Exploring the Science on Measures of Body Composition, Body Fat Distribution, and Obesity: Proceedings of a Workshop Series (2024)
Chapter: 4 Applications and Uses of BMI, Body Composition, and Body Fat Distribution
4
Applications and Uses of BMI, Body Composition, and Body Fat Distribution
The third session sharpened the focus on body mass index (BMI), body composition, and body fat for a more detailed examination of their application to determine obesity and health risks. W. Scott Butsch, the director of obesity medicine at the Bariatric and Metabolic Institute at the Cleveland Clinic, led the session, which had four presentations on the biology of fat and lean body mass, alternative measures to BMI and the financial implications in health care, using BMI in occupational health and safety research, and the lived experience of a person living with obesity. Butsch then moderated a panel discussion with questions from the audience.
ADIPOSE TISSUE, BMI, AND FAT DISTRIBUTION
Michael Jensen, Tomas J. Watson, Jr. Professorship in Honor of Dr. Robert L. Frye at the Mayo College of Medicine and consultant in the Division of Endocrinology and Metabolism, asked the audience to consider if BMI is a surrogate for body fat and why the amount and distribution of fat matter. To answer, Jensen gave a brief lesson in biology on the differences between lean body mass and adipose tissue.
Jensen explained that BMI and body fat are correlated, but body fat percentage varies considerably in any given range of BMI. To illustrate, he referenced his unpublished study of adults with a BMI of 20–25 kg/m2, which showed that women who were metabolically healthy had double the body fat percentage (~30 percent) of men. In the same study, men with a BMI of 30–35 kg/m2 also had about 30 percent body fat but were metabolically unhealthy.
Jensen provided an overview of the role of adipose tissue or body fat in processing dietary fat. Its chief function is to store enough energy for about 2–3 months. After a meal, dietary fat is broken down into triglycerides that circulate through the bloodstream and are removed and stored as body fat. Fat cells produce storage proteins to remove triglycerides from the bloodstream. Body fat or adipose tissue releases the fatty acids into the bloodstream as an energy source for other tissues. Otherwise, dietary fat and triglycerides would build up in the bloodstream, leading to poor metabolic health.
Jensen emphasized that fat metabolism is tightly regulated. When someone is not eating, fat tissue releases 1 teaspoon of fatty acids per minute into the bloodstream, circulating to other body tissues for energy. However, when adipose tissue is not functioning normally, that release is 1.4 teaspoons per minute, leading to an increased risk for hyperlipidemia and diabetes.
A predictor of poor metabolic health is the location of fat distribution in the body, Jensen continued. Visceral fat (in the abdomen) is strongly associated with adverse metabolic consequences (e.g., diabetes, hyperlipidemia), whereas subcutaneous fat (under the skin) is not. Jensen described his research that found a positive relationship between BMI and visceral fat in men and women, although women in any BMI range had less visceral fat. BMI was somewhat predictive of visceral fat, and visceral fat was somewhat predictive of poor metabolic health. However, Jensen shared that his research showed the size of fat cells is more predictive of fat cell dysfunction. Jensen’s study indicated that small fat cells efficiently generated fat storage proteins for triglyceride uptake and rapidly regulated the release of fatty acids. By contrast, large fat cells were dysfunctional within any range of BMI, produced fewer fat storage proteins, and were less efficient at removing triglycerides from the blood.
Returning to BMI as a measure, Jensen stated that despite the positive relationship with fat cell size it is not reliable. Some people with a BMI within a normal range have large fat cells, whereas others with a BMI in the overweight range have small fat cells. To summarize, he said, the smaller the fat cells, the greater efficiency in fat tissue.
Jensen stated that visceral or abdominal fat is considered a predictor of fat cell size. His research found that people with less visceral fat, measured by (smaller) waist circumference, had smaller fat cells. The greater the waist circumference, the more visceral fat, and the greater the likelihood of large fat cells, he said.
Jensen concluded that independent of BMI, centralized fat distribution in the abdomen predicted larger fat cells, which appear most likely to cause metabolic abnormalities or dysfunction. Fat cell dysfunction predicted metabolic consequences (e.g., diabetes and hyperlipidemia). Furthermore, the evidence suggests that fasting hypertriglyceridemia could be an early sign of fat
cell dysfunction in energy metabolism and its ability to take up triglycerides from the bloodstream after a meal and release fatty acids.
