Launching Lifelong Health by Improving Health Care for Children, Youth, and Families (2024)
Chapter: 5 Health Care for Children and Youth
5
Health Care for Children and Youth
Elevate the role of the [health care] system beyond disease prevention and caring for sick children [. . .], design a better system with the patient and their caregiver in mind [. . . and support] the family system as the key pathway to promoting child health.
—Comment to committee from health foundation employee, Houston, Texas
Generally, the U.S. health care system is fragmented and uncoordinated, and it typically responds to diseases and health problems after they arise. Despite shifts to managed care and forms of capitation at the payer level, the fee-for-service payment model still dominates in payments to clinicians and provider organizations, incentivizing inefficient, inequitable, and unnecessarily costly care (see Chapter 6). Overall, the system is optimized to maximize visits, procedures, profits, and treating medical problems after they occur, rather than preventing them from occurring in the first place. This payment model provides little support for health promotion, team care, and coordination (National Academies of Sciences, Engineering, and Medicine [National Academies], 2023a).
As for adults, health care for children and youth in the United States is delivered in a patchwork of settings with little coordination among multiple insurers and siloed delivery systems. Children, youth, and their families find and receive care from a complex array of providers that differs based on geography, community, clinical and social need, and financing. The child health care system has largely been modeled after the adult system; however, as discussed in Chapter 1, five important factors (the “5 Ds”—developmental
change, disease/differential epidemiology, dependence, demographics, and dollars—indicate unique aspects of care delivery for children that require attention.
Despite the needed improvements, health care for children has seen innovations and improvements in many communities over the past few decades, providing a clear and evidence-based strategy for transformation. Advances have included greater attention to various social, family, and community factors influencing health outcomes; changing the content of pediatric care; building connections with other programs to enhance child and family development; coordinating care broadly; and linking families with other critical community resources. Yet bringing these strategies to scale and implementing them consistently have been hampered by payment and other factors. Even with this progress and well-evidenced strategies for change, the health status of children and young families in America is considerably inferior to that in comparable developed countries (see Chapter 4). Several prior reports have noted progress in implementing a life course approach, integrating mental and behavioral health into pediatric care—both primary and subspecialty—and integrating within community systems, although without broad and adequate uptake (National Academies, 2019d, 2022b, 2023c,f,j, 2024b).
Given this complexity, defining the scope of and discussing all the health care system’s elements and issues are difficult. This chapter focuses on a high-level review of health services for children and families and the clinical settings in which they are provided, with a specific examination of the opportunities and challenges for providing mental and behavioral health care. It spans primary care for preventive, acute, and chronic care services, emergency care, chronic care, subspecialty care, inpatient and intensive care, and rehabilitation. The chapter describes innovative expanded advanced primary care and specialty team care models that integrate physical and mental health care and provide a wider set of services to aid families and strengthen child development and wellbeing.
Most of this chapter focuses on transforming primary care to strengthen health promotion and disease prevention, but it also reviews innovations in inpatient and specialty care for children with acute and complex chronic conditions. The chapter concludes with a review of the pediatric health care workforce. Subsequent chapters discuss financing for health care (Chapter 6), care in conjunction with investments in population health (Chapter 7), care in school-based settings (Chapter 8), and measurement and accountability approaches to support an improved focus on health promotion and prevention and integrated, team-based care (Chapter 9).
The child and adolescent health workforce is diverse, including physicians (those with an MD or DO in pediatrics, family medicine, or general medicine), nurse practitioners and physician assistants, nurses, mental
health care providers, community health workers, and others. General pediatricians provide most primary care visits for U.S. children across all pediatric age groups, including adolescents (76% in 2019, 72% in 2020, and 72% in 2021; Hong, Huo, & Desai, 2023). Almost all U.S. children and youth have identified sources of primary care and insurance coverage, although the nature, quality, and accessibility of the services vary, and low-income children often report the local emergency room as their usual source of care. Residents of rural areas often lack access to many services, especially specialized services for children.
Some primary care providers offer mainly the essentials of traditional practice—immunizations, some screenings, identification and treatment of common acute conditions—and refer patients to other providers for needs beyond these basic efforts. In other cases, following the model of the family-centered medical home, primary care has evolved into a multidisciplinary team-based program, with integrated mental and behavioral health and links to other community programs and supports through extended team members, such as community health workers and social services providers. This shift toward team-based care presents a critical opportunity for medical providers and community partners (e.g., caregivers, schools, dietitians and/or nutritionists, specialists, pharmacies, nursing agencies, vendors of durable medical equipment, other home care agencies and counselors) to respond to the unique and evolving needs of children and youth by drawing on a variety of support systems (Katkin et al., 2017). Given the increasingly fragmented and complex landscape of health care, team-based care can serve as a catalyst for fostering more effective patient care and improving the experience of those in the workforce (Smith et al., 2018). In settings that support integrated care, screening and intervention with families has evolved from traditional screenings, such as for lead and anemia, to greater attention to relationships, child development and behavior, and social determinants of health.1 Increasingly, pediatric primary care providers have worked to identify and provide resources for addressing broader influences on child health, although financing rarely incentivizes such changes (see Chapter 6). Although these developments are not the norm, efforts to shift emphasis from diagnosis and treatment to prevention and health promotion require centering individual needs while simultaneously promoting population and community health (see Chapter 7).
Hospitals that provide care to children and adolescents offer a wide array of often very specialized services, building from extensive research advances and new diagnostic and treatment methods. As noted in Chapter 1, most pediatric subspecialists work in academic medical centers. Such placement
___________________
1 Such screenings are recommended through the national Bright Futures Guidelines (American Academy of Pediatrics [AAP], 2017).
has facilitated advances in medical care with astonishing impacts on disease management and children’s survival. The growth of excellent subspecialty care (e.g., for childhood cancers) has also moved a significant amount of specialized care from inpatient to outpatient settings. Today, pediatric inpatient care typically serves children who have relatively rare conditions or marked instability requiring more intensive care (Agency for Healthcare Research and Quality, 2021b, 2022b; Weiss, Liang, & Martin, 2022).
Children and families receive mental health screenings and services in several settings, including traditional practice; community-based mental health centers; schools and preschools; and, increasingly, primary care settings that integrate mental and behavioral health professionals and include community health workers as part of the mental health team. Children and youth also receive some mental and behavioral health services in juvenile justice settings and inpatient hospital settings—some of which are part of a children’s or general hospital, while others are focused solely on psychiatric and mental health. Finally, as an intermediate level between hospital and community settings, residential care provides supervised care at lower acuity levels than hospitals. Despite this array of settings, many children and youth do not receive needed mental and behavioral health care, and there is limited coordination among these settings or with the rest of the health care system, including primary care.
HEALTH CARE AND CRITICAL PERIODS OF DEVELOPMENT
Chapter 2 described sensitive and critical developmental periods, including preconception and prenatal periods; infancy, childhood, and adolescence; and the transition into adulthood. Understanding and optimizing these developmental periods—and ensuring that the health care system provides developmentally appropriate care as children and youth transition across these stages—are essential for children to thrive.
Preconception and Prenatal Health
Health during the preconception and prenatal periods is crucial to minimize the risk of adverse birth outcomes, such as preterm or low birth weight, and to optimize the healthy development of children (including organ formation, fetal growth, epigenetic changes, and long-term health outcomes) and their families (Keikha, Jahanfar, & Hemati, 2022; Khekade et al., 2023). These periods are critical because they lay the foundation for the health and development of the child, influencing outcomes from birth through adulthood (see Chapter 2). Preconception care involves health care interventions and services provided to individuals or couples before
pregnancy to optimize their health and promote favorable outcomes for both the pregnant person and the baby (Keikha, Jahanfar, & Hemati, 2022; Khekade et al., 2023). The Centers for Disease Control and Promotion (CDC), American Association of Family Physicians, and the American College of Obstetricians and Gynecologists provide guidance on prepregnancy or interconception care and counseling (Jack et al., 2008; Wise, 2008). This care includes health promotion and lifestyle adjustments, risk assessment, and management of preexisting conditions. Key components include health education on maintaining a balanced diet and folate supplementation, exercising, and avoiding harmful substances, as well as regular checkups and screening for health risks, medical conditions, genetic counseling, and ensuring immunizations are up to date (Herval et al., 2019; Peahl & Howell, 2021; Soucy et al., 2023). Health and lifestyle choices made before conception can have a profound impact on the health outcomes of future offspring (Atrash et al., 2006; Khekade et al., 2023). Preconception care helps to mitigate risks and support healthy development from the earliest stages, influencing long-term health outcomes for the child and family.
Optimizing preconception health requires broad strategies to reach the population at risk for pregnancy; multiple health care interventions have shown promise (Hemsing, Greaves, & Poole, 2017). Pediatric primary care can support preconception care among parents in their practice who are interconceptional for their next child. A multisite cluster randomized trial of a maternal health screener and brief intervention in primary care was found to be feasible and effective in increasing folate use and decreasing smoking (Chilukuri et al., 2018; Upadhya et al., 2020).
Early Childhood and Family Health
Families have more encounters with pediatric primary care in the first 3 years of life than with the education sector; thus, pediatric primary care represents a critical leverage point in promoting early relational health, in addition to focusing on health creation, prevention, and wellbeing for those with access. Most families bring their children to a health care provider for preventive care, with visits starting just after birth. Preventive care visits can be frequent in the first years of life—12 well child care visits are recommended to be provided to children in their first 3 years of life based on the national Bright Futures Guidelines—offering multiple touchpoints with families; preventive care is nonstigmatizing because it is a universal intervention in the United States (Roby et al., 2021). However, current trends in visits fall short of these national guidelines (see below).
Early intervention services for supporting the health and wellbeing of young children and families have been a focus for improving outcomes.
Home visiting programs starting prenatally or after birth demonstrate improved child, maternal, and family outcomes (see Chapter 7). Integration of home visiting programs with the health care system has been variable, and data sharing and more collaboration are needed (Tschudy, Toomey, & Cheng, 2013). The importance of early childhood preventive care and its impact on long-term health outcomes is well established. Several models have been proposed and studied to transform the delivery of preventive care during this critical period.
The Parent-focused Redesign for Encounters, Newborns to Toddlers (PARENT) model incorporates a culturally responsive parent coach as part of the care team for children aged 0–3 years. PARENT has been shown to improve the receipt of well-child care, enhance parent experiences, and reduce emergency department utilization (Coker et al., 2016; Mimila et al., 2017). The 3-2-1 Integrated Model for Parents and Children Together (IMPACT) program, launched by New York City Health and Hospitals in 2020, provides a comprehensive two-generation program integrating mental health, pediatrics, and women’s health to improve the long-term trajectory for each family unit (NYC Health + Hospitals, 2020). The program offers a personalized approach to care with routine screenings for mothers during pregnancy and postpartum follow-up and pediatrics visits, employing Healthy Steps workers to engage families during visits (HealthySteps, n.d.a,c). Screening identifies when a family has additional medical or nonmedical social needs, such as mental health care or food or income support, with interventions provided in addition to universal parenting supports within health care (Filene et al., 2013; NYC Health + Hospitals, 2020). Preliminary evidence indicates that the 3-2-1 IMPACT model can improve health outcomes among low-income populations (McCord et al., 2024).
School-Age Children
As children start school, health care visits decrease in frequency, occurring annually unless health issues require more frequent follow-up (AAP, 2023; Freedman, 2020; Riley, Morrison, & McEvoy, 2019). During this period, children can learn basic positive health behaviors. It is also a time when several behavioral and mental health disorders can manifest, and screening and early intervention for those conditions is critical for long-term mental and behavioral health (Abramson, 2022). Given the fewer primary care visits during this period (as well as limited access to care for some children), school-based health monitoring, including for mental and behavioral health problems, in collaboration with health care systems provides key preventive services and intervention (see Chapter 8).
Adolescents and Young Adults
Health care services during adolescence and emerging adulthood are critical for ensuring both their present and long-term health and wellbeing. Adolescence is an opportune time to address health-related habits—including diet, exercise, sexual and reproductive health, and substance use—that can impact longer-term health. However, many adolescents, particularly those from historically marginalized groups, face a variety of barriers to accessing health care services, including financial barriers, privacy concerns, lack of culturally responsive care, and timely availability of services. Adolescents also have needs that are distinct from those of children. Health services for adolescents and young adults need to prepare youth and their families for the developmental changes (physical, cognitive, and social) that take place during adolescence and address these changes with culturally informed services that are attentive to the needs of all adolescents (National Academies, 2019c).
Adolescents need access to models of care that consider the entirety of their needs—from medical to social—and other factors in their lives (e.g., social determinants of health, the cultural and social content in which they live; National Academies, 2019d, 2020b). Models of care need to promote communication, collaboration, and coordination among physical health and mental health care providers, youth, and their families.
With increasing independence and autonomy, adolescents need confidential care and preparation for navigating the health care system independently, particularly the transition into adult health care systems, although many do not receive preventive health counseling and key preparatory advice (Akers et al., 2014). Confidentiality concerns remain a critical barrier for adolescents seeking appropriate medical services (Pathak & Chou, 2019). Adolescents who have time alone with clinicians have higher rates of screening and discussion of sensitive topics, more opportunity to navigate the clinic setting and engage with their own health care, and receive confidential care (Al-Shimari et al., 2022; Brown & Wissow, 2009, 2010; Chung et al., 2024; Committee on Adolescent Health Care, 2020; Ford, English, & Sigman, 2004; Klein & Wilson, 2002; McKee, Rubin, & Campos, 2011). Many youth underuse behavioral health services, despite expressed interest and need for such services (Boyd, Butler, & Benton, 2018; MacDonald, McGill, & Murphy, 2018). Like younger children, many adolescents may first seek help for mental health concerns from primary care providers. Others may rely on schools, mental health providers, or crisis centers, or they may seek care at emergency departments or other treatment facilities (National Academies, 2019c).
While adolescent health care addresses health risks such as substance use, risky sex, and poor mental health, care encounters are also opportune for exploring and supporting an adolescent’s goals and strengths (Calabrese
et al., 2022; Lindstrom Johnson, Blum, & Cheng, 2014; Lindstrom Johnson, Jones, & Cheng, 2015). Further, as adolescents and young adults enter childbearing years, sexual and preconception health is of critical importance, as is gender-affirming care.
The transition from pediatric to adult health care is particularly important for adolescents with special health care needs and/or chronic health conditions (Bloom, Cohen, & Freeman, 2012; National Academies, 2018; Stein, Perrin, & Iezzoni, 2010), who, while transitioning within the health care system, also face typical adolescent life transitions and challenges (e.g., postsecondary education or employment, leaving home, parenthood). Factors during the transition into the adult health care system affect not only the uptake of services, but also the adolescents’ ongoing physical and mental health, overall wellbeing, quality of life, and educational and employment outcomes. Many youth and young adults with special health care needs and/or chronic or complex health conditions and their families do not receive the support they need in the transition from pediatric to adult health care (White et al., 2018). Medical care models that are purposeful and planned are critical at this stage in life; such care models prepare the adolescent and their family for the transition from child-centered to adult-oriented health care in a way that considers typical developmental processes as well as access, appropriateness, and continuity of services (Calabrese et al., 2022). Strong evidence supports a continuum approach to health care transitions that incorporates multiple elements of preparation, planning, tracking, and follow-through for all youth and young adults beginning in early adolescence and continuing into young adulthood (Calabrese et al., 2022; Cooley & Sagerman, 2011; Jones, Merrick, & Houry, 2020a; Lemke et al., 2018; Schmidt et al., 2020; White et al., 2018).
PEDIATRIC PRIMARY CARE
Primary care forms the base for every health care system. A report by the National Academies titled Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care defines “high-quality primary care” as “the provision of whole-person, integrated, accessible, and equitable health care by multidisciplinary teams who are accountable for addressing the majority of an individual’s health and wellness needs across settings and through sustained relationships with patients, families, and communities” (National Academies, 2021b, p. 4). The report notes that its definition does not describe what most people in the United States experience today, an observation supported by data from the National Survey of Children’s Health on indicators of quality of care (see Table 5-1). Table 5-2 summarizes data compiled by the committee on children’s health care utilization.
