Disasters are by their very nature devastating to communities,1 often having significant and long-lasting individual- and population-level effects on physical, mental, and social well-being in communities where health in many cases already is suboptimal. In addition to the tragic loss of human life and devastating health consequences for survivors, disasters often necessitate billions of dollars in public, private, and philanthropic expenditures for recovery assistance. Depending on the nature of the disaster and its impact, these expenditures may support strategic planning and decision making on resource allocation; rebuilding of critical public infrastructure, homes, and businesses; workforce development; provision of health and human services; and restoration of care delivery systems. Given the poor health status characterizing so many American communities and the associated financial and societal costs, the traditional characterization of disaster recovery as a process that restores a community to pre-disaster conditions is shortsighted. This report illustrates how the process of preparing for disasters and the comprehensive array of short- and long-term recovery activities represent a continuum of opportunities that, if exploited thoughtfully, can advance the long-term health, resilience, and sustainability of a community and its residents. Pursuit of this underrealized social goal begins with a vision of a healthy, resilient, and sustainable community and requires a recovery approach that incorporates health considerations into every step of the planning process, informed by an assessment of community health and vulnerability.
STUDY CHARGE AND SCOPE
Disaster recovery is a developing discipline that is creating an experiential-based fund of knowledge with insights into community strategic planning and redevelopment, economic revitalization, and health and human services delivery, among other fields. The collective body of knowledge stemming from these continuously learning laboratories represents an invaluable resource to recovering communities and the local officials who must make difficult decisions in the face of uncertainty, armed only with the best information available. Accordingly, there is a need to make lessons learned from past disasters available to guide
________________
1Community can be defined in multiple ways—for example, as a population of individuals that share a geographic area, a culture, religious beliefs, or self-defined interests. For communities defined by geographic area, the scale varies from the macro (e.g., the national level) to the hyperlocal (the neighborhood or even block level). For the purposes of this report, the term “community” refers to a community of place at the city or county level, unless otherwise indicated.
those decisions and for leaders at all levels to act on them. Recognizing a need for better dissemination of this knowledge and evidence to enable communities to build capacity and to support more informed decision making, the Office of the Assistant Secretary for Preparedness and Response (ASPR) at the U.S. Department of Health and Human Services (HHS), the Office of Lead Hazard Control and Healthy Homes at the U.S. Department of Housing and Urban Development (HUD), the Veterans Health Administration at the Department of Veterans Affairs, and the Robert Wood Johnson Foundation requested that the Institute of Medicine convene the committee that conducted this study. The committee was charged with developing recommendations and guidance on how local and national leaders can mitigate disaster-related health impacts and optimize use of disaster resources—which inevitably must be spent in rebuilding—to pursue more proactively, deliberately, and thoughtfully the goal of creating communities that are healthier and more resilient (see Box S-1).
This report is organized into three parts: Part I sets forth the committee’s strategic framework for building healthier and more resilient and sustainable post-disaster communities, while Part II provides operational-level guidance on sector-specific strategies for achieving this goal. Part III provides the report appendixes. The scope of the report is intentionally broad, with the aim of fostering the integration of health considerations into recovery decision making across a range of disciplines and stakeholder groups. The committee’s recommendations and guidance, therefore, are not specific to any particular disaster scenarios but are meant to be tailored for relevance to local realities and the nature and scale of the incident.
AUDIENCES FOR THIS REPORT
This report is directed at several key audiences that fall into two groups—those individuals and organizations involved in planning for and carrying out disaster recovery activities and those involved in planning for and building healthy communities. Through this report, the committee endeavors to bring these two stakeholder groups together so that a health lens is applied to disaster recovery planning, and the menu of tools and resources for health improvement planners is expanded to include those associated with disaster planning and recovery activities. The constituents of these two groups include
- state, local, tribal, and territorial2 elected and public officials who typically hold leadership roles in emergency management and strategic planning (i.e., governors, mayors, city managers and council members, emergency managers, disaster recovery coordinators);
- state, local, tribal, and territorial public health officials;
- infrastructure support professionals such as those in the fields of urban and regional planning, housing, transportation, and public works;
- federal agency stakeholders;
- health care delivery professionals and organizational leaders;
- social services professionals;
- community support (including faith-based) organizations and nongovernmental organizations;
- schools and education sector leaders;
- private-sector stakeholders; and
- empowered community members.
A FRAMEWORK FOR INTEGRATING HEALTH INTO DISASTER RECOVERY
Disaster recovery is a process of strategic community planning similar to that which takes place in communities throughout the country every day, except for the tremendous challenges of time compression—planning processes that would have occurred over decades are compressed into a relatively brief period of
________________
2Throughout this report, the phrase “state and local” is used for the purposes of brevity but should be inferred to include tribal and territorial leaders.
An ad hoc committee will conduct a study and issue a report on how to improve the short-, intermediate-, and long-term health outcomes and public health impact for individuals in a community of place (as contrasted with communities of faith, identity, etc.). The committee will investigate and identify key activities that impact health and public health outcomes in a community of place recovering from a disaster, and develop recommendations for their implementation. In doing so, the committee will consider the determinants of health and how various activities could leverage those determinants to improve health in the post-disaster setting, including the needs of at-risk populations.
The committee will do this by identifying (based in part on a literature review of domestic and international disasters) and recommending a series of recovery practices and novel programs most likely to impact overall community public health and contribute to resiliency for future incidents in the short-, intermediate-, and long-term period during disaster response and following incident stabilization. Specifically the committee will:
- Examine existing guidance and frameworks, peer-reviewed literature, and case studies from post-disaster response and recovery operations;
- – Characterize and identify key determinants of pre- and post-disaster public health, medical, and social services that may serve as indicators for the affected population’s long-term recovery, from various perspectives amongst the different levels of government and nongovernment actors generally located within a community of place;
- – Ascertain which other sectors are responsible for, or have the organizational interest and capacity for, directly affecting the identified determinants, and identify opportunities for collaborative engagement or support amongst those sectors;
- Identify practical guidance for recovery practices and programs for each sector that will benefit community post-disaster health and public health outcomes in the short-, intermediate-, and long-term.
