Addressing Workforce Challenges Across the Behavioral Health Continuum of Care: Proceedings of a Workshop (2025)
Chapter: Session 4: Structural and Policy Challenges
Session 4
Structural and Policy Challenges
Session 4 focused on discussing structural and policy challenges related to strengthening the behavioral health workforce and improving access to care. Common challenges discussed included addressing fragmented systems and inconsistent policies that hinder workforce development and service delivery. Several speakers discussed the importance of improving data collection and tracking workforce activities to assess quality and effectiveness, as well as expanding the scope of practice for nontraditional providers, such as community health workers and peer support specialists. The session also considered opportunities for better alignment between state and federal policies to help support workforce expansion, address liability concerns, and ensure quality services. See Box 5 for more highlights.
The moderator Kathleen R. Delaney, professor emeritus at Rush College of Nursing began by revisiting Frank’s comment in Session 3 on the importance of clearly identifying the workforce problems that need to be addressed. Delaney acknowledged that one significant challenge is building the necessary support and structures to develop and retain a workforce capable of effectively delivering essential mental health care and improving wellness. Delaney underscored the heterogeneity of populations requiring services, referencing Michael Friedman’s essay “Improving Mental Health Policy: No Simple Answers.”1 She emphasized that diverse needs require tailored approaches.
___________________
1 See https://www.michaelbfriedman.com/mbf/images/Improving_American_Mental_Health_Policy--HHPR.pdf (accessed September 22, 2024).
Box 5
Highlights from Individual Workshop Participants in Session 4
- Network adequacy in behavioral health is critical for access to care, but national standards vary significantly across states, with challenges such as low reimbursement rates and geographic disparities in provider distribution. (Seibert)
- States are addressing behavioral health workforce challenges through licensure policies, recruitment initiatives, loan forgiveness programs, and interstate licensure compacts to alleviate workforce shortages. (George)
- The workforce needs to move beyond population-based models to accommodate individualized care approaches that align with the recovery model and focus on personal life goals. (Fukui)
- Client-centered supervision, focusing on individual goals and strengths, can bridge the gap between the medical and recovery models, promoting more personalized care. (Fukui)
- Expanding the scope of practice for nontraditional care providers, such as community health workers and peer support specialists, can enhance access to behavioral health care, but it requires careful state-level policies to maintain quality and safety. (George)
- A focus on data collection and standardized quality measures is essential to track workforce effectiveness and identify gaps in care. (Seibert)
- Addressing fragmented systems and aligning state and federal policies are critical to supporting workforce expansion and improving access to care. (Delaney)
Delaney said that the conceptual shift to “democratizing” the workforce comes with significant policy, data, and financing challenges. She said that Session 4 was designed to explore these issues in more depth, with a focus on tracking the workforce and supporting its activities at national, state, and local levels. Each speaker addressed these challenges from a different perspective, including national-level efforts to track and apply outcome measures to an expanding workforce, state-level approaches to addressing policy issues, such as scope-of-practice laws, and local-level strategies for retaining and supporting community-based workers.
IMPROVING ACCOUNTABILITY FOR BEHAVIORAL HEALTH ACCESS: EVALUATING THE EVIDENCE FOR NETWORK ADEQUACY STANDARDS
Julie Hayes Seibert, assistant vice president, Behavioral Health at the National Committee for Quality Assurance (NCQA), discussed the significant challenges of ensuring network adequacy in behavioral health care, which refers to a health plan’s capacity to provide sufficient access to behavioral health services. This has become increasingly critical due to the rising demand for mental health services, particularly in the aftermath of the COVID-19 pandemic. Seibert emphasized that health plan networks have difficulty demonstrating access to behavioral health care providers, contributing to gaps in care when need is at an all-time high.
A key issue Seibert raised is the difficulty in measuring network adequacy at a national level due to variations in standards across states. Each state uses different criteria to assess plan compliance, making it difficult to establish a consistent national approach. These standards often fail to fully capture the scope of behavioral health services, where specialist (e.g., psychiatrists, social workers) participation is often limited. Seibert cited contributing factors which include provider shortages, particularly in underserved areas, low reimbursement rates, complex licensure laws that vary by state, and the administrative burden that discourages health care providers from joining or staying in networks.
To better understand these challenges, NCQA’s behavioral health team (NCQA, 2024) conducted a study funded by the Sozosei Foundation to assess the state of network adequacy and identify gaps. One aim was to identify where new metrics or standards could be developed. The team adopted a framework defining access based on five criteria: availability, accessibility, accommodation, affordability, and acceptability (Penchansky and Thomas, 1981). The research involved an environmental scan of both peer-reviewed and gray literature, and an inventory of measures used by the Centers for Medicare and Medicaid Services, the National Quality Forum, and the Agency for Healthcare Research and Quality. Additionally, 17 interested groups were interviewed to gather insights from various perspectives.
