A Research Agenda to Protect Human Health and Build Resilience in the Face of a Changing Climate (2025)
Chapter: INTRODUCTION
INTRODUCTION
BACKGROUND AND CONTEXT
Climate change is among the most significant health challenges of the 21st century. Extensive evidence supports the scientific consensus that human health and well-being are profoundly impacted by climate change (IPCC 2023).
Climate change affects human health through a variety of pathways, both direct and indirect. Direct impacts include extreme weather events like heatwaves, hurricanes, and floods, which can cause immediate injury, death, and mental health conditions such as anxiety, depression, and post-traumatic stress disorder. Indirect impacts involve changes in environmental conditions that affect health, such as shifts in the patterns of vector-borne diseases (e.g., malaria and dengue fever), worsening air quality leading to respiratory and cardiovascular problems, and threats to food and water security that can result in malnutrition and waterborne diseases. These effects are further complicated by social drivers of health, including economic status, access to health care, and pre-existing health conditions (Haines and Ebi 2019). As the impacts of climate change intensify, they exacerbate existing health disparities, disproportionately affecting marginalized communities and threatening the well-being of populations worldwide. Addressing these intersections between climate change, human health, and equity are crucial to promoting resilience and well-being for all (EPA 2022; IPCC 2023).
Research on the health impacts of climate change has significantly increased in the past decade (Bartlett et al. 2024). However, gaps in evidence and a shortage of applied research impede the knowledge necessary to implement effective solutions. Furthermore, the protection of human health has only recently become a primary consideration in global climate change policy discussions (Fears et al. 2021). The heightened awareness of health issues is prompting decision makers to demand robust scientific data for knowledge synthesis and policy guidance on health and
health care, including evidence on effect attribution—the process of determining the extent to which specific health outcomes can be directly linked to environmental factors like climate change (Vicedo-Cabrera et al. 2021)—and the quantification of adaptation and mitigation solutions (Hobbhahn et al. 2019). Adaptation refers to actions that adjust practices, processes, and structures to reduce the negative impacts of climate change on human health and infrastructure, while mitigation aims to limit the extent of climate change by reducing greenhouse gas emissions.
There is a need for a research agenda for climate change and human health to advance understanding, guide policy and practice, and ultimately protect and improve human health in the face of a changing climate. A research agenda for climate change and human health is crucial for understanding the complex interactions between climate factors and health outcomes. By studying the complex interactions between climate change and health as well as the health co-benefits of climate action, we can develop evidence-based strategies that inform effective mitigation and adaptation efforts.
This is essential for policymakers and practitioners to make informed decisions that protect public health and allocate resources efficiently to address the most pressing health challenges posed by climate change.
Additionally, a research agenda enhances community resilience and preparedness by identifying targeted interventions and designing health care systems capable of responding to climate-related health threats. It ensures that populations living in vulnerable conditions, such as low-income communities, older adults, pregnant women, children, and those with pre-existing health conditions, are specifically addressed in climate and health strategies. By identifying research gaps and promoting innovation, we can develop new technologies and policies to mitigate and adapt to health impacts. Furthermore, a structured agenda provides a framework for monitoring and evaluating the effectiveness of interventions, facilitating global coordination and collaboration to share knowledge, data, and best practices in tackling the global health impacts of climate change.
To this end, the National Academy of Medicine (NAM) and Kaiser Permanente collaborated to develop a research agenda for climate change and human health. While this research agenda is focused on the United States, the approach and findings are broadly relevant to other countries facing similar challenges. Importantly, the NAM collaborated with stakeholders from various sectors and communities, integrating diverse perspectives to shape the research priorities. This inclusive approach ensures that the research agenda reflects the concerns and priorities of those most affected by climate change. Co-developing the research agenda acknowledges the complex and interconnected nature of the challenges posed by climate change, health disparities, and social inequities. This process
fosters transparency, accountability, and shared ownership among all stakeholders, enhancing the relevance, validity, and impact of the research outcomes.
