Myopia: Causes, Prevention, and Treatment of an Increasingly Common Disease (2024)
Chapter: 8 Identifying Children with Myopia and the Links to Treatment: Methods and Barriers
8
Identifying Children with Myopia and the Links to Treatment: Methods and Barriers
This chapter focuses on medically underserved populations of children and their families that face health disparities, specifically racial and ethnic minority groups, people with lower socioeconomic status, rural communities, and children with disabilities. Sexual and gender minority groups were not included because a quick search yielded no studies on the topic. The chapter, like the rest of this report, focuses on myopia, though it should be noted that childhood visual problems in need of detection extend beyond myopia to other refractive errors, amblyopia, and amblyogenic risk factors (see Box 8-1).
Myopia can be identified through vision screening and comprehensive eye exams. Vision screenings for children may occur in pediatric primary care practices, schools, and community-based settings and are either targeted to medically underserved populations or provided universally to all children. Vision screenings offer a cost-effective way to evaluate key elements of vision in many children. Comprehensive eye exams, by contrast, evaluate the full picture of eye health for each child, are provided by doctors of optometry and ophthalmology where available in local communities, and generally incur higher costs.
The barriers to identifying and treating myopia are vast. To start with, myopia is a condition that most often begins early in life (Kleinstein et al., 2012) when children are unable to articulate that their distance vision is blurry or even realize that blurry vision is not normal. Community- or school-based vision screenings may help identify children with myopia who need a full comprehensive eye exam and a prescription for glasses from an eye care professional. However, if identified myopia is left untreated the vision screening will have had no impact for those children. Furthermore, vision screening by itself fails to establish an “eye care home” for the child with myopia, a lifelong condition that worsens throughout childhood (Houet al., 2018). Comprehensive eye exams for all children may increase the likelihood that a child with myopia will be detected, provided with glasses, and monitored by an eye doctor. However, comprehensive eye exams for all children may not be feasible for reasons including shortages in the supply of eye care professionals, especially pediatric eye care professionals in the United States where 90% of counties do not have a pediatric ophthalmologist (Walsh et al., 2023) and nearly 25% of counties do not have an optometrist (Feng et al., 2020). The provision of a prescription for glasses after a comprehensive eye exam either triggered by vision screening or booked independently may be helpful. However, research suggests that glasses are often unavailable and even when dispensed may not be worn or replaced if broken or lost (Ethan et al., 2010; Nishimura et al.,2024).
Even in ideal models with long-term case-management and cohesive multidisciplinary collaboration, several barriers exist to identifying and treating myopia and its progression: finances, lack of awareness, and logistics such as transportation. Vision screening and
comprehensive eye exams are informed by a range of policies and recommendations across states and professional associations. This range of policies and recommendations, compounded by poor strategies to ensure follow-up, make surveillance challenging. The outcome of this is often inadequate vision care and follow-up with eye care professionals. In short, there is a critical need for novel, effective strategies to ensure adequate detection and management of childhood myopia.
BOX 8-1
Other Childhood Visual Problems Besides Myopia That Deserve Attention
Although the focus of this National Academies report is myopia, childhood visual problems in need of detection extend beyond myopia to other refractive errors, amblyopia, and amblyogenic risk factors. Other refractive errors include hyperopia (far-sightedness), astigmatism (cornea and/or lens non-spherical irregularity), and anisometropia (unequal refractive error between the paired two eyes). In early childhood, hyperopia and astigmatism are more common than myopia, but by middle childhood myopia is the most common refractive error.
Amblyopia is reduced visual acuity, typically in a structurally normal eye, that results from perturbation in visual experience in one eye relative to the other, providing poor binocular input to the visual cortex early in life. Factors that may lead to the development of amblyopia include unequal focus between the eyes (anisometropia), non-straight paired eye alignment (strabismus), and inability to form a clear image because of a high refractive error, as examples. Although less common than refractive error, amblyopia occurs in 3–5% of the population in the United States. It can be effectively treated or prevented before about age 8 years (Holmes & Levi, 2018). After this early neurodevelopmentally sensitive period, it is still possible to improve visual impairment due to amblyopia, but not to the same degree as would be the case in early childhood, and amblyopia remains as a lifelong impairment (Scheiman, 2005).
Amblyogenic conditions other than refractive error that can be due to structural ocular changes include childhood cataracts or glaucoma, corneal cloudiness, vitreous hemorrhage, optic nerve maldevelopment, and significant eyelid droop (ptosis) that covers the pupil, among others.
MODELS FOR IDENTIFYING AND TREATING MYOPIA
Comprehensive Eye Exams
A comprehensive eye exam generally refers to a detailed eye exam that is provided by an eye care professional (optometrist or ophthalmologist) and is the highest standard of care for children’s vision (American Optometric Association & Carey, 2018). Comprehensive eye exams often occur in a doctor’s office, involve multiple assessments and, usually, the use of dilating eye drops. Assessments in a comprehensive eye exam include ocular history, external inspection of the eye structures, distance visual acuity, ocular motility assessment (ability to move the eyes in specified directions), cross cover test (to check for eye misalignment), corneal light reflex, red reflex, pupil examination, ophthalmoscopy (examination of the back of the eye with a special instrument), instrument-based screening (if needed), and color vision (American Optometric Association, 2017). The multiple tests included in a comprehensive eye exam are described in
the chapter on diagnosis (see Chapter 4). Comprehensive eye exams can detect not only myopia but also other refractive errors, amblyopia, and risk factors for amblyopia.
While dilating eye drops are not required in a comprehensive eye exam, they are almost universally recommended in national practice policies for children, because they are likely to enhance the ability to evaluate and diagnose eye and vision problems in children (American Optometric Association, 2017; Flitcroft, 2019; Hutchinson et al., 2023; Saxena et al., 2020). The use of dilating eye drops helps knock out the child’s dynamic focusing system and provides a more stable and precise measure of refractive error and glasses prescription for any discovered myopia. It is also essential for detecting hyperopia in children, because hyperopia can be masked easily by the child’s focusing ability. Dilation also helps doctors evaluate the health of the eye by increasing and stabilizing the size of the pupil so that the retina can be visualized.
Even for children who are asymptomatic or at low risk, the American Optometric Association recommends comprehensive eye exams, the first between 6 and 12 months of age, then at least once between ages 3 and 5 years, then before first grade, and then every one to two years thereafter (Table 8-1; see Table 8-5 for recommendations from other professional associations). Comprehensive eye exams can be more expensive than vision screening; however, they involve a broader evaluation of a child’s vision, eye health, and refractive error; follow-up eye care may also be better (Ekdawi et al., 2021).
| Examination Interval | ||
|---|---|---|
| Patient Age | Asymptomatic/Low Risk | At-risk |
| Birth through 2 years | At 6 to 12 months of age | At 6 to 12 months of age or as recommended |
| 3 through 5 years | At least once between 3 and 5 years of age | At least once between 3 and 5 years of age or as recommended |
| 6 through 18 years | Before first grade and annually thereafter | Before first grade and annually, or as recommended, thereafter |
NOTES: The American Optometric Association Clinical Practice Guidelines provide more information on other eye and vision disorders and their risk factors. (For more information about the practical guidelines, see https://www.aoa.org/practice/clinical-guidelines/clinical-practice-guidelines?sso=y.)
SOURCE: American Optometric Association, 2017.
Vision Screening
Vision screening generally refers to an abbreviated evaluation of vision and is important for the early detection of vision loss in children who may not have had a comprehensive eye exam. Vision screening aims to identify common vision disorders and facilitate diagnosis and
treatment through referrals to eye care providers (optometrists and ophthalmologists). It can be conducted by persons other than eye doctors (e.g., school nurses, trained volunteers) in primary care practices, as a school-based universal screening program, as a community-based program (e.g., at a shopping mall, summer camp, or mobile eye unit), or as a targeted program at sites selected to address a high level of need. Vision screenings may be instrument-based, such that an automated device measures refractive error. Instrument-based screenings may also pick up eye turns and structural issues, including droopy lids and cataracts, and instrument-based screening can be used as early as infancy. For older children, vision screening usually includes a measure of distance visual acuity by having the child view letters or pictures of decreasing size one eye at a time. Some vision screenings also include assessments of eye alignment, stereoscopic 3D depth perception, color vision, and/or near acuity. Vision screening, as an abbreviated evaluation, will not obtain identical results to a comprehensive eye exam. The rate of false positive and false negative screening results varies as a function of the type of vision screening tool used, the age of the child, the referral cut-offs, and the visual impairment. The amount of time needed for each type of vision screening test varies significantly based on the type of tool used. Compared to acuity tests, vision screening with instrument-based tools (e.g., autorefractors or photoscreeners) is quick (less than a minute for newer models) and requires minimal cooperation from the child (Donahue & Nixon, 2016; Donahue et al., 2016a; Loh & Chaing, 2018). Nevertheless, because of their cost and clinical practice recommendations, instrument-based devices are used less often compared to visual acuity tests and physical examination of the eye (Hoover et al., 2023; Oke et al., 2023).
Data on the prevalence of vision screening are often based on small samples of the population that are not representative of the general population, that lack standardized definitions, or that depend on parental 1 reports. An example of data based on parental reporting comes from a large nationwide survey of parents in 2018 and 2019, in which 14% of all U.S. children were reported by their caregivers to have received a vision test in the prior year in school, 28% in pediatric primary care clinics, and 34% in eye clinics (Child and Adolescent Health Measurement Initiative). Figures based on this national survey reflect parental awareness that the child had been screened and may, therefore, underestimate the actual amount of screening. Also, prior to 2021, no national survey has measured whether parents followed up when screening results indicated a referral to an eye doctor was warranted.
Measured Benefits of Vision Screening
Vision screening with follow-up eye care with an eye care professional (optometrist or ophthalmologist) to diagnose and treat vision impairment has been shown to have positive impacts on many aspects of a child’s development. In the Baltimore City public schools, a randomized controlled trial of 2,304 students in grades 3 to 7 found that universal vision screening with the provision of needed prescription glasses for uncorrected refractive errors improved academic achievement in reading over the next year (Harewood et al., 2024; Killeen et al., 2023). A review of nine studies, six of them randomized controlled trials (RCTs) and all of them of satisfactory or good quality (Pirindhavellie et al., 2023) revealed that getting glasses improved children’s math and literacy scores, school behaviors (focusing, practice), and mental health and quality-of-life scores, and it also decreased anxiety, with small effects in each case
___________________
1 Throughout this report, the term “parent” is used to denote any adult in the position of primary caregiver to a child and not restricted to biological parent.
(see also Lee et al, 2023; Muhammad & Tumin, 2022; Shin & Finnegan, 2009; Simon et al., 2007). Three of the studies were conducted in the United States.
Vision Screening in Primary Care Practice
In primary care practice, vision screening (including ocular risk assessments and visual acuity measurements) is provided as part of routine preventive screenings and assessments at well-child visits, starting from infancy and continuing through adolescence (Bright Futures & American Academy of Pediatrics, 2022; Donahue et al., 2016a). Well-child visits are preventive healthcare assessments recommended throughout childhood in pediatric primary care. These well-child visits are scheduled to require about 15–20 minutes on average and include a vision screening and assessments of a child’s medical history.
Vision screenings as part of well-child visits are usually conducted by support staff, such as medical assistants, but the onus is on the primary care clinicians to refer the child to an eye care provider when needed, and to explain to the parent(s) the importance of taking the child for a comprehensive eye exam. If the primary practice provider has an autorefractor, the vision screening for myopia and other refractive errors can take less than a minute. If it involves acuity charts, it will take 5–15 minutes, depending on the age and cooperation of the child.
The Centers for Medicaid & Medicare Services (CMS) provides three different Current Procedural Terminology (CPT) codes for billing insurance for vision screening, specifically CPT 99173 (visual acuity test using optotypes or charts), 99174 (instrument-based screening with off-site analysis) and 99177 (instrument-based screening with on-site analysis).
Vision Screening as a Universal Program at School
One strategy for detecting all children with myopia (and other visual problems) is universal vision screening at school. Elementary schoolchildren are a “captive” population, which makes it possible to provide them with universal access to this first step in eye care. School-based programs at the very minimum usually include a visual acuity measurement and referral to a community eye care provider. Other models have included the use of on-site comprehensive eye exams by eye care professionals (optometrist or ophthalmologist).
Vision Screening Methodologies and Their Applicability
To detect myopia, vision screening programs can use distance visual acuity or photoscreeners (a type of instrument-based tool). The same tools can be used in primary care practices, community-based screening, and targeted screening programs. In the following sections, the methodology behind the successful use of each tool as part of vision screening is described along with its general applicability.
Using Distance Visual Acuity
A survey of screening in school-aged children in 18 countries on five continents found that all programs used some form of distance visual acuity test, and for 44% of countries this was the only test (Chen et al., 2019), perhaps because it is the cheapest. Similarly, distance visual acuity is the most common test in mandated vision screening in the United States (Wahl et al., 2021). There are variations in which symbols are used on the acuity chart, both across countries and across states. Consensus guidelines from the U.S. Committee on Vision and the International Council of Ophthalmology specify that the letters, numbers, or pictures must be of more-or-less
equal legibility, with the same number of items on each line and the items spaced horizontally by the width of each symbol and vertically by the width of the symbols in the next line. The sizes should decrease by approximately 0.1 log units across lines and the symbols should be black on a white background (reviewed in Chaplin & Bradford, 2011). These requirements are fulfilled by Sloan letters, LEA numbers, Tumbling Es with crowding bars, HOTV with proportional spacing or crowding bars, Cambridge crowded acuity, and LEA symbols with proportional spacing.
Acuity must be tested monocularly (one eye at a time) with the child situated at a specified distance away from the symbols (typically 10 or 20 feet). This is because the myopic child might have different refractive errors in the two eyes and because the child may well be able to read the test items at a close distance but fail as they become fuzzy at further distances. There is a marked drop-off in distance acuity with increasing myopia, at least up to −2.0 D (Kleinstein et al., 2021). For younger children, the test is more effective at a closer distance, such as 5 feet, and can be turned into a matching game such that the child points to the letter/symbol on a chart they are holding that matches the one the experimenter is pointing to on the distant test chart (Kulp et al., 2022). For children ages 4–6 years, this can usually be done successfully with letter charts; for younger children, charts with icons for common objects can work better. The Tumbling E chart and Allen picture cards are other options, but they can lead to errors because young children confuse left and right (Tumbling E) or the test can overestimate acuity (Tumbling E and Allen picture cards; reviewed in Chaplin & Bradford, 2011). Children’s distance visual acuity can be tested as young as 3 years of age if they are given a matching card instead of being asked to name the letters and if the testing distance is reduced to 5 feet (Kulp et al., 2022). However, many will be untestable (27% at age 3 vs. 8% at age 4 according to Hered & Wood, 2013) and 4- and 5-year-olds are easier to test. Moreover, overall sensitivity and specificity are higher at age 5 than at age 4 (Nishimura et al., 2020).
The test chart must be illuminated by good lighting, and distractions such as another child being tested nearby need to be avoided. Finishing monocular tests of both eyes typically takes less than 10 minutes for a 4- to 6-year-old child and less time for older children. The advantage of distance acuity testing is that the charts are inexpensive; the disadvantages are the need for a well-lighted space in the school, which can be scarce, and the duration of the test. To detect amblyopia, as opposed to myopia, the symbols/letters need to be “crowded,” meaning surrounded by other symbols/letters or bars (Lalor et al., 2016). This is because many amblyopes can read single letters and have difficulty only when the letters are embedded in print among other letters.
In a sample of 6,017 Chinese children ages 4 to 15 years who were screened at school, a well-designed chart (Early Treatment Diabetic Retinopathy Study or ETDRS) and a cut-off of 6/7.5 for children ages 7 and older was accurate in detecting children with −0.5D of myopia or worse by cyclopleged retinoscopy (sensitivity 91.7% and 95.6% for children ages 7–12 years and 13–15 years, respectively; specificity, 80.3% and 85.4%, respectively). For younger children, that cutoff yielded a sensitivity of 86.5% and a specificity of 51.2%. Specificity improved with a cutoff of 6/9.5 to 84.7%, but then sensitivity dropped to 67.3%; 31.8% of the sample proved to be myopic (Wang et al., 2022).
Using Photoscreeners
Photoscreeners such as the Spot (Welch Allyn) and the Plusoptix devices are faster but more expensive than visual acuity charts. In September 2020, 17 U.S. states permitted the optional use of some type of instrument-based device for screening, especially if the child is
young or unable to complete acuity screening (Wahl et al., 2021). Photoscreeners work by shining a point of infrared light into both eyes off the fixating axis and estimating the refractive error by how well focused is the red reflex that returns from the retina. For school screening, the devices are used without cycloplegia, leading to a possible underestimation of hyperopia (which a child can partially overcome by accommodation) or a slight overestimation of myopia (because the child is focusing hard on the fixation point). Nevertheless, the devices are quite accurate in detecting higher levels of myopia and measuring astigmatism.
Values obtained from the Spot and Plusoptix photoscreeners are highly correlated (Peterseim et al., 2014). Screening typically takes less than a minute and requires only that the child view a fixation attractor in the center of the device (Modest, 2017). The Spot will generally work in any lighting, and it was successful in screening 99.10% of 4,811 children ages 4–5 years in one study, while the PlusoptiX, which requires a darkened space in order to detect the pupil accurately, was successful with only 95.8% of the same children (Nishimura et al., 2019, 2020). In primary care settings, more children were screened successfully with a photoscreener (the Spot; 90%) than with the combination of distance visual acuity and a preschool test of 3D stereoscopic vision (54%), with the largest difference found among 3-year-olds (Modest, 2017). Similarly, the Spot (89.9% successful) and PlusoptiX (73.8% successful) were able to screen most of the 84 children who could not be assessed with the Lea symbols acuity test or the Stereo butterfly test in a preschool screening program for Michigan 3-to-5-year-olds (Musch et al., 2022). Children who are untestable should be referred, because they are more likely to have a vision problem than those who pass screening (Maguire & Vision in Preschool Study Group., 2007).
These screening tools have been used successfully with lay personnel given minimal training (Kulp et al., 2022). Besides screeners, help is needed to fetch and return children to the classroom and to manage the flow between screening stations. Referral values differ with the age of the child because the average eye changes with development from being hyperopic in early childhood to being emmetropic during primary school. The referral cutoff for myopia usually begins around −1.5 D to −3.0 D during the early period when most children are hyperopic and decreases to −0.5 D to −1.0 D when the child is older than 7 years (see, for example, Arnold et al, 2022; Donahue et al., 2016a; Grossman et al., 2017). An unanswered question is whether a child who is already emmetropizing before primary school should be referred for longitudinal screening or regular visits to an eye care professional because this may be a sign of emerging myopia (see Chapter 5). Enough is now known to be concerned about the child showing any myopia before age 7 and to recommend that they have regular follow-up with a comprehensive eye exam (see Box 5-2 in Chapter 5 on Onset and Progression).
Sensitivity and Specificity
The literature gives values for the sensitivity, specificity, and positive predictive value for screening for amblyopia and refractive errors using distance visual acuity, photoscreeners, or both, for children of different ages. The outcome depends on the referral cutoff: a strict cutoff increases sensitivity, resulting in fewer missed eye problems, but it also decreases specificity, allowing more false positives. Constant software updates make it difficult to compare studies precisely. A meta-analysis of 21 studies involving 5,022 children found no significant difference in sensitivity or specificity in detecting all types of refractive error between the Spot and Plusoptix, either in the entire population or in the 10 studies involving 3,221 children under age 7
(Zhang et al., 2019). The results were similar for studies conducted in the United States and in Asia.
Table 8-2 gives the sensitivity and specificity of the Spot and Plusoptix photoscreeners for detecting myopia with different cutoffs. Although there are several studies giving these values for hyperopia and astigmatism, or any type of refractive error, there are fewer for myopia, and those are mainly from China, perhaps because of higher prevalence or concern. A study of French children seen for follow-up in an eye clinic found a correlation of 0.91 between the refractive error value obtained by the Plusoptix and the value obtained by cyclopleged retinoscopy for the 14 myopic children, who were between 18 and 86 months old, with 90% of values within 1.0 D of each other (Payerols et al., 2016).
| Study; Photoscre ener | Type of Sample | Age Range (mean years) | Country | Number of Children | Cut-off for Myopia (diopters) (worse than) | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|
| Qian et al., 2019; Spot | Eye hospital screening or checkup | 4–6 (5.2) | China | 113 | −1.5 in any meridian | 93.5% | 90.3% |
| Mu et al., 2016; Spot | Eye hospital screening or checkup | 4–7 (5.7) | China | 168 | −1.5 in any meridian | 85.6% | 79.65% |
| Yan et al. 2015: Plusoptix | Patients at eye hospital | 2–14 (6.2) | China | 178 | −3.0 in any meridian | 85.7% | 94.7% |
SOURCE: Committee generated.
Community-Based Screening
Another model is to offer vision screening in places where parents often take their children, like shopping malls, summer camps, or community events, where one captures great numbers of children at one time. The screening can be conducted in an empty store space, in an office, in a portable van, or at an after-school program. While the tools used are the same as in screening in schools, the coverage will not be universal. However, the presence of parent(s) means that the results and their importance can be conveyed immediately, and any questions answered. Community-based screening is often conducted by volunteer groups such as the Lions Club. Follow-up rates with eye care providers for individuals screened in these programs is often low unless effective follow-up strategies are used, such as the use of portable equipment to
conduct on-the-spot follow-up comprehensive eye exams for those who fail screening (Asare et al., 2017; Donahue et al., 2006).
Targeted Screening
A general finding from universal school screening is that children from medically underserved neighborhoods are more likely to “fail” screening and be referred for a comprehensive eye exam. Children from medically underserved populations are often less likely to have a family doctor or attend well-child visits. The advantage of targeted screening is that resources are allocated where there is the greatest need and the total cost is less than offering screening in every school (Abdus & Selden, 2022; Asare al., 2022). The tools used are the same as for universal screening in schools.
For example, after photoscreening of 14,000 children in all grades (elementary through high school) in 58 schools in three Virginia school districts, the referral rate correlated with the percentage of economically disadvantaged students in each school (Kruszewski et al., 2023). Similarly, in vision screening of 71,000 4- to 5-year-old children in Queensland, Australia, using distance acuity and a photoscreener, more children from more disadvantaged areas were referred and more of them were also untestable (Harris et al., 2023). Likewise, a study of 4,365 children screened at ages 4–5 in Tayside, Scotland, with distance acuity and an orthoptist’s assessment of binocularity, found that children living in the most disadvantaged area (worst 20%) were 1.4 times as likely to be referred for failed screening as those in the other areas combined; those who had been rated as at-risk near birth because of family instability were 3 times as likely to be referred as children from families labelled stable (O’Colmain et al, 2016).
Targeted screening can also be implemented as part of a community-based program run as an after-school program, like those offered by the Boys and Girls Clubs in the United States, as a student-run clinic, or at community health centers including federally qualified health centers (Register, 2010). An example of a vision screening community event is Philadelphia’s one-day Give Kids Sight Day, held each year on a college campus. Approximately 1,200 children ages 19 and under receive free eye care (Dotan et al., 2015). The program targets uninsured or underinsured children. Free student-run clinics overseen by faculty eye care professionals include one in Indianapolis, which partners with Indiana University’s School of Optometry to provide vision screening services and referrals to the local county hospital for care (Scheive et al., 2022). Another student-run clinic in Philadelphia provides comprehensive eye exams monthly within a long-term homeless shelter (Henstenburg et al., 2019).
Community health centers in the United States are federally funded facilities that serve the healthcare needs of medically underserved communities through an integrated care model in a team-based practice setting (Lam et al., 2019; McNamara & Polse, 2019). U.S. community health centers also enhance patient acceptance of care and the coordination of care for overall health. The cost of care in U.S. community health centers is based on a sliding fee scale or free, thus overcoming financial barriers faced by most families in medically underserved communities. Even though community health centers are an ideal place for providing vision care service to high-risk populations, only 32% of such centers in the United States provide vision care services (Woodward et al., 2024).
VISION CARE POLICIES IN THE UNITED STATES
The detection of myopia in children is heavily influenced by the U.S. insurance structure and state mandates for comprehensive eye exams or vision screenings. When insurance covers the assessment and/or treatment, some barriers are removed. When some form of vision assessment is mandated, even medically underserved children are likely to get some type of service.