A HEALTH SYSTEM AND HEALTH SERVICES RESEARCH PERSPECTIVE ON THE USE OF BMI TO DIAGNOSE AND TREAT OBESITY
David Arterburn, senior investigator at the Kaiser Permanente Washington Health Research Institute and affiliate professor in the Department of Medicine at the University of Washington, was the second speaker; he discussed the practical implications to finance and deliver health care using BMI as a quality measure and the cost implications for alternatives.
Arterburn began by providing some context for BMI in health care. He introduced the National Committee for Quality Assurance (NCQA), which created the Adult BMI Assessment as a performance measure of U.S. adults that had an outpatient visit and who had their BMI documented (NCQA, 2023). In 2009, BMI was documented in 40 percent of health insurance plans and outpatient visitors’ health records, and by 2019, that was over 80 percent of outpatient visits. However, in 2020, NCQA discontinued this because the electronic health record (EHR) automatically calculated BMI, and its performance was not measured alongside lifestyle counseling or other interventions.
Arterburn noted that in 2009, a BMI percentile measure was released for overweight and obesity in children and adolescents. One-third of children’s EHRs included a BMI percentile, which jumped to over two-thirds of EHRs from 2009 to 2021, a considerable increase, he said.
As a standard measure in EHRs, BMI directs insurance coverage for obesity interventions, so Arterburn identified financial implications in health care. He pointed to a study of a nationally representative sample of adults from 2011 to 2016 (Ward et al., 2021). The results showed that a BMI of 18.5–24.9 kg/m2 was associated with the lowest estimated expenditures and total health care costs and that costs increased for men and women with a BMI ≥35 kg/m2. Furthermore, across BMI categories, women had slightly higher costs than men (see Figure 4-1).
In the same study, Arterburn detailed, BMI percentile or BMI z-scores in children and adolescents and the estimated total health care costs were steady across most BMI percentiles, save for a sharp increase for a BMI ≥99th percentile (see Figure 4-2).
After inflation adjusting these numbers to 2023, Arterburn estimated that health care expenditures (Ward et al., 2021) in U.S. adults with a BMI of 30–34.9 kg/m2 were $7,300 per person,1 increasing to $9,300 with a
___________________
1 2023 costs inflation adjusted from 2015 estimates from Ward et al. (2021) using https://www.bls.gov/data/inflation_calculator.htm (accessed September 22, 2023).
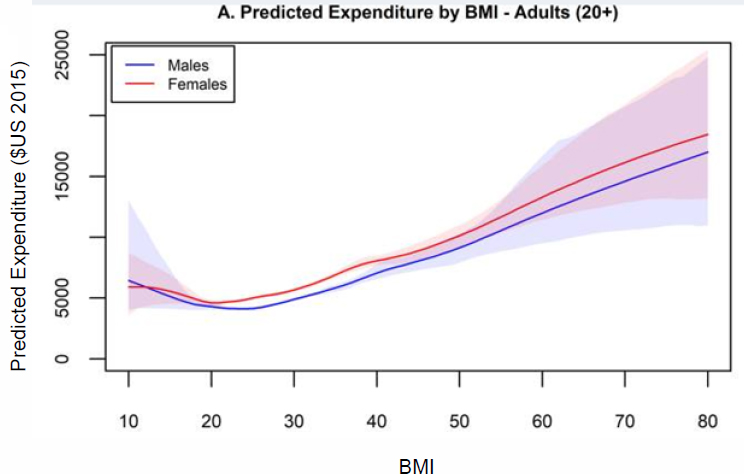
NOTE: BMI = body mass index.
SOURCES: Presented by David Arterburn, April 4, 2023. Ward et al. (2021). Reprinted with permission.
BMI >35 kg/m2. The estimated cost was 26 and 43 percent higher for a BMI over 30 kg/m2 or over 35 kg/m2, respectively, compared to the normal range (18.5–24.9 kg/m2). In 2023, Arterburn reported, 41 percent of Kaiser Permanente Washington region’s health care system patients had a BMI of over 30 kg/m2, which accounted for 50 percent of its health care costs.