The findings revealed that 31 states had adopted at least one quantitative standard to monitor network adequacy for at least one type of insurance product, with 17 states implementing standards specific to behavioral health. However, these standards varied widely and often only addressed one aspect of access, such as geographic criteria, appointment wait times, or provider–enrollee ratios (see Figure 4). Seibert pointed out that measuring just one factor fails to capture the full picture of access, which should also consider aspects such as affordability, acceptability, and care quality. Furthermore, monitoring
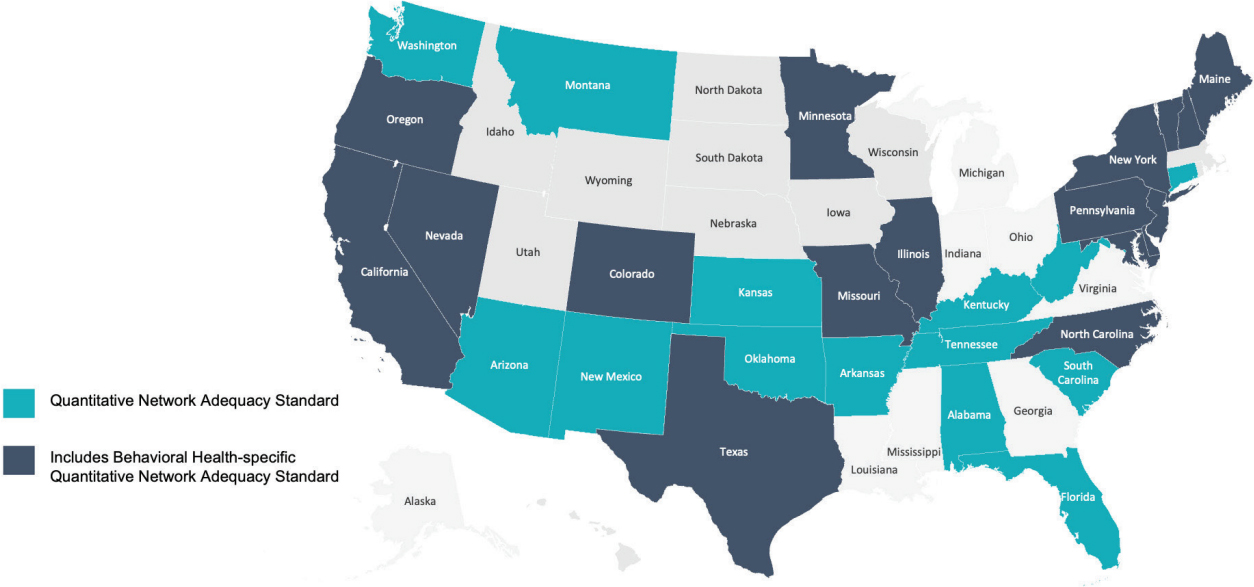
NOTE: Does not include standards applied to states’ Medicaid managed care, emergency-only standards, or states that have adopted national accreditation standards. Data are from Legal Action Center and the National Conference of State Legislatures.
SOURCES: Presented by Julie Seibert on July 11, 2024; NCQA, 2024.
and enforcement of these standards are often lacking, with little evidence of meaningful improvements in access.
In the study interviews, participants raised concerns about the shortcomings of network adequacy standards, arguing that behavioral health requires a different approach compared to other medical specialties. They highlighted the need to create standardized templates for calculating and monitoring network adequacy metrics and to develop new standards that better reflect the unique challenges of behavioral health care. One common concern was that standards do not ensure accountability or improvements in care access, leaving many patients underserved.
To address these issues, Seibert suggested several strategies frequently mentioned by participants, including expanding workforce supports, increasing telehealth, and enhancing crisis team services. The supports could include additional training programs for health care providers, consultation services, and greater use of care teams with paraprofessionals, nurse practitioners, and community health workers. Seibert also recommended developing more comprehensive and standardized measures that reflect the complexity of behavioral health care, along with investments in new care models and technologies to improve access and service delivery. While acknowledging that no “silver bullet” solution exists, she argued that addressing the gaps in standards and improving workforce supports are crucial steps toward ensuring that networks can meet the growing demand for services.
STATE LEGISLATIVE TRENDS IN BEHAVIORAL HEALTH WORKFORCE
Kelsie George, senior policy specialist with the Health Program at the National Conference of State Legislatures (NCSL), discussed state-level strategies for managing and supporting the behavioral health workforce. She provided an overview of recent state legislation addressing key workforce issues, including licensure, certification, recruitment, retention, and training. George highlighted four major trends emerging from state legislative efforts: (1) data collection and analysis, (2) recruitment and retention, (3) licensure and certification, and (4) scope of practice.
George noted that data collection is essential for establishing baselines, understanding workforce needs, and measuring the impact of interventions. She provided information on recent state examples, including Georgia, which has created a behavioral health workforce database, and Illinois, which has established a task force to study mental health service availability for youth in care. These initiatives help states tailor solutions to specific needs.
States are exploring educational pathways and career pipelines to address workforce shortages. However, she noted that recruitment alone will not address workforce challenges across states, as attrition remains high across behavioral health professions. To address retention, at least 10 states have implemented financial incentives, including loan forgiveness, repayment programs, and tax incentives.
