical Care 58(1):e1–e8.
Jim, M. A., E. Arias, D. S. Seneca, M. J. Hoopes, C. C. Jim, N. J. Johnson, and C. L. Wiggins. 2014. Racial misclassification of American Indians and Alaska Natives by Indian Health Service contract health service delivery area. American Journal of Public Health 104(S3):S295–S302.
Johfre, S. S., and A. Saperstein. 2019. Racial and gender identities. Pathways Magazine, special issue. https://inequality.stanford.edu/sites/default/files/Pathways_SOTU_2019_RaceGender.pdf (accessed August 5, 2024).
Johfre, S. S., A. Saperstein, and J. A. Hollenbach. 2021. Measuring race and ancestry in the age of genetic testing. Demography 58(3):785–810.
Johnson, A. L., C. Levesque, N. A. Lewis, Jr., and A. L. Asad. 2024. Deportation threat predicts Latino U.S. citizens and noncitizens’ psychological distress, 2011 to 2018. Proceedings of the National Academy of Sciences 121(9):e2306554121.
Jones, C. P., B. I. Truman, L. D. Elam-Evans, C. A. Jones, C. Y. Jones, R. Jiles, S. F. Rumisha, and G. S. Perry. 2008. Using “socially assigned race” to probe White advantages in health status. Ethnicity & Disease 18(4):496–504.
Katz, T. K., T. Regev, S. Lavie, H. Porat, and R. Avraham. 2020. Those who tan and those who don’t: A natural experiment on colorism. PLOS One 15(7):e0235438.
Kaufman, J. S. 1999. How inconsistencies in racial classification demystify the race construct in public health statistics. Epidemiology 10(2):101–103.
Kautz, M. M., B. A. McArthur, D. P. Moriarity, L. M. Ellman, J. Klugman, C. L. Coe, L. Y. Abramson, and L. B. Alloy. 2023. The impact of early and recent life stress on trajectories of inflammatory biomarkers in a diverse sample of adolescents. Research on Child and Adolescent Psychopathology 51(12):1883–1894.
Keith, V. M., and C. Herring. 1991. Skin tone and stratification in the Black community. American Journal of Sociology 97(3):760–778.
Khan, M. A., H. Nguyen, A. R. Branigan, and R. A. Gordon. 2023. How well do contemporary and historical skin color rating scales cover the lightness-to-darkness continuum? Descriptive results from color science and diverse rating pools. Research in Human Development 20(3–4):1–17.
Khazanchi, R., D. R. Soled, and R. Yearby. 2023. Racism-conscious praxis: A framework to materialize anti-oppression in medicine, public health, and health policy. The American Journal of Bioethics 23(4):31–34.
Kochhar, R., and A. Cilluffo. 2018. Income inequality in the U.S. is rising most rapidly among Asians. Pew Research Center, July 12. https://www.pewresearch.org/social-trends/2018/07/12/income-inequality-in-the-u-s-is-rising-most-rapidly-among-asians/ (accessed August 5, 2024).
Kressin, N. R., B. H. Chang, A. Hendricks, and L. E. Kazis. 2003. Agreement between administrative data and patients’ self-reports of race/ethnicity. American Journal of Public Health 93(10):1734–1739.
Krieger, N. 1999. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services 29(2):295–352.
Kuehn, B. M. 2024. Citing harms, momentum grows to remove race from clinical algorithms. JAMA 331(6):463–465.
Laidley, T., B. Domingue, P. Sinsub, K. M. Harris, and D. Conley. 2019. New evidence of skin color bias and health outcomes using sibling difference models: A research note. Demography 56(2):753–762.
Lam, P. H., J. J. Chiang, E. Chen, and G. E. Miller. 2021. Race, socioeconomic status, and low-grade inflammatory biomarkers across the lifecourse: A pooled analysis of seven studies. Psychoneuroendocrinology 123:104917.
Lam-Hine, T., S. Forthal, C. Y. Johnson, and H. B. Chin. 2024. Asking multicrit questions: A reflexive and critical framework to promote health data equity for the multiracial population. Milbank Quarterly 102(2):398–428.
Lawrence, J. A., I. Kawachi, K. White, M. T. Bassett, N. Priest, J. G. Masunga, H. J. Cory, C. Mita, and D. R. Williams. 2022. A systematic review and meta-analysis of the everyday discrimination scale and biomarker outcomes. Psychoneuroendocrinology 142:105772.