- – Consider how community needs may be integrated into health recovery efforts.
- – Consider any key determinants, differences, and similarities in recovery between rural and urban communities; among household-income strata; among single-family, low-rise multifamily, and high-rise multifamily housing, among households receiving government assistance and unassisted households, etc.
- – Consider how long-term gains for health may be achieved through investments in community, housing, and other non-traditional health infrastructures.
- Identify areas of research that should be explored to answer key questions about where to direct resources before, during, and after an event occurs.
time. Beginning the process before a disaster and leveraging the products of other steady-state community planning processes (as shown in Figure S-1) can make post-disaster recovery planning more efficient but also ensure that opportunities for community betterment (including health improvement) are not missed.
Unfortunately, the committee found that the model that currently predominates is one whereby the development of community comprehensive plans,3 health improvement plans, hazard mitigation plans, sustainability plans, and disaster recovery plans occurs largely in isolation. The general structure of such planning processes is similar. An initial period of laying the groundwork often is followed by a visioning
________________
3The comprehensive plan, also known as the general plan, is the product of a community’s comprehensive planning process, which is used to determine community goals and aspirations for future community development.
process and an assessment of community status and needs, assets, and contextual factors (e.g., the political environment). The results of these two processes are used to establish goals and set priorities by comparing the findings of the assessment against the community’s vision to identify gaps between the community’s current status and desired state. Strategies are developed to close the gaps through stakeholder (including public) input and analysis of alternatives. These strategies are incorporated into a plan, and implementation partnerships (or operational structures) are developed. Finally, the plan is implemented. Resources are identified and applied, and ideally, progress is continuously measured using preestablished benchmarks. Thus, the process of implementation feeds into a continuous cycle of assessment, planning, and implementation. This strategic planning process offers a framework for integrating health considerations into recovery—each of the steps in the cycle presents opportunities:
Visioning: Recovery is viewed as an opportunity to advance a shared vision of a healthier, more resilient, and sustainable community.
Assessment: Community health assessments and hazard vulnerability assessments provide data that show the gaps between the community’s current status and desired state and inform the development of goals, priorities, and strategies.
Planning: Health considerations are incorporated into recovery decision making across all sectors. This integration is facilitated by involving the health sector in integrated planning activities and by ensuring that decision makers are sensitized to the potential health impacts of all recovery decisions.
Implementation: Recovery resources are used in creative and synergistic ways so that the actions of the health sector maximize health outcomes and the actions of other sectors yield co-benefits for health. A learning process is instituted so that the impacts of recovery activities on health and well-being are continuously evaluated and used to inform iterative decision making.
A HEALTHY, RESILIENT, SUSTAINABLE COMMUNITY RECOVERY VISION
Disasters, although unquestionable tragedies, can provide communities access to previously unavailable resources and opportunities for transformation to advance a vision of a healthier and more resilient and sustainable community. However, leveraging the disaster recovery process to this end necessitates an understanding of the diverse determinants that influence health and healthy communities. It is increasingly understood that health is influenced largely by the locally specific built, natural, and social environments within communities—the social determinants of health, defined by the World Health Organization as “the conditions in which people are born, grow, live, work, and age. These circumstances are shaped by the distribution of money, power, and resources at global, national, and local levels” (WHO, 2014). For the purposes of this report, the committee adopted the following definition of a healthy community proposed by the National Network of Public Health Institutes:
A healthy community is one in which a diverse group of stakeholders collaborate to use their expertise and local knowledge to create a community that is socially and physically conducive to health. Community members are empowered and civically engaged, assuring that all local policies consider health. The community has the capacity to identify, address, and evaluate their own health concerns on an ongoing basis, using data to guide and benchmark efforts. As a result, a healthy community is safe, economically secure, and environmentally sound, as all residents have equal access to high quality educational and employment opportunities, transportation and housing options, prevention and healthcare services, and healthy food and physical activity opportunities. (HRIA, 2013, p. 24)
Emerging from this definition are underlying themes of equity, resilience, and sustainability. Health, equity, resilience, and sustainability are interdependent and mutually reinforcing—part of the same vir-
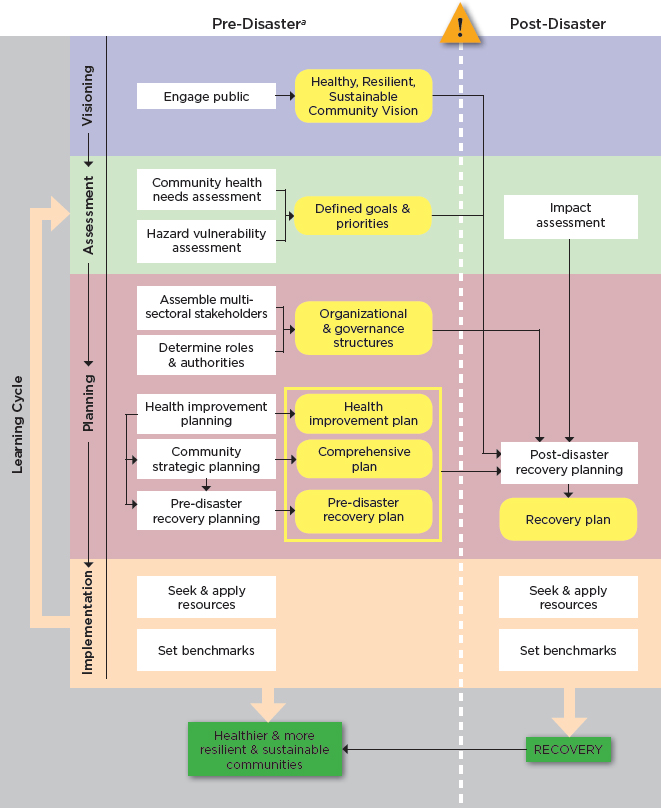
a Although the committee strongly encourages communities to undertake these activities in the pre-disaster period to maximize opportunities for leveraging the post-event recovery process to create healthier and more resilient and sustainable communities, there is still benefit to incorporating them into post-disaster recovery planning if they have not been undertaken beforehand.