Arterburn shifted to alternative measures for visceral fat and their costs and limitations. He admitted that waist circumference and digital anthropometrics are cost effective and possible in the clinical setting. However, the drawbacks are that staff must be trained, patients and staff often find the waist circumference uncomfortable to perform, and additional time is required. Referring to cost estimates from the Healthcare Bluebook (2022), a hypothetical laboratory test to improve the diagnosis of obesity could cost as much as $100 per test, but no viable option exists. He agreed with other presenters that dual X-ray absorptiometry (DEXA) is an accurate measure of visceral adiposity but also expensive, about $200 per test. A computerized tomography (CT) scan of the abdomen and magnetic resonance imaging are better measures of visceral adiposity and even more expensive, estimated at $750 and $1,250 per test, respectively.
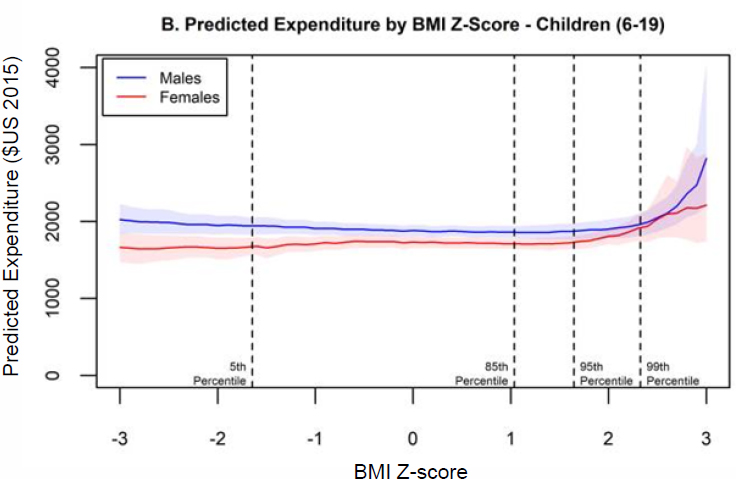
NOTE: BMI = body mass index.
SOURCES: Presented by David Arterburn, April 4, 2023. Ward et al. (2021). Reprinted with permission.
Arterburn described estimates for the Kaiser Permanente health care system with alternative measures for visceral fat in the clinical setting. He indicated that implementing these in a health care system would lead to a dramatic increase in costs. If screened annually in adults with a BMI of 30-34.9 kg/m2, the estimated costs to the health system would be: $150 million per year for laboratory measures, $300 million per year for whole body DEXA, $1.13 billion per year for abdominal CT, and $1.88 billion per year for MRI. Although the cost for obtaining anthropometrics is listed as $0, staff training and time would be considerable.
Arterburn also described the financial implications of obesity treatment. Treatment guidelines recommend comprehensive lifestyle interventions for people with a BMI ≥30 or ≥25 kg/m2 with comorbidities (Jensen et al., 2013). Based on these comorbidities, he estimated that up to 65 percent of U.S. adults could be eligible (unpublished estimates); 50–55 percent with a BMI ≥30 kg/m2 or ≥27 kg/m2 with comorbidities would be eligible for pharmacotherapy with a lifestyle intervention, and up to 30 percent could be eligible for metabolic surgery based on the American Society of
Metabolic and Bariatric Surgery updated guidelines, which includes patients with a BMI ≥35 kg/m2 regardless of comorbidities, adults with a BMI of 30–34.9 kg/m2 and a pre-existing metabolic disease, and an adjusted BMI cutoff (≥27.5 kg/m2) for Asian Americans with an increased health risk (Eisenberg, 2022).
Arterburn reported on recent estimates that if 5 percent of adults with obesity in Medicare Part D received a prescription for semaglutide or phentermine and topiramate, it would cost $13 billion or $659 million (Baig et al., 2023), respectively.
Arterburn concluded that despite its limitations, BMI is more cost effective and efficient than alternatives. He acknowledged the heterogeneity for health risks in patients with a BMI <35 kg/m2. From a practical, population health standpoint, Arterburn suggested narrowing the criteria for those who will benefit most from treatment instead of broadening them with uncertain benefit. He suggested that additional measures for adipose tissue distribution could help identify those who are at greatest risk for health complications and would benefit most from weight loss.