TABLE 5-1 Quality-of-Care Indicators for Children’s Health Care in the United States
| Performance Indicator | National Prevalence, % (Across State Prevalence Range) | U.S. Children with Any Public Health Insurance,a % | U.S. Children with Private Health Insurance,b % |
|---|---|---|---|
| Percent of children ages 0–17 years who have adequate and continuous health insurance | 68.0 (59.2–81.0) |
84.5 | 66.3 |
| Percent of children ages 0–17 years who received care in a setting that met core criteria for being a medical homec | 46.1 (33.8–57.1) |
36.3 | 55.6 |
| Percent of young children ages 9–35 months who received screening for their development | 33.7 (24.5–49.1) |
28.7 | 39.0 |
| Percent of children ages 3–17 years with a mental health condition who received treatment or counseling | 52.8 (31.9–67.6) |
52.0 | 54.9 |
| Percent of children ages 0–17 years whose health insurance and health care met criteria for being a well-functioning system of cared | 17.3 (11.6–23.8) |
14.8 | 21.2 |
| Percent of children enrolled in Medicaid/CHIP who had at least 6 of 9 recommended well-child care visits before age 15 months | Not available (N/A) |
55.7 (30.1–77.4) |
N/A |
| Percent of children enrolled in Medicaid/CHIP who had at least 2 of 4 recommended well-child care visits between ages 15 and 30 months | N/A | 64.9 (36.5–82.3) |
N/A |
a Public insurance is defined as Medicaid, Medical Assistance, or any kind of government assistance plan for those with low incomes or a disability.
b Private insurance is defined as insurance through a current or former employer or union, insurance purchased directly from an insurance company, TRICARE or other military health care, or coverage through the Affordable Care Act or other private insurance.
c The presence of a medical home was measured based on five components: personal doctor or nurse, usual source for sick care, family-centered care, problems getting needed referrals, and effective care coordination when needed.
d A well-functioning system of care was assessed based on children’s experience across several measures: (1) the family feels like a partner in their child’s care, (2) the child has a medical home, (3) the child receives medical and dental preventive care, (4) the child has adequate insurance, and (5) the child has no unmet need. A sixth measure is included for adolescents (ages 12–17 years): preparation for transition to adult health care.
SOURCE: 2021 and 2022 National Survey of Children’s Health (CAHMI, 2024); 2022 Child Core Set Report (Centers for Medicare & Medicaid Services, n.d.a).
TABLE 5-2 Children’s Health Care Utilization
| Health Care Effectiveness Data and Information Set | ||||
|---|---|---|---|---|
| Utilization Measurea | Year | Commercial HMO, % | Commercial PPO, % | Medicaid HMO, % |
| At least 6 well-child visits in first 15 months | 2022 | 81 | 80.8 | 56.8 |
| At least 2 well-child visits between 15 and 30 months | 2022 | 87.3 | 88.2 | 66.7 |
| At least 1 well-child visit in past year (ages 3–6 years) | 2019 | 79.1 | 77.7 | 74.1 |
| At least 1 well-care visit in past year (children and adolescents) | 2022 | 57.6 | 56.2 | 48.6 |
| National Center for Health Statistics, National Health Interview Survey | ||||
| Utilization Measure | Age Group | Year | Characteristic | Value |
| Visits to physician offices and hospital emergency departmentsb | Under age 18 years | 2018 | Number of visits (thousands) | 128,781 |
| People with hospital stays in the past yearc | 1–17 years | 2019 | % with 1 or more hospital stay | 2.6 |
| 1–5 years | 2019 | % with 1 or more hospital stay | 3.2 | |
| 6–17 years | 2019 | % with 1 or more hospital stay | 2.4 | |
| Emergency department visits in the past 12 months among children under age 18 yearsd | All childrene | 2018 | % with 1 or more emergency department visit | 17.6 |
a The percentages indicate the proportion of eligible children who met the criteria for each measure and are based on national averages.
b Data are based on reporting by a sample of office-based physicians and hospital emergency departments
c Data are based on household interviews of a sample of the civilian noninstitutionalized population.
d Data are based on household interviews of a sample of the civilian noninstitutionalized population.
e Includes all other races not shown separately and those with unknown health insurance status.
NOTE: HMO = health maintenance organization; PPO = preferred provider organization.
SOURCE: Generated by the committee, based on data from National Committee for Quality Assurance, n.d., and National Center for Health Statistics (n.d.) CDC Data Finder.
Pediatric primary care includes a broad range of services (National Academies, 2019d), with a priority on provision of comprehensive age-specific physical and mental health promotion and preventive services, particularly as outlined in Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents (AAP, 2017).2 The guidelines cover monitoring physical, cognitive, and socioemotional growth and development. They include screening for metabolic and genetic conditions in the newborn period; developmental screenings at specific ages; screenings for health conditions, such as autism, anemia, and vision or hearing impairment, and exposures, such as lead; screening for socioemotional issues and maternal and adolescent depression; and screening for social and/or other nonmedical drivers of health. There are also resources for age-specific guidelines to educate and counsel parents/caregivers on promoting the healthy development of their children. Pediatric primary care supports health promotion and disease prevention by providing immunization, dental fluoride varnish, and anticipatory guidance on topics related to physical and mental health, as well as physical and emotional development. In addition, a growing number of practices screen for social determinants of health and provide referrals and links to community services to address family needs.
Primary care also includes diagnosing and treating acute health conditions, such as infectious illnesses and injuries, as well as identifying and caring for children with special health care needs and chronic illnesses, such as asthma and attention deficit hyperactivity disorder (ADHD). Depending on the level of complexity of a child’s illness, the primary care clinician may diagnose and treat such conditions or may refer to and coordinate care with pediatric medical and surgical subspecialists. Primary care practices also help coordinate care with households in managing insurance coverage and access to prescriptions; diagnostic testing; subspecialty care; physical, occupational, and speech therapies; and other services. Primary care clinicians often link families to services in other sectors that are important for the overall health and wellbeing of children, such as nutrition programs (e.g., Special Supplemental Nutrition Program for Women, Infants, and Children) and early education programs (e.g., Head Start, school-based preschool programs).
Children and youth obtain primary care in multiple settings: independent pediatric and family medicine practices, larger private group practices (single and multispecialty), health centers (federally qualified health centers [FQHCs] and similar community health centers, Indian Health Service [IHS] facilities, and school-based health centers [SBHCs]), hospital or health care system–based practices, and military treatment facilities (clinics located on
___________________
2 The Bright Futures Program is funded through a cooperative agreement from the Health Resources and Services Administration with the American Academy of Pediatrics to create and share clinical national guidelines for pediatric well-child visits from birth to age 21.
military installations). Nonemergency acute care is also provided through urgent care facilities and retail-based clinics. Although in the previous century, U.S. primary care tended to occur in smaller, independent practices, over time delivery has shifted toward community clinics, hospital outpatient clinics, and health care system practices (Simon et al., 2015).
Primary care office visits are declining both across adult populations (Ganguli, Lee, & Mehrotra, 2019) and among commercially insured children and adolescents, where visits fell approximately 13% between 2008 and 2016 (Ray et al., 2020). Problem-based visits dropped 24%, while preventive care visits increased by 10%, visits to nonprimary care settings increased, and out-of-pocket costs for problem-based visits increased (Ray et al., 2020). This is consistent with findings that the number of FQHCs and the number of patients they serve have increased since 2001 (National Association of Community Health Centers [NACHC], 2014).
The next section reviews some specific settings for primary care for children and youth, including community health centers, settings for specific populations, and SBHCs, and concludes with a discussion of the growing area of telehealth.
Community Health Centers
Community health centers provide primary care and other services for 30 million people, including 12% of all U.S. children (NACHC, 2022). Health centers often serve communities with otherwise limited access to health care and high social need. Most community health centers are FQHCs. Through the Health Resources and Services Administration (HRSA, 2022b), the federal government supports about 1,400 health centers and similar organizations with more than 14,000 service delivery sites across the United States. FQHCs have governance boards with more than 50% patients served by the health center and are designed to meet the specific needs of the communities they serve. Many community health centers offer integrated behavioral health services, dental care, pharmacy, cancer screening, vision and eye care, pharmacy, and diagnostic and laboratory services. They also offer case management and referral to specialty care and social services, if necessary. While community health centers are not all the same, many provide more comprehensive, whole health services that focus on prevention, social needs, and upstream factors than are available in other settings (National Academies, 2023a). FQHCs provide services to about 14% of those in marginalized racial/ethnic groups in the United States, as well as 20% of the country’s individuals who are uninsured, 33% of those living in poverty, and 20% of those in rural areas. Almost 80% of FQHC patients have either public insurance or lack insurance; approximately 90% of patients had income less than 200% of the federal poverty level (NACHC, 2023a,b).
Special Population Health Care Providers
Families and children may access primary care in other settings, including IHS clinics and on-base military treatment facilities. These facilities offer comprehensive and culturally competent care tailored to the specific needs of these populations, address health disparities, and ensure access to essential health services. IHS clinics offer comprehensive services akin to community health centers and are important access points to care for American Indian/Alaska Native tribal nations (see further discussion of the IHS in Chapter 6, see also IHS, n.d.a).
Pediatric clinics located within military treatment facilities are accessible to active-duty and retiree families who are TRICARE beneficiaries (Hero et al., 2021). TRICARE is the Department of Defense insurance program for eligible service members, retirees, and their dependents. On-base pediatric clinics follow a patient-centered medical home model of care (Defense Health Agency, 2019). TRICARE beneficiaries can also access care through the broader TRICARE network of civilian providers.
School-Based Health Centers
SBHCs, located on or near primary and secondary school campuses, may provide primary and preventive medical care, behavioral health services, diagnostic care such as routine screenings, and/or preventive dental care (Medicaid and CHIP Payment and Access Commission, 2018b). SBHCs vary in services provided, accessibility, degree of integration with the school, and quality of care. Although most SBHCs are operated by an FQHC, others receive support from school districts or a combination of local health care systems, public health departments, and community-based organizations. A 2016–2017 census indicated that the number of SBHCs doubled in the previous 20 years, with more than 2,500 SBHCs operating in the United States in 2016, serving 10,629 schools and more than 6.3 million children (Love et al., 2019). As of 2019, 40% of SBHCs served elementary school–age children, 30% middle or high school–age youth, and 30% children in all other grade combinations (Love at al., 2019). While this number represents only about 13% of schools nationwide and services vary widely, these facilities are typically located in areas of higher need, where communities face greater barriers to health care access (Love et al., 2019; Soleimanpour, 2020). SBHCs are more common in schools with larger proportions of socially and economically disadvantaged youth (Love et al., 2019) who may also experience disproportionate academic challenges (Chetty et al., 2019) because of structural inequalities that extend far beyond what SBHC services can influence directly (Soleimanpour, 2020). This complexity adds to the challenge of demonstrating impacts on not only health outcomes but also educational success.
SBHCs are associated with positive short- and long-term outcomes, including increased access to health services for children, families, and communities; improved health including increased use of cost-effective preventive care, such as immunizations, family planning, well-child visits, and behavioral health care; improved clinical quality scores in areas such as well-child visits, immunizations, chlamydia screening, depression screening and follow-up, and asthma control; increased health equity through access to culturally competent, high-quality, first-contact primary care; and increased number of regular patient groups and community engagement for FQHCs, school districts, and other health care providers (Arenson et al., 2019; California School-Based Health Alliance, 2022; Key, Washington, & Hulsey, 2002; Knopf et al., 2016). SBHCs have been shown to manage and treat chronic health conditions effectively, improve prenatal care and pregnancy outcomes for pregnant teens, and decrease teen pregnancy rates (Arenson et al., 2019).
Nearly 70% of SBHCs offer mental health services. Despite limitations, SBHCs can be an important access point for screening and treatment of mental health conditions, especially for children with no insurance or public insurance, who are more likely to seek mental health services at SBHCs than those with commercial insurance (Arenson et al., 2019; Keeton, Soleimanpour, & Brindis, 2012; Knopf et al., 2016). Mental health services in schools improve mental health access and outcomes (see further discussion in Chapter 8).
Overall, for children with access to them, SBHCs are an important source of primary care, chronic condition management, and mental health services. Expansion of SBHCs, particularly in resource-limited settings, is an important strategy for improving equitable access to high-quality care for children and is an approach recommended by CDC’s Community Guide and the Community Preventive Services Task Force (2021) as a means of advancing health equity.
Telehealth
Telehealth is the provision of health services remotely via video, phone, or mobile device. Telehealth can increase patient access; improve care coordination; strengthen the role of the primary care clinician; and allow subspecialists the time to provide inpatient and outpatient care in a manner that is feasible, fulfilling, and financially sustainable and best for children (Curfman, Hackell et al., 2021; Curfman, McSwain et al., 2021a,b; National Academies, 2023c,g,i). The COVID-19 pandemic led to rapid and widespread expansion of telehealth in pediatric primary care, where its use had not been common previously (Curfman, Hackell et al., 2021; Curfman,
McSwain et al., 2021a,b). With the public health emergency, policy changes allowed children with acute and chronic illnesses to connect via telehealth services to their usual source of care for management of their conditions. Many states allowed preventive care using a hybrid model that combined virtual and in-person visits (Hsu et al., 2023). During the pandemic, telehealth improved access to care for many children and youth, although disparities in access to technology and digital infrastructure related to poverty, systemic racism, and other inequities were also highlighted (Zhang et al., 2023). A review of prepandemic studies of the use of telehealth in pediatric care in specific contexts—including asthma, obesity, ADHD, and skin care—found low- to moderate-quality studies with outcomes for telemedicine interventions that were comparable to or sometimes modestly better than routine care, with positive results for parent satisfaction (Shah & Badawy, 2021).
Many mental health care systems have used telehealth to provide virtual consultations with child and adolescent psychiatrists, psychologists, and therapists (University of Texas Rio Grande Valley School of Medicine, n.d.). For example, the Texas Child Health Access Through Telemedicine program links school staff evaluating students to appropriate telehealth services (University of Texas Rio Grande Valley School of Medicine, n.d.) Telehealth allows mental health providers to collaborate with primary care physicians for early detection and treatment of conditions such as anxiety and depression. Virtual visits also make it easier for busy families to access care, reducing transportation barriers and the time between symptom onset and treatment (CDC, n.d.e). Telehealth is proving to be an effective and scalable solution to the pediatric mental health workforce shortage and improving outcomes for children and adolescents (Archer et al., 2021; deMayo et al., 2022; Gajarawala & Pelkowski, 2021; Guthrie & Snyder, 2023; Thomas et al., 2023; Totten, McDonagh, & Wagner, 2020).
Telehealth virtual visits with patients or teleconsultation across specialties are likely to continue to grow as will remote patient monitoring. New technology and the use of artificial intelligence have the potential to increase the efficiency of practice by decreasing documentation time, managing patient communications, synthesizing data, or prereading images. Virtual visits and remote patient monitoring (e.g., for failure to thrive, diabetes management, asthma, hospital follow-up) will keep more patients at home. New models of care building from telehealth are exploring “hospital at home” and “going to where the kids are” with expanded connectivity and services in schools, child care, and in the home (including home visiting). Ethical and equity considerations for patients and the workforce must be central as these innovations evolve. With children being “digital natives,”
and given the developmental origins of health and disease early in the life course, inclusion of pediatrics in these innovations is essential.
Recently, many state Medicaid programs have introduced new telehealth policies and payment opportunities, telehealth portals, telepsychiatry consultations, and collaborative care as solutions to help overcome challenges of geographical access, with a notable increase in the implementation of such models during the COVID-19 pandemic (Federation of State Medical Boards, 2023; Kwong, 2024). Prior to the pandemic, the use of telehealth in Medicaid was becoming more common; in particular, most states offered some coverage of behavioral health services delivered via telehealth, and the majority of telehealth utilization was for behavioral health services and prescriptions. However, Medicaid policies regarding allowable services, providers, and originating sites vary widely across states, with often unclear payment policies. To increase health care access and limit risk of viral exposure during the pandemic, all 50 states and the District of Columbia expanded coverage and/or access to telehealth services in Medicaid (Federation of State Medical Boards, 2023; Kwong, 2024). Many have permanently adopted telehealth policy expansions, although some states have limited coverage of audio-only telehealth. Regionalization of pediatric specialists makes coverage of telemedicine services across state lines of particular importance.