tuous cycle. As a result of this interdependence, initiatives that reduce inequities will yield ancillary or co-benefits for population health, as will efforts to strengthen a community’s sustainability or resilience. Conversely, a healthy population is a critical component of sustainable and thriving economic and social systems and a resilient nation. The determinants that contribute to poor health status are largely the same as those associated with social vulnerability. A community with large concentrations of vulnerable populations will be less resilient in the face of social and economic disruption and slower to recover in the event of a disaster. Thus, leveraging the recovery process to improve health and health equity is not only an important social goal and a cost containment measure but also a means of achieving community health resilience—a national strategic priority.
Although there appears to be growing emphasis on the incorporation of resilience-building efforts into the disaster recovery process (spurred in part by the looming threat of climate change), such efforts tend to focus on critical infrastructure instead of people. Unfortunately, the idea of working simultaneously to enhance the health of communities and their residents does not appear to be widespread. The committee noted only a handful of communities taking this forward-looking and synergistic approach.
In the post-disaster period, there is, understandably, intense pressure from the impacted community’s residents to return to a state of normalcy as quickly as possible. As a result, attempts to address deficiencies in pre-event conditions (including health deficiencies and disparities) through post-disaster planning alone will be challenging and may not be successful. Integration of health considerations into the recovery decision-making process for all sectors will depend on a shared vision of a healthy, resilient, and sustainable community. What this means for an individual community needs to be defined as an integral part of community strategic planning processes conducted before an event so that a clear vision is in place to drive post-disaster decision making as new resources become available and opportunities arise. Unfortunately, the committee found that a healthy, resilient, and sustainable community vision rarely guides the development of pre- and post-disaster recovery plans; as a result, a health lens is not applied to recovery decision making, and unique opportunities are missed.
Recommendation 1: Develop a Healthy Community Vision for Disaster Recovery.
The committee recommends that state and local elected and public officials incorporate a vision for a healthy community into community strategic planning and disaster recovery planning.
Implementation of this recommendation will require action at the state and local as well as federal levels. Specifically, at the state and local levels, the following actions should be taken:
- Public health leaders should enhance health improvement planning through engagement with a comprehensive group of community stakeholders (representing each of the audiences for this report, as outlined above) and ensure that plans are based on the community’s needs and assets.
- Elected and public officials, including emergency managers and local disaster recovery managers, should together lead relevant stakeholders in risk-based disaster recovery planning that develops the procedures, processes, and administrative arrangements to be used for integrated, coordinated recovery.
- Elected and public officials, including emergency managers and local disaster recovery managers, should integrate public health officials and health improvement plans into community strategic planning and disaster recovery planning before and after a disaster. To facilitate that integration, the community’s needs and plans for health improvement should be reflected in disaster recovery priorities.
At the federal level, a coordinated, interagency effort is needed to support state and local stakeholders in the development of recovery plans that ensure that communities build back stronger. To this end, the committee believes that aligned grant guidance and technical assistance are essential motivators. Alignment is key to promoting synergy and ensuring that opportunities are not missed. Federal agencies should use
existing grant programs to enhance the capacity of state and local stakeholders to plan for and implement a healthy community perspective in disaster recovery. Specifically, federal agencies should take the following actions:
- HHS, HUD, the U.S. Department of Transportation (DOT), the U.S. Environmental Protection Agency (EPA), and other federal agencies should use aligned grant guidance and technical assistance for existing and future grant programs to incentivize preparedness, community health, and community development grantees to collaborate on the integration of local health improvement goals into comprehensive plans and disaster recovery plans.
- The Centers for Disease Control and Prevention (CDC) and ASPR should revise preparedness grant guidance related to the recovery capability to include greater focus on long-term recovery and opportunities for using recovery to advance healthier and more resilient and sustainable communities.
- The Federal Emergency Management Agency (FEMA) should incentivize emergency management preparedness program grantees to incorporate health considerations into recovery planning by providing grant guidance and technical assistance aligned with HHS guidance.
A HEALTH IN ALL POLICIES APPROACH TO DISASTER RECOVERY
Intentional consideration of health, including health equity, is needed during recovery to mitigate the negative effects of disasters and seize opportunities to advance population health and well-being. Health in All Policies (HiAP) is “an approach to public policies across sectors that systematically takes into account the health implications of decisions, seeks synergies, and avoids harmful health impacts, in order to improve population health and health equity” (WHO, 2013). Motivation for a HiAP approach comes from understanding that health is essential to achieving a strong economy and a vibrant society, but that health outcomes are influenced by social and physical environments shaped by decisions made outside of the health sector. The committee asserts not only that the aftermath of a disaster is a prime opportunity to apply a HiAP approach but also that there is in fact an acute need for such an approach. The health sector acting alone cannot be successful in addressing the complex population health challenges faced by communities, particularly after a disaster. As a result of the failure to apply a HiAP approach more broadly, the health sector, like many others involved in disaster recovery, has tended to act in isolation rather than as part of a coordinated multidisciplinary group. HiAP in the disaster recovery context is about (1) creating organizational structures that optimally enable the coordination of efforts and the creation of synergies where core missions of other sectors align with healthy community objectives, and (2) ensuring that information on the potential health impacts of recovery decisions is available to the decision makers within those structures.