RESEARCH AGENDA METHODOLOGY
The development of this research agenda involved a multi-phase process (see Figure I-1) designed to ensure inclusivity and comprehensiveness.
The methodology included informational interviews, a review of existing literature, and public feedback through a survey of meeting attendees:
- Phase 1: Discovery: The NAM’s Climate Grand Challenge collaborated with the National Academies of Sciences, Engineering, and Medicine’s Climate Crossroads initiative to conduct 20 informational interviews across all workstreams. Half of the interviewees were researchers across disciplines such as climate change and health, environmental health, epidemiology, public health, geriatrics, and reproductive health. The remaining interviewees included community representatives, sustainability practitioners, policymakers, philanthropists, and members of the Climate Communities Network (CCN) with lived experience. Appendix A is a semi-structured interview protocol that was modified depending on respondent’s expertise. Key words that were derived from the interviews to inform the literature search are included in Appendix B.
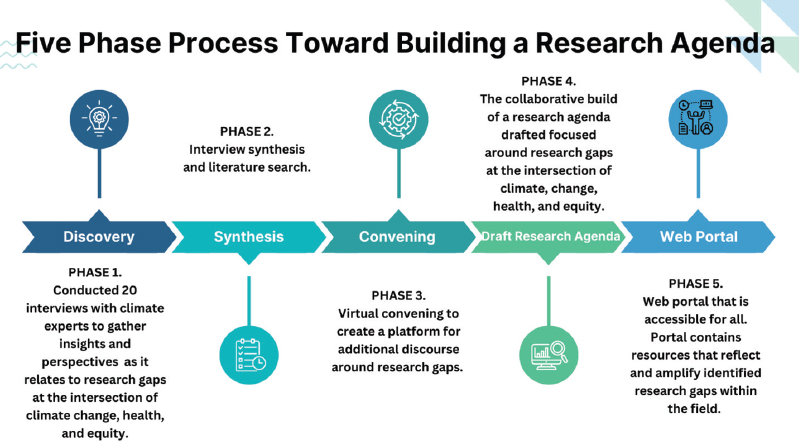
- Phase 2: Literature Search: Information from Phase 1 was synthesized to inform a literature search to explore the intersections of climate change, health, and equity. Key words included information from Phase 1 as well as guidance from the National Academies research center staff. Tailored search strategies with relevant key words (see Appendix B) were developed, focusing on U.S. based publications from the past decade. Databases that were selected included Embase, Medline (PubMed), and Scopus for their comprehensive coverage. The results were analyzed to identify gaps, particularly regarding disparities, biases, and structural inequities. To supplement the scholarly search, governmental resources, such as those from the U.S. Environmental Protection Agency and the U.S. Department of Health and Human Services, were consulted. Research gaps identified across Phases 1 and 2 are listed in Appendix C.
- Phase 3: Convening and Feedback: The NAM convened a full-day online meeting with climate and health experts, including those with lived experience, to discuss gaps in knowledge. Community members were selected through CCN, a program within the NAM Climate Grand Challenge. A survey was distributed to meeting attendees to gather feedback from interested stakeholders for the research agenda. Appendix D contains the survey questions. A subset of respondents from the meeting was targeted to identify additional research gaps and 37 individuals responded. Respondents included professionals from diverse fields focused on climate, health, and equity. Their expertise spans areas such as environmental health, epidemiology, urban development, socioeconomic inequalities, mental health impacts, and public policy (see Appendix E).
- Phase 4: Draft and Validate Research Agenda: Following analysis and synthesis of the informational interviews, literature search results, online convening discussions, and survey results, a proposed research agenda was drafted to address evidence gaps in climate-based health impacts and intervention strategies in the United States.
- Phase 5: Evidence and Tools Portal: A searchable database will be created to support researchers, the general community, and policy advisors, focusing on health equity. This publicly accessible, community-oriented portal aims to inform action beyond academic circles.



