Improving Access to High-Quality Mental Health Care for Veterans: Proceedings of a Workshop (2023)
Chapter: 1 Introduction
1
Introduction
Kenneth W. Kizer, distinguished professor emeritus at University of California, Davis, began the workshop by noting that the mental and behavioral health care needs of Americans have substantially grown over the past few decades. He stated that the Department of Veterans Affairs (VA) is not the only health system encountering challenges in meeting the mental health care needs of its population, although, as the nation’s largest provider of mental health care services, its challenges may be the greatest. Kizer discussed how Americans of all ages and demographics are often unable to get the mental health care services they need. Approximately half of the U.S. population, more than 150 million Americans, lives in areas with a provider shortage (HRSA, 2023). The Department of Health and Human Services estimates that by 2030, the mental health workforce will also shrink by 20 percent, despite a projected 3 percent rise in demand. A recent study illustrates this lack of access for military service members and their families. Researchers found that 35 percent of TRICARE1 beneficiaries lived in communities with inadequate access to psychiatrists (Bacolod et al., 2023). This study found that this shortage was concentrated in rural and economically disadvantaged areas. Kizer noted that this problem will not be solved overnight and that most communities will continue to experience inadequate access for years to come.
___________________
1 TRICARE is the health care program for active-duty service members, active-duty family members, National Guard and Reserve members and their family members, retirees and retiree family members, survivors, and certain former spouses worldwide. See https://www.tricare.mil/Plans/New (accessed August 1, 2023).
To address these challenges, and at the request of VA, the Forum on Mental Health and Substance Use Disorders held a public workshop on Improving Access to High-Quality Mental Health Care for Veterans to explore the U.S. landscape for mental health care services, including telehealth services. The workshop considered ways to improve veterans’ timely access to high-quality care for mental health conditions. In particular, it explored internal and external best practices for three critical needs for mental health access (known as “tripartite access” in VA): urgent/crisis, engagement, and sustained access.
ORGANIZATION OF THE WORKSHOP
The hybrid (in-person and virtual) workshop took place on April 20–21, 2023, at the National Academies of Sciences, Engineering, and Medicine (the National Academies) building in Washington, DC. The first session provided background on the state of VA mental health care services, followed by veterans and a family member sharing their own experiences in accessing these services. Next, speakers discussed various ways to address the growing need with limited staff. Presentations covered other international exemplar systems, innovative caregiver strategies, technology, and community partnerships. Day 2 sessions highlighted ways to embed some of these strategies more systematically and sustainably into systems. To conclude, the planning committee and a speaker from VA discussed future directions and considerations.
ORGANIZATION OF THE PROCEEDINGS
This document2 is organized into seven chapters. After the introduction, Chapter 2 presents firsthand experiences of veterans trying to access mental health services. Chapter 3 highlights the strengths and potential of VA as a national health care system, using several international and one U.S. example of how systems can maximize efficiency with limited resources. Chapter 4 focuses on strategies to improve and sustain mental health services in different settings and with technology. Chapter 5 explores opportunities for improving mental health care through various partnerships. Chapter 6 discusses taking
___________________
2 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop has been prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants, and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
some of these strategies to scale and institutionalizing them within systems, and Chapter 7 closes with a summary and reflections from workshop planning committee members. Appendixes A and B include the workshop Statement of Task and agenda, respectively.
OVERVIEW OF MENTAL HEALTH CARE SERVICES IN THE VETERANS HEALTH CARE SYSTEM
Tamara Campbell, executive director of the Veterans Health Administration (VHA) Office of Mental Health and Suicide Prevention, provided a keynote overview of mental health care services within VA. It has more than 170 medical centers, 1,100 outpatient clinics, and 17,000 licensed mental health care providers. It also has 11 Mental Illness Research, Education, and Clinical Centers; substance abuse treatment programs; integrated primary care and mental health care services; and the National Center for Posttraumatic Stress Disorder (PTSD), a leading research and educational center of excellence on PTSD and traumatic stress. She said that veterans engaging with mental health care services have doubled since 2006. Campbell stated that telemental health visits have also increased, with almost 5.9 million video visits in 2022, a nearly 14 percent increase compared to 2021. With that increase in demand, Campbell explained that VA is integrating telehealth into routine clinical practice, and it has become a standard offering. She shared VA’s approach for continuity of care in mental health, highlighting the stepped care model to promote treatment at the least intensive level that is clinically appropriate and transition between levels as needed (see Figure 1-1).
Campbell also reviewed some of VA’s programs, such as peer support, the opioid safety initiative, and substance use disorder and suicide prevention programs. For the latter, VA uses a public health approach, combining community partnership with evidence-based clinical strategies for intervention. VA focuses efforts on both short-term priorities and long-term efforts to maximize impact over time. Last, Campbell highlighted some of the public outreach and social marketing campaigns VA does to close the veteran–civilian divide. These include About Face and Make the Connection, stories of veterans talking about their experiences and their life after traumatic events; the Veterans Crisis Line, a suicide prevention resource available to all veterans; and mental health summits and national partnerships to engage communities and county-level associations wherever possible.
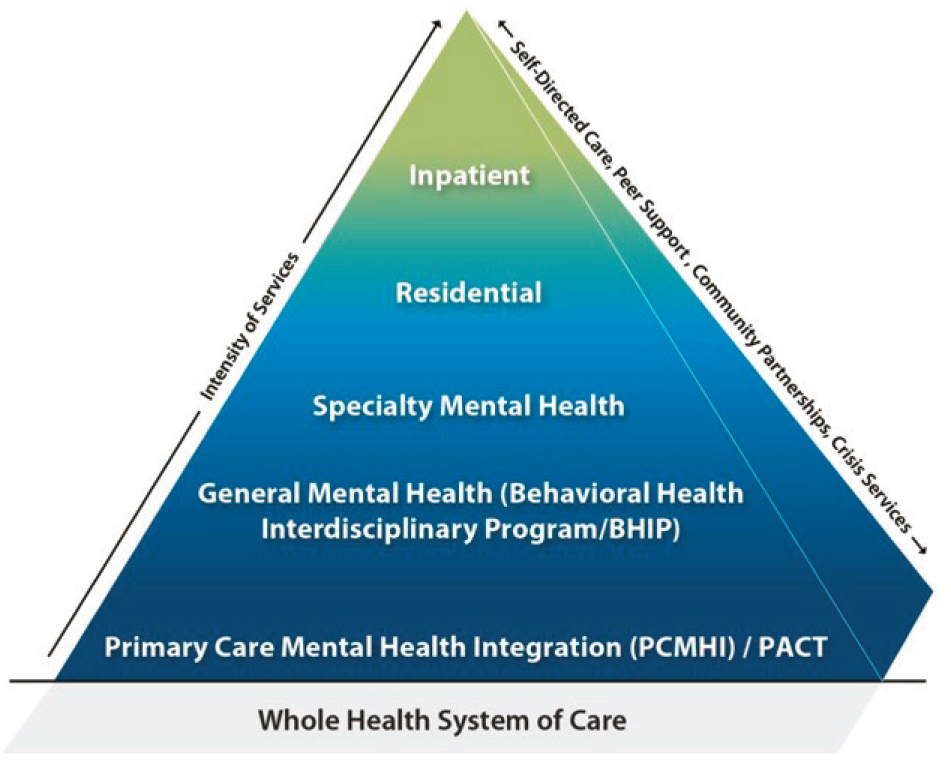
SOURCES: Tamara Campbell presentation, April 20, 2023; Office of Mental Health and Suicide Prevention, U.S. Department of Veterans Affairs.