Organizing for an Integrated Approach
The HiAP concept is compatible with the “whole-community” approach to integrated disaster recovery now being promoted by FEMA and others. In a whole-community approach, government, the nonprofit sector, and the private sector work together as partners. Success depends on (1) the development of organizational and governance structures that create efficient and informed networks for decision making, and (2) a robust engagement process that encourages the participation of all community stakeholders (governmental and nongovernmental), including the community’s residents.
Establishing Organizational and Governance Structures
Communities are complex systems in which decision making is distributed and myriad cross-sector interdependencies exist. Organizational structures influence the siloing of related services and functions, which can impede potential synergies and co-benefits. As a result, successful recovery requires a gover-
nance structure that promotes integration across the full range of stakeholder groups, both horizontally and vertically, so that capabilities and resources, both public and private, are leveraged in a coordinated manner to achieve the best outcome for the community as a whole. All communities have structures and processes in place during steady-state periods to support multisector approaches to strategic decision making regarding investments and prioritization. Among these structures and processes are ongoing collaborations inclusive of governmental and nongovernmental organizations that address a community’s health and social service needs. The task for decision makers in the development of recovery governance structures is to ensure that collaborative arrangements operating prior to a disaster are added to the list of organizational assets and incorporated into the recovery planning effort.
The National Disaster Recovery Framework (NDRF), released in 2011, guides the establishment of an overarching multistakeholder coordination structure and may provide a means of integrating existing health-related community collaborations into a recovery governance structure, although optimal arrangements for doing so have not yet been elucidated (FEMA, 2011). Health and social services are represented prominently as one of six Recovery Support Functions (RSFs) defined in the NDRF. However, since the activities of all sectors will impact health during recovery, either positively or negatively, the committee concludes that health impacts need to be considered in disaster recovery decisions related to each of the other RSFs.
Recommendation 2: Integrate Health Considerations into Recovery Decision Making Through the National Disaster Recovery Framework.
The committee recommends that the Federal Emergency Management Agency (FEMA) and the five other federal agencies that represent coordinating agencies for the Recovery Support Functions take steps to further develop and promote the National Disaster Recovery Framework (NDRF) as the basis for a locally defined organizing structure for disaster recovery at the state and local levels to promote information sharing and alignment of funding streams. Further, to ensure that health considerations are integrated into all recovery operations, FEMA, in consultation with the U.S. Department of Health and Human Services (HHS), should update the NDRF to explicitly include health implications for the activities of all Recovery Support Functions.
State and local elected and public officials should establish a steering committee to guide the development of an operational structure that incorporates the organizing principles of the NDRF—including a disaster recovery coordinator and the Recovery Support Functions—and builds on existing collaborative municipal and civic structures, authorities, and initiatives.
Engaging the Whole Community in Recovery Planning
Successful recovery and the post-disaster rebuilding of healthier and more resilient and sustainable communities require the coordinated efforts of a broad multidisciplinary group of stakeholders from health and nonhealth sectors (i.e., a whole-community approach). Yet many of these stakeholders are unaccustomed to working in the emergency management context and unfamiliar with its processes, terminology, and resources. Following a review of the federal grey literature related to recovery and hearing testimony from experts at the federal, state, and local levels, the committee was concerned by how difficult it is for key stakeholders outside of (and even within) the emergency management field to understand the relationships among the array of federal, state, and local resources that must be mobilized after a disaster; how they interrelate; and who is accountable at each level. The committee concludes that the federal government needs to make information on federal recovery resources and the processes by which they are mobilized available in a simplified and more accessible manner to facilitate maximum involvement by all stakeholders. Further, those leading recovery planning need to be sensitized and trained on the importance of engaging all relevant stakeholder groups, including the health and human services sectors, through robust outreach
efforts. Key stakeholders themselves similarly need to be educated on the importance of their participation and mechanisms by which they should engage proactively in the disaster recovery process.
Recommendation 3: Facilitate the Engagement of the Whole Community in Disaster Recovery Through Simplified and Accessible Information and Training.
To facilitate the engagement of the whole community in building healthier communities after disasters, the Federal Emergency Management Agency should lead an interagency effort centered on increasing the accessibility and coherence of information related to disaster recovery and the provision of relevant training.
Priorities should include
- the development of educational materials, including a single overarching federal document that serves as a primer on the recovery process and is easily accessible on the Web regardless of the pathway by which a stakeholder seeks to enter the recovery planning process;
- the development of companion guidance documents for state, local, and nongovernmental stakeholders for each of the Recovery Support Functions, providing more detailed descriptions that facilitate stakeholder understanding of available resources, best practices, and the pathways by which they can engage in the pre- and post-disaster recovery planning processes; and
- the development of coordinated training programs for stakeholders and their professional societies that raise awareness of threats and opportunities related to health and promote broad stakeholder participation in recovery planning under the NDRF.
Training programs should
- sensitize stakeholders to the importance of short-term health protection concerns and long-term opportunities to build healthier communities during recovery, highlighting the critical role of each sector in advancing community health, resilience, and sustainability;
- strengthen connections among emergency management, public health, community development, community planning, human services, and other stakeholder organizations to better prepare them to work together within the structure of the NDRF to increase the chances that recovery resources will be used for creating healthier communities; and
- raise awareness of steady-state community planning processes and administrative structures (partnerships and municipal and civic structures) and mechanisms for leveraging these existing processes and structures by identifying key partnerships and professional resources/sources of technical assistance.
The involvement of informed and empowered community members through an authentic and robust outreach and engagement process is nearly universally recognized as a factor that determines the success of any community planning endeavor, including disaster recovery. Using an inclusive process that leverages existing community organizations and social networks builds trust, creates a sense of ownership, and ensures that recovery decisions align with the community’s vision. After disasters, community planning initiatives that utilize equitable processes and increase interaction among residents also can build social capital—the social ties that are an integral feature of a community—promoting healing, restoring the social fabric of the community, and strengthening resilience. Local governments, by partnering with schools, neighborhood associations, community groups, and private businesses, can help foster the collaborative potential and sense of community ownership that are critical to optimal community health improvement and recovery planning.