At the federal level, the Bipartisan Safer Communities Act (2022) directed the Centers for Medicare & Medicaid Services (CMS) to issue guidance to states on expanding access to telehealth in Medicaid. In 2023, CMS (2023j) published Telehealth for Providers: What You Need to Know, which outlines various provisions and flexibilities that CMS has issued, including those impacting Medicaid services delivered via telehealth. It provides detailed information on state policies, Medicaid coverage, and best practices for telehealth services, which align with the directive from the Bipartisan Safer Communities Act (CMS, 2023j).
Retail Clinics
Retail clinics, which have spread in many regions, provide easy access for minor illnesses and often advertise convenience and lower costs in providing such services as immunizations or sports physicals (Garbutt et al., 2013; Wong et al., 2017). Among the fastest-growing components of ambulatory care for children and adults, up to 90% of retail clinic pediatric visits focused on ten common conditions, including immunizations (Mehrotra et al., 2008). While increasing access to care, they are ill equipped to provide continuity of care and comprehensive services such as those mandated under Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment services (see discussion in Chapter 6).
INNOVATION AND CHANGE IN PEDIATRIC PRIMARY CARE
Primary care in pediatrics has evolved substantially over the past several decades, from early work by the U.S. Children’s Bureau to the development and growth of the medical home model (National Academies, 2019d), aiming to transform pediatric primary care from individual-centered, treatment-focused care to whole child, family, and community health care as reviewed in Chapter 1. Active implementation of the medical home model began in 1967, with greater recognition of the importance of early life and child and community factors in the development and wellbeing of children (Sia et al., 2004). The medical home transformation called for pediatricians and pediatric clinicians to provide guidance to young families, coordinate their care and access to needed additional services, and serve as a main point of care that families can easily access for help with the broad range of services that they and their children need. The medical home model calls for comprehensive, high-quality primary care for children and youth, emphasizing characteristics of accessibility, family-centeredness, continuity, coordination, compassion, and cultural proficiency (AAP, 2022; Boudreau et al., 2022). The federal Maternal and Child Health Bureau has long championed the medical home concept, collaborating actively with the AAP in its support and development. And the medical home concept underlays key aspects of primary care reform in the Patient Protection and Affordable Care Act (2010).
Medical home models differ in their focus and content for different age groups, but they generally follow a broad set of definitions and standards recognized by several professional organizations such as the AAP and the National Committee for Quality Assurance (Domino, 2021). The AAP, American Academy of Family Physicians, American College of Physicians, and American Osteopathic Association have jointly outlined seven core principles of a patient-centered medical home3 (American Academy of Pediatrics, American Academy of Family Physicians, & American College
___________________
3 The AAP earlier outlined four principles for pediatric medical homes, described as “a family-centered partnership within a community-based system that provides uninterrupted care with appropriate payment to support and sustain optimal health outcomes” (Ad Hoc Task Force on Definition of the Medical Home, 1992, p. 774; see also AAP, 2007; Buka et al., 2022). These principles include: (1) Family-centered partnership: Providing family-centered care through a trusting, collaborative partnership with families, respecting diversity and recognizing families as constant in a child’s life. (2) Community-based system: The medical home is part of a coordinated network of community services designed to promote healthy child development and family wellbeing. (3) Transitions: Facilitating smooth transitions along the continuum of care as the child moves through different systems and into adulthood. (4) Value: Appropriate financing to support and sustain medical homes that promote quality care, optimal health outcomes, family satisfaction, and cost efficiency (AAP, 2007, p. 1).
of Physicians-American Society of Internal Medicine, 2002; see also AAP, 2007; Kellerman & Kirk, 2007):
- Personal physician: Each patient has an ongoing relationship with a personal physician trained to provide first contact, continuous, and comprehensive care.
- Physician-directed medical practice: The personal physician leads a team of individuals that collectively takes responsibility for the ongoing care of patients.
- Whole person orientation: The personal physician is responsible for providing all the patient’s health care needs or taking responsibility for appropriately arranging care with other qualified professionals.
- Coordinated and integrated care: Care is coordinated and integrated across all elements of the complex health care system.
- Quality and safety: Quality and safety are hallmarks of the medical home, with a focus on evidence-based medicine and clinical decision-support tools.
- Enhanced access: Enhanced access to care is available through systems such as open scheduling, expanded hours, and new options for communication.
- Appropriate payment: The payment structure appropriately recognizes the added value provided to patients who have a patient-centered medical home.
These principles developed nearly 20 years ago by physician organizations center the role of physicians. More recently, as discussed in this chapter, a wider range of clinicians provide primary care; however, the principles of a medical home still emphasize continuity of care, in alignment with the concept of whole person health (National Academies, 2023a; see also Chapter 2). Although the medical home model has helped improve care generally, its impact on families living in poverty has been limited because they often do not receive care that aligns with the principles of the medical home (Liljenquist & Coker, 2021; MacArthur & Blewett, 2023).
Nonetheless, development of the medical home concept over the years has led to innovation and testing of new and expanded models of high-performing pediatric primary care. These changes reflect a growing understanding of important characteristics and content of pediatric primary care (see Figure 5-1). Main advances have taken place in the content of primary care, improved coordination of care, and providing access to other services that support whole child and relational health (CMS, n.d.e; InCK Marks, 2020). Advances in the content of care have included increasingly sophisticated screening for social determinants of health and broader assessment of behavior and development. Addition of programs such as Reach Out and Read (Jimenez et al., 2023) and
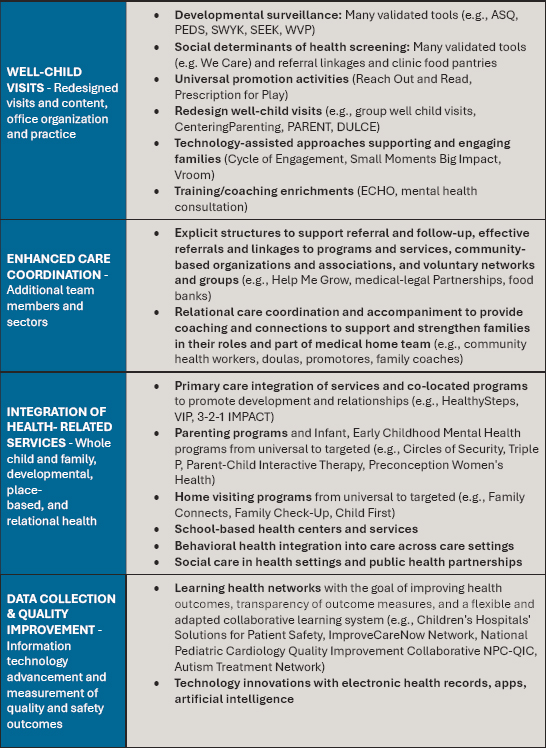
NOTES: This figure is not exhaustive of all evidence-based innovations in child health care transformation but reviews some areas of innovation to the traditional health care model, including redesigned well-child care, integration of systems and added services, personnel, and technology. The maturity of these innovations is variable, with some in their infancy and others progressing rapidly. ASQ = Ages & Stages Questionnaire; DULCE = Developmental Understanding and Legal Collaboration for Everyone; ECHO = Extension for Community Healthcare Outcomes; NPC-QIC = National Pediatric Cardiology Quality Improvement Collaborative; PARENT = Parent-focused Redesign for Encounters, Newborns to Toddlers; PEDS = Parents’ Evaluation of Developmental Status; SEEK = Safe Environment for Every Kid; SWYK = Survey of Well-being of Young Children; VIP = Video Interaction Project; WVP = Well-Visit Planner.
SOURCE: Generated by the committee based on InCK Marks, 2024.
Prescription for Play have enhanced support for parents (Weitzman Institute, 2023). Coordination of care efforts include strategies to help households link to community resources and support, through programs such as medical–legal partnerships or StreetCred (both providing legal counseling and help with accessing various benefit programs in primary care settings), and Help Me Grow, which helps link families with a broad array of community resources (American Hospital Association [AHA], 2020; Boston Medical Center, 2023). Programs such as Healthy Steps (2024) enhance pediatric care by connecting early childhood workers with young families. Others have developed parent behavior training programs through pediatric practices. Box 5-1 describes the initiative Pediatrics Supporting Parents, aimed at using early well-child visits as an opportunity to support relational health. Box 5-2 describes several promising programs with innovative approaches to pediatric team care.
Healthy Steps is among the better-studied programs, with good evidence that the program improves up-to-date well-child visits and immunizations and more family-centered care. Parents also report improved strategies for
BOX 5-1
Opportunities for Centering Relational Health in Pediatric Care
Recognizing the great importance of early childhood and wellbeing—and the importance of supporting relationships within young families—several programs have developed to strengthen and support efforts in pediatric primary care. Well-child visits (usually there are 12 between birth and age 3 years) present a unique context for interacting with and supporting families to promote relational health. In 2017, the Silicon Valley Community Foundation launched Pediatrics Supporting Parents (PSP), with support from five early childhood funders (Cohen Ross et al., 2019; Cornell, 2019). Given the importance and critical nature of early childhood experiences, PSP emphasizes enhancing pediatric care in the early years to help improve socioemotional development through support of the primary caregiver–child relationship (Cohen Ross et al., 2019; Cornell, 2019; Cornell, Therriault, & Dworkin, 2021; PSP, n.d).
The PSP initiative centers on collaboration among health care professionals, educators, and community organizations (Cohen Ross et al., 2019; Cornell, 2019). Pediatricians, child psychologists, and experienced parenting coaches work in tandem to provide evidence-based strategies and practical advice on various aspects of child-rearing. From addressing common concerns such as sleep routines, discipline techniques, and developmental milestones, to tackling more complex issues such as behavioral challenges and special needs, the program offers a comprehensive suite of services tailored to each family’s unique circumstances.
Early work focused on implementing an integrated platform, incorporating tools such as the Survey of Well-Being of Young Children, Well-Visit Planner, Promoting Healthy Development Survey, Welch Emotional Connection Screen, and FINDconnect (Cornell, 2019), and identifying 14 common practices for promoting
managing their young children’s behaviors (HealthySteps, 2024; Minkovitz et al., 2007; Piotrowski, Talavera, & Mayer, 2009). The Video Interaction Project, begun at New York University, uses video tapes of parent–child interactions also to help parents learn strategies to address their children’s behaviors and learn how to support the child’s development (Canfield et al., 2015; Mendelsohn et al., 2005, 2011; Video Interaction Project, n.d.). Reach Out and Read has a substantial evidence base, showing significant improvement in children’s literacy (High et al., 2000; Sinclair et al., 2019). More recent work has documented improvements in parenting stress and parent–child relational interactions (Canfield et al., 2020). All of these (and several other) innovations have developed good evidence for their effects on care and outcomes, and many have seen substantial growth in their uptake in pediatric primary care over the past decades. Nonetheless, as indicated in Chapter 6, financing has not transformed to support these key advances and bring them to scale.
socioemotional development (Center for the Study of Social Policy & Pediatrics Supporting Parents, 2018; Cornell, 2019). Later work has aided practices with strategies for implementing and financing these changes (CSSP, 2018).
Two California programs exemplify the lessons from the earlier PSP work. Built in part on specific California benefits that support whole family health and dyadic care for young families, these two programs have enhanced connections of primary care with other early childhood activities. The LIFT/ACEs LA Medical-Financial Partnership (MFP) and Network of Care addresses the complex social and financial situations of low-income and working-class families by providing clinic-based financial coaching (Bell et al., 2020; Holguin et al., 2023). Existing studies, while limited, have shown that MFPs improve both health outcomes and family finances (Bell et al., 2020; Holguin et al., 2023). The MFP approach provides structured financial counseling and helps families identify their strengths, priorities, goals, and actionable steps aimed at improving economic stability. The University of California, Los Angeles’s MFP assists with connecting families to resources that can assist them in navigating social systems and structures that can otherwise prove prohibitively difficult to engage with. The MFP helps affiliated clinics develop and maintain networks of financial and social resources, which are available to all families served at the clinics (Holguin et al., 2023; Spiker, 2023).
The University of California, San Francisco Center for Child and Community Health and the Ready! Resilient! Rising! (R3) Network serve to transform early childhood health care for low-income children. R3 includes educators, health plans, health providers, and social service agencies collaborating to improve whole child health through trauma-informed screening for basic needs and expanded behavioral health care in pediatric primary care. These trauma-informed programs create pathways for families to combat and overcome toxic stress in early childhood.
Increasingly, the medical home model has moved to team-based care, supporting the changing and expanding content of pediatric primary care
BOX 5-2
Models Supporting Early Child Wellbeing in Pediatric Primary Care
Several programs have innovated models for strengthening pediatric teams and staffing in early childhood care. Each helps pediatric primary care transform to team-based care.
DULCE
Developmental Understanding and Legal Collaboration for Everyone (DULCE) is a team-based approach to pediatric care that transforms how families experience health care (Center for the Study of Social Policy [CSSP], n.d.). Based in the pediatric care setting, it proactively addresses social determinants of health, promotes the healthy development of infants, and provides support to their parents during the critical first 6 months of their child’s life (Center for the Advancement of Youth [CAY], n.d.). DULCE introduces into the care team a family specialist trained in child development, relational practice, and problem solving. Family specialists attend well-child visits with families and providers, get to know the families, provide peer support, and collaborate with the team to connect families with resources and support. The DULCE program includes family specialists, medical providers, legal partners, early childhood systems representatives, and mental health representatives, along with a project lead and a clinic administrator. By addressing the accumulated burden of social and economic hardship, the DULCE team reduces family stress, giving families more time and energy to bond with and care for their new child (Monahan, McCrae, & Arbour, 2024). The DULCE approach to social determinants of health recognizes the inequities in the distribution of power and resources, rooted in a history of racism (McCrae et al., 2021), and uses community health models to create a more equitable distribution of power and resources (CAY, n.d.; CSSP, n.d.a,b).
HealthySteps
HealthySteps is a three-tiered model that integrates developmental and behavioral services into pediatric primary care for children from birth to age 3 years (HealthySteps, n.d.b, 2022; Piotrowski, Talavera, & Mayer, 2009; Valado et al., 2019). It employs HealthySteps specialists, who are experts in child development and behavioral health, to work alongside pediatric providers. These specialists offer services such as developmental screening, positive parenting guidance, care coordination, and referrals to community resources. Evaluations have provided evidence for the model’s effectiveness in promoting healthy child development and family wellbeing (HealthySteps, 2022; Piotrowski, Talavera, & Mayer, 2009; Valado et al., 2019). HealthySteps improves the quality of care and the capacity of pediatric practices to operate as institutional resources within their communities (Barth, 2010; Valado et al., 2019). The model also improves child health outcomes, including breastfeeding rates, age-appropriate nutrition, timely developmental screening and intervention, and socioemotional development (HealthySteps, 2022; Piotrowski, Talavera, & Mayer, 2009; Valado et al., 2019). Other findings include enhanced parenting practices and maternal mental health (Forum on Promoting Children’s Cognitive, Affective, and Behavioral Health, 2014; Minkovitz et al., 2003, 2007; Valado et al., 2019).
Help Me Grow
Help Me Grow (HMG) leverages and expands upon existing resources to create a comprehensive approach to early childhood system-building within any community (HMG National Center, n.d.). The model provides a centralized access point to enhance utilization of existing community resources rather than creating new programs. Research shows HMG positively impacts child and parent factors by improving understanding of child development and increasing access to supportive services (Bogin, 2006; Dworkin & Kelly, 2022; Hill & Hill, 2018; HMG National Center, 2023; Hughes et al., 2016; Therriault et al., 2021). The model integrates with broader child and family-serving systems, addressing complex social needs that impact development. HMG employs targeted universalism to ensure equitable access to quality services. The Centers for Disease Control and Prevention endorsed HMG as a strategy for achieving equity, which bolsters the model’s foundation in targeted universalism and supports its validity and importance (Robinson et al., 2017).
