Translating Knowledge of Foundational Drivers of Obesity into Practice: Proceedings of a Workshop Series (2023)
Chapter: 10 The Science, Strengths, and Limitations of Body Mass Index
10
The Science, Strengths, and Limitations of Body Mass Index
The third (October 2022) workshop began with an introductory, stage-setting session.
THE SCIENCE, STRENGTHS, AND LIMITATIONS OF BODY MASS INDEX AS A MEASURE OF OBESITY
William (Bill) Dietz, chair of the Sumner M. Redstone Global Center on Prevention and Wellness in the Milken Institute School of Public Health at The George Washington University, discussed the science, strengths, and limitations of body mass index (BMI) as a measure of obesity. The core of deliberations and disputes about BMI’s utility, Dietz proposed, is the question of how to assess the health impact of body fat.
Dietz began by listing various methods used to determine body composition, which can be divided into measures of total body fat and measures of fat distribution. He stated that most measures of total body fat are not clinical measures. They include densitometry approaches, such as underwater weighing and body plethysmography (i.e., air displacement in a vessel called the Bod Pod); isotope dilution of deuterium oxide to determine the body water space and convert the figure to lean tissue by multiplying by 0.73; dual x-ray absorptiometry (DEXA); and bioimpedance, which in Dietz’s view is a relatively crude measure that does not offer much value beyond that offered by BMI.
Body fat distribution is a key indicator of obesity-associated risk, Dietz explained, as he turned to listing measures of this indicator: waist circumference, waist:hip ratio, DEXA, and computed tomography (CT) scans. He noted that a waist circumference greater than 40 inches for men and 35 inches for women indicates abdominal obesity and increased risk for a variety of adverse health outcomes. Waist:hip ratio has been used in the past, Dietz observed, with measures greater than 1.0 for men and 0.8 for women being deemed high risk. Because waist:hip ratio is governed largely by abdominal circumference, he elaborated, it is unusual to observe a waist:hip ratio of less than 1.0 in people with severe obesity when body fat is present in both the abdominal and gynoid (below the hips) regions. He flagged gynoid obesity as a subset of obesity that is not well defined, wherein the hip measurement is markedly increased but the waist measurement is not, resulting in a ratio below 0.8 despite the presence of excess body fat. CT scans and magnetic resonance imaging provide the most accurate measure of fat distribution, Dietz continued, and can distinguish visceral from subcutaneous abdominal fat. DEXA cannot make this differentiation, he said, but is useful for measuring total body fat and abdominal fat. Those two fat deposits, he added, as well as the fat deposit around the buttocks, have multiple differences in physiologic function.
Dietz next shared four points to support his rationale for why BMI is a reasonable measure for assessment of obesity in children and adolescents. His first point was that BMI reflects the presence of increased body fat. At BMI ≥95th percentile, 75 percent of youth have increased body fat (defined as ≥85th percentile of total body fat as determined by DEXA); a smaller

NOTE: Data from 875 participants in Project Viva. BMI percentiles based on Centers for Disease Control and Prevention (CDC) growth charts.
SOURCE: Presented by William H. Dietz, October 25, 2022. Boeke et al. (2013). Reprinted with permission.
percentage of youth in the 85th–95th percentiles have increased body fat (using the same definition). Thus, Dietz concluded, BMI is a reasonable measure of body fat in children and adolescents.
To support this point, Dietz presented a figure showing the findings of one study with respect to age- and sex-specific BMI percentiles in relation to DEXA fat mass in children of various races/ethnicities aged 6.5–10.9 (Figure 10-1) (Boeke et al., 2013). Correlation is low at BMI percentiles 0 through 80, he explained, and begins to rise around the 85th percentile before increasing linearly. This pattern indicates that BMI is a suboptimal measure of body fat for the population overall but is a reasonable measure for individuals with BMI ≥85th percentile.
Dietz remarked that BMI is a simple calculation of weight (kilograms) divided by height (meters) squared. Its measurement is easy, he pointed out, because it is not hindered by clothing or dependent on specialized equipment. In another assessment involving the same study cohort, Dietz reported, correlations of three anthropometric measures (sum of skinfolds, waist circumference, and bioimpedance) with body fat as measured by DEXA were comparable to those indicated by BMI (Boeke et al., 2013).
A second point to support the use of BMI in children and adolescents, Dietz continued, is that BMI >95th percentile increases disease risk. For instance, the long-running Bogalusa Heart Study found that among children in its cohort with BMI ≥95th percentile, 70 percent had one risk factor for cardiovascular disease, and 39 percent had two or more (Freedman et al., 2007).
Dietz’s third point was that increased BMI is associated with risk of persistent obesity. That risk increases with age and the severity of obesity (Geserick et al., 2018).