The Affordable Care Act of 2010 requires that all individual, small group, or state-based health insurance plans cover well-child visits and vision care services for children which is one of 10 Essential Health Benefits (Centers for Medicare & Medicaid Services, n.d.b; National Academies of Sciences, Engineering, and Medicine, 2012; Prevent Blindness, 2020). However, the type of coverage mandated for pediatric vision care is decided by each state. Forty-two states cover annual comprehensive eye exams and one pair of prescription glasses per year (Centers for Medicare & Medicaid Services, n.d.b; Prevent Blindness, 2020). Children with Medicaid are entitled to coverage for comprehensive health screenings, including well-child checkups, as part of the federally required Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit (Centers for Medicare & Medicaid Services). In some states, Medicaid also covers comprehensive eye exams and a pair of prescription glasses per year (National Academies, 2016).
Guidelines and Mandates
A few states in the United States require that children have a comprehensive eye exam before entering school, but adherence with this mandate is not universal. For example, Illinois, Kentucky, and Nebraska require that proof of an eye exam be submitted in the first year in which the child is enrolled, although the details of the requirement differ as to how quickly that proof is due and whether it must be conducted by an optometrist or ophthalmologist (Kentucky), other types of physicians (Illinois and Nebraska), or clinic staff (physician’s assistants or advanced practice nurses in Nebraska; Kentucky Department of Education, 2024; State of Illinois, 2024; U.S. Preventative Services Task Force et al., 2022). A 2022-2023 report published by the State of Illinois showed that only 62% (68,349/110,054) of children were reported by schools to have adhered to the mandate (Illinois State Board of Education, 2024). Most states require vision screening instead of a comprehensive eye exam.
A survey of data from September to October 2020 found that 24 states mandated vision screening at school, 9 states mandated that the child must undergo vision screening in the community and produce proof of screening for the school system or other authorities, and 8 states required both, with the details depending on the grade level. Four states (Missouri, Montana, New Hampshire, and South Carolina) only recommended vision screening but did not mandate it. Six states (Alabama, Idaho, North Dakota, South Dakota, Wisconsin, and Wyoming) had no vision screening requirements or recommendations (Wahl et al., 2021). However, at least one state (Alabama) has line-item state funding without a state mandate (State of Alabama, 2024). All states with a vision screening mandate required that the screening be done before or during kindergarten. Some required additional screening in middle school (59%) and/or high school (37%). (See Figure 8-1; Prevent Blindness, 2023.)
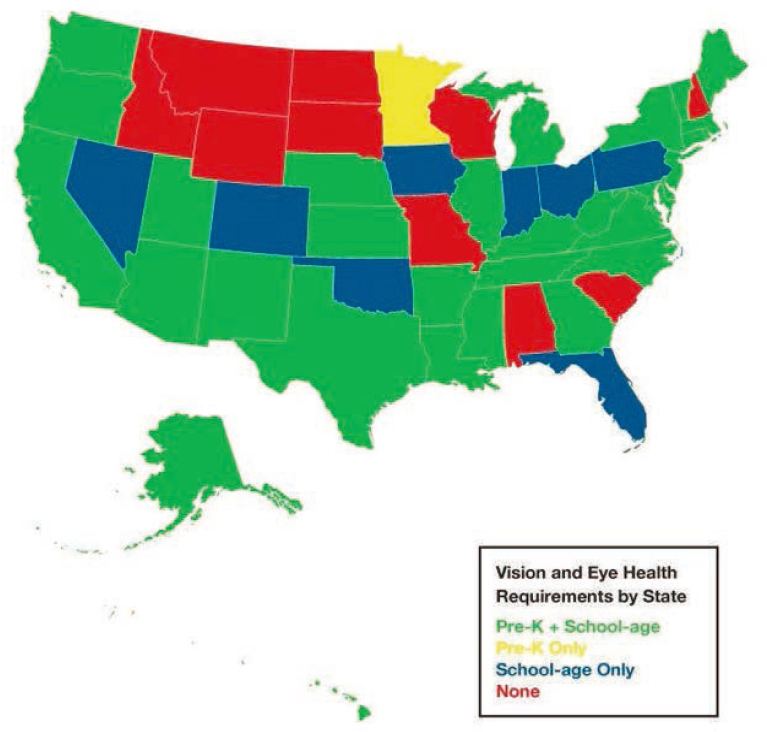
NOTE: The figure shows whether any kind of assessment is mandated by each state (e.g., screening and referral when indicated or comprehensive eye exam). The colors indicate the school ages at which the screening is required.
SOURCE: Prevent Blindness, 2022.
However, funding to conduct screenings is just as important as legislated requirements. A mandate without funding may not be effective, whereas state funding can be effective even without a mandate. For example, Sight Savers America offers screening in 15 states, including Alabama (which has no legislated requirements) and South Carolina (where vision screening is only recommended). In some states, like Alabama, the program includes not only vision screening with the Plusoptix photoscreener but also follow-up care involving a case manager for every child referred for a comprehensive eye exam (Sight Savers America, 2020); over 75% of children who are referred see an eye care professional and receive any prescribed treatment (Sight Savers America, 2020). Of public-school children in Alabama, 60.2% are eligible for free and reduced lunch, which is higher than the national average of 53.3% in 2022–2023 (National Center for Education Statistics, n.d.).
Some consensus exists among vision screening guidelines on the importance of screening and criteria for the identification of vision disorders. Vision screening for children as a preventive strategy for detecting refractive errors, amblyopia, and risk factors for amblyopia is recommended by the World Health Organization (2007); the American Academy of Ophthalmology (American Academy of Ophthalmology Pediatric Ophthalmology/Strabismus Panel, 2018); the American Academy of Pediatrics (AAP), the American Association for
Pediatric Ophthalmology and Strabismus, and the U.S. Preventive Services Task Force (2017). Recommended assessments include a red reflex test, external inspection of the ocular structures, pupil examination, corneal light reflex, cover test, instrument-based screening to detect refractive errors and, where possible, visual acuity (Table 8-3; Donahue & Nixon, 2016).
Age and Recommended Tools
The American Academy of Pediatrics provides the Bright Futures Recommendations for Preventive Pediatric Health Care, which includes recommendations for the assessments that should be done at different ages. They include recommendations for visual acuity screening at various ages (see Table 8-3; American Academy of Pediatrics Committee on Practice and Ambulatory Medicine and Section on Ophthalmology et al., 2003; Bright Futures & American Academy of Pediatrics, 2022). Visual acuity charts for children are recommended as soon as children are capable of cooperating (which is typically age 3 to 4 years). Instrument-based screening is recommended for children 12 months to 3 years to detect risk factors that may lead to vision impairment from amblyopia (amblyopia risk factors; Donahue et al., 2016a). This starting age for visual acuity screening results from the combined facts that younger children cannot be tested reliably with acuity charts and that amblyopia treatment is more effective before about age 8. Instrument-based screening is recommended as an alternative to visual acuity assessments for children ages 3 to 5 years who are unable or unwilling to complete visual acuity screening or who have developmental delays or neurodevelopmental disorders, such as attention deficit hyperactivity disorder (ADHD) or autism spectrum disorder (ASD; Donahue et al., 2016a). Referrals to eye care providers for comprehensive eye examination are recommended if any component of the vision screening is abnormal (Donahue et al., 2016a; Donahue & Nixon, 2016). The American Academy of Pediatric Ophthalmology and Strabismus provides referral criteria for instrument-based screening to detect amblyopia risk factors including myopia (Table 8-4; Donahue & Nixon, 2016). Other organizations such as the American Academy of Pediatrics provide referral cutoffs for visual acuity screening with letter or symbol charts (Donahue et al., 2016a).
TABLE 8-3 Periodicity Schedule for Vision Assessment in Infants, Children, and Young Adults
| Assessment | Newborn–6 mo | 6–12 mo | 1–3 y | 4–5 y | 6 y and older |
|---|---|---|---|---|---|
| Ocular history | x | x | x | x | x |
| External inspection of lids and eyes | x | x | x | x | x |
| Red reflex testing | x | x | x | x | x |
| Pupil examination | x | x | x | x | x |
| Ocular motility assessment | — | x | x | x | x |
| Instrument-based screeninga when available | — | b | x | x | c |
| Visual acuity fixate and follow response | xf | x | x | — | — |
| Visual acuity age-appropriate optotyped assessment | — | — | xe | x | x |
a Current Procedural Terminology code 99174.
b The American Academy of Ophthalmology (AAO) has recommended instrument-based screening at age 6 mo. However, the rate of false-positive results is high for this age group, and the likelihood of ophthalmic intervention is low. A future AAO policy statement will likely reconcile what appears to be a discrepancy.
c Instrument-based screening at any age is suggested if unable to test visual acuity monocularly with age-appropriate optotypes.
d Current Procedural Terminology code 99173.
e Visual acuity screening may be attempted in cooperative 3-y-old children.
f Development of fixating on and following a target should occur by 6 months of age; children who do not meet this milestone should be referred.
SOURCE: Committee on Practice and Ambulatory Medicine et al., 2016. Reproduced with permission from Pediatrics, 137, 28–30, © 2016 by the American Academy of Pediatrics.
| Refractive Risk Factor Targetsa | ||||
|---|---|---|---|---|
| Age, months | Astigmatism | Hyperopia | Anisometropia | Myopia |
| 12–30 | >2.0 D | >4.5 D | >2.5 D | >−3.5 D |
| 31–48 | >2.0 D | >4.5 D | >2.0 D | >−3.0 D |
| >48 | >1.5 D | >3.0 D | >1.5 D | >−1.5 D |
| Nonrefractive Amblyopia Risk Factor Targetsb | ||||
| All ages | Manifest strabismus >8 prism D in primary position Media opacity >1 mm |
|||
NOTE: D = diopters, PD = prism diopters.
a Additional reporting of sensitivity to detect greater-magnitude refractive errors is encouraged.
b For all ages.
SOURCE: Donahue et al., 2013.
BARRIERS TO ACCESSING VISION HEALTH SERVICES IN CHILDREN
In summarizing barriers to vision care, a modified version of Andersen’s Behavioural Model of Health Services Use was utilized to conceptualize the factors that influence access to vision health services for children (Aday & Andersen, 1974, 1981; Andersen, 1968, 1995; Andersen & Davidson, 2007). The model emphasizes the importance of both contextual and individual factors that influence access (see Box 8-2). Andersen’s Behavioural Model of Health Services Use was chosen because it is one of the most widely accepted frameworks for understanding the factors informing access to health care (Aday & Andersen, 1974, 1981; Andersen, 1968, 1995; Andersen & Davidson, 2007). Applying the framework to vision care, an example would be a child with myopia who is screened in school but whose myopia is not detected because of a screening tool with low sensitivity (contextual characteristic). Treatment for their myopia will be delayed (health behavior) which could in turn lead to a mistrust of (predisposing characteristics) and lack of patient/family satisfaction (outcomes) with vision screening programs. Another example is a child with low socioeconomic status (predisposing characteristics) whose family is unable to afford health insurance (enabling resources) and therefore the parents will be less likely to afford or to believe that a comprehensive eye exam (health behavior) is a good value for the money they have to spend; as a result, that child may go without a comprehensive eye exam (health behavior).
BOX 8-2
A Conceptual Framework for Understanding the Barriers to Accessing Vision Care Services for Children
A modified version of the Behavioral Model of Health Services Use was used to conceptualize the factors that influence access to vision health services (vision screening, or comprehensive eye exams) for children (Aday & Andersen, 1968, 1974, 1981; Andersen, 1995; Andersen & Davidson, 2007). The model emphasizes the importance of both contextual and individual factors that influence access (Figure 8-2).
Contextual characteristics are macro- and meso-level factors beyond the child (micro-level) that influence the child’s ability to access vision health services. That is, contextual characteristics are factors in the health system and external environment. Examples include health plans, family units, national healthcare systems, and provider-related and neighborhood factors (Andersen & Davidson, 2007). Children impacted by these factors are either members or residents of these units.
Individual-level characteristics influencing access to vision health services may be predisposing characteristics, enabling resources, and need.
- Predisposing characteristics are pre-existing conditions that indirectly influence a child’s ability to access vision health services. These include a child’s family social structure, health beliefs, and demographic factors.
- Enabling resources support or hinder a child’s access to vision health services. The social determinants of health consist of both predisposing and enabling factors.
- Need represents the conditions that a child, caregiver (perceived need), or a child’s health provider (based on professional judgement and objective measurements, ‘evaluated need’) has identified as needing medical attention and thus resulting in accessing vision health services. Perceived need is determined largely by a child’s (or their caregiver’s) own perceptions of the importance and magnitude of their vision and eye health. Evaluated need on the other hand, informs the type and amount of treatment given to a child after they consult with a vision care provider (Andersen, 1995; Andersen & Davidson, 2007).
Health behavior includes the actual process of accessing or utilizing vision health services that may influence a child’s vision health outcomes. These vision health outcomes are a function of a child’s perceived and evaluated health status and how they feel (satisfaction) about vision health services received. These outcomes influence whether they access vision health services in the future. For example, a caregiver who believes their child has poor vision based on the result of an eye examination by an eye care provider or a vision screening test will feel the need for and likely take action on follow-up appointments for treatment.
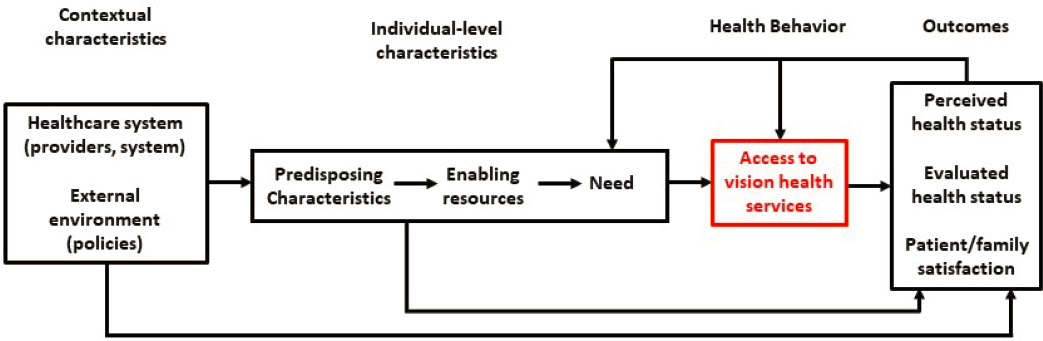
SOURCE: Adapted from Figure 7 in Andersen, 1995.
CONTEXTUAL BARRIERS TO ACCESSING VISION HEALTH SERVICES IN CHILDREN
Contextual Barriers to Vision Screening
Contextual barriers to receiving vision screening include a lack of consensus on the importance and process of vision screening, lack of funding to conduct vision screening, concerns about the accuracy of vision screening tests, instrument malfunction, and limited statewide surveillance of preventive services under the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) Medicaid benefit (Ambrosino et al., 2023; American Optometric Association, 2017; Brener et al., 2007; Donahue & Baker, 2015; Donahue & Nixon, 2016; Donahue et al., 2011, 2016a; Grossman et al., 2017; Levinson, 2010; Lillvis et al., 2020; U.S. Preventative Services Task Force et al., 2017; Wahl et al., 2021).
Lack of Consensus on Importance and Process of Vision Screening
Lack of consensus on the importance and process of vision screening (i.e., types of assessments performed, target age groups, and referral criteria) between states and professional organizations may hinder access to vision screening for children.
Some consensus among professional associations and expert groups has been reached on the importance of routine vision screening of children at risk of myopia progression and other vision disorders (American Academy of Pediatrics, 2003; U.S. Preventative Services Task Force, 2017). This is evidenced by a joint policy statement (published in 2003 and renewed in 2016) supporting early vision screening for children 3 to 5 years and endorsed by the American Academy of Pediatrics (AAP), The American Association for Pediatric Ophthalmology and Strabismus (AAPOS), the American Academy of Ophthalmology (AAOphth), and the American Association of Certified Orthoptists (AACO; Donahue, 2016; Donahue et al., 2016a). The United States Preventive Services Taskforce (USPSTF) also supports the need for vision screening for children aged 3 to 5 years (Donahue et al., 2011; Grossman et al., 2017; Jonas et al., 2017; see Table 8-5). The American Academy of Optometry (AAOpt) endorses the need for both vision
screenings and comprehensive eye exams to ensure the early detection and treatment of vision disorders in childhood (Ciner et al., 2016; Kulp et al., 2016).
There is a lack of consensus among professional groups on the criteria used for referral to eye care professionals, as well as the extent to which such referral is facilitated. AAPOS provides referral thresholds designed for identifying amblyopia risk factors, not myopia. Using the AAPOS thresholds for referral may miss myopia because a child with any myopic refraction before age 6–7 years needs regular follow-up for myopia that is likely increasing with age (Donahue & Nixon, 2016; Grossman et al., 2017).
Vision screening requirements also vary by state (see Figure 8-1) and do not align with professional guidelines (Ambrosino et al., 2023; Wahl et al., 2021). Children might not receive vision screening if they live in a state without vision screening requirements (Lillvis et al., 2020; Wahl et al., 2021). The lack of consensus between states and professional associations may hinder the enactment of additional policies and programs in support of vision care services for children and discourage interested groups such as volunteer and humanitarian organizations from providing vision screening services.
Photoscreening, as described earlier, has been validated as a tool that provides high sensitivity to detect vision disorders in children with ASD (McCurry et al., 2013; Miller et al., 2012; Singman et al., 2013). It is an ideal tool to screen children with ASD and other special healthcare needs because of its unintimidating, largely automated technique, which requires minimal cooperation of the child. Despite this evidence, current vision screening guidelines from the AAP and other professional pediatric and eye care associations do not provide guidance on vision screening for children with ASD (Donahue & Nixon, 2016). Policies to encourage the routine use of photoscreening tools for children at high risk of developing vision disorders are critical to reduce disparities in the provision of vision screening for children. These policies should also address the meager reimbursements by insurance payers in primary care practice for instrument-based vision screening.
| Professional Organization | Vision Disorder | Target Age | Screening Interval | Setting / Personnel |
|---|---|---|---|---|
|
American Academy of Family Physicians (AAFP) Note: AAFP endorses the screening recommendations of the U.S. Preventive Services Task Force; see American Academy of Family Physicians (n.d.) |
Amblyopia, strabismus, anisometropia, astigmatism, hyperopia, myopia | 6 mo–5 y | Not specified | Primary care clinic/family physician, medical assistants or other technicians |
| Joint policy statement by American Academy of Pediatrics, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, & American Association of Certified Orthoptists (Donahue et al., 2016) | Eye tracking disorders, ocular media opacities, strabismus, pupils, refractive error | Newborn–6 y | Newborn–6 mo, 6–12 mo, 1–3 y, 4–5 y, 6 y and older | Primary care clinic/pediatrician, medical assistant or other technicians |
| American Association for Pediatric Ophthalmology and Strabismus (American Association for Pediatric Ophthalmology and Strabismus, n.d.; Arnold et al., 2022) | Eye tracking disorders, retinoblastoma, strabismus, chronic tearing, refractive error | Newborn–5 y | Newborn–12 mo, 12–36 mo, 36 mo–5 y, and repeat screening every 1–2 y after age 5 | During eye exam |
| American Academy of Ophthalmology (Hutchison et al., 2023) | Refractive error (myopia, hyperopia, astigmatism), amblyopia, strabismus, cerebral visual impairment including traumatic brain injury, cataract, retinitis of prematurity, congenital glaucoma, retinoblastoma, pediatric | Newborn–18 y | Newborn–6 mo; 6–12 mo; 1–3 y; 3–4 y; 4–5 y; every 1–2 y after age 5 | Primary care clinic or community setting/physicians, nurses, other health care providers, and lay individuals specifically trained to perform vision screening |
| uveitis, vision, ocular alignment, and the presence of ocular structural abnormalities | ||||
| Joint Policy Statement by the American Academy of Ophthalmology & American Association for Pediatric Ophthalmology and Strabismus (Simon et al., 2016) | amblyopia, strabismus, refractive errors, high-priority on myopia | 3–5 y | Not Specified | Community and school screening programs; primary care clinic |
| American Academy of Optometry (American Academy of Optometry, 2016) | Significant refractive error, amblyopia, strabismus, and observable external ocular disease, color vision deficits | Newborn to < 3 y; preschool; school age | Not Specified | Not specified |
| National Center for Children’s Vision and Eye Health & National Association of School Nurses (Cotter et al., 2015; National Center for Children’s Vision and Eye Health, 2016) | visual impairment—acuity, alignment | Newborn; preschool and up | Neonatal; every month before 6 mo, every 3 mo before 3 y, and every year thereafter | Primary care clinic (well-child visits) |
| United States Preventive Services Task Force (Donahue et al., 2011; Jonas et al., 2017; United States Preventive Services Task Force et al., 2017) | Strabismus, refractive errors, and ocular media opacity; risk factors for vision disorders such as family history in a first-degree relative, prematurity, low birth weight, maternal substance abuse, maternal smoking during pregnancy, and low | 3–5 y | At least once between ages 3–5 y | Primary care setting/pediatrician, family physician, medical assistants and other technicians |
| levels of parental education | ||||
| World Health Organization (World Health Organization, 2024) | Newborn: infections, congenital and/or acquired conditions; Preschool age: reduced visual acuity, amblyopia, strabismus; infection/inflammation; School-age: same as preschool except comprehensive eye exam included |
All ages | Newborn once; early childhood (3–5 y old) once, later childhood (5–18 y old) every 1–2 y, middle to late adulthood (> 60 y old) | Primary care clinic or school program |
SOURCE: Adapted from Harewood et al., 2024.
Lack of Funding to Conduct Vision Screenings
Most states mandate some kind of vision screening, but that mandate is ineffective if funds are not allocated to conduct the screening or to allow effective follow-up with a comprehensive eye exam when warranted. Community-based vision care programs require significant resources, which often negatively impacts their sustainability. Also, instrument-based tools may cost a couple thousand dollars up-front to purchase and bring ongoing maintenance costs, which may make them cost-prohibitive to some programs. In addition, resources need to be sufficient so each child can receive vision screening on a regular basis (Harewood et al., 2024).
Concerns About Accuracy of Screening Methods and Equipment Malfunction
Newer instrument-based vision screening tools developed over the past decade have higher sensitivity and thus lower rates of false negative screening tests. Because of concern about false positive and false negative results, vision screening providers might not refer a child who has vision impairment (‘under referral’) or might refer children that do not have vision impairment (‘over-referral’).
Another concern is that vision screening programs that rely on instrument-based tools may experience interruptions if the tool malfunctions, which can often occur with instrument-based tools. When this happens, not all the children scheduled to be screened that day or in the near future may receive the service. This problem can be overcome by having back-up instruments, although their cost may prohibit the extra purchase.
Limited Statewide Surveillance of Preventive Healthcare Services
Statewide surveillance of preventive healthcare services, especially under Medicaid’s EPSDT program, is important to ensure that low-income children get evidence-based services such as vision screening (Centers for Medicare & Medicaid Services, n.d.a). The EPSDT program requires that vision screening be provided at “reasonable” intervals decided by the States. However, a 2010 examination of nine states (Arkansas, Florida, Idaho, Illinois, Missouri, North Carolina, Texas, Vermont, and West Virginia) by the Office of Inspector General, Department of Health and Human Services, revealed that 60% of children had not received any vision screening (Levinson, 2010; Prevent Blindness, 2020). The nine states indicated they did not monitor the utilization of specific preventive care services (Levinson, 2010). Beginning in 2024, The Center for Medicaid Services will require all states to report annually on the Core Set of Children’s Health Care Quality Measures (Department of Health and Human Services, 2023). However, vision screening and well-child visits in the third, fourth, fifth, and sixth year of life are not included in the core set, even though well-child visits in the first 30 months of life and oral evaluation (dental services) are included (Centers for Medicare & Medicaid Services, 2024; Department of Health and Human Services, 2023).
Contextual Barriers to Vision Screening in Pediatric Primary Care
Contextual barriers to accessing vision screening for children in well-child visits in pediatric primary care include limited physician knowledge of and attitudes about vision screening, perceptions of insufficient time in the clinic workflow, inadequate reimbursement for vision screening, limited number of appointments for well-child visits, and long travel distance
to nearest primary care provider (Guagliardo, 2004; Hered & Wood, 2013; Kemper & Clark, 2006; Marsh-Tootle et al., 2012). Each barrier is discussed in turn, next.
Limited Physician Knowledge
Pediatrician survey responses across three states (Alabama, South Carolina, and Illinois) showed that poorer knowledge and attitudes about preschool vision screening among pediatricians was associated with less likelihood of conducting good pediatric vision screening (Marsh-Tootle et al., 2010). The screener or provider’s lack of self-efficacy with and confidence in vision screening may result in non-referral to an eye care specialist for treatment after an abnormal vision screening test (Anzeljc et al., 2019; Kimel, 2006; Wall et al., 2002). Primary care physicians receive minimal training in the identification and management of myopia and other vision impairment (Hartmann et al., 2006). Limited knowledge in ophthalmology topics may result in over-referral or under-referral of children after vision screening tests.