Lee, J., and K. Ramakrishnan. 2020. Who counts as Asian? Ethnic and Racial Studies 43(10):1733–1756.
Lewis, A. C. F., S. J. Molina, P. S. Appelbaum, B. Dauda, A. Fuentes, S. M. Fullerton, N. A. Garrison, N. Ghosh, R. C. Green, E. M. Hammonds, J. M. Jeff, D. S. Jones, E. E. Kenny, P. Kraft, M. Mauro, A. P. S. Ori, A. Panofsky, M. Sohail, B. M. Neale, and D. S. Allen. 2023. An ethical framework for research using genetic ancestry. Perspectives in Biology and Medicine 66(2):225–248.
Liebler, C. A. 2010. Homelands and Indigenous identities in a multiracial era. Social Science Research 39(4):596–609.
Liebler, C. A. 2018. Counting America’s first peoples. Annals of the American Academy of Political and Social Science 677(1):180–190.
Liebler, C. A., R. Bhaskar, and S. R. Porter 2016. Joining, leaving, and staying in the American Indian/Alaska Native race category between 2000 and 2010. Demography 53(2):507–540.
Liguori, I., G. Russo, F. Curcio, G. Bulli, L. Aran, D. Della-Morte, G. Gargiulo, G. Testa, F. Cacciatore, D. Bonaduce, and P. Abete. 2018. Oxidative stress, aging, and diseases. Clinical Interventions in Aging 13:757–772.
Lo Wang, H. 2021. The census has revealed a more multiracial U.S. One reason? Cheaper DNA tests. https://www.npr.org/2021/08/28/1030139666/2020-census-results-data-race-multiracial-dna-ancestry-test-mixed-biracial (accessed June 26, 2024).
Martschenko, D. O., H. Wand, J. L. Young, and G. L. Wojcik. 2023. Including multiracial individuals is crucial for race, ethnicity and ancestry frameworks in genetics and genomics. Nature Genetics 55(6):895–900.
Massey, D. S., and J. A. Martin. 2003. The NIS skin color scale. https://nis.princeton.edu/downloads/nis-skin-color-scale.pdf (accessed August 5, 2024).
Mathias, R. A., M. A. Taub, C. R. Gignoux, W. Fu, S. Musharoff, T. D. O’Connor, C. Vergara, D. G. Torgerson, M. Pino-Yanes, S. S. Shringarpure, L. Huang, N. Rafaels, M. P. Boorgula, H. R. Johnston, V. E. Ortega, A. M. Levin, W. Song, R. Torres, B. Padhukasahasram, C. Eng, D. A. Mejia-Mejia, T. Ferguson, Z. S. Qin, A. F. Scott, M. Yazdanbakhsh, J. G. Wilson, J. Marrugo, L. A. Lange, R. Kumar, P. C. Avila, L. K. Williams, H. Watson, L. B. Ware, C. Olopade, O. Olopade, R. Oliveira, C. Ober, D. L. Nicolae, D. Meyers, A. Mayorga, J. Knight-Madden, T. Hartert, N. N. Hansel, M. G. Foreman, J. G. Ford, M. U. Faruque, G. M. Dunston, L. Caraballo, E. G. Burchard, E. Bleecker, M. I. Araujo, E. F. Herrera-Paz, K. Gietzen, W. E. Grus, M. Bamshad, C. D. Bustamante, E. E. Kenny, R. D. Hernandez, T. H. Beaty, I. Ruczinski, J. Akey, and K. C. Barnes. 2016. A continuum of admixture in the Western hemisphere revealed by the African diaspora genome. Nature Communications 7:12522.
Mathieson, I., and A. Scally. 2020. What is ancestry? PLOS Genetics 16(3):e1008624.
Mays, V. M., N. A. Ponce, D. L. Washington, and S. D. Cochran. 2003. Classification of race and ethnicity: Implications for public health. Annual Reviews of Public Health 24:83–110.
McArdle, C. E., H. Bokhari, C. C. Rodell, V. Buchanan, L. K. Preudhomme, C. R. Isasi, M. Graff, K. North, L. C. Gallo, A. Pirzada, M. L. Daviglus, G. Wojcik, J. Cai, K. Perreira, and L. Fernandez-Rhodes. 2021. Findings from the Hispanic community health study/study of Latinos on the importance of sociocultural environmental interactors: Polygenic risk score-by-immigration and dietary interactions. Frontier Genetics 12:720750.