Finally, Dietz remarked that BMI in children and adolescents corresponds to BMI in adults. For example, a BMI in the 95th percentile in late adolescence corresponds to a BMI of 30 in adults, and BMI in the 82nd or 83rd percentile corresponds to a BMI of 25 in adults.
Dietz next discussed the rationale for using BMI in adults. As with the data for children and adolescents, he observed, BMI does not correlate with body fat in the 0–30 BMI category, but a reasonable correlation (~0.70) exists for BMI and body fat above BMI of 30 (Flegal et al., 2009). Adult weight increases proportionally to height squared (i.e., it is not a linear function of height). Dietz explained that this is why the BMI calculation is weight (kg)/height (m)2, which helps make BMI a stature-independent measure of weight. BMI is applicable across most ethnicities and throughout the life cycle, Dietz elaborated, although correlations between total body fat and BMI may differ by sex and ethnicity. Lastly, Dietz pointed out that the lowest mortality across the distribution of BMI has been used to define a “healthy” weight; the term “normal” weight is no longer used because there is no normal weight distribution.
Dietz turned to describing “what BMI is not.” BMI is associated with body fat, he reiterated, but is not a direct measure of body fat. It also does not assess the concomitant presence of comorbid conditions, disease risks, or functionality. BMI’s association with health risk is inconsistent and varies with age, sex, and ethnicity, and BMI does not assess risk related to body fat distribution. Finally, Dietz emphasized that BMI is not a diagnostic measure of obesity.
As an example of a situation in which BMI is less useful, Dietz showed a bar graph comparing the prevalence of obesity among non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic men and women (Figure 10-2). The prevalence of obesity among Non-Hispanic Asian adults, he pointed out, is consistently low in such comparisons based on BMI.
One explanation for this, he said, is that at a given BMI, Asian populations have a higher risk of diseases associated with obesity compared with non-Asian populations at the same BMI. A study critical to informing BMI cutpoints for Asian populations determined the BMI in seven different Asian populations that corresponded to a total body fat of 25 percent and 30 percent (based on DEXA) (WHO Expert Consultation, 2004). For the overweight category, which by U.S. standards is a BMI of 25 corresponding to a total body fat of 25 percent, Asian populations with the same percentage of body fat had a BMI of 23. The same relationship held for obesity, Dietz reported, which is defined in the United States as BMI ≥30, but for Asian populations, as BMI ≥27.5. It would be helpful to see this adjustment
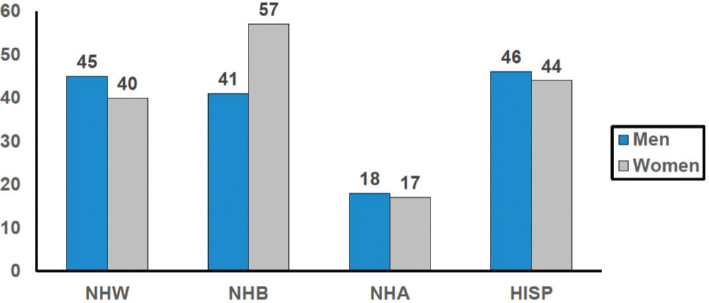
SOURCE: Presented by William H. Dietz, October 25, 2022. Hales et al. (2020). Reprinted with permission.
made in National Health and Nutrition Examination Survey data, he remarked, which would show how the use of an Asian-specific standard would affect the prevalence of obesity in Asian populations.
Dietz moved on to report the results of a 2004 study comparing waist circumference with BMI with respect to the risk of metabolic syndrome among approximately 15,000 men and women with BMIs between 18.5 and 35 (Janssen et al., 2004). Prior to adjustment for waist circumference in men and women (i.e., based on BMI alone), he explained, the odds ratio for metabolic syndrome increased significantly with higher BMI. The increased odds ratio held true when BMI was adjusted for waist circumference category (elevated or not elevated) but disappeared when BMI was adjusted for absolute waist circumference.
Dietz transitioned to discussing the Edmonton Obesity Staging System (EOSS) (Figure 10-3), which represents a shift in how obesity’s comorbidities are assessed. EOSS Stage 0 represents zero medical, mental, or functional clinical risk factors. Stage 1 represents subclinical obesity-related risk factors in those three areas, such as elevated blood pressure, impaired fasting glucose, elevated liver enzymes, and mild functional limitations. Stage 2 represents established diseases such as sleep apnea, hypertension, diabetes, nonalcoholic fatty liver disease, and polycystic ovary disease. Stage 3 represents severe disease, such as heart attack or diabetes complications. Finally, stage 4 represents end-stage disease, such as liver failure or the need for dialysis in renal failure.