Reach Out and Read
The Reach Out and Read program is a nationally recognized early literacy intervention implemented in pediatric primary care settings across the United States (Garbe et al., 2023; Klass, Dreyer, & Mendelsohn, 2009). Founded on the principle that promoting early literacy is essential for children’s cognitive and socioemotional development, the program integrates literacy promotion into routine pediatric visits by providing developmentally appropriate books to children during well-child checkups and offering guidance to parents on the importance of reading aloud (Garbe et al., 2023; Miller et al., 2023). Participation in Reach Out and Read is associated with numerous positive health outcomes, including improved language and literacy skills, enhanced parent–child bonding, increased school readiness, and reduced developmental disparities among children from low-income families (Garbe et al., 2023; Jimenez et al., 2023; Klass, Dreyer, & Mendelsohn, 2009; Needlman et al., 1991).
PlayReadVIP
PlayReadVIP, originally known as the Video Interaction Project, is an evidence-based parenting program developed by a team at the New York University Grossman School of Medicine (NYU Langone Health, n.d.; PlayReadVIP, 2024). The program aims to enhance early child development and literacy by utilizing videotaping and developmentally appropriate toys, books, and resources to help parents engage in pretend play, shared reading, and daily routines with their children (Center for Parents & Children, n.d.; Institute of Human Development and Social Change, n.d.). PlayReadVIP sessions involve one-on-one coaching during routine well-child visits where parents receive feedback on their interactions with their children. Participation in PlayReadVIP improves children’s socioemotional, cognitive, and language development (Cates et al., 2018; Mendelsohn et al., 2011; Miller et al., 2023; Piccolo et al., 2023; Roby et al., 2021), increases parental engagement, and reduces parenting stress and depression (Berkule et al., 2014; Canfield et al., 2023; Cates et al., 2016; Miller, 2023). The program’s integration into pediatric primary care provides a strategic platform for reaching high-risk families and promoting school readiness skills among low-income children.
by basing care in a multidisciplinary team. Teams support more care for behavioral and developmental needs, coordination of care with greater numbers of children and youth with chronic health conditions, and connection to community resources for nonmedical drivers of health. Well-designed team-based models optimize existing resources and personnel to deliver care and leverage the expertise of all team members; address the total whole person needs of the community; and focus on the upstream drivers of health, disease prevention, and health promotion (National Academies, 2023a). Team-based health care has been linked to improved health care quality, patient outcomes, and cost savings, with increasing evidence that it also improves clinician wellbeing (Jacob et al., 2015; Pape et al., 2011; Roberts et al., 2001; Tiel Groenestege-Kreb, van Maarseveen, & Leenen, 2014).
Traditional pediatric office practices typically include one or more clinicians, with support from nurses or medical assistants, and office staff. Extended teams include a variety of additional staff (often depending on community needs) that may include advanced practice nurses (to help coordinate chronic care), mental and behavioral health professionals, and community health workers, as well as care managers, interpreters, nutritionists, lactation specialists, school liaison staff, health educators, health coaches, and attorneys and other medical–legal partnership staff. Figure 5-2 provides examples of an extended health care team and extended community care team, with the patient and the family at the center of the core team.
Team approaches to care, when adequately staffed and resourced, have many benefits in clinical settings. For example, team-based care is associated with reduced workload, increased efficiency, improved quality, improved patient outcomes, reduced fragmentation, and decreased clinician burnout and turnover (National Academies, 2019e, 2021b). Expanding teams addresses some of the major time constraints faced by usual physician-run primary care—where time available to address social, community, and developmental issues can limit services. Well-designed teams can also support nurturing, longitudinal, person-centered care (Mitchell et al., 2012; Sullivan & Ellner, 2015), a key feature of high-quality primary care (National Academies, 2021b). Effective teams are designed to meet the specific needs of the communities they serve. Ideally, teams reflect the diversity of the communities they serve (Katkin et al., 2017) and evolve with the changing needs of the community over time (National Academies, 2021b, p. 182; see also Bodenheimer, 2019; Bodenheimer & Smith, 2013; Brownstein et al., 2011; Coker, Thomas, & Chung, 2013; Coker et al., 2009, 2014; Fierman et al., 2016; Grumbach, Bainbridge, & Bodenheimer, 2012; Katkin et al., 2017; Margolius et al., 2012).
Recent studies have shown the particular value of community health workers (and related workers such as peer counselors and family coaches) in improving health and outcomes (Bruner & Kotelchuck, 2023). Reviews of studies (though mainly among adult populations) found improved treatment adherence and decreased hospitalization and more attention to social
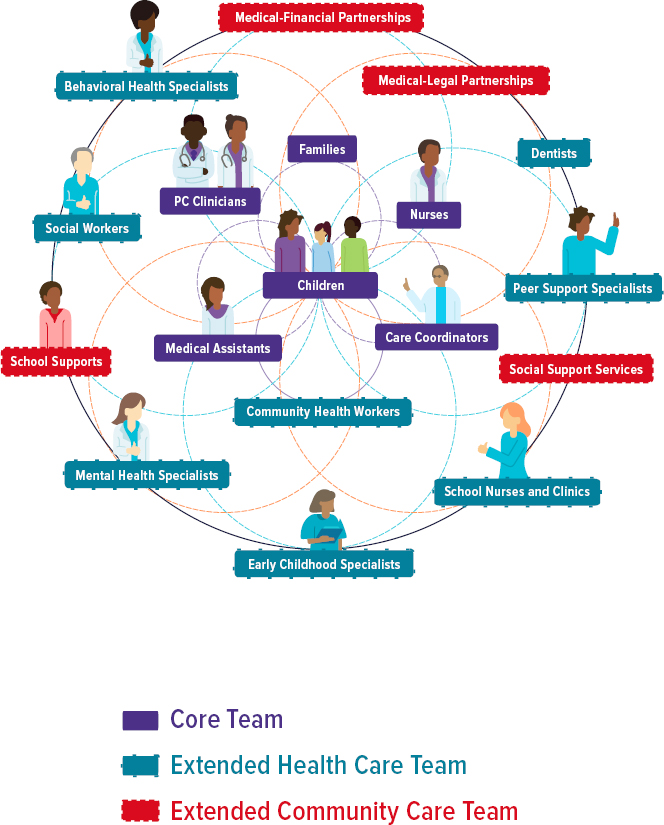
NOTE: PC = primary care.
SOURCE: Adapted from National Academies, 2021b.
determinants of health (Kangovi et al., 2020; National Academies, 2021b; Vasan et al., 2020). The PARENT intervention has documented how family coaches reduced emergency department use and increased preventive care services (Coker et al., 2016; Mimila et al., 2017).
The extended community care team in Figure 5-2 involves clinical–community partnerships and cross-sector, multidisciplinary programs such as medical–legal and medical–financial partnerships, clinic-based food pantries, and embedded and school behavioral health services. Screening for child and family needs and social determinants of health have accompanied
BOX 5-3
Medical–Legal Partnerships (MLPs)
MLPs integrate legal advocates into health care settings to address health-related social needs of the child and family. There are more than 400 MLPs across the United States where legal advocates work with clinicians to co-design social risk screening, educate health care professionals about legal remedies, and intervene to address health-harming legal issues (e.g., housing, public benefits, utilities, educational needs; Beck et al., 2021). Legal advocates are powerful allies in driving upstream changes to promote health, and MLPs enable broader, system-level pattern recognition and advocacy in pursuit of health equity and justice. A retrospective cohort study examining the effect of referral to an MLP on hospitalization rates among urban, low-income children in Greater Cincinnati, Ohio, found that the median predicted hospitalization rate for children in the year after referral was almost 40% lower if children received the legal intervention than if they did not (Beck et al., 2022). Clinicians report that MLPs also increase their self-efficacy for addressing child and family needs by improving their awareness of the social determinants of health and health-harming legal issues, empowering them to engage in systemic advocacy and improving their relationships with patients’ families (Murillo et al., 2022).
team-based care. However, the effect of such screening is often limited without further assistance with referrals, navigation supports for families, and monitoring of follow-up. When linked to facilitated referrals, a comprehensive program can help families increase access to community services. Systematic screening and closed-loop referrals for social determinants during well-child care lead to larger initial enrollment in community resources for families (Garg et al., 2015). Box 5-3 describes the growth of medical–legal partnerships to support pediatric transformation addressing social determinants of health.
While there is compelling evidence that team-based approaches to primary care can foster high-quality, efficient, continuous, and relationship-based care (National Academies, 2021b), making the transition to a team-based approach to care delivery often requires additional support. Many practices—especially independent small to medium-sized practices and those located in resource-limited communities—find the transition challenging, both logistically and financially. Dominant fee-for-service payment offers few incentives for this transformation, not only in terms of paying for additional multidisciplinary team members, but also in terms of financing the development of the clinic-level infrastructure needed to make the shift to team-based delivery. Most team-based care expansions have come from a combination of some billed services (especially for mental and behavioral treatments), grants, and philanthropy (Assistant Secretary for Planning and Evaluation, 2023a). A few state Medicaid programs have allowed billing for various nonphysician personnel or have restructured payment with
incentives to develop team-based care (MassHealth, 2022). Additionally, in 2023, the Centers for Medicare & Medicaid Services (2023c) implemented rule changes designed to improve equity, including a change that makes it easier to cover community health workers on care delivery teams. Most, but not all, states currently allow Medicaid payment for community health workers (see Box 5-4; Haldar & Hinton, 2023).
BOX 5-4
Community Health Workers (CHWs)
CHWs have critical roles in improving access to health care and addressing social determinants of health for children and families, particularly in underserved communities. CHWs serve as trusted liaisons between health care systems and the communities they serve, bridging cultural and linguistic gaps, and providing culturally appropriate support and education (Coker et al., 2016; Rogers et al., 2023). In pediatric care settings, CHWs support caregivers of children with special health care needs, helping them understand and manage their child’s condition, navigate the health care system, and address clinical and social needs (Moheize et al., 2024). CHWs and family coaches have helped reduce hospitalizations and emergency department visits for children with asthma, promoting medication adherence, and empowering families to better manage chronic conditions (Costich et al., 2019). By connecting families with community-based organizations and resources, CHWs address social determinants of health, including transportation, food insecurity, housing instability, and financial strain (Costich et al., 2019; Moheize et al., 2024; Rogers et al., 2023).
Peer- and family-support specialists are nontraditional workforce additions who can also help teams provide comprehensive support and improve health outcomes (Hayhoe et al., 2018; Malcarney et al., 2017; Department of Health and Human Services [HHS], 2007). Peer-support specialists are individuals with lived experience of mental health conditions or substance use disorders who use their personal recovery stories to inspire hope, provide emotional support, and assist others in navigating the recovery process. They facilitate support groups and skill-building activities, and advocate for individuals’ needs and rights, promoting self-determination and empowerment. Research has shown that peer-support services can improve engagement in treatment, reduce hospitalizations, and enhance overall recovery outcomes (Hayhoe et al., 2018; HHS, 2007; Malcarney et al., 2017).
Family-support specialists, also known as family peer advocates or family partners, are caregivers or family members of individuals with disabilities, mental health conditions, or other special health care needs (National Indian Child Welfare Association [NICWA], 2014; Robertson et al., 2023; Substance Abuse and Mental Health Services Administration [SAMHSA], 2017). They leverage their personal experiences to support other families by providing emotional understanding, helping them navigate complex service systems, advocating for family-centered care and rights, facilitating peer-support groups and skill-building workshops, and promoting family empowerment and self-advocacy. The involvement of family-support specialists has been associated with improved family functioning, increased access to services, and better outcomes for children with special health care needs (NICWA, 2014; Robertson et al., 2023; SAMHSA, 2017).
Still, many practices, particularly small and medium-sized independent practices, face both space limitations and difficulty finding needed multidisciplinary personnel, especially in rural areas. Workforce demands and burnout have especially affected the supply of mental and behavioral health personnel. One tactic that small and medium-sized practices can take is banding together to pool resources and sharing certain personnel or community resources (e.g., social services) across multiple practices (Mostashari, 2016).
MENTAL AND BEHAVIORAL HEALTH CARE PROVIDERS AND SETTINGS
The mental health care system is also diverse, including multiple settings, with limited coordination among the several sectors involved. Behavioral health services are provided across six general sectors: behavioral health care systems, schools, child welfare, substance abuse services, medical and primary care clinics, and juvenile justice. Services focus on treatment rather than prevention and often do not meet the basic population-level behavioral health needs of children and youth in the communities they serve (American Psychological Association Task Force on Evidence-Based Practice for Children and Adolescents, 2008).
Traditional models of outpatient mental health services may focus primarily on mental health diagnosis and its intra- and interpersonal complications rather than on the interaction of a diagnosis with physical health and health-maintenance behaviors. Services may take place in the offices of a physician, psychologist, social worker, or mental health counselor and increasingly virtually. Often, such mental health services are out of network or paid for out of pocket, as finding in-network behavioral specialists, particularly psychiatrists, can be more difficult than finding other types of specialists (National Alliance on Mental Illness, 2016, 2017; Overhage et al., 2024).
Other settings may involve a multidisciplinary team of professionals—including psychologists, psychiatrists, developmental and behavioral pediatricians, social workers, and therapists—who collaborate to provide assessment, diagnosis, and treatment (Haines et al., 2018). Clinics may be publicly funded as community mental health centers or may take only commercial insurance (or private pay). Clinics often tailor therapeutic interventions to each child’s specific concerns, utilizing evidence-based approaches such as cognitive-behavioral therapy, dialectical behavior therapy, and play therapy (Bhide & Chakraborty, 2020; Hoagwood et al., 2001; Kaminski & Claussen, 2017). Additionally, these settings may offer medication management as needed. With an emphasis on creating a supportive and nurturing environment, clinicians strive to empower children to explore their emotions, develop coping skills, and foster resilience (Masten & Barnes, 2018; Ronen, 2021). Family involvement is often encouraged to promote holistic healing and facilitate long-term stability and wellbeing for the child (Berger
& Font, 2015; Hogue et al., 2021). Regular monitoring and follow-up ensure that interventions remain effective and adaptable to the child’s evolving needs (Almirall & Chronis-Tuscano, 2016; Colizzi, Lasalvia, & Ruggeri, 2020). Disparities in access for children seeking mental, emotional, and behavioral health care in the United States stem from differences in insurance coverage, geographic availability of services, cultural barriers, and stigma, leading to unequal access to care based on financial resources, location, ethnicity, and perceptions of mental illness (Hoffmann et al., 2022; Mongelli, Georgakopoulos, & Pato, Toure et al., 2022).
School-based mental health programs have emerged as integral components of the children’s mental health care system, providing on-site counseling services, behavioral interventions, and crisis support to students within the familiar environment of their educational settings (see Chapter 8). These programs facilitate early identification and intervention for mental health issues and promote collaboration among educators, mental health professionals, and families to create supportive learning environments conducive to emotional wellbeing.
Inpatient psychiatric treatment provides acute care for those experiencing serious mental health and/or behavioral concerns that require a higher level of care for safety, treatment management, and supervision. Inpatient care provides intensive treatment services ranging from milieu therapy to medication management and a high level of supervision in a restricted, controlled environment. Children and youth may be hospitalized at the recommendation of a physician, mental health provider, or family following assessment. Follow-up outpatient therapy and services are essential for continued stabilization and alleviation of symptoms following inpatient psychiatric treatment, including residential treatment and other options.
The current U.S. child mental health crisis has contributed to a notable shortage of pediatric inpatient psychiatric treatment facilities, especially in rural states (Feuer et al., 2023; Gulliver, Griffiths, & Christensen, 2010; Ibeziako et al., 2022, 2024). This has resulted in pediatric mental health boarding of youth in emergency departments or admitted to inpatient medical/surgical units, awaiting placement in psychiatric treatment programs (Dalton et al., 2023; Feuer et al., 2023; Ibeziako et al., 2022, 2024; Zipursky et al., 2023). Interventions to address this have included enhanced crisis stabilization services, bridge programs to safely discharge patients with a bridge to expedited follow-up, and treatment initiation in the emergency department and on inpatient medical/surgical units for boarding patients awaiting placement.