Arterburn concluded by posing questions when considering tests beyond BMI. Is the test supported by strong scientific evidence? Can it identify people at greater risk of adiposity-related disease? Is it acceptable to patients and providers? Are clinicians effective at administering it? What does it cost? Is a clinical study of treatments (e.g., lifestyle, pharmacotherapy, surgery) needed to test the safety and efficacy and cost effectiveness for new subpopulations identified by it?
OCCUPATIONAL HEALTH AND SAFETY LENS ON BMI
Alberto Caban-Martinez, a board-certified physician-scientist, associate professor of public health sciences, and deputy director of the M.D.–M.P.H. Program at the University of Miami, presented his perspective on the use of BMI for occupational health and safety. He opened by challenging the audience to consider how the work environment could support body weight management in the U.S. worker population, which accounts for 166 million of 334 million documented and undocumented people.
Caban-Martinez asserted that work is a social determinant of health; it establishes a person’s income and economic stability and residence and neighborhood, which affects their access to schools and educational attainment, the availability of healthy and nutritious foods, and, of course, access to health insurance and health care.
Using data from the National Health Interview Survey, Caban-Martinez highlighted trends and the prevalence of obesity in the U.S. workforce from 1986 to 2002 (Caban et al., 2005). The results of his study showed that
Black men and women had a higher BMI rate than White men and women or others in the workforce (Caban et al., 2005).
Examining the data across occupational groups also showed differences in obesity prevalence. Police and firefighters exhibited a 2 percent increase, and blue-collar jobs, such as construction laborers, also had a 1.8 percent increase. Personal service occupations in skin care, hair care, animal care, and funeral service, farm workers, and other agricultural workers, exhibited a decrease, he said.
Caban-Martinez highlighted that women employed in motor vehicle occupations exhibited a 6 percent increase in obesity prevalence, and women in professional specialty occupations had a 2 percent increase. The prevalence among women employed as secretaries, stenographers, and precision production occupations decreased by ≤1 percent.
In 2014, Caban-Martinez shared, an updated paper examined occupations with the highest and lowest obesity prevalence. Employees in motor vehicle operation, construction and related work, law enforcement, and nursing, psychiatric, and home health aide had the highest prevalence; employees in health diagnosing, military, art and design work, and post-secondary school had the lowest (Gu et al., 2014).
Caban-Martinez provided some historical context, highlighting the evolution of the U.S. economy from industry to service-focused economy. In the 1940s, it was labor intensive, with its strengths in manufacturing, agriculture, and mining (Georgetown University Center on Education and the Workforce, 2018). From 1940 through 2016, manufacturing jobs declined significantly, and the U.S. economy shifted toward the service information sector, with greater employment opportunities in administration, educational services, financial activities, and health services (Georgetown University Center on Education and the Workforce, 2018). According to Caban-Martinez, this shift significantly impacted physical activity at work.
Caban-Martinez continued by sharing a recent study of U.S. workers aged 25–74 surveyed before, during, and after the COVID-19 lockdown that found that working from home was correlated with decreased physical activity (Streeter et al., 2021). Furthermore, fully remote workers were likely to spend more time sitting and less time exercising compared to those working partially from home and partially at their place of employment.
Looking at studies of obesity in firefighters in different geographical areas, Caban-Martinez discussed the potential challenges posed in the fire and rescue response. He presented a study with New York firefighters that found that 52 percent had obesity (Smith et al., 2012), compared to about 30 percent in Texas, Florida, and Missouri (Clark et al., 2002; Kling et al., 2020; Poston et al., 2011). Another study looked at a national sample of male firefighters and found that about 30 percent had obesity (Wilkinson et
al., 2014). Caban-Martinez shared his research on the physical activity of fire and rescue responders using wearable devices and actigraphy while at the station and during rescue operations. When self-reporting, firefighters often mischaracterized their level of physical activity when compared to the actigraphy; firefighters who had obesity were the most inconsistent in their level of physical activity.
Caban-Martinez’s research team also piloted a walking meeting to understand if it could reduce sedentary behavior in the office setting; a protocol was implemented and evaluated for its feasibility and acceptability in teams of fewer than six people. Workers wore actigraphy devices for 3 consecutive weeks. A baseline was established and followed to capture physical activity via the protocol. The findings indicated that, weather permitting, the meetings were largely accepted and increased the levels of moderate and very vigorous physical activity.