Perception of Insufficient Visit Time
A potential factor that impedes access to vision screening in pediatric primary care includes provider perceptions of insufficient time to complete recommended assessments in a well-child visit (Hered & Wood, 2013; Kemper & Clark, 2006; Marsh-Tootle et al., 2012). In a single well-child visit, all recommended assessments (per Bright Futures Schedule) are expected to be completed (Bright Futures & American Academy of Pediatrics, 2022; Donahue & Nixon, 2016; Donahue et al., 2016a). When pressed for time, providers may decide to exclude tests (such as vision screening) with meager reimbursement that they perceive to be less of a priority based on a child’s medical history or their initial assessments of the child. This is most likely to occur in community or private clinics that run on a fee-for-service model in which the practitioner’s reimbursement for the screening service is tied to how many children they see (Fairbrother et al., 2001).
Inadequate Reimbursement
Related to a perceived lack of time for vision screening in well-child visits, inadequate practitioner reimbursement of services rendered is a significant deterrent for pediatric primary care providers to conduct vision screening (Hered & Wood, 2013; Kemper & Clark, 2006). This is especially problematic considering the high up-front and maintenance costs of instrument-based screening tools, which may be in themselves prohibitive especially for small pediatric primary care practices (Miller et al., 2012). Reimbursement amounts range between an average of $4 for acuity (chart-based) screening and a median of $24 for instrument-based screening depending on insurance type (Oke et al., 2023). The amount reimbursed varies by state. For comparison, reimbursement for applying fluoride varnish in well-child visits (CPT 99188, which is also a comparatively quick process but with no high-cost equipment) is reimbursed at $14 for Medicaid and up to as much as $35 in commercial plans as of 2019 (Kim et al., 2020). Commercial plans have higher rates of reimbursement for vision screening (CPT code 99177) in the Northeast, West, and parts of the South than the Midwest (Hillrom, 2020). With the increased use of instrument-based screening for young children, the rate of reimbursement for this form of screening has steadily declined since 2013 (Oke et al., 2023). The decision to reimburse may depend on the child’s age and whether or not reimbursement is bundled in the global code for well-child visits. Preventive care services such as vision screening provided under Medicaid’s
EPSDT program are reimbursed at a global rate, and no additional reimbursement is allowed when vision screening is included.
Longer Distance to Providers
Longer distances to health care providers are a recognized barrier to healthcare access in the United States (Guagliardo, 2004). An estimated 1 million children live in areas without access to primary care physicians (Shipman et al., 2011). The number of primary care physicians per 10,000 residents varies across U.S. regions (Guagliardo, 2004). The Northeast, West Coast, Hawaii, Mountain West, and Upper Midwest report higher numbers of primary care physicians per 10,000 residents, as compared with the Great Plains, Lower Mississippi Delta, and Southeast (Guagliardo, 2004). Further variation in the availability of primary care physicians exists between rural and urban regions, with a lower prevalence of primary care physicians in rural areas (Guagliardo, 2004). There is also an uneven distribution of pediatric primary care professionals across the United States, especially as it relates to urban vs rural communities, which leads to significant disparities in access to primary care for children (Drescher & Domingue, 2023; Shipman et al., 2011). Children living in areas with fewer pediatric primary care physicians are six times less likely to have access to primary care than children living in areas with higher numbers of pediatric primary care physicians (Shipman et al., 2011).
Contextual Barriers to Vision Screening in Schools and Communities
Contextual barriers to accessing vision screening in schools or other community settings include variability in state requirements for vision screening in school; limitations due to space, school schedules and calendars; problematic consent processes for children to participate in vision screening; poor communication about the program; and parent socioeconomic barriers (Kimel, 2006; Vongsachang et al., 2020; Wahl et al., 2021). Each of these barriers is discussed in turn in this section.
Variability in State Requirements
There is variability among state requirements with regard to school vision screening. Some children may not get vision screening because they live in states where it is not a requirement or a funding priority (Kindle & Spencer, 2019; State of Alabama, 2024). Even among states that have mandates for vision screening in schools, access is not uniform because private schools are not obligated to adhere to state-mandated vision screening policies (Berntsen & Walline, 2023; Davidson et al., 2016; Nowroozzadeh, 2016; Wolffsohn et al., 2019; Zadnik et al., 2015).
Limited Space or Scheduling Time
Vision screening sessions organized in schools or other community settings are often limited by the availability of space for screening, school schedules, and calendars (Vongsachang et al., 2020). Vision screenings can only be performed when school is in session, on specific days, and during specific hours dictated by school administration. Also, vision screening may require rooms that are large enough to measure distance visual acuity, and in the case of instrument-based tests sufficiently dark rooms with no distractions. There may not be a space available that meets these requirements. Children may also miss out on screening if they are absent from school on a scheduled day and the screeners do not return to pick up previously
absent children. In one Canadian program conducted in a variety of communities (rural and urban; high-needs and non-high needs), on average 6.9% of eligible children missed screening because they were absent from school (range across 43 schools, 1.5–14.3%; Nishimura et al., 2020).
Complex Parent/Guardian Consent Process
The consent process in school-based screening programs may hinder access to vision screening for school children (Vongsachang et al., 2020). Consent forms are usually sent home with children for parents to grant permission for their child to participate in vision screening and other preventive care activities. Children may forget to pass on consent forms or lose them before they get home. Parents are often required to read, sort and complete several consent and information slips at a time. Therefore, they may lose or forget to complete consent forms. School-based screening programs are typically free with no out-of-pocket or insurance requirements (Vongsachang et al., 2020). Parents may not be aware of this and therefore not provide consent if they believe their children are not eligible for free service (Vongsachang et al., 2020). Parents with socioeconomic barriers may particularly struggle to keep up with consent forms and other permission slips for school-based screening.
Contextual Barriers to Comprehensive Eye Exams and Treatment
Barriers to comprehensive eye exams and treatment include poor provider-patient communication of results of a vision test, low reimbursement rates for rendering eye care, low supply of eye care specialists willing to see children, lack of affordable prescription glasses and poor compliance with wear (Anzeljc et al., 2019; Feng et al., 2020; Hartmann et al., 2006; Kemper et al., 2003; Kimel, 2006; Killeen et al., 2021; Kodjebacheva et al., 2015; Lee et al., 2012, 2023; Saydah et al., 2020; Varadaraj et al., 2019; Vongsachang et al., 2020; Wall et al., 2002; Williams et al., 2013).
Poor Communication with Parents
Poorly communicating the results of a vision screening test or comprehensive eye exam may prevent access to treatment (Kimel, 2006; Williams et al., 2013). Children may not get follow-up comprehensive eye exams because their parents did not understand or know their children had an abnormal vision screening test requiring a comprehensive eye exam (Kimel, 2006; Williams et al., 2013), which in turn may be the result of a lost ‘pink slip’ (referral slip) in a school screening (Vongsachang et al., 2020). In well-child visits, where pediatric primary care providers have direct access to parents or caregivers, providers may not have clearly communicated the importance of follow-up care to parents, or parents may not have understood the importance due to language barriers or lack of language concordance with providers (Williams et al., 2013).
For instance, in a study by Frazier et al. (2009), Hispanic immigrant parents reported that they had not sought eye care for their children because of a lack of information about the importance of eye care for children along with language barriers. Interviews in the Midwest with parents whose children attended high-needs schools in kindergarten through Grade 5 revealed financial concerns (31%), including an apparent concern that Medicaid exams and glasses were substandard, and logistical barriers (difficulty scheduling, 22%) as reasons for not receiving an eye exam after failing vision screening; other reasons included appointments being too far in the
future [16%]; Kimel, 2006; see Wang et al., 2023 for similar Canadian data). After initial diagnosis and starting treatment, breakdown in communication may also occur between eye care providers and parents whose children need regular follow-ups with eye care professionals.
Low Reimbursement Rates
Reimbursement rates for vision care services are a barrier to accessing treatment from eye care professionals, who are less likely to see patients with Medicaid insurance than those with private insurance (Biviji et al., 2024; Lee et al., 2018). This may be because of the lower reimbursement associated with Medicaid insurance compared to private insurance (Blanchard et al., 2008). Households with lower incomes may be unable to afford higher-premium commercial health insurance plans, such as preferred provider organization (PPO) plans which give more flexibility to see eye care specialists even outside of their network.
Low Access to Eye Care Professionals
Access to eye care professionals is also limited by low availability, especially in rural and low-income communities, despite an increasing demand for eye care providers (optometrists and ophthalmologists) in the United States (Berkowitz et al., 2024; Feng et al., 2020; Kodjebacheva et al., 2015; Lee et al., 2007, 2023; Siegler et al., 2024). Data from the National Center for Health Workforce Analysis (NCHWA) indicates that across 38 medical and surgical specialties, ophthalmology is projected to have the second worst rate of workforce adequacy (projected supply over projected demand), a rate of 70%, by the year 2035 (Berkowitz et al. 2024). From 2020 to 2035, a 12% decline in supply of ophthalmologists and a 24% increase in demand are expected, indicating a workforce adequacy of just 30% overall, including a 77% vs. 29% workforce adequacy in metro versus nonmetro geographies, respectively (Berkowitz et al. 2024). Importantly, despite identifying nearly 600 pediatric optometrists and just over 1,000 pediatric ophthalmologists in the United States, 96.4% of U.S. counties had neither a pediatric optometrist nor a pediatric ophthalmologist (Siegler et al., 2024). Additionally, counties with neither type of pediatric eye care specialist had the lowest mean household incomes (Siegler et al., 2024).
The density of pediatric ophthalmologists in the United States has decreased significantly since the early to mid-2000s, with little possibility of improvement given the fact that fewer residents are pursuing pediatric ophthalmology fellowships (Lee et al., 2023; Simon et al., 2007). The lower number of pediatric ophthalmologists results in less access to specialist eye care, longer wait times, and longer travel times, especially for children living in rural parts of the United States (Kodjebacheva et al., 2015; Simon et al., 2007). States with the lowest number of pediatric ophthalmologists include North and South Dakota, Delaware, Idaho, and Wyoming (Lee et al., 2023). Increases in the density of optometrists from 1990 to 2017 have resulted in adequacy (100%) of optometrists, but an 89% workforce inadequacy is expected by 2035 under the reduced barriers demand scenario (Berkowitz et al., 2024; Feng et al., 2020).
Similar inadequacies of 60% are expected in the optician workforce by 2035 (Berkowitz et al., 2024). The Health Workforce Simulation Model from the National Center for Health Workforce Analysis describes the demand for physicians under 2 scenarios which include the reduced barriers scenario. The reduced barriers scenario estimates the number of physician full-time equivalents (FTEs) required if populations who historically faced barriers to accessing health care services demonstrated care use patterns comparable to populations perceived to have fewer barriers to accessing care. Therefore, this scenario describes the implications for physician
demand if policies and programs are implemented to reduce access-based disparities to healthcare services (Berkowitz et al., 2024).
This maldistribution of eye care professionals in the United States, especially for rural communities, leads to significant disparities in access to primary and specialist eye care for children (Drescher & Domingue, 2023; Shipman et al., 2011). Less access to specialist care leads to poor vision health outcomes, especially for children with asymptomatic conditions such as myopia and amblyopia, which require early identification and treatment to slow myopia progression and prevent irreversible vision loss, respectively (Lee et al., 2023). An area where the supply of eye care providers is particularly low is in community health centers (Shin & Finnegan, 2009). In a policy brief by Shin and Finnegan published in 2009, seven out of 10 community health centers were reported to not have on-site eye care professionals to provide comprehensive eye exams because of an inability to afford the required space and equipment and/or difficulties creating business plans, designing an appropriate space for eye examinations, and creating an inventory of necessary equipment for eye examinations (Shin & Finnegan, 2009).
High Cost of Prescription Glasses and Compliance with Wear
The cost of prescription glasses is a barrier to treatment for myopia, especially for children with low socioeconomic status (Kemper et al., 2003; Killen et al., 2021; Kodjebacheva et al., 2015; Saydah et al., 2020; Varadaraj et al., 2019). When that barrier is eliminated and its removal is communicated clearly to parents, more children receive treatment. For example, a summer program for children in inner-city Philadelphia that comprised vision screening, immediate follow-up, and two pairs of free glasses if needed found that most parents (64%) came because the program included free glasses (Dotan et al., 2015). (Most [77%] of the children receiving the glasses were myopic.) Concern about the affordability of glasses can also lead parents to not book the referral appointment.
Children who are provided free glasses to correct their myopia, when compared to children for whom the glasses must be purchased by the parents, are more likely to be found wearing glasses and have increased academic performance even with imperfect compliance with glasses wear (Ethan et al., 2010; Ma et al., 2014). A systematic review of randomized controlled trials, mostly conducted in China, provides evidence from 11 studies that children are 2.45 times more likely (odds ratio of 2.45) to be wearing prescribed glasses at an unexpected follow-up visit if they are provided at no charge than if the parents only received a letter with the prescription (Wu et al., 2023). The effect was smaller with longer follow-up time (odds ratio of 2.30 after 6–12 months vs. 3.18 with earlier follow-up). Compliance was higher when the refractive error was higher or visual acuity was poorer. Nevertheless, in some of the RCTs, less than half the children who received free glasses were wearing them at follow-up.
INDIVIDUAL-LEVEL BARRIERS
Predisposing Characteristics Hindering Access to Vision Screening, Comprehensive Eye Exams, and Treatment for Children
Predisposing characteristics that may hinder access to vision screening and treatment include a child’s age, race, ethnicity, mental and physical disabilities, sex, and social determinants of health. Parental factors include parental health beliefs, mistrust and
misconceptions, and mental and physical disabilities (Antonio-Aguirre et al., 2024; Asare et al., 2022; Child and Adolescent Health Measurement Initiative, 2024; Elam et al., 2022; Frazier et al., 2009; Hoover et al., 2023; Killeen et al., 2023; Kimel, 2006; Kodjebacheva et al., 2011, 2015; Muhammad & Tumin, 2022; Qui et al., 2014; Rajesh et al., 2023; Repka et al., 2023; Sharma et al., 2016; Swanson et al., 2020; Varadaraj et al., 2019; Vongsachang et al., 2020; Williams et al., 2013). In this section we report race and ethnicity categories as used in the original articles.
Child’s Age
Younger children are less likely than older children to get vision screening, comprehensive eye exams, or treatment, regardless of socioeconomic status (Antonio-Aguirre et al., 2024; Hoover et al., 2023; Killeen et al., 2023; Muhammad & Tumin, 2022; Repka et al., 2023) Based on nationally representative data from the 2018 and 2019 National Survey of Children’s Health, parents reported that only 7% of children under age 6 received a vision test in school, 28% in primary care, and 10.2% in eye clinics (Table 8-6; Child and Adolescent Health Measurement Initiative, 2024). From the age of 5 years, when children are usually enrolled in school, they have more structured visual tasks (reading, writing, drawing, etc.) and therefore are more likely to recognize and seek help for any impaired vision. Vision screening is also more likely to be offered in the child’s school or checked as part of a well-child visit for school-aged children. Many eye care providers do not offer appointments for young children. For example, a study of every eye care practice (ophthalmologists and optometrists) that could be identified in Arizona (over 1,000 eye care practices) found that only 41% would accept children under the age of 6 years (Biviji et al., 2024).
| Age (years) | Setting for Vision test (%) | No Vision Testing | |||
|---|---|---|---|---|---|
| School | Primary Care | Eye Clinic | |||
| 0–5 | Row % | 6.7 | 27.8 | 10.2 | 58.7 |
| CI | 5.9–7.5 | 26.5–29.2 | 9.4–11.0 | 57.2–60.2 | |
| Sample count | 1,250 | 4,867 | 1,978 | 9,299 | |
| Population estimate | 1,564,386 | 6,503,574 | 2,383,714 | 13,726,380 | |
| 6–11 | Row % | 22.7 | 33.9 | 38.7 | 23.5 |
| Confidence interval | 21.5–24.0 | 32.5–35.3 | 37.3–40.2 | 22.1–24.9 | |
| Sample count | 4,583 | 5,953 | 7,466 | 3,889 | |
| Population Estimate | 5,572,228 | 8,299,418 | 9,479,673 | 5,752,331 | |
| 12–17 | Row % | 11.0 | 22.4 | 51.6 | 25.8 |
| Confidence interval | 10.1–11.9 | 21.2–23.6 | 50.1–53.0 | 24.5–27.1 | |
| Sample count | 2,594 | 5,230 | 13,323 | 6,131 | |
| Population estimate | 2,731,975 | 5,580,245 | 12,846,902 | 6,425,703 | |
NOTES: Rows do not add up to 100% because vision testing could be reported in more than one location and this is not an exhaustive list of settings for vision testing. CI = confidence interval.
SOURCE: Data obtained from interactive data query of the National Survey of Children’s Health (https://www.childhealthdata.org).
Racial and Ethnic Disparities
There are racial and ethnic disparities in accessing vision screening, comprehensive eye exams, and treatment (Antonio-Aguirre et al., 2024; Kodjebacheva et al., 2011; Stults et al., 2024; Varadaraj et al., 2019). A retrospective study, undertaken with data from electronic health records linked to census data for over 20,000 children aged 3 years with a well-child visit to the Palo Alto Medical Foundation in Northern California, reported lower rates of vision screening for Black and Hispanic children compared with Asian and White children (Asian, 73.1%; Black, 58.5%; Hispanic, 63.5%; White, 74.3%; p < 0.001; Stults et al., 2024). The only options for race and ethnicity in the electronic health record used were Asian, Black, Hispanic, White, other (American Indian, Multiracial, Native Hawaiian, and Other Race not further specified), and unknown. Another study using nationally representative and population-based survey data of randomly sampled households (U.S. Census Bureau, 2023) reported that compared to non-Hispanic White children, Hispanic children and those from other non-Hispanic groups (Asian, American Indian or Alaska Native, Native Hawaiian, other Pacific Islanders, and those with two or more races) in the United States are less likely to get vision screening (Antonio-Aguirre et al., 2024). However, after adjusting for key sociodemographic characteristics (specifically, age, children with disabilities, healthcare visits in the past 12 months, insurance type, primary household language, parents’ education, and household income) there is no difference in the likelihood of vision screening or comprehensive eye exams among these groups (Antonio-Aguirre et al., 2024).
Race is a social construct without genetic or biological association (Williams & Eberhardt, 2008). Therefore, this discrepancy in the association between race, ethnicity, and the likelihood of vision screening before adjusting for sociodemographic characteristics suggests that socioeconomic disadvantage related to the history of colonization, racial and ethnic discrimination, and the existence of a social gradient of power and privilege explain most of the disparities in access to vision screening experienced by members of minority racial or ethnic groups (Antonio-Aguirre et al., 2024; Elam et al., 2022; Furtado et al,, 2023; Hamm et al., 2021). This has been demonstrated for many other health outcomes and highlights the importance of considering both race, ethnicity and socioeconomic factors to understand health disparities (Robert Wood Johnson Foundation Commission to Build a Healthier America, 2009).
There are also disparities in the receipt of treatment for vision impairment. Children 12 years and older who are Mexican American or non-Hispanic Black have considerably higher odds of having inadequate refractive correction when they have poor vision compared to non-Hispanic White children, with the biggest disparity observed in children 12 to 19 years of age, according to data from NHANES 2005 to 2008 (Qiu et al., 2014). This was determined by measuring the proportion of children with poor visual acuity (worse than 20/40 with any refractive correction the child already had) that could be improved (to 20/40 or better with a first or better pair of glasses), that is, the proportion of children with uncorrected and under-corrected refractive error (Qui et al., 2014). Also, among first-grade children, Non-Hispanic Black/African American and Latino children are more likely than Non-Hispanic White children to not have prescription glasses despite having poor vision, as determined in a comprehensive eye exam by
an ophthalmologist (adjusted odds ratios of 1.75 and 1.50 respectively adjusting for school, age, sex, and year; Kodjebacheva et al., 2011). (Options for race and ethnicity were non-Hispanic White, Latino, Non-Hispanic Black/African American, Asian/Pacific Islander, and other or mixed races/ethnicities.)
Furthermore, some instrument-based tools have problems screening children with dark irises, which may contribute to Black and Asian children having a lower likelihood of successful vision screening (Vaughan et al., 2010). The challenge with colored irises is especially problematic, because it perpetuates inequities in access for non-White populations, which have and are projected to continue to have the highest number of vision impairment cases through 2060 (Varma et al., 2017). The inequity will continue whenever vision screening is based solely on instrument screening. It also provides an additional justification for facilitating follow-up with a full comprehensive eye exam for children who cannot be screened.
Similar disparities are evident in treatment for strabismus. Using the American Academy of Ophthalmology’s database known as the Intelligent Research In Sight (IRIS) Registry, which includes data on patient visits from electronic health records, Black, Hispanic, and Asian children with strabismus are found to be less likely to receive strabismus surgery, with a longer delay between diagnosis and surgery compared with White children after adjusting for insurance status (Rajesh et al., 2023; Repka et al., 2023). The IRIS Registry version used for the analysis provided a single variable for race and only had patient race categories of White, Black or African American, Asian, and other. While these findings regarding delays in receiving strabismus surgery may be partially explained by the variability by race and ethnicity in the incidence of refractive amblyopia risk factors, this may also reflect the under-diagnosis of amblyopia in non-White groups relative to the actual prevalence of strabismus (exotropia). Also, regardless of insurance status, Black children had a higher probability of experiencing residual amblyopia with strabismus (exotropia), compared to White children (Rajesh et al., 2023).
Children with Disabilities
Despite an increased risk for eye disease, children with disabilities such as those with autism spectrum disorder (ASD), Down Syndrome, or behavioral problems are less likely to get vision screening or comprehensive eye exams and are more likely to have unmet vision needs (Guo et al., 2022; Haller et al., 2022; Heslin et al., 2006; Hoover et al., 2023; Kimel, 2006; Silverstein et al., 2021; Swanson et al., 2020). Children with ASD have lower rates of vision screening at well-child visits than children who have not been diagnosed with ASD (Swanson et al., 2020). This is especially evident among young and Black children with ASD (Swanson et al., 2020). Non-Hispanic Black children with ASD also have lower rates of vision screening compared to non-Hispanic White children with ASD after adjusting for insurance, sex, developmental delays, and geographic region (Hoover et al., 2023).
Sex
Sex is associated with access to vision care (Antonio-Aguirre et al., 2024; Asare et al., 2022; Hoover et al., 2023). Male children are significantly less likely to get vision screening in well-child visits than females after adjusting for insurance type, race, ethnicity, ASD, developmental delays, sex, and geographic region (Hoover et al., 2023). Both referrals to eye care providers after an abnormal vision screening test and visits to an eye doctor are more likely in female than in male children (Antonio-Aguirre et al., 2024). However, this observation may be
due to the higher prevalence of vision disorders in females compared to males (Vitale et al., 2008; Xiao et al, 2015).
Social Determinants of Health and Interrelated Factors
Social determinants of health are “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks” (Healthy People 2030, n.d.; WHO, 2024a). Socioeconomic status, a social determinant of health, is a measure of an individual or family’s economic and social position in relation to others in society measured by income, education and occupation. Socioeconomic status of children is informed by their parents’ highest level of education, income, and employment (Dutton & Levine, 1989). Socioeconomic status and other social determinants of health such as household language may hinder access to vision screening, care, and treatment, including the use of prescription glasses in children (Adler et al., 1994, 2019; Antonio-Aguirre et al., 2024; Asare et al., 2022; Elam et al., 2022; Kimel, 2006; Sharma et al., 2016; Vongsachang et al., 2020; Williams et al., 2013).
Data from the 2021 National Survey of Children’s Health indicate that social determinants of health continue to affect access to vision care in the United States (Antonio-Aguirre et al., 2024). Based on parental report, only 53% of children had a vision screening in the past 2 years. Children were less likely to have had vision screening—with odds adjusted for age, race, ethnicity, sex, special needs, health care visit in the last 12 month, insurance type, primary household language, parents’ education, and household income—if they were younger than 3 years, had no insurance, did not have special health needs, had no health visits in the last year, had parents without more than high school education, or lived in a household with lower income (< 200% of the federal poverty level).