Residential treatment centers offer longer-term therapeutic interventions for children with persistent mental health challenges, providing structured programming, individualized treatment plans, and opportunities for skill-building and rehabilitation (CMS, 2023h). Partial hospitalization programs provide structured and intensive psychiatric treatment for children and adolescents experiencing acute mental health crises or significant
functional impairment (CMS, n.d.f). These programs typically offer a comprehensive range of therapeutic interventions, including group therapy, individual counseling, medication management, and educational support, while allowing participants to return home each day. Residential treatment and partial hospitalizations programs designed for children are in short supply.
To meet growing needs for mental health services, the health care system has evolved to expand access to services through a range of providers and settings that best serve families and children, including a wide variety of mental health professionals. Many of these professionals specialize in child and family health, and some provide team-based care for children and families. Furthermore, efforts are increasing to train other health care professionals, including physicians and primary care providers, to recognize and identify mental health issues and treat mild to moderate issues when possible and/or refer to specialized care. Some health care systems have even engaged, trained, and funded those with lived experience with mental health issues to help others (Levine, 2023).
Extension for Community Healthcare Outcomes (ECHO) programs have emerged as a promising strategy for improving mental health services for children especially in under-resourced areas (Hager et al., 2018; Zhou et al., 2016). These programs leverage technology to connect specialists with primary care providers, behavioral health experts, and other health care professionals allowing them to collaborate, share expertise, and build capacity to effectively address children’s mental health needs. Project ECHO employs a model that connects a specialist team, the “hub,” with providers, or “spokes,” across a wide area using videoconferencing technology (Lalloo et al., 2020). ECHO programs improve providers’ knowledge, confidence, and competence in diagnosing and treating various mental health conditions in children, including depression, anxiety, and behavioral disorders (Sockalingam et al., 2018). Additionally, ECHO programs promote a collaborative and multidisciplinary approach to care, which can lead to more comprehensive and holistic treatment plans that address the unique needs of each child. ECHO programs contribute to reducing disparities in mental health care access and outcomes among underserved populations, ensuring that children receive the support and treatment they require for optimal mental health and wellbeing.
Barriers to Pediatric Behavioral and Mental Health Services
Untreated mental health disorders in childhood have a high likelihood of persisting into adulthood (Mulraney et al., 2021). Yet families face many barriers when trying to engage services, with long delays in accessing care or receiving no care at all. More than half of children with mental health problems do not receive care from a mental health clinician for more than 3 years after a problem arises (Whitney & Peterson, 2019). In all, only about 20% of children with mental and behavioral health disorders receive
care from a mental health clinician (Martini et al., 2012). Accessibility (e.g., distance to agency, coordination of services, knowledge of available services), availability (e.g., mental health workforce shortage, limited scope of services), affordability (e.g., care cost, insurance coverage, copay), and acceptability (e.g., stigma, dual relationships) create barriers, especially for rural communities (National Rural Health Association [NRHA], 2015).
Medicaid and the Children’s Health Insurance Program (CHIP) are the dominant payors for behavioral health services for children and adolescents in the United States (Counts, 2022; Dieleman at al., 2020). However, many behavioral health providers do not accept Medicaid payments, and penetration rates of Medicaid-funded services remain low, with over half of children who need services not accessing care (Pires, McLean, & Allen, 2018). While Medicaid and CHIP provide comprehensive behavioral health services, children with commercial insurance tend to access these services more frequently, likely due to fewer access barriers and higher utilization rates of specific services, such as psychotherapy (Ali et al., 2019; Doupnik et al., 2020; Haley et al., 2023; Kalmin et al., 2023). Many behavioral health providers, including psychiatrists and psychologists, work in private settings and accept no insurance (Bishop et al., 2014; Hamp et al., 2016). Services provided through private practices vary in terms of quality and availability, with little systematic information available on the structure of these services.
The current availability and financing of substance use prevention, assessment, and treatment services fall short of meeting the needs of young people. In 2019, only 8% of adolescents and young adults who required substance use treatment received it, according to data from the Substance Abuse and Mental Health Services Administration (2020). This disparity in treatment access is linked to social, economic, and criminal justice inequities, as well as stigma within the health care system toward substance use (Jordan, Mathis, & Isom, 2020; Marrast, Himmelstein, & Woolhandler, 2016; National Academies, 2016b). Black and Hispanic adolescents and young adults with substance use disorders are particularly affected by these inequities, being less likely than non-Hispanic White youth to receive specialty substance use treatment as of 2021 (Cummings, Wen, & Druss, 2011; Pinedo & Villatoro, 2020). Furthermore, the majority of adolescents and young adults with opioid use disorder do not receive medications for it, and non-Hispanic Black and Hispanic youth are less likely to receive medications than non-Hispanic White youth (Alinsky et al., 2020; Bagley et al., 2020; Mauro et al., 2022; Society for Adolescent Health and Medicine, 2021).
Several reasons explain the lack of availability of treatment. One barrier is the stigma that surrounds mental health. Even in places where resources and mental health supports are available, there can be reluctance to promote them and to make use of them. Another primary barrier is that most communities lack sufficient providers. There are shortages of qualified mental health providers across the spectrum of all licensed practitioners
(especially psychologists, psychiatrists, developmental and behavioral pediatricians, addiction counselors, mental health counselors, and psychiatric–mental health nurse practitioners). A 2018 analysis estimated that 9,956 child and adolescent psychiatrists were practicing actively (approximately 15 practitioners per 100,000 children under age 18 years; Beck et al., 2018). Distribution of clinical child and adolescent psychiatrists and psychologists is uneven across the country, with the majority located in the Northeast and on the West Coast (Andrilla et al., 2018; Lin & Stamm, 2020). Particularly troubling for children and youth is the projected shortage of 21,030 school counselors over the next 15 years; these estimates are based on current use of behavioral health services in the United States and do not consider that significant needs for the same services are currently going unmet (National Center for Health Workforce Analysis [NCHWA], 2023). Children and youth from rural areas have less access to mental health care than their urban peers (NRHA, 2015). Many rural counties have no practicing psychiatrists or social workers at all (Counts, 2023). With such shortages, families often have to travel long distances, endure long wait times to receive services, or go without services.
Disparities in Pediatric Mental and Behavioral Health
Compared with White children and adolescents, children from historically marginalized racial/ethnic groups have a higher prevalence of many mental and behavioral health conditions and are less likely to receive services for them (Hoffmann et al., 2022). Compared with White children, Black and Hispanic children have fewer mental and behavioral health visits, are less likely to be seen by specialists, have lower expenditures, are less likely to be prescribed psychotropic medication, and are less likely to receive evidence-based care for common mental and behavioral health conditions (e.g., anxiety, depression, ADHD, substance use). This unequal access to services and treatment is thought to have led to the poorer outcomes discussed in Chapter 4.
Stark racial/ethnic disparities are evident in diagnosis and care for autism spectrum disorder. Reports from the Autism and Developmental Disabilities Monitoring (ADDM) Network (CDC, 2020c) have consistently found disparities in diagnosing autism in children in Black and Hispanic populations. Potential barriers leading to these disparities include stigma, lack of access to health care services due to noncitizenship or low income, and non-English primary language (ADDM, 2018; CDC, 2019c). What is more, Black children with autism often experience a delay in diagnosis, are underidentified, or are misdiagnosed with a disruptive behavior disorder (Hoffmann et al., 2022).
Literature on disparities in mental health care receipt among U.S. children and adolescents is nuanced and complex. Several studies have highlighted variations in the nature and direction of disparities across different mental health conditions and over time. While racial/ethnic disparities in
ADHD diagnosis and treatment have narrowed in recent years (Coker et al., 2016; McKay & Perente, 2019), disparities persist for conditions such as depression and anxiety, with minority youth being less likely to receive outpatient mental health services (Cummings & Druss, 2011; Hodgkinson et al., 2017; Hoffmann et al., 2023; Lê Cook et al., 2019; Marrast, Himmelstein, & Woolhandler, 2016). Children from low-income families and those without adequate insurance are also less likely to receive needed services (Hodgkinson et al., 2017; Kirkbride et al., 2024). The specific mental health condition, age group, and geographic region studied can influence the nature and direction of disparities, highlighting the complexity of the issue (Hoffmann et al., 2023).
While the many societal, political, and economic factors that created and continue to perpetuate a system of unequal treatment go beyond what the health care system can do alone, the mental health care system can take steps at both the delivery and larger systems levels, to help minimize disparities. At the clinician level, understanding implicit biases and taking steps to minimize them, such as by using standard screening and diagnostic instruments and standardizing their implementation, is one way of reducing disparities (Viswanathan et al., 2022). Similarly, ensuring that the care delivered is culturally competent and trauma informed can help as well (Trent, Dooley, & Dougé, 2019). At an organizational level, eliminating any race or ethnicity considerations that are used in detrimental ways in treatment algorithms or practice guidelines is another way to reduce treatment disparities based on race or ethnicity (Wright et al., 2022). Progress toward reducing disparities must be tracked over time (Harrington et al., 2021).
Integrating Mental and Behavioral Health Care with Primary Care
Integration of behavioral health services into primary care has grown over the last few decades, partly in conjunction with the exponential rise of the mental health challenges children and families face, but also from recognition that prevention and early detection can help avoid more serious conditions later. Early experimentation took place about 50 years ago, with slow but definite growth since that time. In Child Health and the Community, Haggerty (1975) documented the growing mental and behavioral health issues in pediatrics (the “new morbidity”). Integration has the added benefit of improving access to care, improving equity, and reducing silos between service lines and thus managing a workforce more efficiently. Having mental and behavioral health clinicians as part of team-based care also expands the range of care available and can link mental and behavioral health providers with community health workers and others to improve community prevention and treatment strategies. Numerous organizations advocating for children’s health support greater integration of mental and behavioral health into pediatric primary care (Ader et al.,
2015; American Academy of Child and Adolescent Psychiatry, 2023b; National Academies, 2019b).
Pediatric settings are well suited for early identification and intervention of childhood mental and behavioral health concerns (Talmi et al., 2016), as families seeking mental health services often seek care initially from their pediatric clinician. Consequently, mental health symptoms and disorders are among the most common concerns addressed in pediatric care (Yonek et al., 2020). Integrating mental and physical health can help with care coordination, access, efficiency, and outcomes for children and their families (Reiss-Brennan, 2014; Reiss-Brennan et al., 2016; Walter et al., 2019). Team-based integrated behavioral health supports primary care clinicians and families by improving providers’ skills in engaging families to discuss mental and behavioral health concerns, comanaging identification and treatment, sharing information that facilitates coordination and communication across providers, and using evidence-based screening tools for developmental and behavioral disorders (Hine et al., 2017; Talmi et al., 2016; Tyler, Hulkower, & Kaminski, 2017). Operationally, integration can range from simple coordination and colocation of clinical services to a more robust collaborative care model (Asarnow et al., 2015). With collaborative care, primary care and behavioral health professionals, often supported by a care coordinator and other team members, work on a single treatment plan with both behavioral and medical elements in a single system of care that addresses whole child and family health (Gerrity, 2016; National Academies, 2021b,c).
One of the benefits of integrated behavioral health is streamlining the provision of needed services. A common challenge faced by families with mental health needs is navigating the behavioral health care system, referral to appropriate and/or culturally appropriate services, and limited follow-through on community-based mental health referrals (Hine et al., 2017; Talmi et al., 2016). With integrated mental and behavioral health services, most mental and behavioral health needs can be addressed within a single system. In instances when additional services are needed, providers identify and connect patients and families to community resources and programs to address their needs and provide individualized, person-centered care that incorporates family members and caregivers into the treatment plan.
Integrated behavioral health care is a worthwhile investment because it addresses gaps in care seen with traditional models, increases access to specialty care, and improves behavioral health outcomes (Tyler, Hulkower, & Kaminski, 2017). Kolko and Perrin (2014) found positive effects on children’s mental health problems (greater reductions in externalizing and internalizing problems), parent–child interactions, parental distress, and lowered treatment costs per patient, when comparing integrated with usual care. In a follow-up paper, the authors emphasize more distal indicators of
effectiveness in measures of “feasibility, clinical effectiveness, heightened consumer satisfaction, coordination and continuity of care over time, and potential cost savings related to less use of restrictive and costly placements or other services” (Yu, Kolko, & Torres, 2017, p. 57).
Despite the many benefits of integration, the transition to integration can be challenging, requiring supports different from those needed for adult care (National Academies, 2021b). Because child mental health concerns are most often linked to parental mental health and family psychosocial needs, successful pediatric behavioral health integration requires mechanisms for identifying and addressing the mental, social, and parental–child interaction needs of the entire family (Wissow, Platt, & Sarvet, 2021). Relatedly, child mental health is often more behavioral focused and time intensive (and thus resource intensive) than adult care, which is more commonly addressed with medication.
HOSPITAL-BASED AND SPECIALIZED CARE
Hospitals provide a wide range of health services for children and youth, including hospital-based primary care activities and specialty outpatient, urgent, and emergency care. They also provide inpatient care when needed for critical acute conditions, when chronic conditions become unstable, or for severe trauma and injuries. Various surgical procedures require treatment and follow-up in hospitals or surgical centers. Most U.S. births occur in hospitals, including specialized neonatal intensive care for sick newborns.
Consolidation has characterized the hospital sector over the past several decades, including consolidated locations for hospital beds for children and youth, which has contributed to rising costs and reduced access (Goodwin, Levinson, & Hulver, 2023; Levins, 2023). With the decreasing rates of childhood conditions requiring hospitalization (e.g., decreased rates of infectious disease, increasing outpatient care) along with cost concerns in maintaining a pediatric unit where low Medicaid payment compromises revenues, the hospital industry for children and adolescents has seen a continuing decline in numbers of pediatric beds and consolidation of hospital inpatient services in a smaller number of often larger hospitals (Cushing et al., 2021; Leyenaar et al., 2016, 2023; Perrin, Valvona, & Sloan, 1986). Over the past decade more than 200 hospitals in rural areas of the United States have closed labor and delivery units, reducing access to maternity and neonatal care. These closures have been due to financial and workforce issues and result in long drive times to receive care.
One study categorized hospitals as Tier A hospitals that provided care only to children; Tier B hospitals that had key pediatric services, including pediatric emergency departments and pediatric and neonatal intensive care units; Tier C hospitals that provided limited pediatric services; and Tier D
hospitals with no key pediatric services. Classifications were then validated by using publicly available data on hospital membership in various pediatric programs as well as Health Care Cost Institute claims data. Fifty-one hospitals were classified as Tier A; 228 as Tier B; 1,721 as Tier C; and 1,728 as Tier D (Piper et al., 2020). In 2019, a majority of U.S. pediatric hospitalizations occurred at general hospitals, as opposed to freestanding children’s hospitals or high-volume hospitals (Steiner et al., 2023; Weiss, Liang, & Martin, 2022). The number of U.S. hospitals with pediatric units declined from 1,753 in 2008 to 1,418 in 2018, a drop of around 19% (Leyenaar et al., 2023). There has also been an increasing trend of interfacility transfers from general hospital emergency departments to other hospitals for admission for certain pediatric conditions, such as asthma and croup (Cushing, Bucholz, & Michelson, 2020; Leyenaar et al., 2016, 2023).
This redistribution and regionalization of pediatric care influences access to care for pediatric patients because of geographic distance to service (Karamlou et al., 2020; Lorch, Myers, & Carr, 2010; Mahant & Guttmann, 2023; Ramos et al., 2020; Turner, Ricketts, & Leslie, 2020). However, some evidence suggests that regionalization can improve quality of care for certain populations, such as reducing mortality for infants with very low birth weights (Phibbs et al., 2007). Regionalization may also reduce costs in some circumstances (Lorch, Myers, & Carr, 2010). A recent National Academies report on low birth weight babies and disability noted the clear risks associated with premature birth and low birth weight and emphasized that specialized programs can improve outcomes for these babies (National Academies, 2023f; see also Aubin et al., 2023; Nguyen et al., 2013; Rouse et al., 2008; Wilson et al., 2022). Numerous studies demonstrate an association between volume and outcomes in pediatric cardiology with lower volumes associated with higher operative mortality, particularly for highly complex cases (Backer et al., 2023). Multiple professional societies have recommended categorizing centers as either essential care centers (essential services for any program, minimum of 75 index cases per year) or comprehensive care centers (services to optimize comprehensive and high-complexity care), based on structure, process, and outcome metrics (Backer et al., 2023).