George discussed licensure and certification for many health professions, such as physicians, nurses, and counselors in the context of recruitment and retention. Mentorship and supervision are required for licensure for many health occupations, but finding qualified preceptors is challenging. Some states have enacted tax incentive programs to encourage clinical preceptors, particularly in rural and underserved areas. States are also reviewing licensure requirements as a pathway to reimbursement, especially through Medicaid. A major trend is interstate licensure compacts, which allow for either expedited licensure or mutual recognition across states. Telehealth’s rapid expansion during the pandemic spurred more states to join these compacts, facilitating cross-state practice for behavioral health professionals.
George also addressed state activity around scope of practice, which defines the procedures and responsibilities health care professionals are authorized to perform. Some states, such as Utah and Virginia, are expanding scope of practice for new professionals, including those with bachelor’s degrees.
NCSL has maintained a scope-of-practice legislation database since 2015,2 which tracks these trends.
George mentioned two emerging issues NCSL is monitoring: Drug Enforcement Administration prior authorization requirements for prescribing buprenorphine for opioid use disorder and whether states will allow licensed professional counselors to diagnose mental illness or require a referral to another professional for diagnosis and treatment planning.
IDENTIFYING AND FILLING GAPS TO PROMOTE VALUE-BASED CARE THROUGH QUALITY MEASURES AND CLIENT-CENTERED SUPERVISION
Sadaaki Fukui, interim associate dean for research and associate professor at the Indiana University School of Social Work, described client-centered supervision as a crucial mechanism for promoting value-based care across the behavioral health care continuum. He began by discussing the paradigm shift from the traditional medical model, which focuses on diagnosing and treating mental health conditions, to the recovery model, which emphasizes supporting individuals in achieving personal life goals, beyond simply managing symptoms. He highlighted that while the latter has significantly influenced how behavioral health care is conceptualized, implementing this model in daily practice remains challenging due to structural and policy barriers that are rooted in the medical model. He argued that current policies are typically designed around a population-based model, which aims to maximize efficiency and equity by addressing the aggregated needs of individuals with behavioral health conditions. However, this approach often fails to accommodate the unique strengths and goals of each person. Fukui proposed client-centered supervision as a strategy to bridge the gap between policy and practice. It involves tailoring supervision practices to focus on individual clients’ goals and strengths, rather than solely on meeting standardized quality measures or productivity targets. He argued that this bottom-up approach allows for a more personalized form of advocacy that can inform structural and policy changes needed to support the recovery model.
Fukui acknowledged several challenges, however, in implementing client-centered supervision, particularly in systems that are still heavily influenced by the medical model, including misalignment between policy and practice; resource constraints; and lack of training and support to be effective. As a strategy to address these challenges, he emphasized the importance of ongo-
___________________
2 See https://www.ncsl.org/health/scope-of-practice-legislation-database (accessed September 25, 2024).
ing training and support for supervisors and the need for systemic changes that prioritize the recovery model at all levels of care. He also advocated for data-driven approaches to measure the impact of client-centered supervision on both client outcomes and provider job well-being, which could help build the case for broader adoption of this approach.
Fukui reiterated five key takeaway messages:
- behavioral health policies and systems tend to be driven by medical models;
- the recovery-oriented client-centered practice may not fit under the population model;
- evaluating quality measures based on the recovery model promotes opportunities for identifying system and structure gaps;
- those who implement client-centered supervision and management can be the key actors for building the feedback loop for system advocacy; and
- such efforts may not only promote value-based care in the behavioral health continuum but also help regain a strong and quality workforce.
DISCUSSION
A participant raised a question about supporting primary care clinicians—who are the entry point to care for most patients—because a focus on primary care does not seem to fit with the policy landscape’s orientation. Seibert responded that NCQA is reviewing measures to make sure it is capturing primary care clinicians and others who provide behavioral health services in primary care settings and that they are counted in quality measures. She added that NCQA also aims to ensure that primary care and other settings have standards for behavioral health consults and referrals. George mentioned that NCSL is seeing policy initiatives expanded to occupations such as primary care clinicians, for example, tax incentives for rural practice and loan forgiveness programs, many of which were targeted specifically to primary care providers and nurses first, especially in rural and underserved communities.
Another participant asked about the practical challenges of implementing the client-centered supervision model in behavioral health care settings, and specifically whether there were any “real-world” examples of the model and how they were measuring client goals. Fukui responded that he and his colleagues are providing strengths model case management but are still working on how to best implement client-centered supervision and not yet collecting data.
A virtual participant asked about the challenges and successes in reforming scope-of-practice laws at the state level, focused on how states can balance that need for reform with concerns about maintaining quality and safety and protecting these nonphysician care providers from liability. George responded by emphasizing the importance of data-driven decision making in these reforms. She highlighted examples from states such as Utah, where systematic reviews of licensure and scope-of-practice laws have been used to inform policy changes. She also stressed the need for ongoing monitoring and evaluation to ensure that these reforms continue to meet the needs of both care providers and patients without compromising care quality.