Referrals to eye care providers after an abnormal vision screening test were more likely for older children (aged 6 to 17 years vs 5 and under), female children, any ethnicity other than non-Hispanic White, and children with special needs, lower income (< 200% of the federal poverty level), or a primary language other than English. These factors were confounded by the odds of having had a visit to the eye doctor: that occurred for only 38.6% of the children and was more likely for older children (aged 3 to 17 vs. under 3), female children, special-needs children, children with a health visit in the last year, when there was some form of health insurance, and when English was the primary language. At every point, children with no health insurance were less likely to get vision screening or a visit to an eye doctor.
Parents with low health literacy, less education, or language barriers are less likely to understand the process of consenting to their children getting vision screening (Vongsachang et al., 2020). In focus groups on eye care undertaken with Hispanic immigrant parents, the parents reported a lack of knowledge about health care coverage for eye exams (Frazier et al., 2009). Low health literacy hinders access to vision health services for children. Parents with higher levels of education may have higher health literacy and may be more likely to be employed and have higher income. Parents with low socioeconomic status may find it particularly difficult to get permission to be absent from work to attend clinic appointments during the day (Kimel, 2006; Williams et al., 2013; Wolf et al., 2021).
Related to difficulties with permissions to be absent from work, parents may have competing priorities preventing them from attending appointments for well-child visits and comprehensive eye exams (Kimel, 2006). These competing priorities may be related to concerns about basic needs such as food and housing, household structure (single-family homes, multiple
child households, foster care), multiple jobs, and precarious work (Kimel, 2006). Parents may have precarious jobs or other unpredictability in their schedules and therefore be unable to schedule appointments further than 1–2 weeks in advance or may have difficulties getting appointments within the preferred time frame (Kimel, 2006; Kodjebacheva et al., 2011). They also may not have flexibility in their work schedules to attend clinics for health care visits during work hours.
Related to unpredictable schedules and competing priorities, parents report difficulties with remembering scheduled appointments (Kimel, 2006). Also, parents with low health literacy may face increased challenges with scheduling appointments with eye care professionals (Collins et al., 2022b; Dudovitz et al., 2015; Kemper et al., 2006; Kimel, 2006). These challenges may lead to missed preventive care visits for children. Structural racism may indirectly contribute to such social disadvantages in racial and ethnic minoritized populations (Elam et al., 2022).
Parental Health Beliefs and Mistrust of Health Care Systems
Parents may develop a mistrust in vision screening because of high false-positive rates (Couser & Smith-Marshall, 2011; Frazier et al., 2009; Zhou et al., 2023). They may doubt the accuracy of vision screening results, question the safety of the vision screening process, or entertain fears about their children’s inclusion in research studies without their permission (Kimel et al., 2006; Vongsachang et al., 2020). Some parents question whether the screening personnel are licensed or qualified (especially in school screening programs) or may be uncomfortable sharing personal information on consent forms (Vongsachang et al., 2020). Other parents may have mistrust in a school vision screening program if vision impairment they are already aware of is not detected in a vision screening test (Kimel, 2006). A survey of patients in a free clinic in Michigan showed that prior negative experiences with the health care system and subsequent lack of trust in the health care system were reasons for not acquiring glasses (Killeen et al., 2023). More than one-third of parents in the Midwest who have children in kindergarten through Grade 5 in a high-needs school did not follow up by booking an eye exam because they did not believe the results of the vision screening (38%) or did not believe the child needed a follow-up exam (29%; Kimel, 2006).
Parents with Mental and/or Physical Disabilities
Parents with physical or mental disabilities may be unable to offer consent for their children to attend vision screenings or may have trouble scheduling referrals (or follow-through with follow-up eye exams) because of their disability (Kimel, 2006).
Enabling Factors Hindering Access to Vision Screening, Comprehensive Eye Exams, and Treatment for Children
Enabling factors that present barriers to accessing vision care in U.S. children include type and lack of health insurance, household income, transportation, and household structure (Antonio-Aguirre et al., 2024; Centers for Medicare & Medicaid Services, n.d.; Killeen et al., 2023; Kimel, 2006; Kodiebacheva et al., 2015; Muhammad & Tumin, 2022; Newacheck, Hughes, & Stoddard, 1996; Prevent Blindness, 2020; Rajesh et al., 2023; Repka et al., 2023; Swanson et al., 2020; Syed et al., 2013; Williams et al., 2013; Zhang et al., 2012).
Type and Lack of Health Insurance and Household Income
In the 2018 to 2020 National Survey of Children’s Health, parents reported that uninsured children were 41% less likely to get a vision test in pediatric primary care compared to children with private insurance, after adjusting for sex, race and ethnicity, household language, preventive health visit in the past year, and having special health care needs (Killeen et al., 2023). Similarly, children with public insurance were 24% less likely to get vision screening in pediatric primary care compared to children with private insurance, after adjusting for race, ethnicity, ASD diagnosis, developmental delays, sex, and geographic region (Killeen et al., 2023; Swanson et al., 2016). Data from the IRIS Registry demonstrate that Medicaid recipients have much lower chances than other patients of being successfully treated for amblyopia and are more likely to have residual amblyopia, after adjusting for key variables such as age, sex, race and ethnicity (Rajesh et al., 2023; Repka et al., 2023). A “secret shopper” survey conducted on over 1,000 ophthalmologist and optometrist practices in Arizona found that up to 74% of practices did not accept children covered by Arizona’s Medicaid program, the Arizona Health Care Cost Containment System (Biviji et al., 2024).
Even when a child has insurance, co-pays for well-child visits and comprehensive eye exams, disparities in accessing vision care for children remain (Zhang et al., 2012). This is evident in studies conducted in Canada, where disparities in access to comprehensive eye exams remain for children with low socioeconomic status despite universal health coverage (Asare et al., 2022; Jin & Trope, 2011). One such study, conducted in Ontario, Canada, with linked health administrative and demographic data for children under the age of 8 years, found that children with high socioeconomic status were 43% more likely to have had a comprehensive eye examination than children with low socioeconomic status despite universal health insurance covering the cost (Asare et al., 2022). Similarly, in the United States, even among those with health insurance, children from low-income households are less likely to access eye care services by an eye care professional compared to children from high-income households (Asare et al., 2022; Kimel, 2006; Stein et al., 2016).
Despite requirements by the Affordable Care Act for health plans to cover pediatric vision care services, co-pays may be required in older, “grandfathered” health plans that existed prior to the enactment of the Affordable Care Act. Co-pays may also be required in short-term plans (less than 12 months), federal employee plans, some government plans, and membership plans like faith-based cost-sharing services (Center for Consumer Information Insurance Oversight, 2022; Prevent Blindness, 2020). People who work for larger companies (more than 100 employees) or who are self-insured are not covered by Essential Health Benefits of the Affordable Care Act (Center for Consumer Information Insurance Oversight, 2022). In addition, there is variation among states in the benefit for the provision of eye glasses (Center for Consumer Information Insurance Oversight, 2022; Prevent Blindness, 2020).
Transportation
Longer travel distances to healthcare providers, especially for children living in rural (as compared with urban) communities, are exacerbated for children who do not have a reliable form of transportation (Kimel, 2006; Kodjebachva et al., 2015; Newacheck et al., 1996; Syed et al, 2013). This is typically experienced by children experiencing poor social determinants of health (Syed et al., 2013).
Household Structure
Households with multiple children, single parents, or foster-care situations present unique circumstances which may prevent access to comprehensive eye exams and compliance with treatment for children. Coordinating schedules for large families can be difficult or even impossible in such households. Also, single parents may lack a shared caregiver and be overwhelmed with work and family responsibilities. The lack of a consistent home can also lead to difficulties scheduling appointments because caregivers may not know where a child will be on any given day (Kimel, 2006).
Factors Related to Need that Hinder Access to Vision Screening, School Screening, Comprehensive Eye Exams, and Treatment for Children
Factors related to perceived and evaluated need include false positive and negative tests, low health literacy, cultural beliefs, and mistrust of vision screening results (Kimel, 2006; Vongsachang et al., 2020).
False Positive and Negative Screening Tests
False positive and negative vision screening tests impact a patient’s decision to seek eye care. They cause a false sense of security or psychological stress and result in unnecessary use of resources.
Low Health Literacy, Cultural Beliefs and Mistrust of Vision Screening Results
Parents with low health literacy may not understand pediatric vision disorders such as myopia and the impact of delayed vision care and poor vision on learning, and therefore fail to understand the urgency of vision care for their children (Kimel, 2006; Vongsachang et al., 2020). In focus groups with Hispanic immigrant parents to discuss eye care, parents noted that the higher frequency with which children wore glasses in the United States compared to their home countries was worrisome and likely due to something potentially harmful in the environment (Frazier et al., 2009). Alternatively, or in addition, parents may lack a cultural acceptance of prescription glasses and therefore not believe that their children need them (Frazier et al., 2009).
Many Native populations mistrust healthcare services, which together with a lack of cultural safety (which is an inability to safely practice cultural traditions within Western medical settings) contribute to vision disparities (Burn et al., 2021). Barriers based on personal and cultural beliefs, together with poor health literacy, have been shown to disproportionally impact racial and ethnic minority populations (Burn et al., 2021; Yashadhana et al., 2020).
Physicians can help improve access to vision care by following recommendations like those in Box 8-3, which increase the efficiency of screening and leave time for explaining the results and encouraging the follow-up and continuing care that are needed once an eye problem is identified.
BOX 8-3
10 Clinical Practices to Improve Vision Care Access, Adherence, and Continuity
- Successful screening tools can be inexpensive and low-tech (visual acuity testing using optotypes) or more expensive and higher tech (instrument-based). Increasing access to care should be based on local resources available.
- If a child fails an in-office screening, refer and follow up.
- Both referral and follow up care should be case managed and confirmed.
- If a child has had a previous vision screening and passed, repeat screening in office. If failed, refer and follow up. If a child has had a previous vision screening and failed, do not rescreen. If a child fails, believe it. Utilize time to encourage follow up care.
- Avoid passing a previously failed screening. False negatives are the worst outcome.
- If a child has an eye doctor or wears glasses or has a history of wearing glasses, do not rescreen. Utilize time to encourage follow up care with the same eye doctor. Underscore that the eye doctor should take care of the eyes and vision.
- A physical exam of the eyes is likely not enough. Children who are myopic can often function quite well and may have no clinically observable signs of myopia.
- Developmental delay constitutes a failed vision screening. Children with special needs fail by history alone. Conversely, high myopia discovered in a comprehensive eye exam may be a dysmorphic feature that contributes to conditions of broader developmental delay.
- If glasses do not appear to help the child, encourage glasses wear and regular follow up with the eye doctor. Blur despite glasses indicates amblyopia. Children who not wear glasses at a young age and who have amblyogenic factors may never have clear vision.
- If a child is seen by an eye doctor who doesn’t dilate the child’s eyes, choose another eye doctor.
Consequences of Poor Communication of Test Results and False Results
Families’ experiences with vision health services, whether vision screening or a comprehensive eye exam, impact their future use of vision health services. Therefore, barriers to future use of vision health services include poor communication of results of a vision test, false positive and negative vision screening results, and patient and family dissatisfaction with services received.
Poor communication of results of a vision screening or comprehensive eye exam by the service provider to the child or family may give parents the false perception that their child has good vision (perceived health status) and therefore hinder follow-up care for treatment of vision impairment. On other occasions, the parents may perceive that any prescribed treatment is all that is needed with no call for follow-up.
A false positive or negative vision screening result may lead to under-referral or over-referral. As a result of false positive and negative tests, parents may lack confidence in or not be satisfied with vision screening tests. Children or families that are not confident in or satisfied with the care received might not consent to future vision screenings or may not attend follow-up appointments with an eye care provider.
BARRIERS TO RESEARCH TO ACCESS TO PEDIATRIC VISION SCREENING, COMPREHENSIVE EYE EXAMS, AND TREATMENT
Despite recent calls to action by the World Health Organization and the Lancet Commission on Global Eye Health (Burton et al., 2021) for increased research on improved access to vision care for children, there are significant barriers to conducting research on access to vision screening, comprehensive eye exams, and treatment (Burton et al., 2021; WHO, 2019). These barriers include poor data collection for surveillance, limited funding to conduct research, ethical concerns about randomized trials, and poor representation of minoritized populations in research.
Lack of Data Collection for Surveillance
Variability in vision screening policy mandates across U.S. states hinders the collection of standardized surveillance data for research that could inform the development of programs and policies. Similarly, the collection of standardized data is hindered by the poor collection of data on sociodemographic factors such as race vs ethnicity and sex vs. gender.
Limited Funding
There is limited funding to conduct research on the topic of access to care and pediatric populations (Arnold et al., 2018a; Pober et al., 2001; Sung et al., 2003). Few foundations have shown interest in funding population-based research, and when they are interested, the funding is often relatively minimal. For this reason, researchers compete for mainstream funding from federal institutions that have historically favored basic science and adult research (Arnold et al., 2018a; Hunter, 2013; Marzolf et al., 2017; O’Hara, 2016). One of the implications of limited funding for population-based research in the vision-care space is the plethora of cross-sectional, observational studies and secondary data studies that, while important, are limited in the conclusions and impact they can make. Longitudinal and randomized studies are needed to determine the long-term impacts of interventions in populations. However, research funding to conduct such important studies is limited.
Ethical Concerns Regarding the Conduct of Randomized Trials in Children
Randomized trials are essential for determining the efficacy of interventions to improve access to care for children and ultimately to improve health outcomes. However, these studies are rare because of limited funding and, when they do occur, are not adequately powered (Donahue et al., 2013; Jonas et al., 2017). Historically, there has been significant reluctance by caregivers, health care providers, educators, and institutional review boards to include children in clinical trials because of concerns about harming them by withholding treatment from control groups (Arnold et al., 2022; Rajalakshmi & Rajeshwari, 2019; Wahl et al., 2021). The International Myopia Institute (IMI) suggested that it remained ethical to randomize to control in its 2021 statement (Jong et al., 2021). In its 2023 digest, the IMI suggests (Sankaridurg et al., 2023):
Ultimately, ethical questions are best answered region by region, with the availability of on-label myopia control modalities and the prevailing standard of
care being key considerations. Alternative clinical trial designs have been summarized in the “Study Design” section (Bullimore et al., 2023), including using a virtual control group based on previous studies (Chamberlain et al., 2021 2023), comparison with established treatments, or a time-to-treatment-failure (survival analysis) approach (Sankaridurg et al., 2019). (p. 17)
The National Eye Institute supports randomized clinical trials as a gold standard, suggesting that randomization reduces bias and provides a rigorous tool to examine cause-effect relationships between an intervention and outcome. This is because the act of randomization balances participant characteristics (both observed and unobserved) between the groups allowing attribution of any differences in outcome to the study intervention. This is not possible with any other study design. (Hariton & Locascio, 2018). Ultimately, the decision to randomize lies within the potential participant following a judicious informed consent process (Sankaridurg et al., 2023).
Poor Representation of Ethnic and Minority Populations
Marginalized population groups such as ethnic and minority populations and those with lower socioeconomic status are underrepresented in research, and the consequent lack of data can result in compounding health inequities (Bodack et al., 2010; Jones-Jordan et al., 2010; Morrison, 1998). Without representative data including all population groups, especially the most vulnerable and marginalized, interventions designed to address barriers to care will not be as effective as they could otherwise be. Numerous reasons are given for the lack of adequate representation of these key populations, including difficulties accessing specific population groups based on their geographic location, e.g., Native American children living on reserves; limited availability of researchers; significant resources required to translate research documents; and mistrust in research because of negative studies focused on racial and ethnic minorities in history (Wallace et al., 2018). These reasons for nonparticipation of marginalized populations are likely to be continuing problems limiting the inclusion of ethnic and minority groups in population-based research unless specific efforts are made to overcome these barriers.
STRATEGIES RECOMMENDED TO OVERCOME BARRIERS
Note: This section draws heavily on the commissioned paper prepared by Harewood and colleagues (2024) for this study.
Offering Parental Opt-outs Rather than Consent
One strategy for handling low rates of parental consent for vision screening is to send parents a letter describing what will happen at school during a vision screening and telling them how to opt their child out of the screening (Foe & Larson, 2016; Tigges, 2003). A Canadian vision screening project for children ages 4–6 in a variety of geographic locations had an average opt-out rate of 4% when an opt-out model was used and of 8% when active consent was required, but 22% of parents in the latter case failed to return the consent form and hence prevented the screening of their child (Nishimura et al., 2020).
School Visits to Promote Parental Consent
Another strategy that has been recommended to overcome barriers associated with low rates of parental consent is for a member of the vision screening team to make visits to the class
and school to promote the project to principals, teachers, and students (O’Donnell et al., 1997; Secor-Turner et al., 2010; Wolfenden et al., 2009). Other strategies include providing incentives to teachers and students (Ji et al., 2006; O’Donnell et al., 1997; Secor-Turner et al., 2010; Wolfenden et al., 2009), choosing a time of school year with high attendance and few distractions (Detty, 2012), and providing translation services to address literacy and language barriers (Vongsachang et al., 2020).
In-School Follow-Up
Critical to the success of universal vision screening (or any other form of screening) is that referred children go to an eye care professional for follow-up treatment of any eye problem discovered and for continuing care. To promote follow-up, some universal screening programs have brought an eye care professional into the school with portable optometry equipment (Chu et al., 2015; Hark et al., 2018; Hendler et al., 2016; Silverstein et al., 2021; Williams et al., 2013). Any glasses that are ordered are usually also dispensed at the school. The reasoning is that the school is a familiar and trusted space, the program can do the scheduling and check on compliance, and that the wearing of dispensed glasses can be encouraged by the child’s teacher. Such hybrid school-based programs are highly successful, because they eliminate financial, geographic, and transportation barriers to care and because they reduce mistrust (Collins et al., 2022b; Diao et al., 2016; Peterseim et al., 2015 Simon et al., 2007).
The Wills on Wheels Mobile Eye Unit provided in-school follow-up comprehensive eye exams for children enrolled in low-income schools (where more than 80% of students had a household income below $19,090 for a family of three or $23,050 for a family of four) that were referred from the National Football League Philadelphia Eagles Eye Mobile vision screening program. Through this initiative, completed follow-up eye exams increased from 53% prior to its implementation to 62%.
The See Well to Learn Program in San Francisco, CA, provides autorefractor screening in local Head Start preschool programs, comprehensive exams in a mobile van, and two pairs of glasses for children that need them (Sabharwal et al., 2021). Similarly, Vision for Baltimore uses a mobile van to provide vision screenings, comprehensive eye exams, and prescription glasses for elementary and middle school children in Baltimore public schools who require them. On-site school-based vision centers make vision care and eye care professionals part of the child’s wellness team by bringing care closer to students attending local schools at minimal to no cost to families. These centers, which are more permanent than mobile vans, are established within the school or where the school district provides a trusted and safe space. Another advantage of these onsite vision centers is the ability for them to coordinate resources and expertise to support students (Collins et al., 2022b Lyons et al., 2011). They also make it more likely that the child’s teacher will become aware of the child’s need to wear glasses, so that the teacher can encourage compliance. When the teacher is asked to monitor compliance daily, as in the See Well to Learn Program, 64%–77% of children wore their glasses at least half the day during the 28 weeks after they received the glasses (Sabharwal et al., 2021).
Social workers and facilitators have been used by some vision screening programs to assist children who fail a vision screening test to receive follow-up care with an eye care professional (Hamm et al., 2021; Hark et al., 2018; Silverstein et al., 2021). In one study, a social worker assisted parents in scheduling appointments, in obtaining necessary referrals, and in reviewing insurance coverage with the family, which resulted in a 72% adherence rate for completing the eye exam (Silverstein et al., 2021).
Additional strategies recommended to improve adherence with follow-up care include providing no-cost care, offering transportation assistance, implementing email/text reminders, and collecting multiple forms of contact information to ensure effective patient outreach (Hark et al., 2018; Kimel, 2006). For the Philadelphia-based Give Kids Sight Day, a social worker helped ensure accurate contact information was collected, arranged follow-up appointments with eye care professionals, assisted with insurance enrollment, and provided transportation vouchers, reducing many of the commonly cited barriers to completing follow-up care (Dotan et al., 2015). Even after a comprehensive eye exam and prescription of glasses for myopia, the system may break down if the glasses are not worn. See Box 8-4 for the most common reasons such glasses may not be worn.
BOX 8-4
Adherence with Wearing Prescribed Glasses Is Low
Reasons for not wearing the glasses that were dispensed, as reported in both the United States (Dhirar et al., 2020) and China (Congdon et al., 2008), where the incidence of myopia is higher are:
- broken or lost glasses
- wearing the glasses only on special occasions.
- Misunderstanding about the importance of adherence with wearing prescribed glasses perpetuate thoughts that glasses:
- are not needed
- could make vision worse, and/or
- could cause teasing.
These results indicate that any successful treatment for myopia will have to also involve a change in societal attitudes about the importance of diagnosis and treatment.
No-Cost Eye Glasses
Providing glasses at no cost—and ensuring that parents know that will happen in advance—is another effective strategy for reducing barriers. A systematic review of randomized controlled trials, mostly conducted in China, provides evidence from 11 studies that children are 2.45 times more likely to be wearing prescribed glasses at an unexpected follow-up visit if they were provided at no charge than if the parents only received a letter with the prescription (Wu et al., 2023). The effect is smaller with longer follow-up time (odds ratio 2.30 after 6–12 months versus 3.18 with earlier follow-up). Compliance was higher when the refractive error was higher or visual acuity was poorer. Nevertheless, in some of the RCTs, less than half the children who received free glasses were wearing them at follow-up.
One of the studies from China used an interesting comparison relevant to the sustainability of programs offering free glasses: parents in three intervention groups were offered free glasses, but those in two of them were allowed to purchase upgraded glasses (scratch-proof lenses and popular frames) for either $15 or $30, the 25th and 75th percentile of the average cost of purchased glasses at the time (Wang et al., 2017). More revenue was generated when the glasses were not free (control group) or upgrades could be purchased. However, an unannounced visit to the classrooms revealed that only 18%–32% of children were wearing the prescribed glasses, with no difference between children from groups given the upgrade voucher and the
control group. However, the results are likely not generalizable to the United States because at least 97% of parents in each group went to the county hospital to obtain the prescribed glasses even though the county hospital was at a median distance of 27 km from the township of residence. No program in the United States reaches that level of compliance.
A study included in the systematic review (Wu et al., 2023) included children in grades 1 and 2 in New York City public schools serving low-income neighborhoods (Ethan et al., 2010). All schools received the state-mandated vision screening. Children were included if they had failed vision screening the year before and if the parents did not opt out after receiving a letter about the program (less than 1% of parents opted out). Parents of children who failed screening in the four control schools received a letter indicating that they should take the child for an eye exam. Children in the four intervention schools who failed the state screening received a noncyclopleged optometric examination (comprehensive eye exam) and, if needed, two pairs of glasses, one for the teacher to keep and one to wear. In addition, teachers received instruction on children’s visual problems and were asked to “lend” the second pair of glasses when needed. Observations during an unexpected visit to the classroom revealed that 47% of the children prescribed glasses were wearing them in the intervention group compared to 19% in the control group. Some students relied on the loaner glasses all the time at school because the “home” glasses had been lost or broken and not replaced.
An ideal design for vision screening and facilitated follow-up, therefore, should include easy and inexpensive access to comprehensive eye exams for those who fail screening—either by bringing an optometrist into the school or helping with booking at a community provider. It should also include provision of two pairs of subsidized glasses, one of which is kept with the teacher at school, who is made aware of the child’s need to wear glasses for near and/or far work. Broken and lost glasses should be replaced promptly.
However, even with two pairs of free glasses, a program for mostly Native American 8-to 14-year-olds found that 67% were not wearing their glasses a year later, mostly because the glasses were lost (45%) or broken (35%; Messer et al., 2012). Other reasons given were not liking the glasses (15%), thinking they were not needed (2%), and having left them at home (2%). Nevertheless, over 90% of the students reported that the glasses helped them to see more clearly, whether or not they were wearing them (98% vs. 94%). Those with worse acuity were more likely to be wearing their glasses: children were 60% more likely to be wearing their glasses with each line of decreased acuity. Similarly, a comparison of glasses wearing after 1 year in states with programs involving just a referral letter and programs adding free comprehensive eye exams and glasses revealed low compliance overall (27% of children needing glasses were wearing them) with no difference between programs but better compliance when visual acuity was poorer (Manny et al., 2012). In another study, 66% of children in second or third grade who had been given two pairs of glasses after a comprehensive eye exam at school needed replacement glasses before the 1-year follow-up, with nearly half of these students needing replacements two or three times (Huang et al., 2019). Vision Screening programs that go a step further to collaborate with parents to address children’s concerns about discomfort or adaptation have demonstrated improvement in compliance rates and in encouraging children from low-income families to wear glasses (Perez et al., 2022).