Hospitals also provide critical services such as emergency and trauma care, with capacity well beyond that of retail clinics or community urgent care centers. They also provide specialized medical and surgical services and intensive care for children with more severe and complex conditions. As noted in Chapters 1 and 4, pediatric chronic conditions are relatively rare, other than a small number of high-prevalence conditions. Although primary care has a substantive role in the care of these children, they often need regular access to pediatric subspecialists, usually housed in hospital settings and larger cities.
Many low-income patients with chronic conditions have barriers to health care access, at times using multiple health care settings or systems
for care, leading to fragmented care and worse outcomes. Managed care networks increasingly deny claims for needed services (see Chapter 6), disallowing patients from receiving needed care in nearby sites or from out-of-network providers. Hospital closures and higher costs in consolidated markets have exacerbated access problems for many children, especially those from low-income families (Cushing et al., 2021; Levins, 2023; Leyenaar et al., 2023). Research examining the impact of integration of hospitals and clinic systems on costs show increases in health care prices and spending. These increases have been associated with minimal to no improvements in quality of care and potentially worse outcomes for vulnerable adult patient populations (Levin, Komanduri, & Whaley, 2023). A recent study of reports from the AHA annual survey, which included 1,088 hospitals (235 of which joined a larger health care system), found a significant association of joining a health care system with a loss of inpatient services within 5 years (Joseph, Davis, & Kahn, 2023). Less is known about the impact of hospital closures on access to pediatric acute care for children with chronic conditions and medical complexity, or the effects of consolidation on family experiences, child health outcomes, and costs.
Inpatient Care
Hospitals provide inpatient care for acutely ill children who require interventions and monitoring not available in outpatient settings. Most hospitalized children and those with highly complex needs receive care in children’s hospitals or general hospitals with pediatric programs, and the following text uses “children’s hospitals” to refer to both. Most of these two groups are teaching hospitals. Pediatric hospitals serve as regional centers, provide resource-intensive care to the sickest children, and are staffed by health care personnel with specialized training in children’s health (Piper et al., 2020). There are approximately 250 Tier A and B children’s hospitals in the United States (Children’s Hospital Association, n.d.). While children’s hospitals comprise less than 5% of all hospitals in the United States, they account for 40% of pediatric inpatient days and 50% of national pediatric costs (Cohen & Patel, 2014; Piper et al., 2020; Raval, Reiter, & McCarthy, 2022). They provide more than 95% of specialized care to treat acute and chronic conditions, including 97% of all organ transplants and 90% of all pediatric cancer care (Children’s Hospital Association, 2023; Raval, Reiter, & McCarthy, 2022) and are uniquely equipped with specialized staff, technology, and multidisciplinary teams designed to meet the specific needs of children.
Without hospitals designed to serve children, highly complex pediatric care would be more random and uncertain. Complex chronic care hospitalizations make up a growing share of inpatient care and resource utilization (Simon et al., 2010). While the total number of pediatric admissions has declined in
recent years, the percentage of admissions for children with complex chronic conditions increased by 5.7% from 2010 to 2016, and unadjusted readmission rates for patients with complex chronic conditions increased from 6.26% to 7.02% (Bucholz, Toomey, & Schuster, 2019). In 2018, pediatric patients with complex chronic care conditions accounted for 9% of all hospitalized patients, and 23% of all hospitalizations (Oztek Celebi & Senel, 2021).
Although they are far more accessible than children’s hospitals to most families, most community hospitals do not have the necessary resources, such as medical equipment and health care providers trained in pediatric care, for treating pediatric populations, especially when treating mental health conditions or addressing needs of children with disabilities (CDC, 2023d; HRSA, 2023b; National Academies, 2018). In contrast, children’s hospitals provide subspecialty hospital services to children with disabilities who may be hospitalized for an acute illness, chronic illness exacerbation, procedure, or surgery related to their underlying condition. Since only 1 in 20 U.S. hospitals is a children’s hospital, children with disabilities and complex medical conditions often must travel far distances to access services (National Academies, 2018).
Specialized children’s hospitals are also essential for children from disadvantaged backgrounds. Approximately 50% of all care provided in children’s hospitals goes to low-income children, 6% of whom have medically complex conditions (Casimir, 2019). Neighborhood-level characteristics, including household income, overcrowding, exposure to environmental toxins, poverty, and violence, are potential risk factors for hospitalization and illness severity. Using the Child Opportunity Index (COI), a validated tool that incorporates neighborhood-level factors that impact child health (Acevedo-Garcia et al., 2014; Aris et al., 2021), a 2023 study showed that 28 diagnoses (including diabetes mellitus, sickle cell disease, asthma, sleep apnea, COVID-19, and respiratory failure) were significantly more common in hospitalized children from low low-COI neighborhoods (Heneghan, Goodman, & Ramgopal, 2023). Hospitalized children from low-COI neighborhoods also had more severe illness compared with those from more advantaged neighborhoods (Heneghan, Goodman, & Ramgopal, 2023). These findings suggest the need to address disparities in neighborhood characteristics and access to care, especially for children with chronic medical conditions, when allocating resources or developing targeted programming.
Inpatient settings, including critical care units, present an opportunity to screen for and address social determinants of health that impact patient outcomes. Implementing screening for food, housing, and transportation needs in an urban safety-net hospital documented significant correlations between positive screens and race and ethnicity, insurance type, and clinical characteristics like substance use disorder (Byhoff et al., 2017; Chukmaitov et al., 2022). Fritz et al. (2020) surveyed caregivers of hospitalized pediatric patients and found many were comfortable with and accepting of social determinants of health (SDOH) screening during the inpatient stay (Gayle et al., 2023).
Screening for SDOH in the inpatient setting can inform discharge planning, facilitate referrals to community resources, and potentially improve post-discharge outcomes (Chukmaitov et al., 2022; Gayle et al., 2023).
For more than 20 years, a focus on quality improvement and learning health networks in pediatric inpatient care has improved health outcomes. For example, the Children’s Hospitals’ Solutions for Patient Safety Network is an unparalleled, collaborative effort among children’s hospitals working to transform pediatric patient and employee safety in pursuit of eliminating serious harm and improving outcomes across all children’s hospitals. Begun in the 1980s from the Ohio Children’s Hospital Association, it grew to a network of 140+ pediatric hospitals today working together to help each individual hospital make progress on implementation of the network’s best practices reporting. From 2012 to 2024, this national effort estimates 27,509 children saved from serious harm and cost savings of $585.9 million, with a consistent upward trend in harm prevented every month.4 The quality improvement learning network approach includes focused goals, a theory of change, data sharing and communication, strategic partnerships with families, and a relentless focus on results (Terao et al., 2019). Multiple positive patient outcomes have been documented from reductions in hospital-acquired infections and serious safety events to unplanned extubations (AHRQ, n.d.; Klugman et al., 2020; Lyren et al., 2017; Tripathi et al., 2023). This learning network is also focusing on racial/ethnic disparities in quality and safety (Lyren et al., 2024). Learning networks have proliferated as a successful model for innovation and quality improvement for inpatient care and specific disease conditions (Terao et al., 2019).
Subspecialty and Surgical Care
Pediatrics currently has 22 associated pediatric subspecialties accredited by the Accreditation Council for Graduate Medical Education5 (2023a,b); these, along with pediatric subspecialties in other areas,6 provide acute and chronic care expertise and skills for the highest-quality care for children.
___________________
4 See https://www.solutionsforpatientsafety.org/publications
5 The subspecialties are addiction medicine, adolescent medicine, child abuse pediatrics, clinical informatics, developmental-behavioral pediatrics, hospice and palliative medicine, internal medicine-pediatrics, neonatal-perinatal medicine, pediatric cardiology, pediatric critical care medicine, pediatric emergency medicine, pediatric endocrinology, pediatric gastroenterology, pediatric hematology oncology, pediatric hospital medicine, pediatric infectious diseases, pediatric nephrology, pediatric pulmonology, pediatric rheumatology, pediatric transplant hepatology, sleep medicine, and sports medicine.
6 Additional specialties with subspecialties for pediatrics include anesthesiology, dermatology, neurology, obstetrics and gynecology, orthopedics, otolaryngology, pathology, physical medicine and rehabilitation, psychiatry, radiology, surgery, thoracic surgery, and urology.
Health care of children with chronic illnesses, when they are not acutely ill or requiring inpatient care, generally takes place in primary care clinics and subspecialty clinics specific to their health condition. As noted in Chapter 4, children’s chronic conditions have different characteristics from chronic conditions among adult populations. Most children with chronic conditions have high-prevalence conditions, such as asthma, obesity, and mental and developmental conditions, and most receive health care in primary care or other community settings. A smaller number of children have low-prevalence conditions, such as cystic fibrosis, arthritis, cancer, sickle cell disease, or congenital heart disease, and most of these children see pediatric subspecialists regularly while receiving their primary care in community settings (Perrin, Anderson, & van Cleave, 2014).
About 10–20% of U.S. children visit a pediatric subspecialist each year (National Academies, 2023e). Pediatric subspecialty care has expanded over the past few decades because of changing epidemiology of children with medical complexity (including better survival), development of many new treatments, increased demand from parents and primary care providers, and development of new subspecialties within pediatrics. With advances in medicine, some children with conditions that were previously fatal in childhood are now living into adulthood. For instance, 45 years ago children with cystic fibrosis and sickle cell disease had a life expectancy in the teen years and most did not see adulthood; now life expectancy for children with these conditions is over 40 years of age (Cheng, Monteiro, et al., 2016). This success has required focus on transition of care to adult subspecialists and the advent of new adult subspecialties (e.g., adult congenital heart disease). The relative rarity of most pediatric chronic conditions creates different care patterns from those of most adults with chronic conditions (see the 5 Ds in Chapter 1); this differential epidemiology results in care centered at regional specialized children’s hospitals where there are pediatric subspecialists. The smaller number of children with each condition has led to regionalization of that care (unlike for older populations), and few pediatric subspecialists work outside of hospital settings (National Academies, 2023e).
Children with more complex conditions almost always require subspecialists to manage their care or collaborate with primary care providers, depending on the condition (Mosquera, Gonzalez, & Leeds, 2014; Perrin, Anderson, & van Cleave, 2014). Many children’s hospitals have established complex care clinics and programs to provide both outpatient and inpatient coordination and management for youth and young adults with medical complexity (White et al., 2018), with growing use of telemedicine. Some of these programs are disease specific (e.g., sickle cell disease clinic) and multidisciplinary (e.g., cerebral palsy clinic staffed with orthopedic surgeons, neurologists, and developmental pediatricians), while others are not;
this structure is driven by local resources and needs (National Academies, 2018). Clinical trials have shown cost reductions in establishing care coordination programs within hospitals or outpatient clinics (Cohen & Patel, 2014; Cohn et al., 2020; Mosquera, Gonzalez, & Leeds, 2014; Simon et al., 2017), albeit with mixed findings. Care coordination improves quality of care (Simon et al., 2017) and family perceptions of the family-centeredness of care (Hill, Knafl, & Santacroce, 2017; White et al., 2018).
Managing care for youth with intellectual development disorders or autism spectrum disorder provides an important example of needed coordination across subspecialties and services (Brookman-Frazee et al., 2009; McClain et al., 2020; Parker, Diamond, & Guercio, 2019) and with the primary care setting. Specialized care for children with intellectual development disorders is often based at academic children’s hospitals, requiring families to travel long distances to access specialty care (National Academies, 2022c). Programs such as ECHO, described earlier in this chapter, train clinicians in best practices for treating children with autism, making care more accessible in rural areas (Mazurek et al., 2017). More recent models for supporting individuals with intellectual development disorders throughout their lifespan emphasize a medical home that can span an individual’s lifetime from childhood.
Pediatric subspecialists work in partnership with primary care providers in caring for children who have rare health conditions or require technical procedures. Primary care clinicians may also refer to a subspecialist if the patient has not responded to conventional therapy in primary care settings or if they lack time or expertise to initiate care for patients with complex care needs (National Academies, 2023e). Primary care and subspecialty pediatric clinicians often work closely together to deliver comprehensive care for children who require subspecialty care. Team-based care among pediatric subspecialties has been associated with decreased acute health care utilization, greater patient satisfaction, and higher quality of care (National Academies, 2023e).
Many families experience long wait times or limited access to subspecialty care, especially in rural settings. An estimated 1 million to 39 million children (2–53%), depending on subspecialty, reside 80 miles or more from a subspecialist. Across hospital referral regions, there are 1 or fewer subspecialists per 100,000 children for 11 subspecialties (Turner, Ricketts, & Leslie, 2020). The shortage of subspecialty pediatricians limits the ability of health care systems to provide comprehensive, high-quality, and integrated care for children with chronic and complex medical conditions (Orr et al., 2024; Patel & Raphael, 2023; Vinci, 2021). Almost 50% of children’s hospitals reported vacancies in adolescent and child psychiatry and developmental and behavioral pediatrics, and more than 30% reported vacancies in child neurology and genetics (Orr et al., 2024;
Pediatric Nursing Certification Board, 2021; Strianese et al., 2020; Vinci, 2021). This subspecialty supply and demand mismatch also creates barriers to integrating genomics, precision medicine, and biomedical research into clinical care pathways and addressing the high rates of mental, emotional, and behavioral concerns among children and youth (see Chapter 2 and National Academies, 2023e). Genetics, developmental and behavioral pediatrics, pain management, palliative care, and child and adolescent psychiatry are the subspecialties with the longest appointment wait times. Use of telemedicine and electronic consults may mitigate some of the barriers to accessing subspecialty care (National Academies, 2023e).
Type of insurance, out-of-pocket payments, and insurance status can also affect access to subspecialty care, with children insured by Medicaid often finding longer wait times or other barriers compared with children with commercial insurance (Bisgaier & Rhodes, 2011). Other factors contribute to disparities in timely access to subspecialty care, such as language barriers and parental ability to take time off work to bring their child to appointments (National Academies, 2023e). Finally, insurance coverage across state lines can also limit access to specialized care and telemedicine. With a growing proportion of children with chronic and complex illness increasingly cared for at regional specialized children’s hospitals that may be geographically distant, maintaining care in their community can be challenging.
Coordinated care for young people with chronic conditions is also necessary for the complex transition from pediatric care to adult care (Lollar, 2010). The goals of health care transition are to (1) improve the ability of youth and young adults with and without special health care needs to manage their own health care and effectively use health services, and (2) ensure an organized process in pediatric and adult health care practices to facilitate transition preparation, transfer of care, and integration into adult-centered health care (White et al., 2018). Without an effective transition, youth with chronic conditions may face discontinuity of care, poor health outcomes, and increased rates of emergency room visits and hospitalizations (White et al., 2018). Health transitions often coincide with other events in youths’ lives, such as going away to college, starting a new job, changing living arrangements, shifting roles of parents/caregivers, and forming new relationships (Vaks et al., 2016). Common barriers to transition include lack of pediatric and adult provider skills and knowledge, lack of communication and coordination between pediatric and adult providers, lack of infrastructure and limited system supports, the patient’s difficulty in separating from their primary care provider, and lack of skilled adult specialty providers (Hergenroeder, Wiemann, & Cohen, 2015; White et al., 2018).
A structured multidisciplinary transition program may be effective in improving health outcomes for adolescent and young adult patients post-transition (Zhou et al., 2016), especially with consistent tracking to accurately monitor patient outcomes post-transition (Prior et al., 2014;
White et al., 2018; Zhou et al., 2016). These models focus on building specific self-management skills in patients, engaging the receiving team, and guiding patients through the transition, which can be particularly helpful for adolescents and young adults with complex chronic conditions (Vaks et al., 2016).