Dietz pointed out that the distribution of Class I (BMI 30.0–34.9), Class II (BMI 35.0–39.9), and Class III (BMI ≥40.0) obesity is relatively

SOURCE: Presented by William H. Dietz, October 25, 2022. Swaleh et al. (2021). Reprinted with permission.
even throughout the EOSS (Figure 10-4), although the EOSS and BMI measure different things. BMI can still be used for screening, he clarified, but EOSS staging points to the comorbidities of obesity. In his view, a challenge with the EOSS is that all complications have equal weight despite differences among them in risk of severe disease, risk of mortality, and costs. Another challenge, he said, is that assignment to Stage 2 requires only one abnormal finding, but the presence of two or more abnormal findings does not change the EOSS’s assessed risk for that stage.
Next, Dietz described the contribution of adipose tissue to the pathophysiology of obesity. He reiterated that visceral fat—the deposition of body fat intra-abdominally and distributed throughout organs—is a key risk factor for disease. He explained that as obesity develops, adipocytes (i.e., fat cells) multiply and increase in size within visceral adipose tissue, changes that are associated with increased inflammation. Visceral adipose tissue releases inflammatory mediators, which adversely affect both pancreatic and liver function, resulting in decreased insulin secretion and increased insulin resistance, respectively. Muscle is also negatively affected by the inflammatory mediators released from visceral adipose tissue, Dietz added, which impairs glucose uptake and contributes to insulin resistance. An easy measure of visceral fat does not yet exist, he observed, nor does an easy measure with which to examine the degree to which the intermediary factors released by adipocytes contribute to disease.

NOTE: BMI = body mass index.
SOURCE: Presented by William H. Dietz, October 25, 2022. Swaleh et al. (2021). Reprinted with permission.
Finally, Dietz shared a consensus statement of six obesity groups—the Academy of Nutrition and Dietetics, the STOP Obesity Alliance, The Obesity Society, the Obesity Medicine Association, the American Society for Metabolic and Bariatric Surgery, and the Obesity Action Coalition—to ensure consistency of messaging about the disease of obesity.1 Key points from this statement include the following:
- Obesity is a highly prevalent chronic disease characterized by excessive fat accumulation or distribution that presents a risk to health and requires lifelong care. Virtually every system in the body is affected by obesity. Other major chronic diseases associated with obesity include diabetes, heart disease, and cancer.
- BMI is used to screen for obesity, but it does not displace clinical judgment. BMI is not a measure of body fat. Social determinants, race, ethnicity, and age may modify the risk associated with a given BMI.
- Bias and stigmatization directed at people with obesity contributes to poor health and impairs treatment.
- Every person with obesity should have access to evidence-based treatment.
___________________
1 The consensus statement is viewable at https://stop.publichealth.gwu.edu/obesity-statement#:~:text=Obesity%20is%20a%20highly%20prevalent,%2C%20heart%20disease%2C%20and%20cancer (accessed January 5, 2023).
In closing, Dietz observed that much discussion is occurring, particularly among “fat acceptance groups” and people with larger bodies, about how to use the term “obesity” and whether the term itself is stigmatizing. He raised doubt that the field can avoid naming obesity from a medical perspective given the large body of technical support for the diagnosis, but if it is indeed a stigmatizing term, asked, “How do we talk about obesity if we can’t talk about obesity?”
DISCUSSION
Following Dietz’s presentation, Ihuoma Eneli, professor of clinical pediatrics at The Ohio State University College of Medicine and associate director of the American Academy of Pediatrics Institute for Healthy Childhood Weight, moderated the discussion. She posed two questions: one about the Centers for Disease Control and Prevention’s (CDC’s) maps that visualize the U.S. prevalence of obesity by state, and another about advice for new physicians counseling patients with obesity.
U.S. State Maps of Prevalence of Obesity
Eneli referenced the CDC’s popular maps illustrating the prevalence of obesity in each U.S. state and asked Dietz for his prediction as to whether these maps will still be in use 5 years from now. Dietz responded that the maps have effectively illustrated the spread of obesity in the United States and have seen widespread use since their development in 1999. He shared his view that the maps are still compelling, and that using BMI to create the maps remains the best tool currently available for assessing the proliferation of obesity across the United States.
Guidance for New Physicians about Discussing BMI with Patients with Obesity
Dietz urged avoidance of the term “obesity” given evidence that patients regard it as pejorative and would rather talk about “elevated BMI” or “excess weight.” He also suggested that a provider might not need to share a patient’s BMI with the patient, and instead could use the BMI as an indication for how to proceed. He encouraged new physicians to be sensitive to the location where weight is measured (i.e., a private space is best) and how weight is shared with both patient and provider so as not to add to the stigma experienced by people with obesity. He recounted his experience treating patients and shared that a helpful way to begin the conversation is to ask patients whether they are concerned about their weight. He urged the next generation of physicians and trainees to make shared decision making a cornerstone of care, which he noted requires that patients trust and be willing to engage with their providers.