Economic Evaluations
To overcome the barriers related to funding for universal vision screening programs, economic evaluations are needed to inform resource allocation and policy decisions. These
economic evaluations should include a determination of the cost-effectiveness of various vision care models to detect myopia compared to standard of care. In a study examining the cost-effectiveness of providing on-site exams in detecting amblyopia, relatively similar follow-up rates were observed when students who failed a screening were referred to a community provider (59% following up) compared to those who underwent a comprehensive eye exam through an onsite mobile clinic (55%; Lowry & de Alba, 2016; Ross & Stein, 2016). Given that the mobile clinic had a higher cost per case of amblyopia, community-based eye care was deemed more cost-effective. However, the follow-up rate for the mobile clinic was low due to challenges with parental consent. Implementing modifications to improve consent rates could increase the cost-effectiveness of a mobile clinic in detecting amblyopia.
To inform the conduct of economic evaluation of vision care models for myopia, studies on the impact of myopia on quality of life are needed. There is evidence that myopia can negatively impact the quality of life of both children with myopia and their parents for reasons that depend on the type of optical correction (e.g., glasses, contact lenses, refractive surgery). The impact of myopia control treatments on quality of life warrants further study, using instruments specifically developed for this population and condition (Lipson et al., 2022). Studies are also needed on the impact of untreated myopia on quality of life.
Improved Vision Screening Criteria for Myopia
The natural history of myopia development necessitates consistent vision screening throughout the school-age years to identify early onset and progression of myopia. During this period, 23.4% of children in the CLEERE study developed myopia (–0.50D or worse) (Kleinstein et al., 2012). The highest percentage of new cases occurred at age 11, with the onset spanning ages 7 to 16 years. Given the progressive nature of childhood and adolescent myopia, screening examinations encompassing visual acuity are recommended every 1 to 2 years (Hutchinson et al., 2023). Though the average prevalence of myopia is low among children younger than 5 years, it is critical that individuals with risk factors for myopia be identified early to encourage better vision health outcomes. Treatment interventions for delaying the onset of myopia and reducing myopia progression in childhood are available (see chapter 7 on Treatment). Therefore, a targeted strategy of periodic screening and evaluation of children at risk for myopia progression would address the problem of myopia as well as other ocular conditions. This could result in fewer visual disabilities and reduced risk of visual impairment (Bullimore & Brennan, 2019), ultimately alleviating the burden on the entire health care system.
Integrated Data Systems to Improve Surveillance of Children with Myopia
The success of a vision screening program is determined by ensuring that children are screened for vision impairment and that those identified receive follow-up comprehensive eye exams and treatment. Policies directed at addressing this issue can increase the effectiveness of screening programs. One recommended approach has been the implementation of an integrated data system for reporting screening and exam results (Brody et al., 2007; Collins et al., 2022a; Hartmann et al., 2015; Shakarchi & Collins, 2019). The Centers for Disease Control and Prevention’s Vision Health Initiative (VHI) in collaboration with NORC at the University of Chicago developed The Vision and Eye Health Surveillance System (VEHSS) in 2015 to leverage data sources on vision and eye health to better understand the scope of vision loss, eye disorders, and eye care services in the United States (Rein et al., 2018). The current data on
childhood myopia in VEHSS is from claims (Medicare, Medicaid, Managed Vision Care, and commercial medical insurance) and the IRIS Registry, which includes data from electronic health records of ophthalmology practices in the United States. Available vision services data such as vision screening is from national survey data.
Expanding VEHSS to include standardized statewide surveillance data on patient demographics, vision care services (i.e., vision screening, comprehensive eye exams), referrals to eye care providers, and diagnoses of vision disorders for children would not only enhance care integration and communication but also enable monitoring and development of strategic interventions to ensure that follow-up care is received. Such an expanded, national vision surveillance system would support public health efforts to understand if efforts are meeting set targets (Lee et al., 2012).
INNOVATIVE APPROACHES TO ADDRESS BARRIERS TO VISION CARE SERVICES
Innovative approaches for vision screening using smartphones have been introduced over the last decade. These innovations include Peek Vision (Rono et al., 2018), which measures acuity, and GoCheckKids (Arnold et al., 2018b), which measures not only visual acuity but also acts as a photoscreener to detect abnormal refractive errors and other vision problems. These applications are used around the world in remote locations and, in some cases, by parents instructed on their use at home, an innovation that proved useful during COVID-19 (e.g., Davara et al., 2022; reviewed in Thirunavukarasu et al., 2023; Painter et al., 2021). Some of these innovative smartphone applications are integrated with software aimed at encouraging follow-up with an eye care professional. Voluntary organizations such as Sight Savers America are also promoting integrated care (screening using conventional tools and facilitated follow-up) in some U.S. locales.
Peek Vision Foundation
In 2018, Peek Vision Foundation launched what they called a “dynamic social enterprise” with the goal of “vision and eye health for all” (Rono et al., 2018). As part of his PhD project, ophthalmologist Dr. Andrew Bastawrous saw the challenges facing Kenya, where the number of vision problems was high, and the number of resources was low. He set out to create the “eye-phone” to identify individuals with poor vision, using smart phones to allow increased access to screening, even in the most remote places. (See Figure 8-3.)
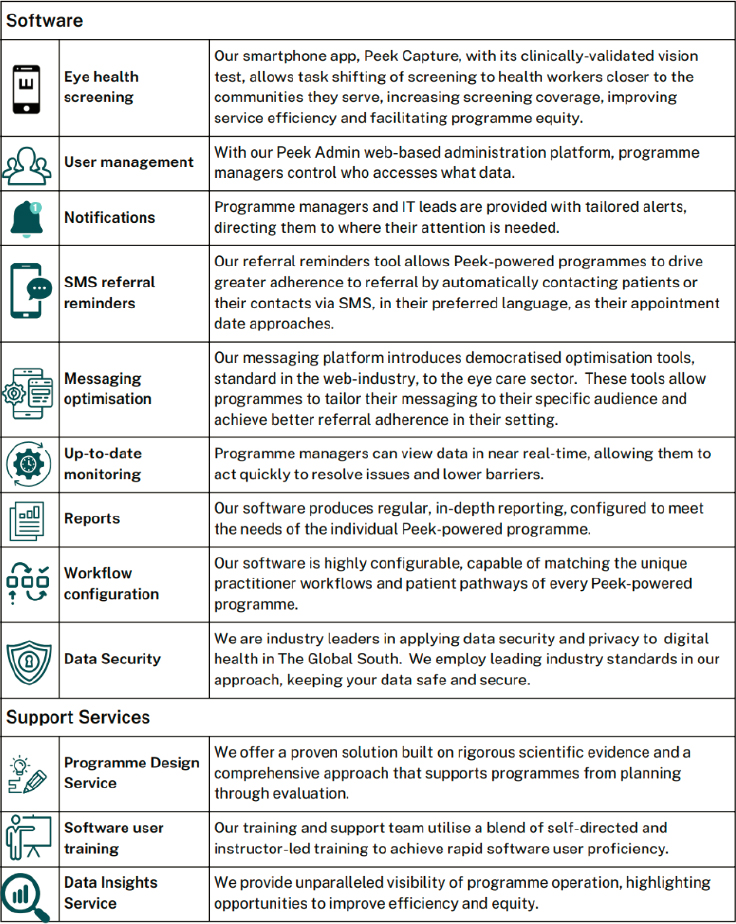
SOURCE: Bastawrous & Peek Vision, n.d.
The first step in Peek’s smartphone-based system is acuity testing, which can be conducted by a health worker or teacher. The screen displays tumbling Es and the child is asked to point in the direction in which the E is pointing. A built-in algorithm quickly determines the sizes that are needed to obtain a threshold. It requires minimal training to use it. The Es are surrounded by a box to create crowding, which improves accuracy of the visual acuity measurement. Comparisons of Peek results to conventional acuity testing have demonstrated good comparability in adults and children (e.g., Bastawrous et al., 2015; Bhaskaran et al., 2022), with better comparability than that found for many of the other smartphone acuity testing apps available (reviewed in De Samanta et al., 2023). However, in a study with children in Paraguay, Peek tended to overestimate acuity compared to a pediatric ophthalmologist’s measurement with a Snellen chart (de Venecia et al., 2018). Only 31% of assessed acuity values agreed exactly, but 59% were within one step and 71% within two steps. One reason may be the higher probability of guessing 1 of 4 directions correctly by chance with Tumbling Es, vs. 1 of 26 letters with standard letter charts.
Importantly, results of Peek acuity applications are integrated with a system for scheduling and encouraging follow-up for children referred for a full comprehensive eye exam. In a recent clustered randomized controlled trial, this integrated system was used in 25 schools in Kenya (Rono et al., 2018). Parents of children who could not see the 20/40 letters after the teacher tested acuity with the Peek system received a picture of how blurry the child’s vision is and repeated SMS messages about how to take the child for follow-up. Similar messages went to the child’s teacher and the hospital to which the child was referred. The comparison was 25 schools in which the teacher tested with a conventional Tumbling E chart and, if the child could not see the 20/40 letters, sent a standard referral letter home. Within the next 8 weeks, only 22% of parents in the standard group brought their children to the hospital for follow-up, compared to 54% of parents in the integrated Peek system group.
The Peek Vision program reports that about five million individuals had been screened with their system in community, school, and workplace settings between 2018 to 2022. More than 20% of them were identified as needing eye care, and more than half of those identified were seen by an eye care specialist.2 The number of people screened each year is now increasing rapidly around the world.3
GoCheckKids
GoCheckKids is a vision screening system that works only via iPhone both to test visual acuity with Sloan letters with crowding bars and to do photoscreening to detect children in need of a referral to an eye doctor. It is being used in schools, Head Start programs, and physicians’ offices in the United States and Europe. The photoscreening capabilities of GoCheckKids have been tested extensively with children (as well as adults) and involve taking a flash picture of the eye in a darkened room while the iPhone is surrounded by a black flash-concentrating case and the child is fixating the screen 6 meters away. The appearance of the reflected red reflex (Bruckner’s reflex) is used to judge whether the child has a referrable refractive error or other visual problem. Judgments can be made remotely by an expert or immediately through AI-powered algorithms. GoCheckKids measurements are eligible for reimbursement under photoscreening billing codes provided by the Centers for Medicare and Medicaid Services, (CPT 99174, CPT 99177) and the system works with a subscription model rather than as a capital purchase.
Studies of the photoscreening app with young children indicate good sensitivity and specificity for amblyopia risk factors compared to findings of a gold-standard cyclopleged eye exam (76% and 85%, respectively, with expert grading, 65% and 83%, with automatic grading; Arnold et al., 2018b), although comparisons are less favorable for children under 1 year of age (positive predictive value of only 26%; Law et al., 2020). Overall, values for sensitivity and specificity of the photoscreening app for detecting amblyopia risk factors compare favorably to those reported for the conventional Spot and Plusoptix photoscreeners (Sopeyin et al., 2021). One limitation is that, at least with young children, slightly more than 10% of images from the GoCheckKids device cannot be scored, mostly because of lack of fixation (Arnold et al., 2018b). A limitation of the GoCheckKids system is its lack of compatibility with other smartphone systems besides the iPhone. However, this is limitation is mitigated by its use of a subscription service which includes an iPhone device with the necessary software.
___________________
2 For more information, see https://peekvision.org/our-impact
3 See https://peekvision.org/wp-content/uploads/2023/11/Peek-Vision-Brochure.pdf
Sight Savers America—Alabama
Although the State of Alabama does not have a mandate to provide vision care to children, it has had an annual line item in the budget for statewide vision screening and comprehensive follow-up eye care for public school kindergarten, second, and fourth grades since 2004 (Prevent Blindness, 2022). After competitive re-evaluation in 2021 and 2022, Sight Savers America remained the sole recipient of allocated state funding for Alabama’s comprehensive follow-up eye care program. A 501(c)(3) nonprofit program since 1997, Sight Savers America has reached over 750,000 children with case management support for comprehensive dilated eye exams, eyeglasses, medications, surgeries, and other eye care treatments4 (Sight Savers America, 2024). Sight Savers America helps coordinate care and establish an eye care home for on-going vision needs for over 50,000 children each year from Alabama, Texas, Louisiana, Mississippi, Georgia, and South Carolina.
Children who fail the vision screening step are assigned a case specialist, who helps manage care throughout the multistep process from consent and vision screening to the establishment of an eye care home and long-term treatment. Case specialists use motivational health coaching techniques to educate parents about vision screening and the importance of obtaining a comprehensive dilated eye examination for children who fail screenings to facilitate compliance. Personnel from Sight Savers America help those who qualify obtain Medicaid insurance, which will provide an annual comprehensive eye exam to the child. For medically underserved families, transportation and prescribed treatments are provided at no cost to the families. Data on the success of this integrated approach is provided annually on the program’s website and to state personnel. State-allocated funds are leveraged with private financial gifts and gifts in-kind.
The capture rate for comprehensive eye examination following vision screening has been reported in the United States to be roughly 39% in primary care pediatric practices (Hered & Wood, 2013; Sight Savers America, 2024). Sight Savers America reports that through their integrated, case-managed eye care program, 71% of children who were reached following failed vision screening received a comprehensive eye exam (Sight Savers America, 2024). Sight Savers attributes their cost-effectiveness and success to using a quick vision screening tool, individual case managers, and a network of eye care providers who increase their patient base and help with costs by donating prescription glasses and discounting comprehensive eye exams when necessary.
The following three tables summarize contextual (Table 8-7), individual-level (Table 8-8), and research (Table 8-9) barriers, potential actors and strategies to overcome barriers to vision screening, comprehensive eye exams and treatment for myopia and other refractive errors in children.
___________________
4 For more information, see https://sightsaversamerica.org/eye-care
| Barrier | What Can Be Done? | Who Can Help? |
|---|---|---|
| A lack of consensus on the importance and conduct of vision screening | Engage in consensus building to develop standardized vision screening guidelines for myopia |
|
| A lack of funding for vision screening programs |
|
|
| Concerns about the accuracy of vision screening tests | Increase education on conducting effective and frequent vision screenings and the variability in accuracy of instrument-based screening devices and gain consensus on referral criteria |
|
| Instrument malfunction, availability |
|
|
| Limited statewide surveillance of preventive services under the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) Medicaid benefit |
|
|
| Pediatric Primary Care | ||
| Perceptions of insufficient time in the clinic workflow | Research to understand clinic workflow, develop and implement strategies to overcome barriers |
|
| Inadequate reimbursement for vision screening | Reimbursement for vision screening is low and should not be bundled into the global code of well-child visits |
|
| Limited number of appointments for well-child visits, especially in resource-deprived communities |
|
National professional associations (AAP, AAFP, AAOpt, AAOphth, AAPOS, NMA) |
| Long travel distance to nearest primary care provider |
|
National professional associations (AAP, AAFP, AAOpt, AAOphth, AAPOS, NMA) |
| School and Community Vision Screening | ||
| Variability in state requirements for vision screening in schools | Develop national standardized guidelines for vision screening |
|
| Limitations due to space, school schedules, and calendars |
|
|
|
||
| Problematic consent processes for children to participate in vision screening |
|
|
| Poor communication about the program |
|
|
| Parent socioeconomic barriers |
|
|
| Comprehensive Eye Exams and Treatment | ||
| Lack of follow-up with eye care professional |
|
|
| Poor provider–patient communication of results of a vision test | Offer physician continuing culturally sensitive training, refresher training/courses, and changes to medical curricula | National professional associations (AAP, AAFP, AAOpt, AOA, AAOphth, AAPOS, NMA, AMA) |
| Low reimbursement rates for rendering eye care | Increase rates of reimbursement for rendering eye care |
|
| Low supply of eye care specialists willing to see children |
|
National professional associations (AAP, AAFP, AAOpt, AOA AAOphth, AAPOS, NMA, AMA, ASCO) |
| Lack of affordable prescription glasses and compliance with wear |
|
|
|
|
|
| Lack of consensus on guidelines for comprehensive eye exams by professional organizations |
|
|
NOTE: AAFP = American Academy of Family Physicians; AAOpt = American Academy of Optometry; AAOphth = American Academy of Ophthalmology; AAP = American Academy of Pediatrics; AAPOS = American Academy of Pediatric Ophthalmology and Strabismus; AHRQ = Agency for Healthcare Research and Quality; AMA = American Medical Association; AOA = American Optometric Association; APHA = American Public Health Association; ASCO = Association of Schools and Colleges of Optometry; CDC = Centers for Disease Control and Prevention; CMS = The Centers for Medicare & Medicaid Services; DHHS = Department of Health and Human Services; NACHW = National Association of Community Health Workers; NASN = National Association of School Nurses; NIH = National Institute of Health; NMA = National Medical Association; PCORI = Patient-Centered Outcomes Research Institute; RPB = Research to Prevent Blindness; USPSFT = United States Preventive Services Taskforce.
SOURCE: Committee generated.
| Barrier | What Can Be Done? | Who Can Help? |
|---|---|---|
| Predisposing Characteristics | ||
| Age Race, Ethnicity Sex Special healthcare needs Social determinants of health |
|
|
| Parental health beliefs | Public education to improve awareness and vision health literacy by patient navigators and peer ambassadors from local communities who understand the culture and social context of parents’ beliefs |
|
| Parent mistrust and misconceptions | Public education to improve awareness and vision health literacy by patient navigators and peer ambassadors from local communities who understand the culture and social context of parent’s beliefs |
|
| Parent mental and physical disabilities | Funding for local programs to address barriers to access for vision care in medically underserved and health-disparity populations |
|
| Enabling Factors | ||
| Type and lack of health insurance Household income Transportation Household structure |
|
|
| Need Factors | ||
| False positive and negative tests |
|
|
|
||
| Lack of priority setting for eye and vision care | Public education to improve awareness and vision health literacy provided by patient navigators and peer ambassadors from local communities who understand the culture and social context of parental beliefs |
|
| Mistrust of vision screening results | Public education to improve awareness and vision health literacy by patient navigators and peer ambassadors from local communities who understand the culture and social context of parental beliefs |
|
NOTES: AAFP = American Academy of Family Physicians; AAOphth= American Academy of Ophthalmology; AAOpt = American Academy of Optometry; AAPOS = American Academy of Pediatric Ophthalmology and Strabismus; AHRQ = Agency for Healthcare Research and Quality; AOA= American Optometric Association; APHA = American Public Health Association; CMS = The Centers for Medicare & Medicaid Services; DHHS = Department of Health and Human Services; NACHW = National Association of Community Health Workers; NASN = National Association of School Nurses; NIH = National Institute of Health; NMA = National Medical Association; RPB = Research to Prevent Blindness; USPSFT = United States Preventive Services Taskforce.
SOURCE: Committee generated.
| Barrier | What Can Be Done? | Who Can Help? |
|---|---|---|
| Poor data collection for surveillance | National, standardized guidelines for vision screening and the collection of sociodemographic factors such as race vs ethnicity, and sex vs. gender. |
|
| Limited funding to conduct research | Funding institutions to prioritize research for randomized trials to determine the efficacy of |
|
| interventions to improve access to vision care for children |
|
|
| Ethical concerns about randomized trials | Public education on the importance and safety of randomized trials; timely evaluation of treatment outcomes as it relates to standard of care and research |
|
| Poor representation of minoritized populations in research |
|
|
NOTES: AAP = American Academy of Pediatrics; AAFP = American Academy of Family Physicians; AAOpt = American Academy of Optometry; AAOphth = American Academy of Ophthalmology; AAPOS = American Academy of Pediatric Ophthalmology and Strabismus; AHRQ = Agency for Healthcare Research and Quality; AOA = American Optometric Association; CDC = Centers for Disease Control and Prevention; DHHS = Department of Health and Human Services; IRB = Institutional Review Board; NEI = National Eye Institute; NIH = National Institutes of Health; NMA = National Medical Association; RPB = Research to Prevent Blindness; USPSTF = United States Preventive Services Task Force.
SOURCE: Committee generated.
CONCLUSIONS
Several common themes emerged from the analysis of barriers to myopia detection and treatment. Those barriers are described here in three conclusions that inform the recommendations that follow.
Conclusion 8-1: Multiple barriers to vision care for children exist. The most significant barriers are an uneven awareness of the importance of checking children’s vision health, parents’ difficulties in gaining access to an eye care professional, and barriers to compliance with prescribed treatments.
Conclusion 8-2: Vision screening is important in identifying children with vision impairment and facilitating access to treatment, but many children are not receiving vision screening and, when they do receive it, often do not receive any recommended referral. One model that has been used successfully is to provide vision screening to all children in congregate locations (schools, fairs, etc.). An alternative that has been successful when resources are scarce is to offer vision screening to targeted groups at increased risk of vision problems or of not receiving treatment (e.g., medically underserved communities, rural communities). For children with lower socioeconomic status and from medically underserved populations, vision screenings within community health centers and federally qualified health centers are an excellent way to provide access to vision care. School boards can also take advantage of Medicaid dollars provided through the Healthy Schools Campaign.
Conclusion 8-3: Vision screening is ineffective without receipt of follow-up eye care for children that need it. Therefore, it is critical that vision screening programs provide effective strategies to ensure that children identified with potential vision impairment receive a comprehensive eye exam by an eye care professional (skilled in providing vision care to children) to diagnose vision disorders and provide treatment. Comprehensive eye exams by eye care professionals, along with facilitators such as social workers or community health workers as patient navigators who assist caregivers with scheduling comprehensive eye exams and provide frequent reminders to attend appointments, have been shown to be effective in increasing follow-up compliance. However, myopia is a lifelong condition requiring follow-up eye examinations and, when needed, replacement of lost or broken glasses. The same barriers to the initial detection of children’s vision problems impact continuing care, underscoring a need for an eye care home.
RECOMMENDATIONS
Considering the findings of this consensus report, the committee makes the following recommendations to improve detection and treatment of myopia in children and to address the disparities in accessing vision care.
Recommendation 8-1: The U.S. Department of Health and Human Services, in collaboration with departments of education at the state level, should take measures to ensure that children receive a vision screening before first grade and a comprehensive eye exam, when needed. To facilitate this:
- Federal agencies such as the Centers for Disease Control and Prevention and other agencies that support public health programming should encourage the implementation of effective vision care programs for children by providing funding or other incentives for vision health care systems that follow the 12 Components of a Strong Vision Health System of Care provided by the National Center for Children’s Vision and Eye Health. Priority should be given to programs targeting high-risk groups (i.e., children with lower socioeconomic status, of younger ages [under 6 years], with disabilities, with parents who have low health literacy, or from racial or ethnic minority groups [specifically, Hispanic, non-Hispanic Black, Asian, American Indian, Alaskan Natives, and Pacific Islanders], and children living in medically underserved communities [e.g., rural]).
- The Department of Health and Human Services should oversee the provision of cost-effective, standardized, evidence-based national vision screening guidelines to detect refractive errors, amblyopia, and other vision conditions. These guidelines should include a consensus on the ideal target age for screening, screening frequency, the need for re-screening, types of screening tests, tools, and referral criteria.
- For children under age 7, the referral criteria for instrument-based screening should include any amount of myopia or a family history of myopia based on the evidence that these predict likely progression to significant myopia.
- The Association of Schools and Colleges of Optometry, the National Medical Association, and the American Medical Association should use innovative means to encourage optometric and medical graduates of all backgrounds to pursue residencies in pediatric optometry and residents to pursue fellowships in pediatric ophthalmology. This should be done using innovative strategies such as pipeline and incentive programs to improve the vision care workforce, especially the workforce in rural and low-income communities. Continuing education should be provided for practicing optometrists and ophthalmologists to encourage them to include young children in their practice.
Recommendation 8-2: An integrated, national data surveillance system is needed to collect state-level data on vision screening, referrals to eye care providers, sociodemographics (age, race, ethnicity, sex, and geographic location) and outcomes of referrals. This data system would not only enhance care integration and communication, but also enable monitoring to ensure that follow-up care is received, especially in high-risk populations. A surveillance system would also support the Department of Health and Human Services’ Office of Disease Prevention and Health Promotion’s Healthy People 2030 goal of increasing the proportion of children who get vision screening. To facilitate the creation of this system:
- The Centers for Medicare & Medicaid Services should include vision screening in the Core Set of Children’s Health Care Quality Measures that are reported annually by all states.
- The Centers for Medicare & Medicaid Services should require reimbursement for vision screening to not be bundled into the global code of well-child visits.