Two programs, Project SEARCH and Rising Ground, have been successful in supporting the transition from pediatric to adult care for youth and young adults with intellectual development disorders. Project SEARCH (2018), an international network developed at Cincinnati Children’s Hospital Medical Center in 1996, primarily seeks to secure competitive employment for people with disabilities. It includes a 1-year employment preparation program, featuring workplace immersion with hands-on training, classroom instruction, and career exploration. The efficacy of the Project SEARCH model in acquiring competitive employment after graduation has been evaluated in youth with autism (Wehman et al., 2017, 2020). Rising Ground is a human services organization based in New York City that offers support to individuals with intellectual developmental disorders. It features day and community programs, community residencies, and employment training to help acquire skills needed for independence (Rising Ground, n.d.).
Urgent and Emergent Care
In addition to hospital inpatient services, children also receive acute urgent and emergent care in urgent care centers and retail clinics, as well as emergency care centers. Children have specific health care needs that require specialized training, equipment, and facilities to ensure proper care (see Chapter 1; Institute of Medicine [IOM], 1998; Newgard et al., 2023). However, many general hospitals lack the necessary resources to adequately address these needs, a situation that can lead to tragic consequences (Owusu-Ansah et al., 2015). IOM conducted two major studies, including Emergency Care for Children: Growing Pains (IOM, 2007a), highlighting the deficiencies in emergency care for children and calling for systemic improvements (IOM, 1993; see also Foster et al., 2022; Newgard et al., 2023; Whyte & Evans, 2023; Woolf, Wolf, & Rivara, 2023).
Urgent care centers typically provide acute care, but at a lower level of severity than in hospital emergency centers. Retail clinics, usually staffed by nurse practitioners or physician assistants, are often co-located at pharmacies or large retail outlets and offer lower-acuity care than urgent care clinics. They can treat minor illness, administer vaccines, and treat other minor conditions. As with urgent care centers, most retail clinics are not designed to offer the whole child and family health care described in Chapter 1, which is longitudinal, relationship-based, continuous, and coordinated. While urgent care centers and retail clinics may provide convenient access at particular times of need (such as after regular office hours), they do not
replace primary care and generally do not offer routine screening, developmental surveillance, or other services characteristic of ongoing primary care in a medical home (Conners et al., 2017). In 2019, at least 25% of children (26.4%) had visited an urgent care center or retail health clinic in the previous 12 months. Non-Hispanic white children (29.2%) had higher utilization of urgent care centers and retail health clinics than non-Hispanic Black children (24.9%) and Hispanic children (22.6%; Black & Zablotsky, 2020). Commercially or publicly insured children had higher utilization than uninsured children (27.6% and 25.3% vs. 19.3%, respectively). Older children used retail clinics more than younger children, especially those under age 2 years (Mehrotra et al., 2008).
Emergency care centers that care for children may be housed within community, regional, or urban hospitals or as freestanding emergency departments, providing broader services than urgent care centers. These centers vary dramatically in the staff available to care for children, including family-trained providers working in smaller, community emergency care centers, and other staff who may be trained in other disciplines (e.g., general surgery). The level of care provided to children depends on the skill and training of providers who may care for children.
Community emergency departments frequently refer to regional specialized children’s hospitals and designated pediatric trauma centers when the care extends beyond the general care boundary outlined above in urgent or retail care settings. Regional hospital–based pediatric emergency care centers can provide specialized acute, emergent, and critical care to children of all ages. These centers are frequently staffed by board-certified emergency medicine or pediatric emergency medicine physicians, along with advanced practice registered nurses and physician assistants. Pediatric emergency care centers can provide a number of services to children, ranging from meeting the gaps in care in community settings to critical care, including intubation and ventilation; resuscitation; subspeciality consults; and transfer to inpatient care, operating room, or intensive care unit, as dictated by the patient’s condition.
This spectrum of service sites can be difficult to navigate, and parents may bring a sick child to a site that does not have the capacity to provide needed services. Earlier National Academies reports call for improving and clarifying access to emergency services, to avoid potentially tragic results (IOM, 2007; Jenkins et al., 2023; Newgard et al., 2023; Whyte & Evans, 2023).
Emergency department utilization patterns can identify high-risk patient groups, as well as areas of disparities or information gaps of patients and/or parents/caregivers. Of parents surveyed in two studies, children with asthma, disabilities, and behavioral health complaints had higher rates of urgent care and emergency department utilization than children without acute care needs (Montalbano et al., 2017). However, pediatric patients continue to utilize emergency departments for reasons that caregivers note
include perceived lack of access to their regular clinic and the perception that emergency room staff can help their child’s medical problem (Perrin et al., 1996; Pethe et al., 2019). Additional evidence has shown no association between the strength of the patient–provider relationship and nonurgent emergency department visits (Kirby, Connell, & Linneman, 2021). Likewise, children with public insurance, Black caregivers, or caregivers with lower educational attainment were significantly less likely to seek out care from their primary care provider before accessing emergency care (Ravi et al., 2021). Greater access to primary care is associated with decreased emergency department visits among the insured (Cowling et al., 2013; Johnson et al., 2021; van den Berg, van Loenen, & Westert, 2016; Vogel at al., 2019). Strategies addressing these specific high-utilizing groups need to be considered in the transformed health care system and when designing strategies to address whole population health.
PEDIATRIC HEALTH CARE WORKFORCE
A range of practitioners is responsible for the health care of children. For example, general pediatricians and pediatric subspecialty physicians focus exclusively on the health and development of infants, children, adolescents, and young adults. Historically, general pediatricians have served as the usual source of care for most U.S. children, although in rural areas family medicine physicians provide a key source of primary care for children, related in part to the fact that 95% of pediatricians practice in urban areas (Willis et al., 2020). Apart from pediatricians, primary care clinicians such as nurses (including registered and advanced practice registered nurses, nurse practitioners, and physician assistants) increasingly provide care for children, particularly in multidisciplinary team-based models of care. While many of these clinicians are involved in addressing psychosocial needs of their patients, professionals such as psychiatrists, psychologists, mental health counselors, and social workers focus their attention primarily on mental health, behavioral health, and psychosocial care needs. Many other professionals specialize in the care of children, such as dentists, pharmacists, podiatrists, and a broad array of therapists. While these members of the overall pediatric workforce are not the main focus of this report, many are active at the front lines of care and play a critical role in integrated multidisciplinary team-based care described above, as well as referral and access to health care more generally. Communication and integration of team-based care is critical for the whole child and family health care approach described in Chapter 1. Table 5-3 highlights some of these professionals and their roles.
The COVID-19 pandemic underscored the critical role of a robust and sustainable health care workforce in supporting essential health care infrastructure. The pandemic highlighted severe existing workforce shortages and
TABLE 5-3 Types of Providers for Pediatric Health Care
| Pediatric Clinicians | |
|---|---|
| Pediatricians (MD, DO) | General pediatricians focus exclusively on the health and development of infants, children, adolescents, and young adults. They often form ongoing relationships with children and their families to support their development into adulthood with unique understanding of all the factors that affect their wellbeing. |
| Pediatric subspecialists, pediatric surgeons | Pediatric subspecialists (physicians who typically complete a pediatric residency and then receive additional fellowship training in discrete areas) and pediatric surgeons are critical to ensuring state-of-the-science care and pursuing research to improve prevention, diagnosis, and treatment for children. Pediatric subspecialists augment the care provided by primary care clinicians, such as general pediatricians, advanced practice providers (e.g., advanced practice registered nurses, physician assistants), and family medicine physicians by caring for children who require technical procedures or have health conditions that occur too infrequently for primary care clinicians to gain and maintain up-to-date clinical knowledge. Approximately 10–20% of U.S. children visit a pediatric subspecialist each year (National Academies, 2023e). |
| Registered nurses | Registered nurses (RNs) are critical members of the pediatric health care team who assume numerous roles to meet a variety of care needs across diverse care settings (International Council of Nurses, 2022; National Academies, 2021e). RNs can assume essential responsibilities related to (1) caring for children with special health care needs; (2) leading teams to improve the care and reduce the costs of high-need, high-cost patients; (3) coordinating the care of children with special health care needs between primary and subspecialty clinicians; (4) assessing problems to educate and plan with patients and families; and (5) evaluating outcomes (National Academies, 2021a,b). RNs can also lead transition initiatives between pediatric and adult care. In general, nurses cover a broad continuum of care—from health promotion and disease prevention, to curative care and care coordination, to palliative care (IOM, 2011). With appropriate education and training, RNs may provide the same care traditionally delivered by other clinicians, such as “diagnostics, treatment, referral to other services, health promotion, management of chronic diseases, or management of acute problems needing same-day consultations” (Laurant et al., 2018, p. 2). In acute care settings, RNs assume care management responsibilities, supporting management of changing patient conditions, preparing patients and families for discharge by providing education and self-management support, facilitating transitions from acute to outpatient settings, and coordinating follow-up care and resources (Gonçalves et al., 2022; Semanco, Wright, & Rich, 2022). |
| Nurse practitioners | Nurse practitioners (NPs) are advance practice nurses with additional education and clinical training in the care of a specific patient population that enables them to provide care to patients autonomously (National Organization of Nurse Practitioner Faculties, 2022). While most NPs are trained in and practice in primary care settings, many pediatric NPs work in hospital and inpatient settings and one-third work in ambulatory and clinical settings, providing pediatric subspecialty care (American Association of Nurse Practitioners [AANP], 2022; Gigli et al., 2021). NPs increase children’s access to care by practicing in settings that include federally qualified health centers, retail clinics, home health and telehealth settings, schools and school-based health centers, nurse-managed health centers, ambulatory care clinics, and community and tertiary care hospitals (Pediatric Nursing Certification Board [PNCB], 2022). Most NPs who care for children are not certified specifically in pediatrics (e.g., family or psychiatric mental health NPs), and the extent of their contribution to the delivery of pediatric subspecialty care is not well known (Gigli et al., 2021). Less than 4% of NPs specialize in pediatrics (2.4% primary care pediatric NPs, 0.6% acute care pediatric NPs; AANP, 2022); the majority are family NPs (70.3%). Pediatric acute and primary care NPs report working in multiple subspecialties with pediatric patients, including adolescent care, cardiology, critical care, emergency care, gastroenterology, hematology and oncology, neonatology, and pulmonology (PNCB, 2022). |
| Clinical nurse specialists | Clinical nurse specialists (CNSs) have additional education and clinical training and follow requirements for licensure and certification. According to a 2008 report, “The CNS has a unique APRN role to integrate care across the continuum and through three spheres of influence: patient, nurse, system” (APRN Joint Dialogue Group, 2008, p. 8). CNSs may provide direct patient care, but they also collaborate with other professionals to promote evidence-based care and processes, particularly for patients with complex care needs, and they provide support and education to other health care workers and promote quality improvement initiatives (Lewandowski & Adamle, 2009; Saunders, 2015; Valdivia, 2022). In a study of the 9,470 CNSs who were registered with a national provider identifier, only 6% indicated a specialty as oncology/pediatrics, pediatrics, perinatal, or neonatal, and an additional 3% indicated a specialty in either child and adolescent or child and family psychiatric or mental health. The same study showed that the number of new CNSs specializing in pediatrics with a national provider identifier decreased between 2015 and 2019 (Reed, Arbet, & Staubli, 2021). |
| School nurses | An estimated 132,300 school nurses care for children in U.S. schools (Willgerodt, Brock, & Maughan, 2018). School nurses are frontline health care providers, serving as a bridge between the health care and education systems. Hired by school districts, health departments, or hospitals, school nurses attend to the physical and mental health of students in school. As public health sentinels, they engage school communities, parents, and health care providers to promote wellness and improve health outcomes for children. School nurses are essential to expanding access to quality health care for students, especially in light of the increasing number of students with complex health and social needs. Access to school nurses helps increase health care equity for students. For many children living in or near poverty, the school nurse may be the only health care professional they access regularly (National Academies, 2021e, p. 108). Schools are increasingly being recognized not just as core educational institutions, but also as community-based assets that can be a central component of building healthy and vibrant communities (National Academies, 2017a). Accordingly, schools and, by extension, school nurses are being incorporated into strategies for improving health care access, serving as hubs of health promotion and providers of population-based care (Maughan, 2018; National Academies, 2021e). |
| Physician assistants | Physician assistants (PAs) have the potential to play an important role in the care of children in the United States, and the National Commission on the Certification of Physician Assistants (NCCPA, 2023) offers a certification of added qualifications in pediatrics. However, the impact of PAs is limited by their relative scarcity in pediatric practice (Freed et al., 2010). According to a survey of 3,373 PAs who were certified for the first time (in 2019), 23.1% work in primary care (i.e., family medicine, internal medicine, general pediatrics; NCCPA, 2020). However, only 59 (1.8%) reported a principal clinical practice area in general pediatrics and an additional 53 (1.6%) worked in the pediatric subspecialties; none reported a principal clinical practice area in adolescent medicine. Few studies exist on the actual or conceptual use of PAs in pediatrics (Doan et al., 2012, 2013; Freed et al., 2011; Mathur et al., 2005). |
| Family medicine physicians | As part of their training, family physicians learn how to provide neonatal and routine newborn care, manage children who are acutely ill, and provide preventive health services to children (Accreditation Council for Graduate Medical Education [ACGME], 2022). ACGME has program requirements for family medicine residency programs regarding the preparation of family medicine physicians in the care of children, but most program directors report challenges in meeting the required number of encounters (Krugman et al., 2023). |
| Mental Health, Behavioral Health, and Social Care Professionals | |
| Child and adolescent psychiatrists | A child and adolescent psychiatrist (CAP) “specializes in the diagnosis and treatment of disorders of thinking, feeling, and/or behavior affecting children, adolescents, and their families” (American Academy of Child & Adolescent Psychiatry, 2023a, para. 1). CAPs work with patients and families to develop care plans that may include individual, group, or family psychotherapy; medication; and/or consultation with other physicians or professionals from schools, juvenile courts, social agencies, or other community organizations. CAPs also act as advocates for the best interests of children and adolescents and perform consultations in a variety of settings (e.g., schools, juvenile courts, social agencies). |
| Developmental-behavioral pediatricians | Developmental-behavioral pediatricians (DBPs) have had pediatric specialty training in child development and behavior. Often working in multidisciplinary settings in close collaboration with other professionals, DBPs evaluate, treat, and manage infants, children, and adolescents with a wide range of developmental and behavioral concerns and conditions, as well as physical complaints that are best addressed via a biobehavioral approach. DBPs also evaluate and monitor progress in children at risk for developmental and behavioral disorders on the basis of biological and social factors, adding understanding of the social, educational, and cultural influences on children. DBPs help train general pediatricians and other pediatric subspecialists to understand child development and behavior and improve early screening and identification. A developmental and behavioral pediatrician assesses children’s development, learning skills, and behavior and suggests remedies. They try to find underlying causes for deviations in development and behavior and coordinate treatment to move children toward the expected development pathway. |
| Psychologists | Roberts and Steele (2017) define “pediatric psychology” as a multidisciplinary field that includes “both research and clinical practice that address a range of issues related to physical and psychosocial development, health, and illness among children, adolescents, and their families” (p. 3). Psychologists possess the expertise and clinical proficiency to assist individuals in acquiring better coping strategies to manage mental health issues and various challenges in life through therapy (American Psychological Association, 2023). Psychologists can be integrated in pediatric health care settings and systems (e.g., hospitals, pediatric subspecialty clinics, primary care) to help meet the needs of children and families facing chronic illnesses or disabilities (White & Belachew, 2022). Areas of expertise for pediatric psychologists include “psychosocial, developmental and contextual factors contributing to the etiology, course and outcome of pediatric medical conditions; assessment and treatment of behavioral and emotional concomitants of illness, injury, and developmental disorders; prevention of illness and injury; promotion of health and health-related behaviors; education, training, and mentoring of psychologists and providers of medical care; improvement of health care delivery systems and advocacy for public policy that serves the needs of children, adolescents, and their families” (Society of Pediatric Psychology [SPP], 2023, para. 4). Psychologists can also receive specialty training in clinical child and adolescent psychology (Lin & Stamm, 2020). |
| Social workers | For children, social workers can play a critical role on health care teams, and can contribute to coordinating care, integrating behavioral health and primary care, and providing psychosocial support for inpatient and outpatient pediatric patients and their families (Children’s National Hospital, 2023b; Hospital for Special Surgery, 2023; Johns Hopkins Medicine, 2023; Jones et al., 2018; Ross et al., 2018). The National Association of Social Workers (NASW; 2023a) offers a Specialty Practice Section for supporting the development of children, adolescents, and young adults. The section has a particular focus on physical, emotional, and behavior disorders and supporting transitions through young adulthood. Furthermore, social workers play a key role in children’s wellbeing through their involvement in child welfare (e.g., child protective services, case management; NASW, 2023b). In general, including social workers in primary care settings has been associated with improved health outcomes (Cornell et al., 2020; Rehner, Brazeal, & Doty, 2017). |
| Additional mental and behavioral health clinicians | While they also have specialized training and assist with delivering clinical care, these clinicians often focus on prevention and recovery. They sometimes work in partnership with licensed providers, who may refer patients to them. Clinical supporters include social workers, mental health counselors, occupational therapists, certified addiction counselors, nurses, certified peer specialists, and recovery coaches. They generally focus on educating clients about their conditions; building educational, occupational, housing, and social skills; coordinating care; advocating for patients; and providing social supports to achieve behavioral health recovery goals (Counts, 2022, 2023). |
| Other Related Health Professionals | |
| Care coordinators | A variety of individuals with various titles and overlapping responsibilities help patients to coordinate their care needs across providers and to navigate the health care system overall. Some of the most common titles include care coordinators, care managers, case managers, and patient navigators. These roles are often filled by nurses or social workers. In these roles, care coordinators help to overcome barriers to care at the level of the patient, their socioeconomic environment, and the larger health care system. Activities may include patient education; assistance with insurance, transportation, or legal issues; referral to community resources; and encouragement to adhere to follow-up care (Joo & Huber, 2017; Kelly et al., 2015; Paskett, Harrop, & Wells, 2011; Woodward & Rice, 2015). While there are discrepancies in the definitions, scopes of practice, or qualifications for these individuals, there is evidence that care coordination contributes to improved outcomes in health care broadly (Berry et al., 2013; Gorin et al., 2017; NEJM Catalyst, 2018; Ruggiero, Pratt, & Antonelli, 2019). |
| Community health workers | Community health workers (CHWs) are also known as outreach workers, community health advocates, community health representatives, and patient navigators (Rosenthal, 1998; Rosenthal et al., 2010). There are more than 60,000 paid CHWs in the United States (Bureau of Labor Statistics [BLS], 2023), as well as many volunteers (HRSA, 2023a; Rosenthal et al., 2010). There is no standardized education, training, or scope of practice, for CHWs (Catalani et al., 2009). CHWs provide a wide range of services, including health education and coaching, medication adherence, care coordination, social support, outreach and engagement, health assessment and screenings, patient navigation, case management, program implementation, and referral management for medical and social services (BLS, 2023; HRSA, 2023a; National Academies, 2020b). CHWs also play an important role in addressing health disparities and improving health outcomes, particularly for underserved and marginalized populations (Cosgrove et al., 2014; HRSA, 2023a; Lewin et al., 2010; Vasan et al., 2020). Research has shown that CHWs increase disease knowledge, self-management, and health outcomes for children and youth with chronic diseases (Coutinho et al., 2020; Fox et al., 2007; Lewin et al., 2010; Randolph, 2021; Viswanathan et al., 2010). CHWs work collaboratively with clinicians, social workers, and other professionals to improve the health and wellbeing of the communities they serve; they work in a variety of settings, such as community clinics, federally qualified health centers, hospitals, schools, and public health agencies. They also often make home visits and serve an important role in engaging communities with health care services and improving access to care. |
| Child life specialists | Child life specialists (CLSs) play a crucial role in pediatric health care by providing developmentally appropriate support to children and their families. They use therapeutic play, age-appropriate communication, and preparation strategies to help children understand and cope with medical experiences, reducing anxiety and stress. CLSs collaborate with health care teams to offer psychosocial support, prepare children for procedures, and educate families about treatments. Their work contributes to improved patient satisfaction, better clinical outcomes, and enhanced overall health care experiences. By addressing the emotional and developmental needs of pediatric patients, CLSs significantly improve the quality of care and support provided in health care settings (Rosenblatt et al., 2024). |
SOURCE: Adapted from National Academies, 2023b.