Recommendation 4: Enhance and Leverage Social Networks in Community Health Improvement and Recovery Planning.
Local elected and public officials should develop and support programs designed to strengthen social networks and deepen trust among community members before and after disasters, thereby increasing resilience. Strategies for enhancing and preserving social networks should be specifically included in community health improvement and disaster recovery plans. Before and after a disaster, existing social networks, such as neighborhood associations, should be leveraged to enhance mechanisms for integrating the community into recovery planning.
Informing Recovery Decision Making Through Health Information
Organizational structures provide the necessary scaffolding to support decision-making processes but by themselves are not sufficient. The effectiveness of an integrated planning and recovery approach is greatly enhanced by shared information. At the same time that operational structures for recovery are being developed and exercised, pathways for sharing information, including health information, need to be evaluated and delineated. To this end, a pre-disaster investment in infrastructure—and in some cases, data-sharing agreements—is required. Continuous evaluation of health and recovery indicators through a learning system approach enables decision makers to evaluate progress toward a healthy, resilient, and sustainable community vision and adapt future recovery management strategies as needed.
Recommendation 5: Establish Pathways by Which Health Information Can Inform Recovery Decision Making.
State and local elected and public officials should ensure that clear pathways for integration and dissemination of health information are established, including mechanisms that enable concerns and priorities of community members to be transmitted to disaster recovery decision makers. Additionally, a continual feedback process should be established to allow for updating to reflect changes in conditions and measured progress toward recovery. Thus, indicators for measuring progress and success should be (1) developed, (2) incorporated into pre-disaster recovery plans, and (3) updated after a disaster based on its health impact.
Several kinds of information can be used to support the incorporation of health considerations into the recovery decision-making process to improve health outcomes after a disaster. These include (1) knowledge of the potential health impacts of alternatives being considered; (2) historical knowledge from past disaster experiences and, in particular, information on effective (and ineffective) practices; (3) knowledge of available resources; and (4) up-to-date information on health status and human needs. Reliable sources of each of these kinds of information should be identified in advance of a disaster as part of pre-event planning. Sources of such information include
- health impact assessments;
- guidance, training, and technical assistance; and
- health information systems.
Leveraging Recovery Resources to Improve Health, Resilience, and Sustainability
Although a diverse set of resources (federal, state, private, philanthropic) becomes available after a disaster to support the rebuilding of community features and the restoration of services that impact health, these resources often are not mobilized with the conscious goal of advancing a vision of a healthier and more resilient and sustainable community. The committee concludes that communities are missing opportunities during the post-disaster recovery process to maximize the health benefits that can be derived from
the resources applied by nonhealth sectors in the course of achieving their sector-specific goals. Funders need to take steps to ensure that recovery decision makers use financial resources more effectively to achieve such synergies. To this end, it will be necessary to apply a coordinated approach and remove impediments that restrict the flow of funds across vertical hierarchies and their creative use to address multiple priorities simultaneously.
Recommendation 6: Leverage Recovery Resources in a Coordinated Manner to Achieve Healthier Post-Disaster Communities.
Federal agencies (the Federal Emergency Management Agency [FEMA], the U.S. Department of Housing and Urban Development [HUD], the U.S. Department of Health and Human Services [HHS], the U.S. Department of Transportation [DOT], and other federal partners) providing funding for recovery, including pre-event recovery planning, should lead and promote an integrated recovery approach by
- aligning technical requirements and guidance for federal recovery funding opportunities within and across agencies around identified core needs;
- including a requirement and financial incentives for grantees to demonstrate how health considerations will be incorporated into short- and long-term recovery planning conducted using those funds; and
- identifying and removing disincentives that impede the coordination of efforts and the combining of different funding streams to support a healthy community approach to recovery.
Working with private and philanthropic organizations, elected and public officials should ensure that state and local funding regulations and guidelines are consistent with these federal integration efforts.
SECTOR-SPECIFIC STRATEGIES
Part II of this report presents the committee’s recommendations and operational-level guidance for specific sectors, focusing on (1) health and human services strategies to support human recovery—the processes by which the physical and psychological health and social functioning of a community are restored; and (2) place-based recovery strategies that promote and protect health through alteration of a community’s interconnected physical and social environments.
Health and Human Services Strategies
Activities of the health and human services sectors can improve post-disaster health outcomes in a number of ways. Key among these are (1) the delivery of services to meet the public health, medical, behavioral health, and social service needs of disaster survivors; and (2) the collection, assessment, and dissemination of health information to inform decision making during recovery. The three recommendations below represent strategic priorities necessary to support health and human services stakeholders at the state and local levels in carrying out these two key functions.
The best way to ensure that health information is available after a disaster is to ensure that the necessary infrastructure and expertise are in place beforehand. Thus, the threat of disaster provides an additional motivating factor for the establishment of health information technology infrastructure. In the event that such systems are not in place before a disaster, however, the recovery process can be leveraged to advance both infrastructure and plans for its use to ensure continuity of care and ongoing community health improvement after an event. The committee found that current information technology systems do not adequately support post-disaster coordination of health and human services at the individual and community levels.
Recommendation 7: Ensure a Ready Health Information Technology Infrastructure.
State and local governmental officials should ensure the necessary leadership and accountability to support establishment of the interconnected data systems and analytic capacity that are essential to the continuity of health care and social services delivery across the continuum of disaster response and recovery. To this end, coordination of efforts will be required among local and regional public health, health care, health insurance plans, private-sector information technology innovators and vendors, and regulatory and governmental stakeholders at all levels.