McClendon, J., K. Chang, M. J. Boudreaux, T. F. Oltmanns, and R. Bogdan. 2021. Black–white racial health disparities in inflammation and physical health: Cumulative stress, social isolation, and health behaviors. Psychoneuroendocrinology 131:105251.
McNamee, L. 2020. Colonial legacies and comparative racial identification in the Americas. American Journal of Sociology 126(2):318–353.
Merrick, M. T., D. C. Ford, K. A. Ports, and A. S. Guinn. 2018. Prevalence of adverse childhood experiences from the 2011–2014 Behavioral Risk Factor Surveillance System in 23 states. JAMA Pediatrics 172(11):1038–1044.
Monk Jr., E. P. 2015. The cost of color: Skin color, discrimination, and health among African-Americans. American Journal of Sociology 121(2):396–444.
Monk Jr., E. P. 2021. The unceasing significance of colorism: Skin tone stratification in the United States. Daedalus 150(2):76–90.
Monk Jr., E. P. 2023. The Monk skin tone scale. SocArXiv, 4 May. https://osf.io/preprints/socarxiv/pdf4c (accessed August 5, 2024).
Moreno-Estrada, A., S. Gravel, F. Zakharia, J. L. McCauley, J. K. Byrnes, C. R. Gignoux, P. A. Ortiz-Tello, R. J. Martínez, D. J. Hedges, R. W. Morris, C. Eng, K. Sandoval, S. Acevedo-Acevedo, P. J. Norman, Z. Layrisse, P. Parham, J. C. Martínez-Cruzado, E. G. Burchard, M. L. Cuccaro, E. R. Martin, and C. D. Bustamante. 2013. Reconstructing the population genetic history of the Caribbean. PLOS Genetics 9(11):e1003925.
Moreno-Estrada, A., C. R. Gignoux, J. C. Fernández-López, F. Zakharia, M. Sikora, A. V. Contreras, V. Acuña-Alonzo, K. Sandoval, C. Eng, S. Romero-Hidalgo, P. Ortiz-Tello, V. Robles, E. E. Kenny, I. Nuño-Arana, R. Barquera-Lozano, G. Macín-Pérez, J. Granados-Arriola, S. Huntsman, J. M. Galanter, M. Via, J. G. Ford, R. Chapela, W. Rodriguez-Cintron, J. R. Rodríguez-Santana, I. Romieu, J. J. Sienra-Monge, B. del Rio Navarro, S. J. London, A. Ruiz-Linares, R. Garcia-Herrera, K. Estrada, A. Hidalgo-Miranda, G. Jimenez-Sanchez, A. Carnevale, X. Soberón, S. Canizales-Quinteros, H. Rangel-Villalobos, I. Silva-Zolezzi, E. G. Burchard, and C. D. Bustamante. 2014. Human genetics. The genetics of Mexico recapitulates Native American substructure and affects biomedical traits. Science 344(6189):1280–1285.
Morning, A., and D. Sabbagh. 2005. From sword to plowshare: Using race for discrimination and antidiscrimination in the United States. International Social Science Journal 57(183):57–73.
Morning, A., and A. Saperstein. 2018. The generational locus of multiraciality and its implications for racial self-identification. Annals of the American Academy of Political and Social Science 677(1):57–68.
Moscou, S., and S. Baker. 2018. The role of race in clinical decision making. The Nurse Practitioner 43(3):41–46.
Muscatell, K. A., S. N. Brosso, and K. L. Humphreys. 2020. Socioeconomic status and inflammation: A meta-analysis. Molecular Psychiatry 25(9):2189–2199.
Nagel, J. 1995. American Indian ethnic renewal: Politics and the resurgence of identity. American Sociological Review 60(6):947–965.
Nalven, T., N. S. Spillane, and J. S. Rossi. 2021. Racial discrimination, racial identity affiliation, and heavy alcohol use among multiracial individuals. Alcoholism: Clinical and Experimental Research 45(8):1653–1663.
Nandi, A., and L. Platt. 2009. Developing ethnic identity questions for Understanding Society, the UK household longitudinal study. Essex, UK: University of Essex.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2023. Using population descriptors in genetics and genomics research: A new framework for an evolving field. Washington, DC: The National Academies Press.