- Professional associations such as the American Academy of Optometry, American Optometric Association, and American Academy of Ophthalmology should work with device manufacturers to create a national database of eye care providers that provide care to children, especially children under the age of 6 years, and the types of health insurance they accept. This database should be in a format that is easily accessible by caregivers and the general public.
- The National Institutes of Health “All of US” Research Program and the Healthy Brain and Child Development Study should include additional measures of adult and child vision disorders.
Recommendation 8-3: The National Institutes of Health, Agency for Healthcare Research and Quality, as well as foundations, nonprofits, and industry and other organizations that support research, such as Research to Prevent Blindness, should seek and encourage opportunities to fund work supporting continued efforts by vision researchers to determine:
- Genetic predisposition to myopia development and progression in racial and ethnic minoritized populations;
- The implementation, effectiveness, and cost-effectiveness of existing and novel interventions in real-world settings to improve access to vision screening, adherence with referrals to eye care providers, and coordination of care across providers compared to standard of care, especially for populations at high risk for vision impairment.
- The prevalence of myopia, referrals to eye care providers, completion of comprehensive eye exams, and treatment in children, especially those from high-risk populations
- Differences in reimbursement processes (e.g., bundled vs. unbundled with global code for well-child visits), reimbursement rates (for vision screening, new and ongoing care by eye care providers) and coverage for prescription glasses across states and health insurance plans; and the influence of those differences on vision health outcomes, especially as it relates to children from high-risk populations; and
- Strategies for promoting adherence with referrals, follow-up care, compliance with wearing prescribed glasses, and improved public awareness of and health education on vision and eye health in children, especially those from high-risk populations.
Recommendation 8-4: Global organizations, such as the World Health Organization and the International Myopia Institute, should identity and inventory best practices for improving access to vision care for medically underserved populations. Where
culturally appropriate, these practices can be generalized to and from the United States.
Recommendation 8-5: Myopia should be classified as a disease and therefore a medical diagnosis by The Centers for Medicare & Medicaid Services. This reclassification is to ensure efforts not only to treat blurry vision resulting from uncorrected or under-corrected refractive error, but also to ensure that the prevention and management of the progression of myopia gets the warranted attention from stakeholders such as federal and state agencies, professional associations, patients, and caregivers. Myopia is a disease with increasing worldwide prevalence and severity, and recognition of the impact of its downstream complications needs to be taken seriously.
REFERENCES
Abdus, S., & Selden, T. M. (2022). Well-child visit adherence. JAMA Pediatrics, 176(11), 1143–1145. https://doi.org/10.1001/jamapediatrics.2022.2954
Aday, L. A., & Andersen, R. (1974). A framework for the study of access to medical care. Health Services Research, 9(3), 208–220. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1071804/
Aday, L. A., & Andersen, R. M. (1981). Equity of access to medical care: A conceptual and empirical overview. Medical Care, 19(12), 4–27. https://pubmed.ncbi.nlm.nih.gov/11643688/
Adler, N. E., Boyce, T., Chesney, M. A., Cohen, S., Folkman, S., Kahn, R. L., & Syme, S. L. (1994). Socioeconomic status and health: The challenge of the gradient. The American Psychologist, 49(1), 15–24. https://doi.org/10.1037//0003-066x.49.1.15
Adler, N. E., & Ostrove, J. M. (1999). Socioeconomic status and health: What we know and what we don’t. Annals of the New York Academy of Sciences, 896(1), 3–15. https://doi.org/10.1111/j.1749-6632.1999.tb08101.x
Ambrosino, C., Dai, X., Antonio Aguirre, B., & Collins, M. E. (2023). Pediatric and school-age vision screening in the United States: Rationale, components, and future directions. Children (Basel), 10(3). https://doi.org/10.3390/children10030490
American Academy of Family Physicians. (n.d.). Clinical preventive service recommendation: Visual difficulties and impairment. https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/visual.html
American Academy of Ophthalmology. (2018). Preferred Practice Pattern Guidelines. American Academy of Ophthalmology Pediatric Ophthalmology/Strabismus Panel. www.aao.org/ppp.eith.
___. (2022). Vision screening for infants and children. https://www.aao.org/Assets/660a518b-66d6-435d-a614-99b21853626d/638006528877300000/vision-screening-for-infants-and-children-2022-pdf
American Academy of Optometry. (2016). American Academy of Optometry policy statement: Childhood vision screening. https://aaopt.org/position-paper/
American Association for Pediatric Ophthalmology and Strabismus. (n.d.). Vision screening recommendations. https://higherlogicdownload.s3.amazonaws.com/AAPOS/159c8d7c-f577-4c85-bf77-ac8e4f0865bd/UploadedImages/Documents/vision_screening_rec.pdf
American Optometric Association. (2017). Comprehensive Pediatric Eye and Vision Examination. https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf
American Optometric Association, & Cary, D. (2018). AOA Advocacy Tool Kit. https://www.aoa.org/AOA/Documents/Advocacy/AOA%20Children%27s%20Vision%20Advocacy%20Toolkit%20MASTER%201.30.18.pdf
Andersen, R. A. (1968). A behavioral model of families’ use of health services. Center for Health Administration Studies, University of Chicago.
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36(1), 1–10. https://doi.org/10.2307/2137284
Andersen, R. M., & Davidson, P. L. (2007). Improving access to care in America: Individual and contextual indicators. In R. M. Andersen, T. H. Rice, & G. F. Kominski (Eds.), Changing the U.S. Health Care System: Key Issues in Health Services Policy and Management (3rd ed., pp. 3–31). Jossey-Bass.
Antonio-Aguirre, B., Block, S. S., Asare, A. O., Baldanado, K., Ciner, E. B., Coulter, R. A., DeCarlo, D. K., Drews-Botsch, C., Fishman, D., Hartmann, E. E., Killeen, O. J., Yuen, J., & Collins, M. E. (2024). Association of sociodemographic characteristics with pediatric vision screening and eye care: An analysis of the 2021 National Survey of Children’s Health. Ophthalmology, 131(5), 611–621. https://doi.org/10.1016/j.ophtha.2023.12.005
Anzeljc, S., Ziemnik, L., Koscher, S., Klein, W., Bridge, C., & Van Horn, A. (2019). Preschool vision screening collaborative: Successful uptake of guidelines in primary care. Pediatric Quality & Safety, 4(6), e241. https://doi.org/10.1097/pq9.0000000000000241
Arnold, R. W., Arnold, A. W., Hunt-Smith, T. T., Grendahl, R. L., & Winkle, R. K. (2018a). The positive predictive value of smartphone photoscreening in pediatric practices. Journal of Pediatric Ophthalmology and Strabismus, 55(6), 393–396. https://doi.org/10.3928/01913913-20180710-01
Arnold, R. W., Donahue, S. P., Silbert, D. I., Longmuir, S. Q., Bradford, G. E., Peterseim, M. M. W., Hutchinson, A. K., O’Neil, J. W., de Alba Campomanes, A. G., Pineles, S. L., & AAPOS Vision Screening and Research Committees. (2022). AAPOS uniform guidelines for instrument-based pediatric vision screen validation 2021. Journal of American Association for Pediatric Ophthalmology and Strabismus, 26(1), e1–e6. https://doi.org/10.1016/j.jaapos.2021.09.009
Arnold, R. W., O’Neil, J. W., Cooper, K. L., Silbert, D. I., & Donahue, S. P. (2018b). Evaluation of a smartphone photoscreening app to detect refractive amblyopia risk factors in children aged 1-6 years. Clinical Ophthalmology, 12, 1533–1537. https://doi.org/10.2147/OPTH.S171935
Asare, A. O., Malvankar-Mehta, M. S., & Makar, I. (2017). Community vision screening in preschoolers: initial experience using the Plusoptix S12C automated photoscreening camera. Canadian Journal of Ophthalmology, 52(5), 480–485. https://doi.org/10.1016/j.jcjo.2017.02.002
Asare, A. O., Maurer, D., Wong, A. M. F., Ungar, W. J., & Saunders, N. (2022). Socioeconomic status and vision care services in Ontario, Canada: A population-based cohort study. The Journal of Pediatrics, 241, 212–220.. https://doi.org/10.1016/j.jpeds.2021.10.020
Bastawrous, A., Rono, H. K., Livingstone, I. A., Weiss, H. A., Jordan, S., Kuper, H., & Burton, M. J. (2015). Development and Validation of a smartphone-based visual acuity test (peek acuity) for clinical practice and community-based fieldwork. JAMA Ophthalmology, 133(8), 930–937. https://doi.org/10.1001/jamaophthalmol.2015.1468
Bastawrous, A. & Peek Vision. (n.d.). Making the invisible, visible. https://peekvision.org/wpcontent/uploads/2023/11/Peek-Vision-Brochure.pdf
Berkowitz, S. T., Finn, A. P., Parikh, R., Kuriyan, A. E., & Patel, S. (2024). Ophthalmology workforce projections in the United States, 2020 to 2035. Ophthalmology, 131(2), 133–139. https://doi.org/10.1016/j.ophtha.2023.09.018
Berntsen, D. A., & Walline, J. J. (2023). Delaying the onset of nearsightedness. JAMA. 329(6):465–466. doi:10.1001/jama.2022.24386
Bhaskaran, A., Babu, M., Abhilash, B., Sudhakar, N. A., & Dixitha, V. (2022). Comparison of smartphone application-based visual acuity with traditional visual acuity chart for use in teleophthalmology. Taiwan Journal of Ophthalmology, 12(2), 155–163. https://doi.org/10.4103/tjo.tjo_7_22
Biviji, R., Vora, N., Thomas, N., Sheridan, D., Reynolds, C. M., Kyaruzi, F., & Reddy, S. (2024). Evaluating the network adequacy of vision care services for children in Arizona: A cross-sectional study. AIMS Public Health, 11(1), 141–159. https://doi.org/10.3934/publichealth.2024007
Blanchard, J., Ogle, K., Thomas, O., Lung, D., Asplin, B., & Lurie, N. (2008). Access to appointments based on insurance status in Washington, D.C. Journal of Health Care for the Poor and Underserved, 19(3), 687–696. https://doi.org/10.1353/hpu.0.0036
Bodack, M. I., Chung, I., & Krumholtz, I. (2010). An analysis of vision screening data from New York City public schools. Optometry, 81(9), 476–484. https://doi.org/10.1016/j.optm.2010.05.006
Brener, N. D., Wheeler, L., Wolfe, L. C., Vernon-Smiley, M., & Caldart-Olson, L. (2007). Health services: Results from the School Health Policies and Programs Study 2006. Journal of School Health, 77(7), 464–485. https://doi.org/10.1111/j.1746-1561.2007.00230.x
Bright Futures, & American Academy of Pediatrics. (2022). Recommendations for preventive pediatric health care. https://downloads.aap.org/AAP/PDF/periodicity_schedule.pdf
Brody, B. L., Roch-Levecq, A. C., Klonoff-Cohen, H. S., & Brown, S. I. (2007). Refractive errors in low-income preschoolers. Ophthalmic Epidemiology, 14(4), 223–229. https://doi.org/10.1080/01658100701486822
Bullimore, M. A., & Brennan, N. A. (2019). Myopia control: Why each diopter matters. Optometry and Vision Science, 96(6), 463–465. https://doi.org/10.1097/opx.0000000000001367
Bullimore, M. A., Brennan, N. A., & Flitcroft, D. I. (2023). The future of clinical trials of myopia control. Ophthalmic & Physiological Optics: The Journal of the British College of Ophthalmic Opticians (Optometrists), 43(3), 525–533. https://doi.org/10.1111/opo.13120
Burn, H., Hamm, L., Black, J., Burnett, A., Harwood, M., Burton, M. J., Evans, J. R., & Ramke, J. (2021). Eye care delivery models to improve access to eye care for Indigenous peoples in high-income countries: A scoping review. BMJ Global Health, 6(3), e005208. https://doi.org/10.1136/bmjgh-2020-004484
Burton, M. J., Ramke, J., Marques, A. P., Bourne, R. R. A., Congdon, N., Jones, I., Ah Tong, B. A. M., Arunga, S., Bachani, D., Bascaran, C., Bastawrous, A., Blanchet, K., Braithwaite, T., Buchan, J. C., Cairns, J., Cama, A., Chagunda, M., Chuluunkhuu, C., Cooper, A., Crofts-Lawrence, J., … Faal, H. B. (2021). The Lancet Global Health Commission on Global Eye Health: Vision beyond 2020. The Lancet Global Health Commission, 9(4), e489–e551. https://doi.org/10.1016/S2214-109X(20)30488-5
Centers for Medicare & Medicaid Services. (n.d.a). Early and periodic screening, diagnostic, and treatment. https://www.medicaid.gov/medicaid/benefits/early-and-periodic-screening-diagnostic-and-treatment/index.html
___. (n.d.b). Information on Essential Health Benefits (EHB) benchmark plans. https://www.cms.gov/marketplace/resources/data/essential-health-benefits
___. (2024). 2024 mandatory core set of children’s health care quality measures for Medicaid and CHIP (Child Core Set). https://www.medicaid.gov/sites/default/files/2023-08/2024-child-core-set_0.pdf
Chamberlain, P., Lazon de la Jara, P., Arumugam, B., & Bullimore, M. A. (2021). Axial length targets for myopia control. Ophthalmic & Physiological Optics: The Journal of the British College of Ophthalmic Opticians (Optometrists), 41(3), 523–531. https://doi.org/10.1111/opo.12812
Chaplin, P. K., & Bradford, G. E. (2011). A historical review of distance vision screening eye charts: What to toss, what to keep, and what to replace. NASN School Nurse, 26(4), 221–228. https://doi.org/10.1177/1942602x11411094
Chen, A. H., Abu Bakar, N. F., & Arthur, P. (2019). Comparison of the pediatric vision screening program in 18 countries across five continents. Journal of Current Ophthalmology, 31(4), 357–365. https://doi.org/10.1016/j.joco.2019.07.006
Child and Adolescent Health Measurement Initiative. (2018-2019). National Survey of Children’s Health (NSCH) data query. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). www.childhealthdata.org
Chu, R., Huang, K., Barnhardt, C., & Chen, A. (2015). The effect of an on-site vision examination on adherence to vision screening recommendations. Journal of School Nursing, 31(2), 84–90. https://doi.org/10.1177/1059840514524599
Ciner, E., Cotter, S., Kulp, M., Hatch, S., Jackson, K., Moore, B., Mutti, D., & Summers, A. (2016). Childhood Vision Screening. https://aaopt.org/position-paper/
Collins, M. E., Guo, X., Mudie, L. I., Slavin, R. E., Madden, N., Chang, D., Owoeye, J., Repka, M. X., & Friedman, D. S. (2022a). Baseline vision results from the Baltimore Reading and Eye Disease Study. Canadian Journal of Ophthalmology, 57(1), 29–35. https://doi.org/10.1016/j.jcjo.2021.02.014
Collins, M. E., Guo, X., Repka, M. X., Neitzel, A. J., & Friedman, D. S. (2022b). Lessons learned from school-based delivery of vision care in Baltimore, Maryland. Asia-Pacific Journal of Ophthalmology, 11(1), 6–11. https://doi.org/10.1097/apo.0000000000000488
Committee on Practice and Ambulatory Medicine, Section on Ophthalmology. American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, & American Academy of Ophthalmology. (2003). Eye examination in infants, children, and young adults by pediatricians. Pediatrics, 111(4 Pt 1), 902–907. https://pubmed.ncbi.nlm.nih.gov/12671132/
Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology, Simon, G. R., Boudreau, A. D. A., Baker, C. N., Barden, G. A., Hackell, J. M., Hardin, A. P., Meade, K. E., Moore, S. B., Richerson, J., Lehman, S. S., Granet, D. B., Bradford, G. E., Rubin, S. E., Siatkowski, R. M., & Suh, D. W. (2016). Visual System Assessment in Infants, Children, and Young Adults by Pediatricians. Pediatrics, 137(1), 28–30. https://doi.org/10.1542/peds.2015-3596
Congdon, N., Zheng, M., Sharma, A., Choi, K., Song, Y., Zhang, M., Wang, M., Zhou, Z., Li, L., Liu, X., Liu, X., & Lam, D. S. C. (2008). Prevalence and Determinants of spectacle nonwear among rural Chinese secondary schoolchildren. Archives of Ophthalmology, 126(12), 1717–1723. https://doi.org/10.1001/archopht.126.12.1717
Cotter, S. A., Cyert, L. A., Miller, J. M., & Quinn, G. E. for the National Expert Panel to the National Center for Children’s Vision and Eye Health. (2015). Vision screening for children 36 to <72 months: Recommended practices. Optometry and Vision Science, 92(1), 6–16. https://doi.org/10.1097%2FOPX.0000000000000429
Couser, N. L., & Smith-Marshall, J. (2011). The Washington Metropolitan Pediatric Vision Screening Quality Control Assessment. ISRN Ophthalmology, 2011, 1–5. https://doi.org/10.5402/2011/801957
Davara, N. D., Chintoju, R., Manchikanti, N., Thinley, C., Vaddavalli, P. K., Rani, P. K., & Satgunam, P. (2022). Feasibility study for measuring patients’ visual acuity at home by their caregivers. Indian Journal of Ophthalmology, 70(6), 2125–2130. https://doi.org/10.4103/ijo.IJO_3085_21
Davidson, S. L., O’Hara, M., & Wagner, R. S. (2016). Management of progressive myopia. Journal of Pediatric Ophthalmology & Strabismus, 53(3), 134–136. https://doi.org/10.3928/01913913-20160418-01
De Samanta, A., Mauntana, S., Barsi, Z., Yarlagadda, B., & Nelson, P. C. (2023). Is your vision blurry? A systematic review of home-based visual acuity for telemedicine. Journal of Telemedicine and Telecare, 29(2), 81–90. https://doi.org/10.1177/1357633X20970398
de Venecia, B., Bradfield, Y., Trane, R. M., Bareiro, A., & Scalamogna, M. (2018). Validation of Peek Acuity application in pediatric screening programs in Paraguay. International Journal of Ophthalmology, 11(8), 1384–1389. https://doi.org/10.18240/ijo.2018.08.21
Department of Health and Human Services. (2023). Medicaid Program and CHIP mandatory Medicaid and Children’s Health Insurance Program (CHIP) core set reporting 2023. https://www.govinfo.gov/content/pkg/FR-2023-08-31/pdf/2023-18669.pdf
Detty, A. M. R. (2012). School-Based survey Participation: Oral health and BMI survey of Ohio third graders. Maternal and Child Health Journal, 17(7), 1208–1214. https://doi.org/10.1007/s10995-012-1107-7
Dhirar, N., Dudeja, S., Duggal, M., Gupta, P. C., Jaiswal, N., Singh, M., & Ram, J. (2020). Compliance to spectacle use in children with refractive errors—A systematic review and meta-analysis. BMC Ophthalmology, 20(1), 71. https://doi.org/10.1186/s12886-020-01345-9
Diao, W., Patel, J., Snitzer, M., Pond, M., Rabinowitz, M. P., Ceron, G., Bagley, K., Dennis, K., Weiner, R., Martinez-Helfman, S., Maria, K. S., Burke, B., Aultman, W. B., & Levin, A. V. (2016). The effectiveness of a mobile clinic in improving follow-up eye care for at-risk children. Journal of Pediatric Ophthalmology & Strabismus, 53(6), 344–348. https://doi.org/10.3928/01913913-20160629-04
Donahue, S. P., Arthur, B., Neely, D. E., Arnold, R. W., Silbert, D., Ruben, J. B., & POS Vision Screening Committee (2013). Guidelines for automated preschool vision screening: a 10-year, evidence-based update. Journal of AAPOS, 17(1), 4–8. https://doi.org/10.1016/j.jaapos.2012.09.012
Donahue, S. P., Baker, C. N., Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology, Simon, G. R., Boudreau, A. D. A., Barden, G. A., 3rd, Hackell, J. M., Hardin, A. P., Meade, K. E., Moore, S. B., Richerson, J., Lehman, S. S., Granet, D. B., Bradford, G. E., Rubin, S. E., Siatkowski, M., & Suh, D. W. (2016). Procedures for the evaluation of the visual system by pediatricians. Pediatrics, 137(1). https://doi.org/10.1542/peds.2015-3597
Donahue, S. P., Baker, J. D., Scott, W. E., Rychwalski, P., Neely, D. E., Tong, P., Bergsma, D., Lenahan, D., Rush, D., Heinlein, K., Walkenbach, R., & Johnson, T. M. (2006). Lions Clubs International Foundation core four photoscreening: Results from 17 programs and 400,000 preschool children. Journal of AAPOS, 10(1), 44–48. https://doi.org/10.1016/j.jaapos.2005.08.007
Donahue, S. P., & Nixon, C. N. (2016). Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics, 137(1), 28–30. https://doi.org/10.1542/peds.2015-3596
Donahue, S. P., Ruben, J. B., American Academy of Ophthalmology, American Academy of Pediatrics, Ophthalmology Section, American Association for Pediatric Ophthalmology and Strabismus, Children’s Eye Foundation, & American Association of Certified Orthoptists (2011). US Preventive Services Task Force vision screening recommendations. Pediatrics, 127(3), 569–570. https://doi.org/10.1542/peds.2011-0020
Dotan, G., Truong, B., Snitzer, M., McCauley, C., Martinez-Helfman, S., Santa Maria, K., & Levin, A. V. (2015). Outcomes of an inner-city vision outreach program: Give kids sight day. JAMA Ophthalmology, 133(5), 527–532. https://doi.org/10.1001/jamaophthalmol.2015.8
Drescher, J., & Domingue, B. W. (2023). The distribution of child physicians and early academic achievement. Health Services Research, 58(Suppl 2), 165–174. https://doi.org/10.1111/1475-6773.14188
Dudovitz, R. N., Izadpanah, N., Chung, P. J., & Slusser, W. (2015). Parent, teacher, and student perspectives on how corrective lenses improve child wellbeing and school function. Maternal and Child Health Journal, 20(5), 974–983. https://doi.org/10.1007/s10995-015-1882-z
Dutton, D. B., & Levine, S. (1989). Socioeconomic status and health: Overview, methodological critique, and reformulation. In J. P. Bunker, D. S. Gomby, & B. H. Kehrer (Eds.), Pathways to Health: The Role of Social Factors (pp. 29–69). The Henry J. Kaiser Family Foundation.
Ekdawi, N., Kipp, M. A., & Kipp, M. P. (2021). Mandated kindergarten eye examinations in a US suburban clinic: Is it worth the cost? Clinical Ophthalmology, 15, 1331–1337. https://doi.org/10.2147/OPTH.S300725
Elam, A. R., Tseng, V. L., Rodriguez, T. M., Mike, E. V., Warren, A. K., Coleman, A. L., & American Academy of Ophthalmology Taskforce on Disparities in Eye Care (2022). Disparities in vision health and eye care. Ophthalmology, 129(10), e89–e113. https://doi.org/10.1016/j.ophtha.2022.07.010
Ethan, D., Basch, C. E., Platt, R., Bogen, E., & Zybert, P. (2010). Implementing and evaluating a school-based program to improve childhood vision. The Journal of School Health, 80(7), 340–370. https://doi.org/10.1111/j.1746-1561.2010.00511.x
Fairbrother, G., Siegel, M. J., Friedman, S., Kory, P. D., & Butts, G. C. (2001). Impact of financial incentives on documented immunization rates in the inner city: results of a randomized controlled trial. Ambulatory Pediatrics, 1(4), 206–212. https://doi.org/10.1367/15394409(2001)001<0206:iofiod>2.0.co;2
Feng, P. W., Ahluwalia, A., Feng, H., & Adelman, R. A. (2020). National trends in the United States eye care workforce from 1995 to 2017. American Journal of Ophthalmology, 218, 128–135. https://doi.org/10.1016/j.ajo.2020.05.018
Flitcroft, D. I., He, M., Jonas, J. B., Jong, M., Naidoo, K., Ohno-Matsui, K., Rahi, J., Resnikoff, S., Vitale, S., & Yannuzzi, L. (2019) IMI – Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Investigative Ophthalmology & Visual Science, 60(3), M20–M30. https://doi.org/10.1167/iovs.18-25957
Foe, G., & Larson, E. L. (2016). Reading level and comprehension of research consent forms: An integrative review. Journal of Empirical Research on Human Research Ethics, 11(1), 31–46. https://doi.org/10.1177/1556264616637483
Frazier, M., Garces, I., Scarinci, I., & Marsh-Tootle, W. (2009). Seeking eye care for children: perceptions among Hispanic immigrant parents. Journal of Immigrant and Minority Health, 11(3), 215–221. https://doi.org/10.1007/s10903-008-9160-4
Furtado, J. M., Fernandes, A. G., Silva, J. C., Del Pino, S., & Hommes, C. (2023). Indigenous eye health in the Americas: The burden of vision impairment and ocular diseases. International Journal of Environmental Research and Public Health, 20(5). https://doi.org/10.3390%2Fijerph20053820
Guo, X., Nguyen, A. M., Vongsachang, H., Kretz, A. M., Mukherjee, M. R., Neitzel, A. J., Shakarchi, A. F., Friedman, D. S., Repka, M. X., & Collins, M. E. (2022). Refractive error findings in students who failed school-based vision screening. Ophthalmic Epidemiology, 29(4), 426–434. https://doi.org/10.1080/09286586.2021.1954664
Haller, K., Stolfi, A., & Duby, J. (2022). Comparison of unmet health care needs in children with intellectual disability, autism spectrum disorder and both disorders combined. Journal of Intellectual Disability Research, 66(7), 617–627. https://doi.org/10.1111/jir.12932
Hamm, L. M., Yashadhana, A., Burn, H., Black, J., Grey, C., Harwood, M., Peiris-John, R., Burton, M. J., Evans, J. R., & Ramke, J. (2021). Interventions to promote access to eyecare for non-dominant ethnic groups in high-income countries: A scoping review. BMJ Global Health, 6(9), e006188. https://doi.org/10.1136/bmjgh-2021-006188
Harewood, J. H, Contreras, M. C., Huang, K. H., Leach, S. L., & Wang, J. (2024). [Access to myopia care—A scoping review]. Paper commissioned by the Committee on Focus on Myopia: Pathogenesis and Rising Incidence.