At the federal level, the Office of the National Coordinator for Health Information Technology should build on its current efforts and develop a 3-year implementation plan for health information technology integration. This plan should be designed to facilitate data sharing and portability of individual health records across health care settings in support of pre- and post-disaster recovery health care planning and optimal recovery of essential infrastructure for medical and behavioral health care, public health, and social services.
A disaster both increases human needs in a community and, as a result of disruption to the public health, health care, behavioral health, and social services systems that collectively support human recovery, diminishes a community’s capacity to help individual community members and families recover. The committee observed significant gaps, siloing, and fragmentation in the systems needed to support human recovery. Clear, accountable leadership and a national strategy or framework for meeting these human recovery needs are notably lacking.
Recommendation 8: Develop a National Disaster Behavioral Health Policy.
The U.S. Department of Health and Human Services and the Federal Emergency Management Agency should engage state and local governments, as well as private- and nonprofit-sector stakeholders, in the development of a national disaster behavioral health policy. This policy should delineate the roles, responsibilities, and authorities of the federal government for optimal integration of behavioral health services across the continuum of health care, public health, social services, and all other sectors (e.g., housing, public safety, education) before, during, and after a disaster or other emergency.
To support the implementation of this recommendation, the following steps should be taken at the federal level:
- Federal agencies responsible for funding and developing behavioral health policy should support and collaborate with behavioral and other health professional societies to enhance national understanding of the importance of behavioral health to the realization of healthy communities so that this agenda will be included more effectively in general community health planning.
- HHS should use its preparedness funding requirements and currently existing collaborative bodies (e.g., Disaster Behavioral Health Preparedness Forum, Federal Community Health Resilience Coalition), as well as other mechanisms, to overcome the fragmentation of disaster behavioral health services and stimulate their coordination and integration with health care, social support, emergency management, and information technology services.
- HHS should commission a study to analyze current federal behavioral health programs and generate recommendations for efforts at the federal level to address the long-term behavioral health needs of individuals and communities after a disaster or other emergency.
At the state and local levels, the following steps should be taken:
- State and local government disaster preparedness, response, and recovery officials should make the necessary efforts to ensure that behavioral health professionals at all levels are included in disaster preparedness planning and in emergency operations centers after a disaster.
- State and local government public health and mental health officials, supported by federal preparedness funding from the Hospital Preparedness Program (HPP) and Public Health Emergency Preparedness (PHEP) cooperative agreements, should work together and with other key community stakeholders, including state and local emergency managers, to integrate behavioral health into efforts to build community resilience and enhance planning for long-term behavioral health recovery. Opportunities to leverage other funding sources, such as the Substance Abuse Prevention and Treatment Block Grant, Community Mental Health Services Block Grant, and Social Services Block Grant, should be evaluated.
- Given the scale and range of mental health consequences associated with disasters and the need for local capacity to support long-term behavioral health recovery, the adequacy of the behavioral health workforce to meet disaster-related needs should be enhanced. Efforts to this end should include pre-disaster identification of trained professionals; training and exercising of support personnel; attention to licensure and credentialing requirements; and coordination of government mental health care systems, community- and faith-based organizations, and for-profit provider companies.
Recommendation 9: Develop an Integrated Social Services Recovery Framework.
The U.S. Department of Health and Human Services should lead the development of an integrated post-disaster social services framework that more effectively meets human services needs during recovery.
The following steps should be taken to enable the development of the framework:
- ASPR should commission a study to analyze federal programs related to disaster recovery social services and to generate recommendations for decreasing duplication and fragmentation, streamlining processes, and optimally meeting the needs of the affected populations.
- Based on the results of this study, ASPR should work with federal and nonfederal partners—including but not limited to FEMA, HHS (including the Administration for Children and Families, the Substance Abuse and Mental Health Services Administration, and the Health Resources and Services Administration), HUD, the U.S. Department of Agriculture, the U.S. Department of Education, the U.S. Department of Veterans Affairs, the American Red Cross, and other appropriate nongovernmental organizations—to create a framework linking current and future funding sources, policies, and regulations to the recommended strategies for optimizing social services after disasters.
- The multiple federal agencies and nongovernmental organizations that provide day-to-day funding for human services and funding to support social services during recovery (including those agencies cited above) should condition funding on the creation by each state or municipality (in cases where large municipalities receive funding directly) of an integrated strategy for social services delivery. This strategy should be designed to facilitate the accessibility of these services through such means as collocation of services and data portability for disaster survivors.
- Departments responsible for human/social services within states and municipalities should serve as the coordinators for operationalizing the above strategy and for coordinating faith-based and other nongovernmental organizations as well as related state agencies that are implementing the post-disaster social services framework.
Place-Based Recovery Strategies
Disasters often necessitate significant efforts to restore the physical infrastructure of a community, including repair of roads and bridges, reconstruction of housing and other buildings, repair of public works, and restoration of natural resources. Rather than rebuilding to a prior state, the recovery process offers a unique opportunity to mitigate against future hazards and create environments intentionally designed to support health through healthier housing and community features that enhance active lifestyles and improve equitable access to critical goods (e.g., healthy food), community services (e.g., medical care), and amenities (e.g., libraries, schools, recreational/physical fitness facilities). A well-planned recovery also attends to the economic vitality of the affected area, seeking commercial revitalization, industrial and business development, and greater employment opportunities, thereby improving financial prospects for both residents and businesses. To ensure that these opportunities are not missed, professionals from diverse fields, including planning and design, housing, community development, environmental management, and public health, need to be engaged in the development of pre- and post-disaster recovery strategies, which should tie back to community plans to improve health and social well-being developed in advance of a disaster. Communities that have plans in hand when a disaster strikes are equipped to transition to recovery more quickly with a long-term objective of health, resilience, and sustainability. Given that the pool of resources for recovery is limited, creative uses of funds that meet multiple objectives simultaneously can improve the efficiency of recovery and the opportunities to integrate health considerations. Such opportunities deserve special attention in disaster recovery plans.