burnout across health care professions in the United States. It also exacerbated discrepant workforce distribution, leading to severe systemic disparities across geographic, racial, and socioeconomic divides (ASPE, 2022b). It magnified the barriers to timely and appropriate health care access in uninsured, rural, low socioeconomic, under-resourced, and historically marginalized communities. The COVID-19 pandemic did drive the explosion of innovative telehealth services supporting existing health care infrastructure and services, but further development may be limited by existing inequities in funding and shortage of staff to support these services (Association of American Medical Colleges, 2021; Boudreau et al., 2022). The pandemic also emphasized the value of coordinated, multidisciplinary team-based models of care, which, as discussed earlier in this chapter, can link families with needed community resources. In addition to improving patient outcomes, team-based care may help improve clinician wellbeing and mitigate burnout (Mijakoski et al., 2015; Smith et al., 2018; Welp & Manser, 2016).
The pediatric health care workforce faces a number of challenges, including a shortage of well-distributed, trained professionals for primary care and subspecialty care; maldistribution of professionals and lack of representativeness in the workforce (see Chapter 3); and reduced health care worker wellbeing and increased burnout. Optimal pediatric care requires teams of clinicians and professionals, including the breadth of relevant practitioners, that specialize in whole child and family health care, are skilled in management of childhood conditions, and are knowledgeable in child development and child, adolescent, and family needs.
The recent National Academies report on the pediatric subspecialty workforce (National Academies, 2023e) documented shortages of pediatric primary care and subspecialty care physicians. The 2024 National Resident Matching Program accentuated concerns with an increase in unfilled pediatric positions and less than 8% of medical students choosing pediatrics as their specialty (Schering, 2024). Popularity of pediatrics has waned, as pediatricians are among the lowest-paid physicians and educational debt is rising. Of pediatric residents graduating with educational debt, the average debt increased to $264,000 in 2020 (after adjusting for inflation) and half of all residents reported $200,000 or more in debt (AAP, 2024a). Unfortunately, this is consistent with the lower pay of other professions who care for children, the nation’s most treasured resource (e.g., schoolteachers, child care workers, child life specialists).
Shortage and Maldistribution of Pediatric Health Care Professionals
Shortages in the pediatric health care workforce reflect the current and projected landscape of severe health care worker shortages across the nation and the need to expand the workforce, especially in primary care, pediatric subspecialty care, and mental health. Through 2036, the NCHWA projects
a shortage of 3,100 pediatricians, especially in nonmetro areas, where the projected supply is only 69% for pediatricians (vs. 101% in metro areas; HRSA, 2023a). Family medicine physicians provide 16–21% of children’s visits to physicians (Jetty et al., 2021; National Academies, 2023d; Phillips et al., 2005); they also have significant projected shortages (HRSA, 2022a) and often spend less time caring for children than pediatricians (Bazemore et al., 2012; Eden et al., 2020; Freed, Segalowitz, & Dewey, 2004; Freed et al., 2010; Wasserman et al., 2019).
Similar to concerns about primary care shortages, growing demands of the pediatric population may outpace the growth of the pediatric subspecialty workforce (see National Academies, 2023e). The nationwide epidemics of mental illness and substance use disorders have highlighted the dramatic shortage (discussed earlier in this chapter) of qualified professionals across the spectrum of all licensed practitioners (especially psychologists, psychiatrists, addiction counselors, mental health counselors, and psychiatric and mental health nurse practitioners), for both adults and children and youth.
The lack of diversity in the pediatric workforce contributes to health care disparities and the maldistribution of providers in underserved areas (Montez, 2021; Vinci, 2021). Physicians from under-represented racial/ethnic groups are more likely to practice in areas with higher proportions of underserved populations. For example, Xierali and colleagues (2021) found that Black, Hispanic, and American Indian/Alaska Native physicians were more likely to care for larger shares of underserved populations compared to their White counterparts. Increasing workforce diversity can therefore help address provider shortages in underserved communities (Guevara et al., 2023). Furthermore, patient–provider racial/ethnic concordance can improve communication, increase patient satisfaction, and enhance adherence to treatment recommendations (Montez, 2021; Orr et al., 2024). As the pediatric population in the United States becomes increasingly diverse, it is crucial for the workforce to reflect this diversity to provide culturally competent care and build trust with patients and families from diverse backgrounds. Efforts to enhance diversity in the pediatric pipeline, such as pipeline programs, holistic admissions processes, and inclusive institutional climates, are essential to cultivating a workforce equipped to meet the needs of all children (Guevara et al., 2023; Orr et al., 2024).
Workforce Wellbeing and Burnout
The pediatric workforce, like other parts of the health care workforce, has faced substantial burnout, exacerbated by the pandemic. While burnout has been a growing problem for years (National Academies, 2019e), the COVID-19 pandemic was a serious stressor on an already fragile workforce. A 2022 AAP report noted that burnout among pediatricians increased
from 35.3% in 2011 to 46.3% in 2014 (McClafferty et al., 2022), with reports of more than 50–60% in 2022 (Lucy et al., 2023).
Burnout affects productivity in the workforce, with reduced efforts among health workers (Dyrbye, Satele, & West, 2021). Conversely, clinician wellbeing supports improved patient–clinician relationships, a high-functioning care team, and an engaged and effective workforce (National Academies, 2019e). Some groups experience additional stressors that can increase burnout. Doctors of color and those working in underserved communities face disproportionate amounts of stress because of the sociopolitical-economic challenges of the particularly vulnerable children in the disenfranchised communities they serve (McClafferty et al., 2022). Women, who make up two-thirds of pediatric doctors, report higher levels of burnout than male physicians (Lyubarova, Salman, & Rittenberg, 2023; McClafferty et al., 2022), especially in emotional distress measurements, with higher risk of suicidality. Long hours of practice are compounded by carrying the bulk of family responsibilities; women who are employed full time spend an additional 8.5 hours per week on domestic care (Jolly et al., 2014). One-third of physician mothers reported discrimination related to their role as a mother, primarily regarding pregnancy or maternity leave (Adesoye et al., 2017; Halley et al., 2018). Women in pediatrics, notably women of color, also report gender-based harassment in the workplace (McClafferty et al., 2022). Expressing fatigue and the desire for self-care remains stigmatized in a workforce culture that discourages asking for help with mental health.
Several strategies exist for diminishing burnout, including team-based care, environments that support providers in their mental health, and improved work hours. A 2019 systematic review of about 50 studies concluded that strategies that promoted team-based care and incorporated medical assistants or scribes to complete electronic health record documentation and other administrative tasks were strongly linked to reducing clinician burnout and stress (DeChant et al., 2019). Other aspects of teamwork that reduced burnout included improved communication among physicians and expanded team member responsibilities that allowed team members to work at the top of their skills and better allocate clinical workload. The following section continues the discussion of strategies to address workforce challenges.
Strategies for Addressing Workforce Challenges
Multiple strategies are needed to address pediatric workforce shortages, maldistribution, and burnout. As described earlier, team-based care in both primary and subspecialty pediatrics can both transform care and address some workforce challenges. Building teams with the capacity to address the array of social, educational, developmental, health, and community
needs of children and families, including those with chronic conditions, can improve care and decrease demands on pediatric clinicians to meet these varied needs alone. The growth of teams—with adequate and appropriate financing—provides one of the most promising approaches to meeting child health workforce needs.
Among several strategies, a focus on fixing salary disparities between pediatrics and other specialties and improving workforce diversity is needed. Additional strategies must include training of the broad array of participants in the child health workforce, increased focus on evidence-based practices, innovating new models of care including upstream prevention, and using new technology to increase care efficiency and reach.
Pediatric primary care clinicians have increased their capacity to address some subspecialty and mental health issues, a strategy promoted for additional expansion in the National Academies subspecialty workforce report. Pediatric nurse practitioners have increased in primary and subspecialty care in outpatient and inpatient settings with further growth expected (Gigli et al., 2019; Toia et al., 2024). The workforce of community health workers as part of the team has grown with increasing evidence of improved outcomes and reduced disparities (Coker et al., 2014). New models of team care such as the use of genetic counselors with nurse practitioners will be necessary to address shortages (Stewart & Svihovec, 2022). A focus on upstream primary prevention emphasized in this report can reduce the need for more intensive and costly health services.
CONCLUSION
This chapter described the nature of health care in clinical settings, changes occurring with the settings and workforce, resulting opportunities and challenges, and the progress made in strengthening the content of pediatric primary and subspecialty care for children and youth. Progress has included growth in early intervention and mental and behavioral health services, improved coordination of care among multiple providers, and greater inclusion of community health workers and similar staff to help families develop skills, find resources, enhance their children’s lives, and build lasting relationships. These recent trends all include strategies for better addressing the needs of children across the life course.
The pediatric health care system is broad and diverse. Main components of the system include primary care, hospital care, subspecialty care, and their interaction. Primary care comes from a diverse array of programs, from traditional office practice to community health centers, large medical groups, hospitals, and various public clinics. The mental and behavioral health care system, comprising office practices, hospital care, community programs, and more, has long had only limited integration and interaction
with the rest of the pediatric care system, although increasing efforts to integrate mental health into primary and subspecialty care have shown promise. Schools too (see Chapter 8) provide substantial amounts of prevention and treatment, especially for mental and behavioral health issues. Progress in improving health and wellbeing outcomes has occurred in all these sectors; however, health care financing has not kept pace with these advances and has prevented their widespread and coordinated uptake (see Chapter 6).
In addition, the health care system in general suffers from a workforce shortage, exacerbated by increased demand for services, workforce stress and burnout, geographical disparities, and training gaps. Most components of the pediatric health care system have faced similar challenges with burnout and workforce shortages. Projections indicate that these shortages will worsen, necessitating innovative approaches to payment, recruitment, training, and retention of pediatric health care providers and teams, as well as new health care delivery models for addressing the evolving needs of children and families.
The transformation of child health care practices has involved adopting more holistic, preventive, and developmental approaches that integrate health care practice with community services. Innovations in primary care, especially broadening the scope of services to include new ways of supporting families and identifying issues of concern, often built from interdisciplinary teams, have shown success in improving child health and wellbeing and decreasing unnecessary care. Supporting upstream prevention in pediatric care has helped to address root causes of health issues before they manifest as clinical symptoms or conditions. This approach recognizes the influence of social, economic, environmental, and relational factors that affect child health and wellbeing, and includes interventions at the earliest stages to promote optimal health and wellbeing in children and their life trajectories. The several stages in child development, including pregnancy and childbirth, infancy, early childhood, school age, adolescence, and young adulthood, each require different strategies and activities for health care. There is evidence to support the ability of these holistic approaches to address health disparities and community health concerns—the need now is to bring these many advances to scale.
Hospital and subspecialty care have also changed in recent years, with fewer hospitalizations; more concentration in urban centers; and greater capacity for subspecialty care, coordinated with the primary care community. The tremendous growth in new science and the understanding of many chronic conditions have made hospital-based subspecialty care ever more complex and sophisticated in pediatric evaluations and treatments. Telehealth has proven to be a valuable tool in pediatric care, offering flexibility, increased access, and improved outcomes with recent growth in other forms of remote monitoring and communication. There is
a need for consistent coverage policies across states and payers to ensure equitable access to these services. Effective coordination between primary and specialty care, essential for managing complex cases, requires robust care coordination mechanisms, integrated health information systems, and collaborative care models to ensure seamless transitions and comprehensive care. Learning health systems offer key strategies for improving quality and lowering costs.
This page intentionally left blank.

























