Caban-Martinez ended by highlighting opportunities to use the work environment to reduce sedentary behavior and improve body weight management, particularly in occupations with a demonstrated increase in obesity. He urged the audience to consider opportunities to work with employers, their employees, and the work environment to reduce sedentary behavior and support healthy body weight management through physical activity (Kling et al., 2016).
BMI OUTSIDE THE CLINIC: THE PATIENT PERSPECTIVE
Faith Anne Heeren, Ph.D. candidate at the University of Florida and founder and president of Outreach, Community, Engagement, Advocacy, Non-Discriminatory Support (OCEANS), a nonprofit advocacy group for adolescents with obesity, provided her perspectives and patient experience as a person living with obesity (OCEANS, 2023).
Heeren recounted that her weight trended in the 99th percentile from an early age. Her mother was concerned about her health and sought advice from health care providers. However, she found that their guidance was generally unhelpful (e.g., do not serve cookies for dinner) and not actionable or evidence based.
Despite her mother’s efforts to serve her natural and sugar-free foods, Heeren continued, she gained weight through childhood and adolescence, developing hypertension and insulin resistance. Through online research, Heeren’s mother discovered the Healthy Lifestyles program at Duke University that offered bariatric surgery for teenagers. Heeren decided to have bariatric surgery and attended monthly visits with Duke’s multidisciplinary team in preparation.
Heeren immediately felt the physical and mental health benefits of surgery. Her insulin resistance and high blood pressure resolved and did
not return. She had surgery in early summer before her junior year of high school, and by early fall, she had more energy and successfully earned a place on the varsity tennis team. Her confidence grew, and she began living a relatively carefree teenage life, shopping for prom dresses with friends, and participating in Senior Skip Day by walking limitlessly at the zoo. Her confidence was sustained in college, walking to classes on the UNC Chapel Hill campus, running 5K races, playing intramural sports, and participating in fitness classes at the student recreation center with friends. Heeren also started OCEANS to advocate for and offer support groups to adolescents living with obesity and undergoing treatment interventions.
Later in life, during graduate school and the COVID-19 lockdown, personal and family hardships and stress led to significant weight gain. She was challenged to complete activities of daily living without excessive fatigue and hip pain. In early 2023, she began to participate in an evidence-based behavioral weight-management program. After a month and a half, she lost weight, met with her provider to discuss anti-obesity medication, and had bloodwork that revealed additional health concerns. In February 2023, Heeren added topiramate. She achieved clinically significant weight loss and described less joint pain and more energy and confidence to continue monitoring her health and bloodwork. However, her health insurance refused to cover her weight-management services, so her plan is compromised and uncertain: “I have been on every side of the patient journey. I have had information and access to treatment, and now, I have information and am limited in my choices moving forward with treatment.”
PANEL AND AUDIENCE DISCUSSION
Butsch led a moderated panel. The audience asked Jensen, Arterburn, Caban-Martinez, and Heeren about the effect of excess weight on the musculoskeletal system; utilization rates for obesity treatments and the impact on health care costs; costs for diabetes screening and medications to treat metabolic-related diseases; diversity and inclusion in walking meetings; measuring adipocytes in the clinical setting; and identifying adipocyte density through an ultrasound.
Impact of Excess Weight on the Musculoskeletal System Beyond Cardiometabolic Health
An audience member opened the discussion with an appreciative comment for Heeren’s presentation and emphasized the importance of learning about her increase in energy and decrease in joint pain with her weight loss. More attention is typically given to obesity and cardiometabolic health
and less to the pressure on the musculoskeletal system or the mechanical implications of obesity, although they are clearly significant.
Caban-Martinez added that joint pain and lack of energy are important considerations, particularly for occupational health and safety; individuals who have obesity and work in manual labor, handling materials and staying in constant motion, often experience lower back and neck pain, with a load placed on the axial skeleton. Heeran’s presentation on her quality of life and impact of weight on her musculoskeletal system emphasized that the same experience was common among people with obesity or excess body weight.
Real-World Utilization Rates for Bariatric Surgery Through Kaiser Permanente
Referring to Arterburn’s presentation on using BMI or alternative measures to direct obesity treatment, a participant asked about data from Kaiser Permanente on the utilization rates for bariatric surgery. Arterburn responded that annually, 1–2 percent of members are eligible for and undergo it. However, the treatment guidelines encourage broader use; the cost estimate he presented was in response to these guidelines.