Recommendation 10: Design for Healthy Post-Disaster Communities.
State and federal agencies (the Federal Emergency Management Agency, the U.S. Department of Transportation, the U.S. Department of Housing and Urban Development, the U.S. Environmental Protection Agency, the U.S. Department of Health and Human Services, and others), acting alone or as components of the federal Partnership for Sustainable Communities, should ensure through funding requirements that the use of federal community development and disaster recovery and preparedness funds optimizes the built environment in support of healthy communities by creating places that protect against health threats, promote good health, and address unmet social needs.
Local and state planning entities should develop a team-based approach to integrated recovery planning aligned with the policies and processes of the Partnership for Sustainable Communities so as to maximize efficiency in the use of federal resources to enhance smart growth, equity, hazard mitigation, resilience, sustainability, and other elements necessary to the creation of healthy communities. Priority areas for funding should specifically address the following essential health-enhancing requirements that are pertinent to the community’s needs as laid out in pre- and post-disaster health improvement and comprehensive plans:
- physical activity-enhancing infrastructure that includes trails, bike paths, sidewalks, and parks and recreational spaces, as well as walkable, mixed-use neighborhood designs; and
- comprehensive transportation infrastructure and land use policies that ensure the accessibility of healthy food retail outlets, employment, health and social services, schools, and community amenities such as libraries and community centers for all residents.
Optimal health, social well-being, and safety are dependent on avoiding or reducing the impacts of disasters by using best practices of hazard mitigation, including both structural and nonstructural (e.g., zoning and land use) standards and strategies. Forward-looking strategic plans, improved infrastructure, and stronger construction codes need to be used in combination to address identified community vulner-
abilities, thereby reversing the nation’s trend toward higher disaster losses and the attendant human misery and social and economic costs, as well as preparing the nation for the potential effects of climate change.
Recommendation 11: Mitigate Against Future Health Hazards.
Building on the National Mitigation Framework, federal agencies, led by the Federal Emergency Management Agency, should immediately intensify their efforts, undertaken collectively and supported by aligned funding eligibility requirements, to ensure that all critical infrastructure and facilities—such as hospitals (public and private), nursing homes, fire stations, and public utilities—constructed after a disaster are designed and built with a level of protection that better ensures post-disaster safety and functionality essential to protecting health and recovering more quickly. When feasible, they should be located outside of known hazard zones. Additionally, requirements should ensure that existing critical infrastructure and facilities restored with federal recovery funds are upgraded to the new standards.
Housing meets some of people’s most basic needs (shelter from the elements, privacy, a place of respite, and socialization). Disasters can compromise living conditions, making rapid and appropriate provision of housing after a disaster essential for health and well-being. However, it is also critical to ensure that the urgency of post-disaster housing reconstruction does not give rise to practices that compromise health and preclude opportunities to promote long-term housing affordability, resiliency, and sustainability.
Recommendation 12: Ensure Healthy and Affordable Post-Disaster Housing.
To reduce housing-related health risks, federal, state, and local governmental housing agencies should require that new residential construction and substantial rehabilitation of existing residences financed with public funds after disasters comply fully with Enterprise Green Communities standards or their equivalent and with the minimum requirements set forth in the National Healthy Housing Standard. Federal and state funding agencies should tie these requirements to recovery funds, and private funders should consider incentivizing compliance with these standards. Additionally, multiple affordable housing options should be considered during redevelopment to ensure that people of all income levels can remain in the community.
CONCLUSION
The committee’s recommendations are designed to provide practical strategies to assist disaster-impacted communities in making key decisions relevant to realizing a healthy, resilient, and sustainable community vision. These recommendations call for multiple and coordinated actions at a variety of levels by a wide range of governmental and nongovernmental actors. Box S-2 provides key recovery strategies for each sector that, if implemented, would support the implementation of the committee’s recommendations. Given the broad scope and complexity of the subject matter, it is expected that this initial product will prompt further work, providing the opportunity for deeper analysis and elucidation of the influences and relationships that will advance the nation’s sophistication in the process of disaster recovery, one critical aspect of which is health.
Table S-1 shows those stakeholders whose coordinated actions are needed to lead the implementation of each of the committee’s recommendations. If acted upon in a coordinated and comprehensive manner, these recommendations will enable all stakeholders involved in the pre-disaster and immediate- and long-term post-disaster strategic planning processes to be engaged, empowered, and supported in maximizing the opportunities to transform an unfortunate crisis into long-term benefit in the form of healthier communities and individuals.
BOX S-2
Summary of Key Health Recovery Strategies by Sector
PUBLIC HEALTH SECTOR
- Leverage existing relationships and networks (e.g., coalitions, collaboratives) to integrate public health and other community partners into recovery planning.
- Identify opportunities for alignment between ongoing public health improvement processes (e.g., accreditation prerequisites of community health assessments and community health improvement plans) and recovery planning.
- Educate nonhealth sectors and the community on why health is integral to recovery and how recovery activities impact health outcomes.
- Use and expand health technology infrastructure for data collection and analysis to facilitate data sharing, evidence-based decision making, and continual evaluation of progress toward an optimally healthy community.
HEALTH CARE SECTOR
- Use multidisciplinary team-based care strategies to meet multifaceted health care needs.
- Ensure continuity of access to health care services.
- Use health information technology to drive decision making for individual and community health and to inform future planning.
- Leverage health care coalitions and other relationships with local care providers for strategic decision making on health care services and alignment of clinical resources.
BEHAVIORAL HEALTH SECTOR
- Integrate behavioral health activities and programming into other sectors (e.g., education, health care, social services) to reduce stand-alone services, reach more people, foster resilience and sustainability, and reduce stigma.