NASEM. 2024. Unequal treatment revisited: The current state of racial and ethnic disparities in health care: Proceedings of a workshop. Washington, DC: The National Academies Press.
National Archives and Records Administration. 2016. Dawes rolls. https://www.archives.gov/research/native-americans/dawes/tutorial/intro.html (accessed June 26, 2024).
Neblett, Jr., E. W., D. Rivas-Drake, and A. J. Umaña-Taylor. 2012. The promise of racial and ethnic protective factors in promoting ethnic minority youth development. Child Development Perspectives 6(3):295–303.
NIH (National Institutes of Health). 2001. NIH policy on reporting race and ethnicity data: Subjects in clinical research. https://grants.nih.gov/grants/guide/notice-files/not-od-01-053.html (accessed July 3, 2024).
Noe-Bustamante, L., Gonzalez-Barrera, A., Edwards, K., Mora, L., Hugo Lopez, M. 2021. Measuring the racial identity of Latinos. Pew Research Center. https://www.pewresearch.org/race-and-ethnicity/2021/11/04/measuring-the-racial-identity-of-latinos/ (accessed August 5, 2024).
Noren Hooten, N., N. L. Pacheco, J. T. Smith, and M. K. Evans. 2022. The accelerated aging phenotype: The role of race and social determinants of health on aging. Ageing Research Reviews 73:101536.
Norton, H. L., R. A. Kittles, E. Parra, P. McKeigue, X. Mao, K. Cheng, V. A. Canfield, D. G. Bradley, B. McEvoy, and M. D. Shriver. 2006. Genetic evidence for the convergent evolution of light skin in Europeans and East Asians. Molecular Biology and Evolution 24(3):710–722.
Okah, E., J. Thomas, A. Westby, and B. Cunningham. 2022. Colorblind Racial Ideology and Physician Use of Race in Medical Decision-Making. Journal of Racial and Ethnic Health Disparities 9(5):2019–2026.
Olufadeji, A., N. M. Dubosh, and A. Landry. 2021. Guidelines on the use of race as patient identifiers in clinical presentations. Journal of the National Medical Association 113(4):428–430.
OMB (U.S. Office of Management and Budget). 1977. Directive No. 15: Race and ethnic standards for federal statistics and administrative reporting. https://spd15revision.gov/content/spd15revision/en/history/1977-standards.html (accessed January 8, 2025).
OMB. 1997. Revisions to the standards for the classification of federal data on race and ethnicity. https://obamawhitehouse.archives.gov/omb/fedreg_1997standards (accessed August 5, 2024).
OMB. 2024. Revisions to OMB’s Statistical Policy Directive No. 15: Standards for maintaining, collecting, and presenting federal data on race and ethnicity. Federal Register. https://www.federalregister.gov/documents/2024/03/29/2024-06469/revisions-to-ombs-statistical-policy-directive-no-15-standards-for-maintaining-collecting-and (accessed August 5, 2024).
OMH (Office of Minority Health). 2024. Explanation of data standards for race, ethnicity, sex, primary language, and disability. https://minorityhealth.hhs.gov/explanation-data-standards-race-ethnicity-sex-primary-language-and-disability#top (accessed July 10, 2024).
Ostfeld, M. C., and N. D. Yadon. 2022. ¿Mejorando la raza?: The political undertones of Latinos’ skin color in the United States. Social Forces 100(4):1806–1832.
Patten, E. 2015. Who is multiracial? Depends on how you ask. https://www.pewresearch.org/social-trends/2015/11/06/who-is-multiracial-depends-on-how-you-ask/ (accessed June 26, 2024).
Pauker, K., C. Meyers, D. T. Sanchez, S. E. Gaither, and D. M. Young. 2018. A review of multiracial malleability: Identity, categorization, and shifting racial attitudes. Social and Personality Psychology Compass 12(6):e12392.
Penner, A. M., and A. Saperstein. 2015. Disentangling the effects of racial self-identification and classification by others: The case of arrest. Demography 52(3):1017–1024.
Perreira, K. M., and J. M. Pedroza. 2019. Policies of exclusion: Implications for the health of immigrants and their children. Annual Review of Public Health 40:147–166.
Phelan, J. C., B. G. Link, S. Zelner, and L. H. Yang. 2014. Direct-to-consumer racial admixture tests and beliefs about essential racial differences. Social Psychology Quarterly 77(3):296–318.