Data Availability on the Impact of Treatment on Health Care Costs
An audience member asked Arterburn about the increased cost of treating obesity and the medical care costs in his presentation. Are data available on the impact of different treatments on costs? Arterburn responded that data are not readily available, with a need for more research, including randomized trials, and long-term longitudinal studies to evaluate the impact of treatments on health care use and costs to evaluate their impact. He suggested that research could focus on patients with higher adiposity-related risks with measures to help identify subpopulations most likely to benefit from metabolic or mechanical treatments.
Diversity and Inclusion for People with Disabilities for Walking Meetings
An audience member commented on Caban-Martinez’s presentation and cited examples of people with disabilities and cultural aspects of women’s hair that may cause discomfort walking in a humid environment. They asked how issues of diversity and inclusion for people with visible and invisible disabilities are considered when promoting physical activity and exertion in the workplace, such as walking meetings. Caban-Martinez responded that only some work groups or offices can and should attend walking meetings. He emphasized the need for discussion about
the capabilities, limitations, and concerns of potential participants when the meetings are proposed. Considerations can range from footwear and activewear to issues of interruption, all of which should be discussed beforehand.
Cost of Diabetes Screening and Medications
An online participant inquired about the cost of a routine diabetes screening test. Arterburn responded that a hemoglobin A1C test (HbA1C) costs much less than $100 per test. The current recommendation for diabetes screening is to screen most or all people with a BMI of over 30 kg/m2 and those with a BMI over 25 kg/m2 with another metabolic-related health condition to help identify people with diabetes or prediabetes (to prevent the progression to diabetes).
Butsch followed up, inquiring about the costs of antihypertensives or cholesterol medications. Arterburn said that pharmacotherapies for different health conditions vary widely in cost and their impact on weight and metabolic health but noted a need for long-term data on the effects of obesity medications on reducing the incidence of cardiometabolic disease or mortality.
Antihypertensives and cholesterol medications show reductions in cardiovascular events and mortality when tested in long-term randomized controlled trials, which supports their cost, said Arterburn. He pointed out the wide variation in their costs. Pharmacotherapy for type 2 diabetes, which can include the glucagon-like peptide 1 (GLP-1) receptor agonists and sodium–glucose cotransporter 2 (SGLT2) inhibitors that lower glucose, are expensive but increasingly proposed in the clinical guidelines. The cost of care for type 2 diabetes is rapidly escalating.
Measuring Adipocytes in the Clinical Setting
A participant commented that Jensen’s presentation highlighted the size of adipocytes as predictive of metabolic health. How can the size of fat cells be measured and integrated into clinical settings? Jensen acknowledged the challenge and suggested that, ideally, providers could administer mini-liposuction or biopsy fat cells to determine their size, but this is unrealistic. Long term, he said, the goal is to have information available for providers to discern fat cell size, perhaps using fat distribution, sex, and age, without invasive procedures at regular appointments. However, fat cell size is irrelevant to the strain caused by excess weight on the musculoskeletal system.
Non-Health Care Professionals Communicating Technical Health Information to Students, Parents, and Workers
Butsch turned to BMI in school, asking Heeren about her experience and professional opinion. How is BMI used in that setting? Is it a surrogate marker? Heeren responded that in some school districts, parents receive a BMI report card for their child(ren). The problem, she said, is that parents do not always know how to interpret BMI or have access to evidence-based care to help guide what actions to take. So, she asked, what is the point of sharing BMI?
Caban-Martinez added that an objective from his study with firefighters with excess weight is to identify the most important technical, medical, and laboratory information and figure out how to optimally communicate with the participant.
Ultrasound Techniques to Identify the Density of Adipose Tissue
An audience member had a final question for Jensen. Could an ultrasound detect a difference in the density of adipose tissue with small versus large fat cells? Jensen responded that it is possible with new ultrasound techniques that have extremely high resolution; with ultrasound, researchers could identify fibrosis, vasculature, and characteristics of adipocytes. However, it is expensive, and acquiring funding for studies with it would be an obstacle.