Hariton, E., & Locascio, J. J. (2018). Randomised controlled trials—The gold standard for effectiveness research: Study design: Randomised controlled trials. BJOG: An International Journal of Obstetrics and Gynaecology, 125(13), 1716. https://doi.org/10.1111/1471-0528.15199
Hark, L. A., Shiuey, E., Yu, M., Tran, E., Mayro, E. L., Zhan, T., Pond, M., Tran, J., Siam, L., & Levin, A. V. (2018). Efficacy and outcomes of a summer-based pediatric vision screening program. Journal of AAPOS, 22(4), 309.e1–309.e7. https://doi.org/10.1016/j.jaapos.2018.04.006
Harris, N., Roche, E., Lee, P., Asper, L., Wiseman, N., Keel, R., Duffy, S., & Sofija, E. (2023). Vision screening outcomes of 4-5 year-olds reflect the social gradient. Clinical & Experimental Optometry, 106(6), 640–644. https://doi.org/10.1080/08164622.2022.2109947
Hartmann, E. E., Block, S. S., Wallace, D. K., & National Expert Panel to the National Center for Children’s Vision and Eye Health. (2015). Vision and eye health in children 36 to <72 months: proposed data system. Optometry and Vision Science, 92(1), 24–30. https://doi.org/10.1097%2FOPX.0000000000000445
Hartmann, E. E., Bradford, G. E., Chaplin, P. K., Johnson, T., Kemper, A. R., Kim, S., Marsh-Tootle, W., & PUPVS Panel for the American Academy of Pediatrics. (2006). Project Universal Preschool Vision Screening: A demonstration project. Pediatrics, 117(2), e226–e237. https://doi.org/10.1542/peds.2004-2809
Healthy People 2030. (n.d.). Social determinants of health. https://health.gov/healthypeople/priority-areas/social-determinants-health
Hendler, K., Mehravaran, S., Lu, X., Brown, S. I., Mondino, B. J., & Coleman, A. L. (2016). Refractive errors and amblyopia in the UCLA Preschool Vision Program: First year results. American Journal of Ophthalmology, 172, 80–86. https://doi.org/10.1016/j.ajo.2016.09.010
Henstenburg, J., Thau, A., Markovitz, M., Plumb, J., & Markovitz, B. (2019). Visual impairment and ocular pathology among the urban American homeless. Journal of Health Care for the Poor and Underserved, 30(3), 940–950. https://doi.org/10.1353/hpu.2019.0066
Hered, R. W., & Wood, D. L. (2013). Preschool vision screening in primary care pediatric practice. Public Health Reports, 128(3), 189–197. https://doi.org/10.1177/003335491312800309
Heslin, K. C., Casey, R., Shaheen, M. A., Cardenas, F., & Baker, R. S. (2006). Racial and ethnic differences in unmet need for vision care among children with special health care needs. Archives of Ophthalmology, 124(6), 895–902. https://doi.org/10.1001/archopht.124.6.895
Hillrom. (2020). Reimbursement guide for instrument-based vision screening. https://www.hillrom.com/content/dam/hillrom-aem/us/en/marketing/products/spot-vision-screener/documents/APR101102-EN-R1_Spot-Vision-Screener-Reimbursement-Guide_LR.pdf
Holmes, J. M., & Levi, D. M. (2018). Treatment of amblyopia as a function of age. Vision Neuroscience, 35, E015. https://doi.org/10.1017/S0952523817000220
Hoover, K., Di Guglielmo, M. D., & Perry, B. (2023). Disparities in vision screening in primary care for young children with autism spectrum disorder. Pediatrics, 151(4). https://doi.org/10.1542/peds.2022-059998
Hou, W., Norton, T. T., Hyman, L., Gwiazda, J., & COMET Group (2018). Axial elongation in myopic children and its association with myopia progression in the correction of myopia evaluatin trial. Eye & Contact Lens, 44(4), 248–259. https://doi.org/10.1097/ICL.0000000000000505
Huang, A. H., Guo, X., Mudie, L. I., Wolf, R., Owoeye, J., Repka, M. X., Friedman, D. S., Slavin, R. E., & Collins, M. E. (2019). Baltimore Reading and Eye Disease Study (BREDS): Compliance and satisfaction with glasses usage. Journal of AAPOS, 23(4), 207.e1–207.e6. https://doi.org/10.1016/j.jaapos.2019.01.018
Hunter, D. G. (2013). Targeting treatable disease—not just risk factors—in pediatric vision screening. Journal of AAPOS, 17(1), 2–3. https://doi.org/10.1016/j.jaapos.2012.10.009
Hutchinson, A. K., Morse, C. L., Hercinovic, A., Cruz, O. A., Sprunger, D. T., Repka, M. X., Lambert, S. R., Wallace, D. K., & American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. (2023). Pediatric eye evaluations preferred practice pattern. Ophthalmology, 130(3), P222–P270. https://doi.org/10.1016/j.ophtha.2022.10.030
Illinois State Board of Education (2024). Data & accountability: Health requirements/student health data.
Ji, P., Flay, B., Dubois, D., Patton, V., & Day, J. (2006). Consent form return rates for third-grade urban elementary students. American Journal of Health Behavior, 30(5), 467–474. https://doi.org/10.5555/ajhb.2006.30.5.467
Jin, Y. P., & Trope, G. E. (2011). Eye care utilization in Canada: disparity in the publicly funded health care system. Canadian Journal of Ophthalmology. Journal Canadien D’ophtalmologie, 46(2), 133–138. https://doi.org/10.3129/i10-120
Jonas, D. E., Amick, H. R., Wallace, I. F., Feltner, C., Vander Schaaf, E. B., Brown, C. L., & Baker, C. (2017). Vision screening in children aged 6 months to 5 years: Evidence report and systematic review for the US Preventive Services Task Force. JAMA, 318(9), 845–858. https://doi.org/10.1001/jama.2017.9900
Jones-Jordan, L. A., Sinnott, L. T., Manny, R. E., Cotter, S. A., Kleinstein, R. N., Mutti, D. O., Twelker, J. D., Zadnik, K., & Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group. (2010). Early childhood refractive error and parental history of myopia as predictors of myopia. Investigative Ophthalmology & Visual Science, 51(1), 115–121. https://doi.org/10.1167/iovs.08-3210
Jong, M., Jonas, J. B., Wolffsohn, J. S., Berntsen, D. A., Cho, P., Clarkson-Townsend, D., Flitcroft, D. I., Gifford, K. L., Haarman, A. E. G., Pardue, M. T., Richdale, K., Sankaridurg, P., Tedja, M. S., Wildsoet, C. F., Bailey-Wilson, J. E., Guggenheim, J. A., Hammond, C. J., Kaprio, J., MacGregor, S., & Smith, E. L., 3rd. (2021). IMI 2021 Yearly Digest. Investigative Ophthalmology & Visual Science, 62(5), 7. https://doi.org/10.1167/iovs.62.5.7
Kemper, A. R., & Clark, S. J. (2006). Preschool vision screening in pediatric practices. Clinical Pediatrics, 45(3), 263–266. https://doi.org/10.1177/000992280604500309
Kemper, A. R., Bruckman, D., & Freed, G. L. (2003). Receipt of specialty eye care by children. Ambulatory Pediatrics, 3(5), 270–274. https://doi.org/10.1367/15394409(2003)003<0270:ROSECB>2.0.CO;2
Kemper, A. R., Uren, R. L., & Clark, S. J. (2006). Barriers to follow-up eye care after preschool vision screening in the primary care setting: findings from a pilot study. Journal of AAPOS, 10(5), 476–478. https://doi.org/10.1016/j.jaapos.2006.07.009
Kentucky Department of Education. (2024). Student health services: Student health data. https://www.education.ky.gov/districts/SHS/Pages/Student-Health-Data.aspx
Killeen, O. J., Cho, J., Newman-Casey, P. A., Kana, L., & Woodward, M. A. (2021). Barriers and facilitators to obtaining eyeglasses for vulnerable patients in a Michigan free clinic. Optometry and Vision Science, 98(3), 243–249. https://doi.org/10.1097/opx.0000000000001661
Killeen, O. J., Choi, H., Kannan, N. S., Asare, A. O., Stagg, B. C., & Ehrlich, J. R. (2023). Association between health insurance and primary care vision testing among children and adolescents. JAMA Ophthalmology, 141(9), 909–911. https://doi.org/10.1001/jamaophthalmol.2023.3644
Kim, P., Daly, J. M., Berkowitz, S., & Levy, B. T. (2020). Use of the Fluoride Varnish Billing Code in a Tertiary Care Center Setting. Journal of Primary Care & Community Health, 11. https://doi.org/10.1177/2150132720913736
Kimel, L. S. (2006). Lack of follow-up exams after failed school vision screenings: An investigation of contributing factors. The Journal of School Nursing, 22(3), 156–162. https://doi.org/10.1177/10598405060220030601
Kindle, T., & Spencer, T. (2019). A review of childhood vision screening laws and programs across the United States. South Dakota Medicine, 72(7), 299–302. https://pubmed.ncbi.nlm.nih.gov/31461584/
Kleinstein, R. N., Mutti, D. O., Sinnott, L. T., Jones-Jordan, L. A., Cotter, S. A., Manny, R. E., Twelker, J. D., Zadnik, K., & Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study Group. (2021). Uncorrected refractive error and distance visual acuity in children aged 6 to 14 years. Optometry and Vision Science, 98(1), 3–12. https://doi.org/10.1097/opx.0000000000001630
Kleinstein, R. N., Sinnott, L. T., Jones-Jordan, L. A., Sims, J., Zadnik, K., & Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study Group. (2012). New cases of myopia in children. Archives of Ophthalmology, 130(10), 1274–1279. https://doi.org/10.1001/archophthalmol.2012.1449
Kodjebacheva, G., Brown, E. R., Estrada, L., Yu, F., & Coleman, A. L. (2011). Uncorrected refractive error among first-grade students of different racial/ethnic groups in southern California: Results a year after school-mandated vision screening. Journal of Public Health Management and Practice, 17(6), 499–505. https://doi.org/10.1097/PHH.0b013e3182113891
Kodjebacheva, G. D., Maliski, S., & Coleman, A. L. (2015). Use of eyeglasses among children in elementary school: Perceptions, behaviors, and interventions discussed by parents, school nurses, and teachers during focus groups. American Journal of Health Promotion, 29(5), 324–331. https://doi.org/10.4278/ajhp.120315-QUAL-140
Kodjebacheva, G., Brown, E. R., Estrada, L., Yu, F., & Coleman, A. L. (2011). Uncorrected refractive error among first-grade students of different racial/ethnic groups in southern California: results a year after school-mandated vision screening. Journal of Public Health Management and Practice, 17(6), 499-505. doi:10.1097/PHH.0b013e3182113891
Kruszewski, K., May, C., & Silverstein, E. (2023). Evaluation of a combined school-based vision screening and mobile clinic program. Journal of AAPOS, 27(2), 91.e1–91.e5. https://doi.org/10.1016/j.jaapos.2023.01.010
Kulp, M. T., & Group, V. I. P. S. (2009). Findings from the Vision in Preschoolers (VIP) Study. Optometry and Vision Science, 86(6), 619–623. https://doi.org/10.1097/OPX.0b013e3181a59bf5
Kulp, M. T., Ciner, E., Maguire, M., Moore, B., Pentimonti, J., Pistilli, M., Cyert, L., Candy, T. R., Quinn, G., & Ying, G. (2016). Uncorrected hyperopia and preschool early literacy. Ophthalmology, 123(4), 681–689. https://doi.org/10.1016/j.ophtha.2015.11.023
Kulp, M. T., Ciner, E., Ying, G. S., Candy, T. R., Moore, B. D., Orel-Bixler, D., & VIP Study Group, and the VIP-HIP Study Group. (2022). Vision screening, vision disorders, and impacts of hyperopia in young children: Outcomes of the Vision in Preschoolers (VIP) and Vision in Preschoolers - Hyperopia in Preschoolers (VIP-HIP) studies. Asia-Pacific Journal of Ophthalmology, 11(1), 52–58. https://doi.org/10.1097/APO.0000000000000483
Lalor, S. J. H., Formankiewicz, M. A., & Waugh, S. J. (2016). Crowding and visual acuity measured in adults using paediatric test letters, pictures and symbols. Vision Research, 121, 31–38. https://doi.org/10.1016/j.visres.2016.01.007
Lam, M., & Grasse, N. (2019). Community health centers (CHCs) under environmental uncertainty: An examination of the Affordable Care Act of 2010 and early Medicaid expansion on CHC margin. Nonprofit Policy Forum, 10(2). https://doi.org/10.1515/npf-2019-0016
Law, M. X., Pimentel, M. F., Oldenburg, C. E., & de Alba Campomanes, A. G. (2020). Positive predictive value and screening performance of GoCheck Kids in a primary care university clinic. Journal of AAPOS, 24(1), 17.e1–17.e5. https://doi.org/10.1016/j.jaapos.2019.11.006
Lee, K. E., Sussberg, J. A., Nelson, L. B., & Thuma, T. B. (2023). What we learned about the economic and workforce issues in pediatric ophthalmology: Access to eye care and possible solutions. Journal of Pediatric Ophthalmology & Strabismus, 60(5), 323–329. https://doi.org/10.3928/01913913-20230620-02
Lee, P. P., Hoskins, H. D., & Parke, D. W. (2007). Access to care: Eye care provider workforce considerations in 2020. Archives of Ophthalmology, 125(3), 406–410. https://doi.org/10.1001/archopht.125.3.406
Lee, P. P., West, S. K., Block, S. S., Clayton, J., Cotch, M. F., Flynn, C., Geiss, L. S., Klein, R., Olsen, T. W., Owsley, C., Primo, S. A., Rubin, G. S., Ryskulova, A., Sharma, S., Friedman, D. S., Zhang, X., Crews, J. E., & Saaddine, J. B. (2012). Surveillance of disparities in vision and eye health in the United States: An expert panel’s opinions. American Journal of Ophthalmology, 154(6 Suppl), S3–S7. https://doi.org/10.1016/j.ajo.2012.09.006
Lee, Y. H., Chen, A. X., Varadaraj, V., Hong, G. H., Chen, Y., Friedman, D. S., Stein, J. D., Kourgialis, N., & Ehrlich, J. R. (2018). Comparison of access to eye care appointments between patients with Medicaid and those with private health care insurance. JAMA Ophthalmology, 136(6), 622–629. https://doi.org/10.1001/jamaophthalmol.2018.0813
Levinson, D. R. (2010). Most Medicaid children in nine states are not receiving all required preventive screening services. Office of Inspector General, U.S. Department of Health and Human Services. https://oig.hhs.gov/oei/reports/oei-05-08-00520.pdf
Lillvis, J. H., Lillvis, D. F., Towle-Miller, L. M., Wilding, G. E., & Kuo, D. Z. (2020). Association of state vision screening requirements with parent-reported vision testing in young children. Journal of AAPOS, 24(5), 291.e1–291.e6. https://doi.org/10.1016/j.jaapos.2020.04.015
Lipson, M. J., Boland, B., & McAlinden, C. (2022). Vision-related quality of life with myopia management: A review. Contact Lens & Anterior Eye: The Journal of the British Contact Lens Association, 45(3), 101538. https://doi.org/10.1016/j.clae.2021.101538
Loh, A. R., & Chiang, M. F. (2018). Pediatric vision screening. Pediatrics in Review, 39(5), 225–234. https://doi.org/10.1542/pir.2016-0191
Lowry, E. A., & de Alba Campomanes, A. G. (2016). Cost-effectiveness of school-based eye examinations in preschoolers referred for follow-up from visual screening. JAMA Ophthalmology, 134(6), 658–664. https://doi.org/10.1001/jamaophthalmol.2016.0619
Lyons, S. A., Johnson, C., & Majzoub, K. (2011). School based vision centers: Striving to optimize learning. Work, 39(1), 15–19. https://doi.org/10.3233/wor-2011-1146
Ma, X., Zhou, Z., Yi, H., Pang, X., Shi, Y., Chen, Q., Meltzer, M. E., le Cessie, S., He, M., Rozelle, S., Liu, Y., & Congdon, N. (2014). Effect of providing free glasses on children’s educational outcomes in China: Cluster randomized controlled trial. BMJ (Clinical research ed.), 349, g5740. https://doi.org/10.1136/bmj.g5740
Maguire, M. G., & Vision in Preschoolers Study Group. (2007). Children unable to perform screening tests in vision in preschoolers study: Proportion with ocular conditions and impact on measures of test accuracy. Investigative Ophthalmology & Visual Science, 48(1), 83–87. https://doi.org/10.1167/iovs.06-0384
Manny, R. E., Sinnott, L. T., Jones-Jordan, L. A., Messer, D., Twelker, J. D., Cotter, S. A., Kleinstein, R. N., Crescioni, M., & CLEERE Study Group. (2012). Predictors of adequate correction following vision screening failure. Optometry and Vision Science, 89(6), 892–900. https://doi.org/10.1097/OPX.0b013e318255da73
Marsh-Tootle, W. L., Frazier, M. G., Kohler, C. L., Dillard, C. M., Davis, K., Schoenberger, Y. M., & Wall, T. C. (2012). Exploring pre-school vision screening in primary care offices in Alabama. Optometry and Vision, 89(10), 1521–1531. https://doi.org/10.1097/OPX.0b013e318269ca9f
Marsh-Tootle, W. L., Funkhouser, E., Frazier, M. G., Crenshaw, K., & Wall, T. C. (2010). Knowledge, attitudes, and environment: What primary care providers say about pre-school vision screening. Optometry and Vision Science, 87(2), 104–111. https://doi.org/10.1097/OPX.0b013e3181cc8d7c
Marzolf, A. L., Peterseim, M. M., Forcina, B. D., Papa, C., Wilson, M. E., Cheeseman, E. W., & Trivedi, R. H. (2017). Use of the Spot Vision Screener for patients with developmental disability. Journal of AAPOS, 21(4), 313–315.e1. https://doi.org/10.1016/j.jaapos.2017.04.008
McCurry, T. C., Lawrence, L. M., Wilson, M. E., & Mayo, L. (2013). The plusoptiX S08 photoscreener as a vision screening tool for children with autism. Journal of AAPOS, 17(4), 374–377. https://doi.org/10.1016/j.jaapos.2013.05.006
McNamara, N. A., & Polse, K. A. (2019). Community health centers: A model for integrating eye care services with the practice of primary care medicine. Optometry and Vision Science, 96(12), 905–909. https://doi.org/10.1097/OPX.0000000000001458
Medicine, I. O. (2012). Essential health benefits. National Academies Press. https://doi.org/10.17226/13234
Messer, D. H., Mitchell, G. L., Twelker, J. D., Crescioni, M., & CLEERE Study Group. (2012). Spectacle wear in children given spectacles through a school-based program. Optometry and Vision Science, 89(1), 19–26. https://doi.org/10.1097/OPX.0b013e3182357f8c
Miller, J. M., Lessin, H. R., American Academy of Pediatrics Section on Ophthalmology, Committee on Practice and Ambulatory Medicine, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, & American Association of Certified Orthoptists. (2012). Instrument-based pediatric vision screening policy statement. Pediatrics, 130(5), 983–986. https://doi.org/10.1542/peds.2012-2548
Modest, J. R., Majzoub, K. M., Moore, B., Bhambhani, V., McLaughlin, S. R., & Vernacchio, L. (2017). Implementation of instrument-based vision screening for preschool-age children in primary care. Pediatrics, 140(1), e20163745. https://doi.org/10.1542/peds.2016-3745
Morrison, A. S. (1998). Screening. In K. J. Rothman & S. Greenland (Eds.), Modern Epidemiology (2nd ed., p. 510). Lippincott Williams & Wilkins.
Mu, Y., Bi, H., Ekure, E., Ding, G., Wei, N., Hua, N., Qian, X., & Li, X. (2016). Performance of spot photoscreener in detecting amblyopia risk factors in Chinese pre-school and school age children attending an eye clinic. PloS One, 11(2), e0149561. https://doi.org/10.1371/journal.pone.0149561
Muhammad, M., & Tumin, D. (2022). Unmet needs for vision care among children with gaps in health insurance coverage. Journal of AAPOS, 26(2), 63.e1–63.e4. https://doi.org/10.1016/j.jaapos.2021.12.005
Musch, D. C., Andrews, C. A., Schumann, R. A., & Baker, J. D. (2022). A comparative study of two photoscreening devices with manual vision screening involving preschool children. Journal of Pediatric Ophthalmology & Strabismus, 59(1), 46–52. https://doi.org/10.3928/01913913-20210610-01
National Academies of Sciences, Engineering, and Medicine. (2016). Making eye health a population health imperative: Vision for tomorrow. The National Academies Press. https://doi.org/10.17226/23471
National Center for Children’s Vision and Eye Health. (2016). Vision screening guidelines by age. https://nationalcenter.preventblindness.org/vision-screening-guidelines-by-age/
National Center for Education Statistics. (n.d.). Number and percentage of public school students eligible for free or reduced-price lunch, by state: Selected school years, 2000-01 through 2021-22. https://nces.ed.gov/programs/digest/d22/tables/dt22_204.10.asp
Nebraska Legislature, State ex rel. Shineman v. Board of Education, 152 Neb. 644, 42 N.W.2d 168 (1950).
Newacheck, P. W., Hughes, D. C., & Stoddard, J. J. (1996). Children’s access to primary care: differences by race, income, and insurance status. Pediatrics, 97(1), 26–32.