Phillips, E. M., A. O. Odunlami, and V. L. Bonham. 2007. Mixed race: Understanding difference in the genome era. Social Forces 86(2):795–820.
Piña, R., R. Alejandro, and C. Ma. 2023. Classification algorithm for skin color (CASCo): A new tool to measure skin color in social science research. Social Science Quarterly 104(2):168–179.
Reynolds, L. 2021. Measuring race and ethnicity with the 2020 census redistricting data. Cornell Program on Applied Demographics.
Rhoades, D. A. 2005. Racial misclassification and disparities in cardiovascular disease among American Indians and Alaska Natives. Circulation 111(10):1250–1256.
Rodriguez-Lonebear, D. 2021. The blood line: Racialized boundary making and citizenship among native nations. Sociology of Race and Ethnicity 7(4):527–542.
Roth, W. D. 2016. The multiple dimensions of race. Ethnic and Racial Studies 39(8):1310–1338.
Royal, C. D., J. Novembre, S. M. Fullerton, D. B. Goldstein, J. C. Long, M. J. Bamshad, and A. G. Clark. 2010. Inferring genetic ancestry: Opportunities, challenges, and implications. American Journal of Human Genetics 86(5):661–673.
Samari, G., A. Nagle, and K. Coleman-Minahan. 2021. Measuring structural xenophobia: US state immigration policy climates over ten years. SSM - Population Health 16:100938.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2021. Highlights by race/ethnicity for the 2021 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/2022-12/2021NSDUHFFRHighlightsRE123022.pdf (accessed June 26, 2024).
Sanchez, D. T. 2010. How do forced-choice dilemmas affect multiracial people? The role of identity autonomy and public regard in depressive symptoms. Journal of Applied Social Psychology 40(7):1657–1677.
Saperstein, A. 2006. Double-checking the race box: Examining inconsistency between survey measures of observed and self-reported race. Social Forces 85(1):57–74.
Saperstein, A. 2012. Capturing complexity in the United States: Which aspects of race matter and when? Ethnic and Racial Studies 35(8):1484–1502.
Saperstein, A., J. M. Kizer, and A. M. Penner. 2016. Making the most of multiple measures. American Behavioral Scientist 60(4):519–537.
Scanlon, P. D., and M. D. Shriver. 2010. “Race correction” in pulmonary-function testing. New England Journal of Medicine 363(4):385–386.
Schroeder, H., M. C. Ávila-Arcos, A. S. Malaspinas, G. D. Poznik, M. Sandoval-Velasco, M. L. Carpenter, J. V. Moreno-Mayar, M. Sikora, P. L. Johnson, M. E. Allentoft, J. A. Samaniego, J. B. Haviser, M. W. Dee, T. W. Stafford, Jr., A. Salas, L. Orlando, E. Willerslev, C. D. Bustamante, and M. T. Gilbert. 2015. Genome-wide ancestry of 17th-century enslaved Africans from the Caribbean. Proceedings of the National Academy of Sciences 112(12):3669–3673.
Shalley, F., K. Griffiths, and T. Wilson. 2023. No longer Indigenous. Population Research and Policy Review 42(4):53.
Shiao, J. L. 2019. When (in)consistency matters: Racial identification and specification. Socius 5:2378023119848268.
Simons, R. L., M.-K. Lei, S. R. H. Beach, A. B. Barr, L. G. Simons, F. X. Gibbons, and R. A. Philibert. 2018. Discrimination, segregation, and chronic inflammation: Testing the weathering explanation for the poor health of Black Americans. Developmental Psychology 54(10): 1993–2006.
Sjoding, M. W., R. P. Dickson, T. J. Iwashyna, S. E. Gay, and T. S. Valley. 2020. Racial bias in pulse oximetry measurement. New England Journal of Medicine 383(25):2477–2478.
Snipp, C. M. 1986. Who are American Indians? Some observations about the perils and pitfalls of data for race and ethnicity. Population Research and Policy Review 5(3):237–252.
Snipp, C. M. 2003. Racial measurement in the American census: Past practices and implications for the future. Annual Review of Sociology 29(1):563–588.
Snowden, F. M. 1983. Before color prejudice: The ancient view of blacks. Cambridge, MA: Harvard University Press.