- Provide a spectrum of behavioral health services and use an approach based on stepped care (from supportive intervention to long-term treatment).
- Maximize the participation of the local affected population in recovery planning with respect to behavioral health, and identify and build on available resources and local capacities and networks (community, families, schools, and friends) in developing recovery strategies.
- Promote a sense of safety, connectedness, calming, hope, and efficacy at the individual, family, and community levels.
REFERENCES
FEMA (Federal Emergency Management Agency). 2011. National disaster recovery framework. Washington, DC: FEMA.
HRIA (Health Resources in Action). 2013. Defining healthy communities. http://hria.org/uploads/catalogerfiles/defining-healthy-communities/defining_healthy_communities_1113_final_report.pdf (accessed October 21, 2014).
SOCIAL SERVICES SECTOR
- Build on existing relationships and establish comprehensive plans for collaboration among social services funders and providers, nongovernmental and faith-based organizations, and advocates to ensure coordinated social services delivery through all phases of disaster planning and recovery.
- Integrate social services recovery plans into other disaster recovery services.
- Create compatible structures, policies, and procedures to promote the flow of funding and information across federal, state, and local systems.
- Provide support to reunite families and promote resilience through community programming designed to strengthen social support networks.
- Focus on restoring normalcy through key community services/activities, such as child care, elder care, foster care, behavioral health services, schools, housing, jobs, and transportation.
- Enhance efforts to increase accessibility and reach the most vulnerable populations to provide needed social services.
- Promote ongoing evaluation and continuous learning to advance social services efforts in achieving health community goals.
URBAN AND REGIONAL PLANNING, TRANSPORTATION, ENVIRONMENTAL MANAGEMENT, AND COMMUNITY DEVELOPMENT SECTORS
- Reduce health disparities and improve access to essential goods, services, and opportunities.
- Preserve and promote social connectedness.
- Use a systems approach to community redevelopment that acknowledges the connection among social, cultural, economic, and physical environments.
- Seek holistic solutions to socioeconomic disparities and their perverse effects on population health through place-based interventions.
- Rebuild for sustainability and resilience.
- Capitalize on existing planning networks to strengthen recovery planning, including attention to public health, medical, and social services, especially for vulnerable populations.
HOUSING SECTOR
- Protect survivors and recovery workers from health hazards associated with unhealthy or unsafe housing.
- Preserve and promote social connectedness in plans for immediate response, short-term housing, and long-term rebuilding.
- Consider needs for access to health and social services during all phases of housing recovery.
- Incentivize the use of healthy and/or green criteria for the rebuilding of homes, buildings, and neighborhoods.
- Engage community members, including representatives of and advocates for vulnerable populations, in the development of post-disaster housing plans to ensure that the needs of all community members are met.
WHO (World Health Organization). 2013. Health in All Policies. http://www.healthpromotion2013.org/healthpromotion/health-in-all-policies (accessed December 4, 2014).
WHO. 2014. Social determinants of health. http://www.who.int/social_determinants/en (accessed October 30, 2014).
TABLE S-1 Key Stakeholders Involved in Leading the Implementation of the Committee’s Recommendations
| Key Stakeholders | |||||||||
| Committee Recommendation | Federal Gov. |
State Gov. |
Local Gov. |
Nonprofit/ Faith-based |
Private Sector |
Community Members |
|||
| 1 | Develop a Healthy Community Vision for Disaster Recovery | ✓ MULTa |
✓ | ✓ | ✓ | ✓ | ✓ | ||
| 2 | Integrate Health Considerations into Recovery Decision Making Through the National Disaster Recovery Framework | ✓ DHS (FEMA)/HHS |
✓ | ✓ | |||||
| 3 | Facilitate the Engagement of the Whole Community in Disaster Recovery Through Simplified and Accessible Information and Training | DHS (FEMA) |
|||||||
| 4 | Enhance and Leverage Social Networks in Community Health Improvement and Recovery Planning | ✓ | ✓ | ✓ | |||||
| 5 | Establish Pathways by Which Health Information Can Inform Recovery Decision Making | ✓ | ✓ | ||||||
| 6 | Leverage Recovery Resources in a Coordinated Manner to Achieve Healthier Post-Disaster Communities | ✓ MULT |
✓ | ✓ | ✓ | ✓ | |||
| 7 | Ensure a Ready Health Information Technology Infrastructure | ✓ HHS |
✓ | ✓ | ✓ | ||||
| 8 | Develop a National Disaster Behavioral Health Policy | ✓ DHS (FEMA)/HHS |
✓ | ✓ | ✓ | ✓ | |||
| 9 | Develop an Integrated Social Services Recovery Framework | ✓ HHS |
✓ | ✓ | ✓ | ||||
| 10 | Design for Healthy Post-Disaster Communities | ✓ MULT |
✓ | ✓ | ✓ | ✓ | |||
| 11 | Mitigate Against Future Health Hazards | ✓ DHS (FEMA) |
✓ | ✓ | ✓ | ||||
| 12 | Ensure Healthy and Affordable Post-Disaster Housing | ✓ HUD |
✓ | ✓ | ✓ | ✓ | |||
a MULT = Indicates multiple federal agencies will need to work cooperatively to implement the recommendation. Depending on the recommendation, these may include but are not limited to the Federal Emergency Management Agency (FEMA) at the U.S. Department of Homeland Security (DHS), the U.S. Department of Health and Human Services (HHS), the U.S. Department of Housing and Urban Development (HUD), the U.S. Department of Transportation (DOT), the U.S. Environmental Protection Agency (EPA), the U.S. Department of Agriculture (USDA), the U.S. Department of the Interior, the U.S. Department of Commerce, the U.S. Department of Education, and the U.S. Department of Veterans Affairs (VA).
Gov. = Government.

