Nishimura, M., Wong, A., Cohen, A., Thorpe, K., & Maurer, D. (2019). Choosing appropriate tools and referral criteria for vision screening of children aged 4-5 years in Canada: a quantitative analysis. British Medical Journal Open, 9(9), e032138. https://doi.org/10.1136/bmjopen-2019-032138
Nishimura, M., Wong, A., Dimaris, H., & Maurer, D. (2020). Feasibility of a school-based vision screening program to detect undiagnosed visual problems in kindergarten children in Ontario. Canadian Medical Association Journal, 192(29), E822–E831. https://doi.org/10.1503/cmaj.191085
Nishimura, M., Wong, A., & Maurer, D. (2024). Continued care and provision of glasses are necessary to improve visual and academic outcomes in children: Experience from a cluster-randomized controlled trial of school-based vision screening. Canadian Journal of Public Health. https://doi.org/10.17269/s41997-024-00884-8
Nowroozzadeh, M. H. (2016). School-based myopia prevention effort. JAMA, 315(8), 819–820. https://jamanetwork.com/journals/jama/fullarticle/2492866
O’Colmain, U., Low, L., Gilmour, C., & MacEwen, C. J. (2016). Vision screening in children: A retrospective study of social and demographic factors with regards to visual outcomes. British Journal of Ophthalmology, 100(8), 1109–1113. https://doi.org/10.1136/bjophthalmol-2015-307206
O’Donnell, L., Duran, R., San Doval, A., Breslin, M., & Juhn, G. (1997). Obtaining written parent permission for school-based health surveys of urban young adolescents. Journal of Adolescent Health, 21, 376–383. https://doi.org/10.1016/S1054-139X(97)00110-3
O’Hara, M. A. (2016). Instrument-based pediatric vision screening. Current Opinion in Ophthalmology, 27(5), 398–401. https://doi.org/10.1097/icu.0000000000000289
Oke, I., Lutz, S. M., Hunter, D. G., & Galbraith, A. A. (2023). Vision screening among children with private insurance: 2010–2019. Pediatrics, 152(3), e2023062114. https://doi.org/10.1542/peds.2023-062114
Painter, S., Ramm, L., Wadlow, L., O’Connor, M., & Sond, B. (2021). Parental home vision testing of children during COVID-19 pandemic. British and Irish Orthoptic Journal, 17(1), 13–19. https://doi.org/10.22599/bioj.157
Payerols, A., Eliaou, C., Trezeguet, V., Villain, M., & Daien, V. (2016). Accuracy of PlusOptix A09 distance refraction in pediatric myopia and hyperopia. BMC Ophthalmology, 16, 72. https://doi.org/10.1186/s12886-016-0247-8
Perez, S., Sabharwal, S., Nakayoshi, A., & de Alba Campomanes, A. G. (2022). Parental perspectives on factors influencing eyeglass wear compliance in preschoolers from low-income families in San Francisco. Journal of AAPOS, 26(4), 183.e1–183.e6. https://doi.org/10.1016/j.jaapos.2022.05.004
Peterseim, M. M. W., Papa, C. E., Wilson, M. E., Cheeseman, E. W., Wolf, B. J., Davidson, J. D., & Trivedi, R. H. (2014). Photoscreeners in the pediatric eye office: Compared testability and refractions on high-risk children. American Journal of Ophthalmology, 158, 932–938. https://doi.org/10.1016%2Fj.ajo.2014.07.041
Peterseim, M. M., Papa, C. E., Parades, C., Davidson, J., Sturges, A., Oslin, C., Merritt, I., & Morrison, M. (2015). Combining automated vision screening with on-site examinations in 23 schools: ReFocus on Children Program 2012 to 2013. Journal of Pediatric Ophthalmology and Strabismus, 52(1), 20–24. https://doi.org/10.3928/01913913-20141124-01
Pirindhavellie, G. P., Yong, A. C., Mashige, K. P., Naidoo, K. S., & Chan, V. F. (2023). The impact of spectacle correction on the well-being of children with vision impairment due to uncorrected refractive error: a systematic review. BMC Public Health, 23(1), 1575. https://doi.org/10.1186/s12889-023-16484-z
Pober, J. S., Neuhauser, C. S., & Pober, J. M. (2001). Obstacles facing translational research in academic medical centers. FASEB Journal, 15(13), 2303–2313. https://doi.org/10.1096/fj.01-0540lsf
Prevent Blindness. (2020). Pediatric vision benefits available under the Affordable Care Act. https://preventblindness.org/pediatric-vision-benefits-available-under-the-affordable-care-act/
___. (2022). Analysis of School-Age Vision Screening by State. https://preventblindness.org/vision-screening-requirements-by-state/
Qian, X., Li, Y., Ding, G., Li, J., Lv, H., Hua, N., Wei, N., He, L., Wei, L., Li, X., & Wang, J. (2019). Compared performance of Spot and SW800 photoscreeners on Chinese children. The British Journal of Ophthalmology, 103(4), 517–522. https://doi.org/10.1136/bjophthalmol-2018-311885
Rajalakshmi, A. R., & Rajeshwari, M. (2019). Efficacy of bruckner’s test for screening of refractive errors by non-ophthalmologist versus ophthalmologist: A comparative study. Middle East African Journal of Ophthalmology, 26(4), 185–188. https://doi.org/10.4103%2Fmeajo.MEAJO_121_19
Rajesh, A. E., Davidson, O., Lacy, M., Chandramohan, A., Lee, A. Y., Lee, C. S., Tarczy-Hornoch, K., & IRIS® Registry Analytic Center Consortium. (2023). Race, Ethnicity, Insurance, and Population Density Associations with Pediatric Strabismus and Strabismic Amblyopia in the IRIS® Registry. Ophthalmology, 130(10), 1090–1098. https://doi.org/10.1016/j.ophtha.2023.06.008
Register, S. J. (2010). Visual acuity and stereopsis screening results in an underserved community. Optometry, 81(4), 200–204. https://doi.org/10.1016/j.optm.2009.11.002
Rein, D. B., Wittenborn, J. S., Phillips, E. A., Saaddine, J. B., & Vision and Eye Health Surveillance System Study Group. (2018). Establishing a vision and eye health surveillance system for the nation: A status update on the vision and eye health surveillance system. Ophthalmology, 125(4), 471–473. https://doi.org/10.1016/j.ophtha.2017.10.014
Repka, M. X., Li, C., & Lum, F. (2023). Multivariable analyses of amblyopia treatment outcomes from a clinical data registry. Ophthalmology, 130(2), 164–166. https://doi.org/10.1016/j.ophtha.2022.09.005
Robert Wood Johnson Foundation Commission to Build a Healthier America. (2009). Race and socioeconomic factors affect opportunities for better health (Issue Brief No. 5). https://folio.iupui.edu/bitstream/handle/10244/659/commission2009issuebrief5.pdf?sequence=2
Rono, H. K., Bastawrous, A., Macleod, D. A. I., Wanjala, E., Di Tanna, G. L., Weiss, H. A., & MJ, B. (2018). Smartphone-based screening for visual impairment in Kenyan school children: A cluster randomised controlled trial. Lancet Global Health, 6, 924–932. https://doi.org/10.1016/s2214-109x(18)30244-4
Ross, E. L., & Stein, J. D. (2016). Enhancing the Value of Preschool Vision Screenings. JAMA Ophthalmology, 134(6):664–665. doi:10.1001/jamaophthalmol.2016.0822
Sabharwal, S., Nakayoshi, A., Lees, C. R., Perez, S., & de Alba Campomanes, A. G. (2021). Prevalence and factors associated with eyeglass wear compliance among preschoolers from low-income families in San Francisco, California. JAMA Ophthalmology, 139(4), 433–440. https://doi.org/10.1001/jamaophthalmol.2020.7053
Sankaridurg, P., Berntsen, D. A., Bullimore, M. A., Cho, P., Flitcroft, I., Gawne, T. J., Gifford, K. L., Jong, M., Kang, P., Ostrin, L. A., Santodomingo-Rubido, J., Wildsoet, C., & Wolffsohn, J. S. (2023). IMI 2023 Digest. Investigative Ophthalmology & Visual Science, 64(6), 7. https://doi.org/10.1167/iovs.64.6.7
Saxena, R., Sharma, P., & Pediatric Ophthalmology Expert Group. (2020). National consensus statement regarding pediatric eye examination, refraction, and amblyopia management. Indian Journal of Ophthalmology, 68(2), 325–332. https://doi.org/10.4103/ijo.IJO_471_19
Saydah, S. H., Gerzoff, R. B., Saaddine, J. B., Zhang, X., & Cotch, M. F. (2020). Eye care among US adults at high risk for vision loss in the United States in 2002 and 2017. JAMA Ophthalmology, 138(5), 479–489. https://doi.org/10.1001/jamaophthalmol.2020.0273
Scheive, M., Rowe, L. W., Tso, H. L., Wurster, P., Kalafatis, N. E., Camp, D. A., & Yung, C. W. R. (2022). Assessment of patient follow-up from student-run free eye clinic to county ophthalmology clinic. Scientific Reports, 12(1). https://doi.org/10.1038/s41598-022-05033-0
Secor-Turner, M., Sieving, R., Widome, R., Plowman, S., & Vanden Berk, E. (2010). Active parent consent for health surveys with urban middle school students: Processes and outcomes. Journal of School Health, 80(2), 73–79. https://doi.org/10.1111/j.1746-1561.2009.00468.x
Shakarchi, A. F., & Collins, M. E. (2019). Referral to community care from school-based eye care programs in the United States. Survey of Ophthalmology, 64(6), 858–867. https://doi.org/10.1016/j.survophthal.2019.04.003
Sharma, A., Wong, A. M., Colpa, L., Chow, A. H., & Jin, Y. P. (2016). Socioeconomic status and utilization of amblyopia services at a tertiary pediatric hospital in Canada. Canadian Journal of Ophthalmology, 51(6), 452–458. https://doi.org/10.1016/j.jcjo.2016.05.001
Shin, P., & Finnegan, B. (2009). Assessing the need for on-site eye care professionals in community health centers. Policy brief (George Washington University Center for Health Services Research and Policy), 1–23. https://hsrc.himmelfarb.gwu.edu/cgi/viewcontent.cgi?article=1021&context=sphhs_policy_briefs
Shipman, S. A., Lan, J., Chang, C. H., & Goodman, D. C. (2011). Geographic maldistribution of primary care for children. Pediatrics, 127(1), 19–27. https://doi.org/10.1542/peds.2010-0150
Siegler, N. E., Walsh, H. L., & Cavuoto, K. M. (2024). Access to pediatric eye care by practitioner type, geographic distribution, and US population demographics. JAMA Ophthalmology, 142(5), 454–461. https://doi.org/10.1001/jamaophthalmol.2024.0612
Sight Savers America. (2020). 2019–2020 Biennial Report. https://sightsaversamerica.org/wp-content/uploads/2021/08/2019-2020-Biennial-Report.pdf
Silverstein, M., Scharf, K., Mayro, E. L., Hark, L. A., Snitzer, M., Anhalt, J., Pond, M., Siam, L., Tran, J., Hill-Bennett, T., Zhan, T., & Levin, A. V. (2021). Referral outcomes from a vision screening program for school-aged children. Canadian Journal of Ophthalmology, 56(1), 43–48. https://doi.org/10.1016/j.jcjo.2020.07.009
Simon, G. R., Boudreau, A. D. A., Baker, C. N., Barden, G. A., Hackell, J. M., Hardin, A. P., Meade, K. E., Moore, S. B., Richerson, J., Lehman, S. S., Granet, D. B., Bradford, G. E., Rubin, S. E., Siatkowski, R. M., Suh, D. W., & Granet, D. B. (2016). Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics, 137(1). https://doi.org/10.1542/peds.2015-3596
Simon, J. W., Bradfield, Y., Smith, J., Ahn, E., & France, T. D. (2007). Recruitment and manpower in pediatric ophthalmology and strabismus. Journal of AAPOS, 11(4), 336–340. https://doi.org/10.1016/j.jaapos.2007.04.004
Singman, E., Matta, N., Fairward, A., & Silbert, D. (2013). Evaluation of PlusoptiX photoscreening during examinations of children with autism. Strabismus, 21(2), 103-105. https://doi.org/10.3109/09273972.2013.786736
Sopeyin, A., Young, B. K., & Howard, M. A. A. (2021). 2020 evaluation of portable vision screening instruments. Yale Journal of Biology and Medicine, 94, 107–114. https://pubmed.ncbi.nlm.nih.gov/33795987/
State of Alabama. (2024). State of Alabama Executive Budget fiscal year 2024. https://budget.alabama.gov/wp-content/uploads/2023/03/State-of-Alabama-Budget-Report-2024-FINAL-Updated.pdf
State of Illinois. (2024). State of Illinois eye examination report. http://www.idph.state.il.us/HealthWellness/EyeExamReport.pdf
Stein, J. D., Andrews, C., Musch, D. C., Green, C., & Lee, P. P. (2016). Sight-threatening ocular diseases remain underdiagnosed among children of less affluent families. Health affairs (Project Hope), 35(8), 1359–1366. https://doi.org/10.1377/hlthaff.2015.1007
Stults, C. D., Liang, S. Y., Wilcox, J., & Nyong’o, O. L. (2024). Amblyopia care trends following widespread photoscreener adoption. JAMA Ophthalmology, 142(3), 188–197. https://doi.org/10.1001/jamaophthalmol.2023.6434
Sung, N. S., Crowley, W. F., Jr, Genel, M., Salber, P., Sandy, L., Sherwood, L. M., Johnson, S. B., Catanese, V., Tilson, H., Getz, K., Larson, E. L., Scheinberg, D., Reece, E. A., Slavkin, H., Dobs, A., Grebb, J., Martinez, R. A., Korn, A., & Rimoin, D. (2003). Central challenges facing the national clinical research enterprise. JAMA, 289(10), 1278–1287. https://doi.org/10.1001/jama.289.10.1278
Swanson, M. W., Lee, S. D., Frazier, M. G., Bade, A., & Coulter, R. A. (2020). Vision screening among children with autism spectrum disorder. Optometry and Vision Science, 97(11), 917–928. https://doi.org/10.1097/opx.0000000000001593
Syed, S. T., Gerber, B. S., & Sharp, L. K. (2013). Traveling towards disease: Transportation barriers to health care access. Journal of Community Health, 38(5), 976–993. https://doi.org/10.1007/s10900-013-9681-1
Thirunavukarasu, A. J., Hassan, R., Limonard, A., & Savant, S. V. (2023). Accuracy and reliability of self-administered visual acuity tests: Systematic review of pragmatic trials. PLoS One, 18(6), e0281847. https://doi.org/10.1371/journal.pone.0281847
Tigges B. B. (2003). Parental consent and adolescent risk behavior research. Journal of Nursing Scholarship, 35(3), 283–289. https://doi.org/10.1111/j.1547-5069.2003.00283.x
United States Department of Health and Human Services. (2024). Social Determinants of Health. https://health.gov/healthypeople/priority-areas/social-determinants-health
United States Preventive Services Task Force. (2024). AAFP Clinical Preventive Services Recommendations. https://www.aafp.org/family-physician/patient-care/clinical-recommendations/aafp-cps.html
U.S. Census Bureau. (2023, September 28). NSCH Datasets. Census.gov. https://www.census.gov/programs-surveys/nsch/data/datasets.html
U.S. Preventive Services Task Force, Grossman, D. C., Curry, S. J., Owens, D. K., Barry, M. J., Davidson, K. W., Doubeni, C. A., Epling, J. W., Jr, Kemper, A. R., Krist, A. H., Kurth, A. E., Landefeld, C. S., Mangione, C. M., Phipps, M. G., Silverstein, M., Simon, M. A., & Tseng, C. W. (2017). Vision screening in children aged 6 months to 5 years: US Preventive Services Task Force recommendation statement. JAMA, 318(9), 836–844. https://doi.org/10.1001/jama.2017.11260
U.S. Preventive Services Task Force, Loh, A. R., Chiang, M. F., Donahue, S. P., Baker, C. N., Committee on Practice and Ambulatory Medicine, section on Ophthalmology, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology, Child Vision Collaborative, UNMC College of Public Health, Omaha Public Schools, Hospital, C., Center, M., Kerkman, J., & Dingman, H. (2022). VISION SCREENING GUIDE. https://www.education.ne.gov/wp-content/uploads/2023/06/VisionScreeningGuide-2022-21.pdf
Varadaraj, V., Frick, K. D., Saaddine, J. B., Friedman, D. S., & Swenor, B. K. (2019). Trends in eye care use and eyeglasses affordability: The US National Health Interview Survey, 2008-2016. JAMA Ophthalmology, 137(4), 391–398. https://doi.org/10.1001/jamaophthalmol.2018.6799
Varma, R., Tarczy-Hornoch, K., & Jiang, X. (2017). Visual impairment in preschool children in the United States: Demographic and geographic variations from 2015 to 2060. JAMA Ophthalmology, 135(6), 610–616. https://doi.org/10.1001/jamaophthalmol.2017.1021
Vaughan, J. M., Wheeler, D., & Summers, A. (2010) Lay vision screening: Can the Plusoptix vision screener replace the LEA symbol chart and random dot stereotest? Investigative Ophthalmology & Visual Science, 51, 2341. https://iovs.arvojournals.org/article.aspx?articleid=2371008
Vitale, S., Ellwein, L., Cotch, M. F., Ferris, F. L., 3rd, & Sperduto, R. (2008). Prevalence of refractive error in the United States, 1999–2004. Archives of Ophthalmology, 126(8), 1111–1119. https://doi.org/10.1001/archopht.126.8.1111
Vongsachang, H., Friedman, D. S., Inns, A., Kretz, A. M., Mukherjee, M. R., Callan, J., Wahl, M., Repka, M. X., & Collins, M. E. (2020). Parent and Teacher Perspectives on Factors Decreasing Participation in School-Based Vision Programs. Ophthalmic Epidemiology, 27(3), 226–236. https://doi.org/10.1080/09286586.2020.1730910
Wahl, M. D., Fishman, D., Block, S. S., Baldonado, K. N., Friedman, D. S., Repka, M. X., & Collins, M. E. (2021). A comprehensive review of state vision screening mandates for schoolchildren in the United States. Optometry and Vision Science, 98(5), 490–499. https://doi.org/10.1097/OPX.0000000000001686
Wall, T. C., Marsh-Tootle, W., Evans, H. H., Fargason, C. A., Ashworth, C. S., & Hardin, J. M. (2002). Compliance with vision-screening guidelines among a national sample of pediatricians. Ambulatory Pediatrics, 2(6), 449–455. https://doi.org/10.1367/1539-4409(2002)002<0449:CWVSGA>2.0.CO;2
Wallace, D. K., Morse, C. L., Melia, M., Sprunger, D. T., Repka, M. X., Lee, K. A., Christiansen, S. P., & American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. (2018). Pediatric Eye Evaluations Preferred Practice Pattern®: I. Vision screening in the primary care and community setting; II. Comprehensive ophthalmic examination. Ophthalmology, 125(1), P184–P227. https://doi.org/10.1016/j.ophtha.2017.09.032.
Walsh, H. L., Parrish, A., Hucko, L., Sridhar, J., & Cavuoto, K. M. (2023). Access to pediatric ophthalmological care by geographic distribution and US population demographic characteristics in 2022. JAMA Ophthalmology, 141(3), 242–249. https://doi.org/10.1001/jamaophthalmol.2022.6010
Wang, J., Xie, H., Morgan, I., Chen, J., Yao, C., Zhu, J., Zou, H., Liu, K., Xu, X., & He, X. (2022). How to Conduct School Myopia Screening: Comparison Among Myopia Screening Tests and Determination of Associated Cutoffs. Asia Pac J Ophthalmol (Phila), 11(1), 12-18. https://doi.org/10.1097/APO.0000000000000487
Wang, P., Bianchet, S., Carter, M., Hopman, W., & Law, C. (2023). Utilization and barriers to eye care following school-wide pediatric vision screening. Canadian Journal of Ophthalmology, 58(5), 465-471. https://doi.org/10.1016/j.jcjo.2022.04.009
Wang, X., Congdon, N., Ma, Y., Hu, M., Zhou, Y., Liao, W., Jin, L., Xiao, B., Wu, X., Ni, M., Yi, H., Huang, Y., Varga, B., Zhang, H., Cun, Y., Li, X., Yang, L., Liang, C., Huang, W., . . . Ma, X. (2017). Cluster-randomized controlled trial of the effects of free glasses on purchase of children’s glasses in China: The PRICE (Potentiating Rural Investment in Children’s Eyecare) study. PLoS One, 12(11), e0187808. https://doi.org/10.1371/journal.pone.0187808
Williams, M. J., & Eberhardt, J. L. (2008). Biological conceptions of race and the motivation to cross racial boundaries. Journal of Personality and Social Psychology, 94(6), 1033–1047. https://doi.org/10.1037/0022-3514.94.6.1033
Williams, S., Wajda, B. N., Alvi, R., McCauley, C., Martinez-Helfman, S., & Levin, A. V. (2013). The challenges to ophthalmologic follow-up care in at-risk pediatric populations. Journal of AAPOS, 17(2), 140–143.
Williams, S., Wajda, B. N., Alvi, R., McCauley, C., Martinez-Helfman, S., & Levin, A. V. (2013). The challenges to ophthalmologic follow-up care in at-risk pediatric populations. Journal of AAPOS, 17(2), 140-143. doi:10.1016/j.jaapos.2012.11.021
Wolf, E. R., Donahue, E., Sabo, R. T., Nelson, B. B., & Krist, A. H. (2021). Barriers to Attendance of Prenatal and Well-Child Visits. Academic Pediatrics, 21(6), 955-960. doi:10.1016/j.acap.2020.11.025
Wolfenden, L., Kypri, K., Freund, M., & Hodder, R. (2009). Obtaining active parental consent for school-based research: A guide for researchers. Australian and New Zealand Journal of Public Health, 33, 270-5. https://doi.org/10.1111/j.1753-6405.2009.00387.x
Wolffsohn, J. S., Flitcroft, D. I., Gifford, K. L., Jong, M., Jones, L., Klaver, C. C. W., Logan, N. S., Naidoo, K., Resnikoff, S., Sankaridurg, P., Smith, E. L., 3rd, Troilo, D., & Wildsoet, C. F. (2019). IMI - Myopia Control Reports Overview and Introduction. Investigative Ophthalmology & Visual Science, 60(3), M1–M19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6735780/
Woodward, M. A., Hicks, P. M., Harris-Nwanyanwu, K., Modjtahedi, B., Chan, R. V. P., Vogt, E. L., Lu, M. C., Newman-Casey, P. A., & American Academy of Ophthalmology Taskforce on Ophthalmology and Community Health Centers (2024). Eye care in federally qualified health centers. Ophthalmology. https://doi.org/10.1016/j.ophtha.2024.04.019
World Health Organization (WHO). (2007). Global initiative for the elimination of avoidable blindness: Action plan 2006-2011. WHO Press. https://apps.who.int/iris/handle/10665/43754
___. (2019, May 30). Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
___. (2024). Vision and eye screening implementation handbook. WHO Press.
Wu, L., Feng, J., & Zhang, M. (2023). Implementing interventions to promote spectacle wearing among children with refractive errors: A systematic review and meta-analysis. Frontiers in Public Health, 11. https://doi.org/10.3389/fpubh.2023.1053206
Xiao, O., Morgan, I. G., Ellwein, L. B., He, M., & Refractive Error Study in Children Study Group (2015). Prevalence of amblyopia in school-aged children and variations by age, gender, and ethnicity in a multi-country refractive error study. Ophthalmology, 122(9), 1924–1931. https://doi.org/10.1016/j.ophtha.2015.05.034
Yan, X. R., Jiao, W. Z., Li, Z. W., Xu, W. W., Li, F. J., & Wang, L. H. (2015). Performance of the Plusoptix A09 photoscreener in detecting amblyopia risk factors in Chinese children attending an eye clinic. PloS One, 10(6), e0126052. https://doi.org/10.1371/journal.pone.0126052
Yashadhana, A., Fields, T., Blitner, G., Stanley, R., & Zwi, A. B. (2020). Trust, culture and communication: Determinants of eye health and care among Indigenous people with diabetes in Australia. BMJ Global Health, 5(1), e001999. https://doi.org/10.1136/bmjgh-2019-001999
Zadnik, K., Sinnott, L. T., Cotter, S. A., Jones-Jordan, L. A., Kleinstein, R. N., Manny, R. E., Twelker, J. D., Mutti, D. O., & Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group (2015). Prediction of juvenile-onset myopia. JAMA Ophthalmology, 133(6), 683–689. https://doi.org/10.1001/jamaophthalmol.2015.0471
Zhang, X., Elliott, M. N., Saaddine, J. B., Berry, J. G., Cuccaro, P., Tortolero, S., Franklin, F., Barker, L. E., & Schuster, M. A. (2012). Unmet eye care needs among U.S. 5th-grade students. American Journal of Preventive Medicine, 43(1), 55–58. https://doi.org/10.1016/j.amepre.2012.01.032
Zhang, X., Wang, J., Li, Y., & Jiang, B. (2019). Diagnostic test accuracy of Spot and Plusoptix photoscreeners in detecting amblyogenic risk factors in children: A systemic review and meta-analysis. Ophthalmic and Physiological Optics: Journal of the College of Optometrists, 39(4), 260–271. https://doi.org/10.1111/opo.12628
Zhou, Y., Chia, M. A., Wagner, S. K., Ayhan, M. S., Williamson, D. J., Struyven, R. R., Liu, T., Xu, M., Lozano, M. G., Woodward-Court, P., Kihara, Y., Allen, N., Gallacher, J. E. J., Littlejohns, T., Aslam, T., Bishop, P., Black, G., Sergouniotis, P., Atan, D., . . . Keane, P. A. (2023). A foundation model for generalizable disease detection from retinal images. Nature, 622(7981), 156–163. https://doi.org/10.1038/s41586-023-06555-x





































