Solís, P., B. Güémez, and R. M. Campos-Vázquez. 2023. Skin tone and inequality of socioeconomic outcomes in Mexico: A comparative analysis using optical colorimeters and color palettes. Sociology of Race and Ethnicity. https://doi.org/10.1177/23326492231217232.
Solomon, T. G. A., R. R. B. Starks, A. Attakai, F. Molina, F. Cordova-Marks, M. Kahn-John, C. L. Antone, M. Flores, and F. Garcia. 2022. The generational impact of racism on health: Voices from American Indian communities. Health Affairs 41(2):281–288.
Sosina, V. E., and A. Saperstein. 2022. Reflecting race and status: The dynamics of material hardship and how people are perceived. Socius 8:23780231221124578.
Stepanikova, I. 2010. Applying a status perspective to racial/ethnic misclassification: Implications for health. Advances in Group Processes 27:159–183.
Stepanikova, I., and G. R. Oates. 2016. Dimensions of racial identity and perceived discrimination in health care. Ethnicity & Disease 26(4):501–512.
Stewart, Q. T., R. J. Cobb, and V. M. Keith. 2020. The color of death: Race, observed skin tone, and all-cause mortality in the United States. Ethnicity & Health 25(7):1018–1040.
Sweet, E., T. W. McDade, C. I. Kiefe, and K. Liu. 2007. Relationships between skin color, income, and blood pressure among African Americans in the CARDIA study. American Journal of Public Health 97(12):2253–2259.
Swilley-Martinez, M. E., S. A. Coles, V. E. Miller, I. Z. Alam, K. V. Fitch, T. H. Cruz, B. Hohl, R. Murray, and S. I. Ranapurwala. 2023. “We adjusted for race”: Now what? A systematic review of utilization and reporting of race in American Journal of Epidemiology and Epidemiology, 2020–2021. Epidemiologic Reviews 45(1):15–31.
Szanton, S. L., S. E. LaFave, and R. J. Thorpe Jr. 2022. Structural racial discrimination and structural resilience: Measurement precedes change. New York: Oxford University Press.
Tavernise, S., T. Mzezewa, and A. G. Heyward. 2021. Behind the surprising jump in multiracial Americans, several theories. The New York Times, August 13. https://www.nytimes.com/2021/08/13/us/census-multiracial-identity.html (accessed August 5, 2024).
Telles, E. 2014. Pigmentocracies: Ethnicity, race, and color in Latin America. Chapel Hill, NC: University of North Carolina Press.
Telles, E. E., and N. Lim. 1998. Does it matter who answers the race question? Racial classification and income inequality in Brazil. Demography 35(4):465–474.
Thorpe Jr, R. J., K. C. Norris, B. M. Beech, and M. A. Bruce. 2019. Racism across the life course. In C. L. Ford, D. M. Griffith, Marino A. Bruce, and K. L. Gilbert (eds.), Racism: Science & tools for the public health professional. Washington, DC: APHA Press.
Tian, C., R. Kosoy, A. Lee, M. Ransom, J. W. Belmont, P. K. Gregersen, and M. F. Seldin. 2008. Analysis of east Asia genetic substructure using genome-wide SNP arrays. PLOS One 3(12):e3862.
Tipton, K., B. F. Leas, E. Flores, C. Jepson, J. Aysola, J. Cohen, M. Harhay, H. Schmidt, G. Weissman, J. Treadwell, N. K. Mull, and S. M. Siddique. 2023. Impact of healthcare algorithms on racial and ethnic disparities in health and healthcare. Comparative Effectiveness Review no. 268. Rockville, MD: Agency for Healthcare Research and Quality.
U.S. Census Bureau. 2001. Overview of race and Hispanic origin: Census 2000 brief. https://www2.census.gov/library/publications/decennial/2000/briefs/c2kbr01-01.pdf (accessed July 10, 2024).
U.S. Census Bureau. 2021. 2020 census illuminates racial and ethnic composition of the country. https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html (accessed July 11, 2024).
U.S. Census Bureau. 2023. 2020 census shows increase in multiracial population in all age categories. https://www.census.gov/library/stories/2023/06/nearly-a-third-reporting-two-or-more-races-under-18-in-2020.html (accessed July 11, 2024).
Umaña-Taylor, A. J., and N. Shin. 2007. An examination of ethnic identity and self-esteem with diverse populations: Exploring variation by ethnicity and geography. Cultural Diversity and Ethnic Minority Psychology 13(2):178–186.
Urban Institute. 2023. Measuring structural racism: Approaches from the health literature. Washington, DC: Urban Institute. https://www.urban.org/research/publication/measuring-structural-racism (accessed August 5, 2024).
Van Natta, M., N. Burkeb, I. Yen, M. Fleming, C. Hanssmann, M. Rasidjan, and J. Shim. 2018. Stratified citizenship, stratified health: Examining Latinx legal status in the U.S. healthcare safety net. Social Science & Medicine 220:49–55.
Vargas, N., and J. Kingsbury. 2016. Racial identity contestation: Mapping and measuring racial boundaries. Sociology Compass 10(8):718–729.
Verkruysse, W., M. B. Jaffe, M. Lipnick, and C. Zemouri. 2024. Challenges of subjective skin color scales: The case for the use of objective pigmentation measurement methods in regulatory pulse oximetry studies. Anesthesia & Analgesia 139(2):e15–e17.
Vinluan, A. C., and J. D. Remedios. 2020. Who do multiracials consider part of their racial in-group? Social Psychological and Personality Science 11(4):522–532.
Viruell-Fuentes, E. A., P. Y. Miranda, and S. Abdulrahim. 2012. More than culture: Structural racism, intersectionality theory, and immigrant health. Social Science and Medicine 75(12):2099–2106.
Vyas, D. A., L. G. Eisenstein, and D. S. Jones. 2020. Hidden in plain sight—Reconsidering the use of race correction in clinical algorithms. New England Journal of Medicine 383(9):874–882.
Wallman, K., S. Evinger, and S. Schechter. 2000. Measuring our nation’s diversity: Developing a common language for data on race/ethnicity. American Journal of Public Health 90:1704–1708.
Wang, K. 2024. Data justice and community-engagement: the collection and use of race and ethnicity data in the EHR. Presentation at Committee on the Use of Race and Ethnicity in Biomedical Research Meeting #3. January 31, 2024.
Wang, S. Y., R. Melles, and S. C. Lin. 2014. The impact of central corneal thickness on the risk for glaucoma in a large multiethnic population. Journal of Glaucoma 23(9):606–612.
Ware, O. R., J. E. Dawson, M. M. Shinohara, and S. C. Taylor. 2020. Racial limitations of Fitzpatrick skin type. Cutis 105(2):77–80.
Weinreb, C., and D. S. Sun. 2023. To dismantle structural racism in science, scientists need to learn how it works. Neuropsychopharmacology 48(4):579–582.
White, K. 2011. The sustaining relevance of W. E. B. Dubois to health disparities research. Du Bois Review: Social Science Research on Race 8(1):285–293.
WHO (World Health Organization). 2008. Closing the gap in a generation: Health equity through action on the social determinants of health: Commission on social determinants of health final report. Geneva: World Health Organization.
Wight, V. R., Michelle Chau, and Y. Aratani. 2011. Who are America’s poor children?: The official story. New York: National Center for Children in Poverty.
Wilkins, D. E. 2006. The “actual state of things”: Teaching about law in political and historical context. North Dakota Law Review 82(3):903–914.
Williams, D. R., and S. A. Mohammed. 2009. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine 32(1):20–47.
Wright, J. L., W. S. Davis, M. M. Joseph, A. M. Ellison, N. J. Heard-Garris, T. L. Johnson, and the American Academy of Pediatrics Board Committee on Equity. 2022. Eliminating race-based medicine. Pediatrics 150(1):e2022057998.
Xu, J., A. Saperstein, A. Morning, and S. Iverson. 2021. Gender, generation, and multiracial identification in the United States. Demography 58(5):1603–1630.
Yearby, R. 2020a. Structural racism: The root cause of the social determinants of health. https://blog.petrieflom.law.harvard.edu/2020/09/22/structural-racism-social-determinant-of-health/ (accessed August 5, 2024).
Yearby, R. 2020b. Structural racism and health disparities: Reconfiguring the social determinants of health framework to include the root cause. Journal of Law, Medicine & Ethics 48(3):518–526.
Yoon, P. 2021. Alternative methods for grouping race and ethnicity to monitor COVID-19 outcomes and vaccination coverage. Morbidity and Mortality Weekly Report 70(32):1075–1080.











































